-
PDF
- Split View
-
Views
-
Cite
Cite
Carolien M. Wind, Maarten F. Schim van der Loeff, Magnus Unemo, Rob Schuurman, Alje P. van Dam, Henry J. C. de Vries, Test of Cure for Anogenital Gonorrhoea Using Modern RNA-Based and DNA-Based Nucleic Acid Amplification Tests: A Prospective Cohort Study, Clinical Infectious Diseases, Volume 62, Issue 11, 1 June 2016, Pages 1348–1355, https://doi.org/10.1093/cid/ciw141
Close - Share Icon Share
Abstract
Background. The use of nucleic acid amplification tests (NAATs) to diagnose Neisseria gonorrhoeae infections complicates the performance of a test of cure (TOC) to monitor treatment failure, if this is indicated. As evidence for the timing of TOC using modern NAATs is limited, we performed a prospective cohort study to assess time to clearance when using modern RNA- and DNA-based NAATs.
Methods. We included patients with anogenital gonorrhoea visiting the Sexually Transmitted Infection Clinic Amsterdam from March through October 2014. After treatment with ceftriaxone mono- or dual therapy (with azithromycin or doxycycline), anal, vaginal, or urine samples were self-collected during 28 consecutive days, and analyzed using an RNA-based NAAT (Aptima Combo 2) and a DNA-based NAAT (Cobas 4800). Clearance was defined as 3 consecutive negative results, and blips as isolated positive results following clearance.
Results. We included 77 patients; 5 self-cleared gonorrhoea before treatment and 10 were lost to follow-up. Clearance rate of the remaining 62 patients was 100%. Median time to clearance was 2 days, with a range of 1–7 days for RNA-based NAAT and 1–15 days for DNA-based NAAT. The risk of finding a blip after clearance was 0.8% and 1.5%, respectively. One patient had a reinfection.
Conclusions. If indicated, we recommend that TOC be performed for anogenital gonorrhoea at least 7 or 14 days after administering therapy, when using modern RNA- or DNA-based NAATs, respectively. When interpreting TOC results for possible treatment failure, both the occurrence of blips and a possible reinfection need to be taken into account.
(See the Editorial Commentary by Barbee and Golden on pages 1356–9.)
Antimicrobial resistance (AMR) is an emergent worldwide public health problem, also affecting sexually transmitted infections (STIs). Treatment failures and resistance of Neisseria gonorrhoeae to the last-resort monotherapy of extended-spectrum cephalosporins have been reported globally [1–6].
To diagnose gonorrhoea international guidelines recommend a nucleic acid amplification test (NAAT) because of superior sensitivity compared to bacterial culture [7, 8]. As molecular methods to determine AMR are still suboptimal, the decreased use of culture compromises AMR surveillance [9, 10].
The frequent occurrence of asymptomatic infections (10%–90% depending on sex and anatomical site) and the limited possibilities to determine AMR [8] call for other methods to monitor treatment outcome, such as test of cure (TOC). In many countries, TOC was abandoned mainly due to excellent treatment results [11, 12]. The World Health Organization, Centers for Disease Control and Prevention, and international guidelines suggest that TOC be performed for gonorrhoea in certain cases (eg, pharyngeal infections, persistent symptoms, or nonstandard therapy) [7, 8, 13, 14].
Traditionally, TOC is based on bacterial culture, and evidence for the timing of TOC when using NAATs is limited [15–18]. We conducted a prospective cohort study to assess the appropriate timing of TOC after treatment of anogenital gonorrhoea when using modern RNA- and DNA-based NAATs.
METHODS
Study Population
We included patients visiting the STI Outpatient Clinic in Amsterdam, the Netherlands, from March through October 2014. Eligible were patients with anogenital gonorrhoea, who were 18 years of age or older and to whom routine treatment was prescribed (Supplementary Figure 1). Patients coinfected with Chlamydia trachomatis were not excluded. Patients participated in the study only once, and only 1 anatomical site was designated for follow-up. We gave endocervical and rectal infections priority over urethral infections to create a balanced inclusion. Sociodemographic and clinical characteristics were extracted from the electronic patient file. Ethical approval was obtained from the medical ethics committee of the Academic Medical Center Amsterdam (NL45935.018.13); all patients provided written informed consent.
Sample Size
We assumed 100% clearance of N. gonorrhoeae after 21 days [15, 16]. We considered TOC not recommendable before at least 95% of patients cleared the infection, so the upper limit of the 95% confidence interval (CI) of the proportion cleared had to be ≤0.05. With these assumptions and 30% expected dropout, the required sample size was 80.
Study Procedure
Patients received instructions on the self-collection of anal, vaginal, or urine samples. They self-collected pretreatment NAAT samples: 1 for RNA-based and 1 for DNA-based NAAT. They received routine treatment consisting of a single intramuscular dose of 500 mg ceftriaxone [19]. If coinfection with C. trachomatis was suspected or proven, azithromycin 1000 mg once orally was given for urogenital infections and doxycycline 100 mg twice daily for 7, 14, or 21 days for anorectal infections.
Following treatment, patients self-collected RNA and DNA samples of the designated anatomical site for 28 consecutive days, and stored these at room temperature. When half the sample size for rectal or vaginal samples was reached, the instructed collection order of RNA and DNA swabs was reversed. Patients were requested to abstain from sexual contact or use condoms, and refrain from vaginal or rectal douching. Additionally, they kept a diary on sample collection, medication use, sexual contact, and vaginal/rectal douching during the study period. Within 35 days after inclusion, patients visited the STI clinic to return their samples and diary. At this end-of-study visit, a study nurse collected samples from urethra, rectum, or endocervix for both NAATs and for direct culture.
NAAT Testing for N. gonorrhoeae
Samples for RNA-based NAAT were collected using Aptima vaginal swab specimen kits for vaginal and anal samples, and Aptima urine specimen kits for urine samples. All were tested using the Aptima Combo 2 assay for N. gonorrhoeae and C. trachomatis on the Tigris direct tube sampling system (Hologic, San Diego, California), and relative light units (RLUs) were reported. Equivocal results were retested using the Aptima GC assay (Hologic). Repeated equivocal results were considered positive for the analysis. We excluded samples with repeated invalid results. Pretreatment samples negative for N. gonorrhoeae were considered proof of self-clearance and these patients were excluded.
Samples for DNA-based NAAT were collected using Cobas polymerase chain reaction (PCR) female swab sample kits for vaginal and anal sampling, and the Cobas PCR urine sample kits for urine samples. All were tested using the Cobas 4800 assay for N. gonorrhoeae and C. trachomatis (Roche, Basel, Switzerland); the cycle threshold (Ct) of positive samples was reported. If in retrospect the pretreatment sample was negative for N. gonorrhoeae, we excluded the DNA results of that patient from the analysis. Pretreatment samples with discrepant RNA and DNA results were retested, using the Aptima GC assay for RNA samples, and the Abbott RealTime CT/NG assay (Abbott, Abbott Park, Illinois) for DNA samples.
Samples negative for both N. gonorrhoeae and C. trachomatis on the first day after treatment were tested for human DNA, using the β-globin internal control of the Cobas 4800 HPV assay (Roche, Basel, Switzerland). If β-globin was negative, we assumed the collection was incorrect and excluded the patient from the corresponding NAAT analysis.
Direct N. gonorrhoeae Culture
A study nurse collected direct N. gonorrhoeae cultures before treatment and at the end-of-study visit, using GC-Lect agar plates (Becton Dickinson, Breda, the Netherlands) incubated at 37°C in 5% carbon dioxide for 48–72 hours. Neisseria gonorrhoeae was species verified using colony morphology, catalase and oxidase testing, Gram-stained smears, and DNA hybridization (AccuProbe, Hologic). Minimal inhibitory concentrations of ceftriaxone, azithromycin, and doxycycline in N. gonorrhoeae isolates were determined using Etests (bioMérieux, Marcy-l’Étoile, France), according to the manufacturer's instructions, and interpreted using European Committee on Antimicrobial Susceptibility Testing breakpoints. For doxycycline we used the tetracycline breakpoint [20].
Statistical Analysis
The primary endpoint was clearance of N. gonorrhoeae nucleic acids using RNA- or DNA-based NAAT. We defined clearance as 3 consecutive negative results following a positive result; we allowed 1 missing sample between the last positive and the first negative result. In a secondary analysis we used a more lenient definition: 2 consecutive negative NAAT results. Clearance was compared by anatomical site using χ2, Fisher exact, or Kruskal–Wallis tests. We analyzed determinants for time to clearance using Kaplan–Meier curves, log-rank testing, and Cox regression analysis.
We defined reinfection as positive test results on at least 3 consecutive days after clearance; tests had to be positive for both RNA and DNA on at least 1 day.
The secondary endpoint was intermittent presence of bacterial RNA or DNA (“blip”) [15]. We defined a blip as a positive test following clearance not due to reinfection or treatment failure. In patients without an exact day of clearance due to missing samples, we considered all samples after the first 3 consecutive negative results at risk for blips. We analyzed possible predictors by logistic regression using generalized estimated equation models to account for correlated data.
RESULTS
Participants
At the STI outpatient clinic, 462 patients were diagnosed with anogenital gonorrhoea from March through October 2014 (Supplementary Figure 1). After evaluation of the inclusion and exclusion criteria, patients were invited to participate. Upon receiving information about the study, 77 patients participated. Five patients had self-cleared their infection and were excluded in the first week after inclusion. Ten patients were lost to follow-up, resulting in 62 patients included in the analysis. Those retained were significantly more often coinfected with C. trachomatis than those lost-to follow-up (data not shown).
Baseline Characteristics
The study population consisted of 21 women with an endocervical infection, 20 men with a urethral infection, and 21 with a rectal infection (Table 1). Six men (15%) were heterosexual and 35 (85%) were men who have sex with men (MSM). The median age was 24 years (interquartile range, 22–34 years); women were significantly younger than men (median age, 22 years and 29 years, respectively; P < .001). Twelve men (19%) were human immunodeficiency virus positive; 83% had CD4+ cell counts of at least 500 cells/µL. Twenty-three patients (37%) had a coinfection with C. trachomatis. Sixty per cent of patients were symptomatic, which was significantly more common in urethral infections. The median time between diagnosis and inclusion was 7 days (range, 0–9 days). Direct culture was performed in 57 patients (92%); 51 were positive (89%). No isolates were resistant to ceftriaxone, 2 were resistant to azithromycin, and 21 were resistant to doxycycline. At inclusion, 23 patients (37%) received ceftriaxone monotherapy, 27 (44%) received ceftriaxone with azithromycin, and 12 (19%) received ceftriaxone with doxycycline.
| Characteristic . | Total . | Urethra . | Rectum . | Endocervix . | P Value . |
|---|---|---|---|---|---|
| Included patients | 62 | 20 | 21 | 21 | |
| Sex | … | ||||
| Male | 41 (66) | 20 (100) | 21 (100) | 0 (0) | |
| Female | 21 (34) | 0 (0) | 0 (0) | 21 (100) | |
| Age, y, median (IQR) | 24 (22–34) | 29 (24–34) | 32 (24–41) | 22 (19–23) | .0001 |
| Ethnicity | .02 | ||||
| Dutch | 27 (44) | 5 (25) | 14 (67) | 8 (38) | |
| Non-Dutch | 35 (56) | 15 (75) | 7 (33) | 13 (62) | |
| Sexual risk group | … | ||||
| MSM | 35 (56) | 14 (70) | 21 (100) | 0 (0) | |
| Heterosexual male | 6 (10) | 6 (30) | 0 (0) | 0 (0) | |
| Female | 21 (34) | 0 (0) | 0 (0) | 21 (100) | |
| HIV infected | 12 (19) | 5 (25) | 7 (33) | 0 (0) | .01 |
| Using cART | 10 (83) | 3 (60) | 7 (100) | … | .15 |
| CD4+ count, cells/µL | 1.00 | ||||
| 350–499 | 2 (17) | 1 (20) | 1 (14) | … | |
| ≥500 | 10 (83) | 4 (80) | 6 (86) | … | |
| Neisseria gonorrhoeae infection | |||||
| Urogenital | 41 (66) | 20 (100) | 0 (0) | 21 (100) | … |
| Rectal | 31 (50) | 5 (25) | 21 (100) | 5 (24) | … |
| Pharyngeal | 14 (23) | 4 (20) | 7 (33) | 3 (14) | .36 |
| Chlamydia trachomatis coinfection | 23 (37) | 7 (35) | 7 (33) | 9 (43) | .79 |
| Symptoms or signs at examinationa,b | 37 (60) | 18 (90) | 10 (48) | 9 (43) | .003 |
| Time to inclusion, d, median (IQR) | 7 (0–9) | 0 (0–0) | 9 (0–11) | 9 (7–10) | .0001 |
| Positive Gram-stained smear | 25/34 (74) | 18/18 (100) | 7/7 (100) | 0/9 (0) | <.0001 |
| Positive culturec | 51/57 (89) | 18/18 (100) | 19/20 (95) | 14/19 (73) | .02 |
| MIC, mg/L, mean (range) | |||||
| Ceftriaxone | 0.006 (<0.002–0.047) | 0.006 (0.002–0.047) | 0.008 (0.002–0.047) | 0.003 (<0.002–0.008) | .10 |
| Azithromycin | 0.142 (<0.016–1) | 0.159 (<0.016–0.75) | 0.222 (0.047–1) | 0.068 (0.023–0.19) | .001 |
| Doxycycline | 1.093 (0.094–24) | 1.067 (0.125–8) | 1.415 (0.5–24) | 0.793 (0.094–8) | .15 |
| RLU value pretreatment, mean (range)d | 1226.2 (567–1350) | 1261.0 (1217–1350) | 1177.8 (567–1322) | 1249.8 (957–1327) | .57 |
| Ct value pretreatment, mean (range) | 28.5 (23.5–37.9) | 26.2 (23.5–30.6) | 28.6 (24.8–32.1) | 31.0 (26.4–37.9) | .0001 |
| Treatment at inclusion | <.0001 | ||||
| Ceftriaxone monotherapy | 23 (37) | 3 (15) | 9 (43) | 11 (52) | |
| Ceftriaxone + azithromycin | 27 (44) | 17 (85) | 2 (10) | 8 (38) | |
| Ceftriaxone + doxycycline | 12 (19) | 0 (0) | 10 (48) | 2 (10) |
| Characteristic . | Total . | Urethra . | Rectum . | Endocervix . | P Value . |
|---|---|---|---|---|---|
| Included patients | 62 | 20 | 21 | 21 | |
| Sex | … | ||||
| Male | 41 (66) | 20 (100) | 21 (100) | 0 (0) | |
| Female | 21 (34) | 0 (0) | 0 (0) | 21 (100) | |
| Age, y, median (IQR) | 24 (22–34) | 29 (24–34) | 32 (24–41) | 22 (19–23) | .0001 |
| Ethnicity | .02 | ||||
| Dutch | 27 (44) | 5 (25) | 14 (67) | 8 (38) | |
| Non-Dutch | 35 (56) | 15 (75) | 7 (33) | 13 (62) | |
| Sexual risk group | … | ||||
| MSM | 35 (56) | 14 (70) | 21 (100) | 0 (0) | |
| Heterosexual male | 6 (10) | 6 (30) | 0 (0) | 0 (0) | |
| Female | 21 (34) | 0 (0) | 0 (0) | 21 (100) | |
| HIV infected | 12 (19) | 5 (25) | 7 (33) | 0 (0) | .01 |
| Using cART | 10 (83) | 3 (60) | 7 (100) | … | .15 |
| CD4+ count, cells/µL | 1.00 | ||||
| 350–499 | 2 (17) | 1 (20) | 1 (14) | … | |
| ≥500 | 10 (83) | 4 (80) | 6 (86) | … | |
| Neisseria gonorrhoeae infection | |||||
| Urogenital | 41 (66) | 20 (100) | 0 (0) | 21 (100) | … |
| Rectal | 31 (50) | 5 (25) | 21 (100) | 5 (24) | … |
| Pharyngeal | 14 (23) | 4 (20) | 7 (33) | 3 (14) | .36 |
| Chlamydia trachomatis coinfection | 23 (37) | 7 (35) | 7 (33) | 9 (43) | .79 |
| Symptoms or signs at examinationa,b | 37 (60) | 18 (90) | 10 (48) | 9 (43) | .003 |
| Time to inclusion, d, median (IQR) | 7 (0–9) | 0 (0–0) | 9 (0–11) | 9 (7–10) | .0001 |
| Positive Gram-stained smear | 25/34 (74) | 18/18 (100) | 7/7 (100) | 0/9 (0) | <.0001 |
| Positive culturec | 51/57 (89) | 18/18 (100) | 19/20 (95) | 14/19 (73) | .02 |
| MIC, mg/L, mean (range) | |||||
| Ceftriaxone | 0.006 (<0.002–0.047) | 0.006 (0.002–0.047) | 0.008 (0.002–0.047) | 0.003 (<0.002–0.008) | .10 |
| Azithromycin | 0.142 (<0.016–1) | 0.159 (<0.016–0.75) | 0.222 (0.047–1) | 0.068 (0.023–0.19) | .001 |
| Doxycycline | 1.093 (0.094–24) | 1.067 (0.125–8) | 1.415 (0.5–24) | 0.793 (0.094–8) | .15 |
| RLU value pretreatment, mean (range)d | 1226.2 (567–1350) | 1261.0 (1217–1350) | 1177.8 (567–1322) | 1249.8 (957–1327) | .57 |
| Ct value pretreatment, mean (range) | 28.5 (23.5–37.9) | 26.2 (23.5–30.6) | 28.6 (24.8–32.1) | 31.0 (26.4–37.9) | .0001 |
| Treatment at inclusion | <.0001 | ||||
| Ceftriaxone monotherapy | 23 (37) | 3 (15) | 9 (43) | 11 (52) | |
| Ceftriaxone + azithromycin | 27 (44) | 17 (85) | 2 (10) | 8 (38) | |
| Ceftriaxone + doxycycline | 12 (19) | 0 (0) | 10 (48) | 2 (10) |
Data are presented as No. (%) unless otherwise indicated.
Abbreviations: cART, combination antiretroviral therapy; Ct, cycle threshold; HIV, human immunodeficiency virus; IQR, interquartile range; MIC, minimal inhibitory concentration; MSM, men who have sex with men; RLU, relative light unit.
a Symptoms included discharge, itch, burning, frequent or painful urination, bleeding, abdominal pain, pain during sex, anal cramps or pain, and changed defecation.
b Signs included red urethra, discharge, bleeding, fragile mucosa, swelling, or anal ulcerations.
c All cultures were obtained by a nurse from urethral or rectal specimens; of the endocervical infections, 5 cultures were from vaginal specimens (of which 3 were culture positive) and 14 were from endocervical specimens (of which 11 were culture positive).
d Based on 39 samples positive for N. gonorrhoeae only.
| Characteristic . | Total . | Urethra . | Rectum . | Endocervix . | P Value . |
|---|---|---|---|---|---|
| Included patients | 62 | 20 | 21 | 21 | |
| Sex | … | ||||
| Male | 41 (66) | 20 (100) | 21 (100) | 0 (0) | |
| Female | 21 (34) | 0 (0) | 0 (0) | 21 (100) | |
| Age, y, median (IQR) | 24 (22–34) | 29 (24–34) | 32 (24–41) | 22 (19–23) | .0001 |
| Ethnicity | .02 | ||||
| Dutch | 27 (44) | 5 (25) | 14 (67) | 8 (38) | |
| Non-Dutch | 35 (56) | 15 (75) | 7 (33) | 13 (62) | |
| Sexual risk group | … | ||||
| MSM | 35 (56) | 14 (70) | 21 (100) | 0 (0) | |
| Heterosexual male | 6 (10) | 6 (30) | 0 (0) | 0 (0) | |
| Female | 21 (34) | 0 (0) | 0 (0) | 21 (100) | |
| HIV infected | 12 (19) | 5 (25) | 7 (33) | 0 (0) | .01 |
| Using cART | 10 (83) | 3 (60) | 7 (100) | … | .15 |
| CD4+ count, cells/µL | 1.00 | ||||
| 350–499 | 2 (17) | 1 (20) | 1 (14) | … | |
| ≥500 | 10 (83) | 4 (80) | 6 (86) | … | |
| Neisseria gonorrhoeae infection | |||||
| Urogenital | 41 (66) | 20 (100) | 0 (0) | 21 (100) | … |
| Rectal | 31 (50) | 5 (25) | 21 (100) | 5 (24) | … |
| Pharyngeal | 14 (23) | 4 (20) | 7 (33) | 3 (14) | .36 |
| Chlamydia trachomatis coinfection | 23 (37) | 7 (35) | 7 (33) | 9 (43) | .79 |
| Symptoms or signs at examinationa,b | 37 (60) | 18 (90) | 10 (48) | 9 (43) | .003 |
| Time to inclusion, d, median (IQR) | 7 (0–9) | 0 (0–0) | 9 (0–11) | 9 (7–10) | .0001 |
| Positive Gram-stained smear | 25/34 (74) | 18/18 (100) | 7/7 (100) | 0/9 (0) | <.0001 |
| Positive culturec | 51/57 (89) | 18/18 (100) | 19/20 (95) | 14/19 (73) | .02 |
| MIC, mg/L, mean (range) | |||||
| Ceftriaxone | 0.006 (<0.002–0.047) | 0.006 (0.002–0.047) | 0.008 (0.002–0.047) | 0.003 (<0.002–0.008) | .10 |
| Azithromycin | 0.142 (<0.016–1) | 0.159 (<0.016–0.75) | 0.222 (0.047–1) | 0.068 (0.023–0.19) | .001 |
| Doxycycline | 1.093 (0.094–24) | 1.067 (0.125–8) | 1.415 (0.5–24) | 0.793 (0.094–8) | .15 |
| RLU value pretreatment, mean (range)d | 1226.2 (567–1350) | 1261.0 (1217–1350) | 1177.8 (567–1322) | 1249.8 (957–1327) | .57 |
| Ct value pretreatment, mean (range) | 28.5 (23.5–37.9) | 26.2 (23.5–30.6) | 28.6 (24.8–32.1) | 31.0 (26.4–37.9) | .0001 |
| Treatment at inclusion | <.0001 | ||||
| Ceftriaxone monotherapy | 23 (37) | 3 (15) | 9 (43) | 11 (52) | |
| Ceftriaxone + azithromycin | 27 (44) | 17 (85) | 2 (10) | 8 (38) | |
| Ceftriaxone + doxycycline | 12 (19) | 0 (0) | 10 (48) | 2 (10) |
| Characteristic . | Total . | Urethra . | Rectum . | Endocervix . | P Value . |
|---|---|---|---|---|---|
| Included patients | 62 | 20 | 21 | 21 | |
| Sex | … | ||||
| Male | 41 (66) | 20 (100) | 21 (100) | 0 (0) | |
| Female | 21 (34) | 0 (0) | 0 (0) | 21 (100) | |
| Age, y, median (IQR) | 24 (22–34) | 29 (24–34) | 32 (24–41) | 22 (19–23) | .0001 |
| Ethnicity | .02 | ||||
| Dutch | 27 (44) | 5 (25) | 14 (67) | 8 (38) | |
| Non-Dutch | 35 (56) | 15 (75) | 7 (33) | 13 (62) | |
| Sexual risk group | … | ||||
| MSM | 35 (56) | 14 (70) | 21 (100) | 0 (0) | |
| Heterosexual male | 6 (10) | 6 (30) | 0 (0) | 0 (0) | |
| Female | 21 (34) | 0 (0) | 0 (0) | 21 (100) | |
| HIV infected | 12 (19) | 5 (25) | 7 (33) | 0 (0) | .01 |
| Using cART | 10 (83) | 3 (60) | 7 (100) | … | .15 |
| CD4+ count, cells/µL | 1.00 | ||||
| 350–499 | 2 (17) | 1 (20) | 1 (14) | … | |
| ≥500 | 10 (83) | 4 (80) | 6 (86) | … | |
| Neisseria gonorrhoeae infection | |||||
| Urogenital | 41 (66) | 20 (100) | 0 (0) | 21 (100) | … |
| Rectal | 31 (50) | 5 (25) | 21 (100) | 5 (24) | … |
| Pharyngeal | 14 (23) | 4 (20) | 7 (33) | 3 (14) | .36 |
| Chlamydia trachomatis coinfection | 23 (37) | 7 (35) | 7 (33) | 9 (43) | .79 |
| Symptoms or signs at examinationa,b | 37 (60) | 18 (90) | 10 (48) | 9 (43) | .003 |
| Time to inclusion, d, median (IQR) | 7 (0–9) | 0 (0–0) | 9 (0–11) | 9 (7–10) | .0001 |
| Positive Gram-stained smear | 25/34 (74) | 18/18 (100) | 7/7 (100) | 0/9 (0) | <.0001 |
| Positive culturec | 51/57 (89) | 18/18 (100) | 19/20 (95) | 14/19 (73) | .02 |
| MIC, mg/L, mean (range) | |||||
| Ceftriaxone | 0.006 (<0.002–0.047) | 0.006 (0.002–0.047) | 0.008 (0.002–0.047) | 0.003 (<0.002–0.008) | .10 |
| Azithromycin | 0.142 (<0.016–1) | 0.159 (<0.016–0.75) | 0.222 (0.047–1) | 0.068 (0.023–0.19) | .001 |
| Doxycycline | 1.093 (0.094–24) | 1.067 (0.125–8) | 1.415 (0.5–24) | 0.793 (0.094–8) | .15 |
| RLU value pretreatment, mean (range)d | 1226.2 (567–1350) | 1261.0 (1217–1350) | 1177.8 (567–1322) | 1249.8 (957–1327) | .57 |
| Ct value pretreatment, mean (range) | 28.5 (23.5–37.9) | 26.2 (23.5–30.6) | 28.6 (24.8–32.1) | 31.0 (26.4–37.9) | .0001 |
| Treatment at inclusion | <.0001 | ||||
| Ceftriaxone monotherapy | 23 (37) | 3 (15) | 9 (43) | 11 (52) | |
| Ceftriaxone + azithromycin | 27 (44) | 17 (85) | 2 (10) | 8 (38) | |
| Ceftriaxone + doxycycline | 12 (19) | 0 (0) | 10 (48) | 2 (10) |
Data are presented as No. (%) unless otherwise indicated.
Abbreviations: cART, combination antiretroviral therapy; Ct, cycle threshold; HIV, human immunodeficiency virus; IQR, interquartile range; MIC, minimal inhibitory concentration; MSM, men who have sex with men; RLU, relative light unit.
a Symptoms included discharge, itch, burning, frequent or painful urination, bleeding, abdominal pain, pain during sex, anal cramps or pain, and changed defecation.
b Signs included red urethra, discharge, bleeding, fragile mucosa, swelling, or anal ulcerations.
c All cultures were obtained by a nurse from urethral or rectal specimens; of the endocervical infections, 5 cultures were from vaginal specimens (of which 3 were culture positive) and 14 were from endocervical specimens (of which 11 were culture positive).
d Based on 39 samples positive for N. gonorrhoeae only.
Behavior After Inclusion
Of the included 62 patients, 58% missed at least 1 sample (Table 2). The median number of collected samples was 27 (range, 20–28). Rectal or vaginal douching was reported by 11 patients (26%), sexual contact by 40 (65%), and unprotected sex by 17 (27%) patients. Two patients used antibiotics other than the initial doxycycline treatment: 1 patient received a second dose of azithromycin due to vomiting within 24 hours of the initial dose, and 1 patient received ofloxacin and metronidazole for intercurrent pelvic inflammatory disease. In retrospect, both patients took the additional antibiotics after clearance of N. gonorrhoeae.
Behavior After Inclusion and Clearance of Neisseria gonorrhoeae RNA and DNA
| Characteristic . | Total . | Urethra . | Rectum . | Endocervix . | P Value . |
|---|---|---|---|---|---|
| Behavior after inclusion | |||||
| No. of samples collected, median (range) | 27 (20–28) | 28 (25–28) | 28 (20–28) | 27 (20–28) | .01 |
| Patients with missed samples | 36 (58) | 8 (40) | 10 (48) | 18 (86) | .006 |
| Rectal/vaginal douching | 11 (26) | … | 7 (33) | 4 (19) | .29 |
| Sexual contact | 40 (65) | 14 (70) | 12 (57) | 14 (67) | .67 |
| Unprotected sex | 17 (27) | 4 (20) | 5 (24) | 8 (38) | .39 |
| RNA clearancea | |||||
| Patients in the analysisb | 61 | 19 (31) | 21 (34) | 21 (34) | |
| Clearance during follow-up | 61 (100) | 19 (100) | 21 (100) | 21 (100) | |
| Reinfection after clearance | 1 (2) | 0 (0) | 0 (0) | 1 (5) | .63 |
| Day of clearance definablec | 56 (92) | 17 (89) | 21 (100) | 18 (86) | .26 |
| Time to clearance, d, median (range) | 2 (1–7) | 2 (1–5) | 2 (1–6) | 3 (1–7) | .04 |
| RNA blipsd | |||||
| Samples at risk for blip | 1308 | 438 | 468 | 402 | |
| No. of blips | 11 | 0 | 8 | 3 | |
| No. of patients | 6 (10) | 0 (0) | 4 (19) | 2 (10) | .15 |
| Time to first blip, d, median (range) | 7 (3–23) | … | 7.5 (3–23) | 6 (3–9) | .48 |
| RLU value, mean (range)e | 220.6 (91–463) | … | 241.1 (116–463) | 195.9 (91–407) | .48 |
| DNA clearancea | |||||
| Patients in the analysisf | 61 | 20 (33) | 20 (33) | 21 (34) | |
| Clearance during follow-up | 61 (100) | 20 (100) | 20 (100) | 21 (100) | |
| Reinfection after clearance | 1 (2) | 0 (0) | 0 (0) | 1 (5) | 1.00 |
| Day of clearance definablec | 59 (97) | 19 (95) | 20 (100) | 20 (95) | 1.00 |
| Time to clearance, d, median (range) | 2 (1–15) | 3 (1–15) | 2 (1–4) | 3.5 (1–8) | <.001 |
| DNA blipsd | |||||
| Samples at risk for blip | 1285 | 422 | 461 | 402 | |
| No. of blips | 19 | 5 | 10 | 4 | |
| No. of patients | 10 (16) | 2 (10) | 5 (25) | 3 (14) | .48 |
| Time to first blip, d, median (range) | 4.5 (1–9) | 2 (1–3) | 5 (2–9) | 6 (3–6) | .23 |
| Ct value, mean (range) | 37.9 (35.4–39.5) | 38.5 (38.0–39.3) | 37.5 (35.7–39.5) | 38.0 (35.4–39.3) | .54 |
| Characteristic . | Total . | Urethra . | Rectum . | Endocervix . | P Value . |
|---|---|---|---|---|---|
| Behavior after inclusion | |||||
| No. of samples collected, median (range) | 27 (20–28) | 28 (25–28) | 28 (20–28) | 27 (20–28) | .01 |
| Patients with missed samples | 36 (58) | 8 (40) | 10 (48) | 18 (86) | .006 |
| Rectal/vaginal douching | 11 (26) | … | 7 (33) | 4 (19) | .29 |
| Sexual contact | 40 (65) | 14 (70) | 12 (57) | 14 (67) | .67 |
| Unprotected sex | 17 (27) | 4 (20) | 5 (24) | 8 (38) | .39 |
| RNA clearancea | |||||
| Patients in the analysisb | 61 | 19 (31) | 21 (34) | 21 (34) | |
| Clearance during follow-up | 61 (100) | 19 (100) | 21 (100) | 21 (100) | |
| Reinfection after clearance | 1 (2) | 0 (0) | 0 (0) | 1 (5) | .63 |
| Day of clearance definablec | 56 (92) | 17 (89) | 21 (100) | 18 (86) | .26 |
| Time to clearance, d, median (range) | 2 (1–7) | 2 (1–5) | 2 (1–6) | 3 (1–7) | .04 |
| RNA blipsd | |||||
| Samples at risk for blip | 1308 | 438 | 468 | 402 | |
| No. of blips | 11 | 0 | 8 | 3 | |
| No. of patients | 6 (10) | 0 (0) | 4 (19) | 2 (10) | .15 |
| Time to first blip, d, median (range) | 7 (3–23) | … | 7.5 (3–23) | 6 (3–9) | .48 |
| RLU value, mean (range)e | 220.6 (91–463) | … | 241.1 (116–463) | 195.9 (91–407) | .48 |
| DNA clearancea | |||||
| Patients in the analysisf | 61 | 20 (33) | 20 (33) | 21 (34) | |
| Clearance during follow-up | 61 (100) | 20 (100) | 20 (100) | 21 (100) | |
| Reinfection after clearance | 1 (2) | 0 (0) | 0 (0) | 1 (5) | 1.00 |
| Day of clearance definablec | 59 (97) | 19 (95) | 20 (100) | 20 (95) | 1.00 |
| Time to clearance, d, median (range) | 2 (1–15) | 3 (1–15) | 2 (1–4) | 3.5 (1–8) | <.001 |
| DNA blipsd | |||||
| Samples at risk for blip | 1285 | 422 | 461 | 402 | |
| No. of blips | 19 | 5 | 10 | 4 | |
| No. of patients | 10 (16) | 2 (10) | 5 (25) | 3 (14) | .48 |
| Time to first blip, d, median (range) | 4.5 (1–9) | 2 (1–3) | 5 (2–9) | 6 (3–6) | .23 |
| Ct value, mean (range) | 37.9 (35.4–39.5) | 38.5 (38.0–39.3) | 37.5 (35.7–39.5) | 38.0 (35.4–39.3) | .54 |
Data are presented as No. (%) unless otherwise indicated.
Abbreviations: Ct, cycle threshold; RLU, relative light unit.
a Based on a definition of 3 consecutive negative tests following a positive test.
b One of 62 patients was excluded due to negative results for Neisseria gonorrhoeae, Chlamydia trachomatis, and human DNA (β-globin) in the first sample after treatment.
c The exact day of clearance could not be defined due to missing samples in the period of clearance.
d Blip was defined as a positive test following clearance. Samples from all patients were included; for those without an exact day of clearance due to missing samples, all samples after the first 3 consecutive negative results were considered at risk for blips.
e Including samples positive for N. gonorrhoeae only (n = 7).
f One of 62 patients was excluded due to a negative pretreatment result for N. gonorrhoeae DNA.
Behavior After Inclusion and Clearance of Neisseria gonorrhoeae RNA and DNA
| Characteristic . | Total . | Urethra . | Rectum . | Endocervix . | P Value . |
|---|---|---|---|---|---|
| Behavior after inclusion | |||||
| No. of samples collected, median (range) | 27 (20–28) | 28 (25–28) | 28 (20–28) | 27 (20–28) | .01 |
| Patients with missed samples | 36 (58) | 8 (40) | 10 (48) | 18 (86) | .006 |
| Rectal/vaginal douching | 11 (26) | … | 7 (33) | 4 (19) | .29 |
| Sexual contact | 40 (65) | 14 (70) | 12 (57) | 14 (67) | .67 |
| Unprotected sex | 17 (27) | 4 (20) | 5 (24) | 8 (38) | .39 |
| RNA clearancea | |||||
| Patients in the analysisb | 61 | 19 (31) | 21 (34) | 21 (34) | |
| Clearance during follow-up | 61 (100) | 19 (100) | 21 (100) | 21 (100) | |
| Reinfection after clearance | 1 (2) | 0 (0) | 0 (0) | 1 (5) | .63 |
| Day of clearance definablec | 56 (92) | 17 (89) | 21 (100) | 18 (86) | .26 |
| Time to clearance, d, median (range) | 2 (1–7) | 2 (1–5) | 2 (1–6) | 3 (1–7) | .04 |
| RNA blipsd | |||||
| Samples at risk for blip | 1308 | 438 | 468 | 402 | |
| No. of blips | 11 | 0 | 8 | 3 | |
| No. of patients | 6 (10) | 0 (0) | 4 (19) | 2 (10) | .15 |
| Time to first blip, d, median (range) | 7 (3–23) | … | 7.5 (3–23) | 6 (3–9) | .48 |
| RLU value, mean (range)e | 220.6 (91–463) | … | 241.1 (116–463) | 195.9 (91–407) | .48 |
| DNA clearancea | |||||
| Patients in the analysisf | 61 | 20 (33) | 20 (33) | 21 (34) | |
| Clearance during follow-up | 61 (100) | 20 (100) | 20 (100) | 21 (100) | |
| Reinfection after clearance | 1 (2) | 0 (0) | 0 (0) | 1 (5) | 1.00 |
| Day of clearance definablec | 59 (97) | 19 (95) | 20 (100) | 20 (95) | 1.00 |
| Time to clearance, d, median (range) | 2 (1–15) | 3 (1–15) | 2 (1–4) | 3.5 (1–8) | <.001 |
| DNA blipsd | |||||
| Samples at risk for blip | 1285 | 422 | 461 | 402 | |
| No. of blips | 19 | 5 | 10 | 4 | |
| No. of patients | 10 (16) | 2 (10) | 5 (25) | 3 (14) | .48 |
| Time to first blip, d, median (range) | 4.5 (1–9) | 2 (1–3) | 5 (2–9) | 6 (3–6) | .23 |
| Ct value, mean (range) | 37.9 (35.4–39.5) | 38.5 (38.0–39.3) | 37.5 (35.7–39.5) | 38.0 (35.4–39.3) | .54 |
| Characteristic . | Total . | Urethra . | Rectum . | Endocervix . | P Value . |
|---|---|---|---|---|---|
| Behavior after inclusion | |||||
| No. of samples collected, median (range) | 27 (20–28) | 28 (25–28) | 28 (20–28) | 27 (20–28) | .01 |
| Patients with missed samples | 36 (58) | 8 (40) | 10 (48) | 18 (86) | .006 |
| Rectal/vaginal douching | 11 (26) | … | 7 (33) | 4 (19) | .29 |
| Sexual contact | 40 (65) | 14 (70) | 12 (57) | 14 (67) | .67 |
| Unprotected sex | 17 (27) | 4 (20) | 5 (24) | 8 (38) | .39 |
| RNA clearancea | |||||
| Patients in the analysisb | 61 | 19 (31) | 21 (34) | 21 (34) | |
| Clearance during follow-up | 61 (100) | 19 (100) | 21 (100) | 21 (100) | |
| Reinfection after clearance | 1 (2) | 0 (0) | 0 (0) | 1 (5) | .63 |
| Day of clearance definablec | 56 (92) | 17 (89) | 21 (100) | 18 (86) | .26 |
| Time to clearance, d, median (range) | 2 (1–7) | 2 (1–5) | 2 (1–6) | 3 (1–7) | .04 |
| RNA blipsd | |||||
| Samples at risk for blip | 1308 | 438 | 468 | 402 | |
| No. of blips | 11 | 0 | 8 | 3 | |
| No. of patients | 6 (10) | 0 (0) | 4 (19) | 2 (10) | .15 |
| Time to first blip, d, median (range) | 7 (3–23) | … | 7.5 (3–23) | 6 (3–9) | .48 |
| RLU value, mean (range)e | 220.6 (91–463) | … | 241.1 (116–463) | 195.9 (91–407) | .48 |
| DNA clearancea | |||||
| Patients in the analysisf | 61 | 20 (33) | 20 (33) | 21 (34) | |
| Clearance during follow-up | 61 (100) | 20 (100) | 20 (100) | 21 (100) | |
| Reinfection after clearance | 1 (2) | 0 (0) | 0 (0) | 1 (5) | 1.00 |
| Day of clearance definablec | 59 (97) | 19 (95) | 20 (100) | 20 (95) | 1.00 |
| Time to clearance, d, median (range) | 2 (1–15) | 3 (1–15) | 2 (1–4) | 3.5 (1–8) | <.001 |
| DNA blipsd | |||||
| Samples at risk for blip | 1285 | 422 | 461 | 402 | |
| No. of blips | 19 | 5 | 10 | 4 | |
| No. of patients | 10 (16) | 2 (10) | 5 (25) | 3 (14) | .48 |
| Time to first blip, d, median (range) | 4.5 (1–9) | 2 (1–3) | 5 (2–9) | 6 (3–6) | .23 |
| Ct value, mean (range) | 37.9 (35.4–39.5) | 38.5 (38.0–39.3) | 37.5 (35.7–39.5) | 38.0 (35.4–39.3) | .54 |
Data are presented as No. (%) unless otherwise indicated.
Abbreviations: Ct, cycle threshold; RLU, relative light unit.
a Based on a definition of 3 consecutive negative tests following a positive test.
b One of 62 patients was excluded due to negative results for Neisseria gonorrhoeae, Chlamydia trachomatis, and human DNA (β-globin) in the first sample after treatment.
c The exact day of clearance could not be defined due to missing samples in the period of clearance.
d Blip was defined as a positive test following clearance. Samples from all patients were included; for those without an exact day of clearance due to missing samples, all samples after the first 3 consecutive negative results were considered at risk for blips.
e Including samples positive for N. gonorrhoeae only (n = 7).
f One of 62 patients was excluded due to a negative pretreatment result for N. gonorrhoeae DNA.
Clearance of N. gonorrhoeae RNA
One patient was excluded due to negative results for N. gonorrhoeae RNA and human DNA in the first RNA sample after treatment (Table 2). None of the other patients experienced a treatment failure. Because of missing samples in the days around clearance, we determined the exact day of clearance for 56 patients (92%). The median time to clearance was 2 days (range, 1–7 days). After 6 days, 95% of patients had cleared RNA (Figure 1A); this was reached after 5 days for urethra and rectum, and after 7 days for endocervix. Results were identical with the alternative definition of clearance (2 consecutive negative results; data not shown). One patient was reinfected at day 13 (7 days after clearance; RLU value at day 13, 1307).
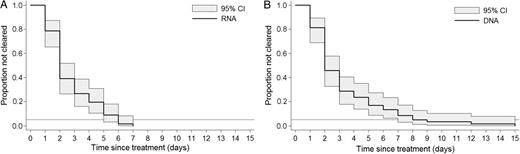
Time to clearance of Neisseria gonorrhoeae RNA (A) and DNA (B), with 95% confidence interval (CI). The horizontal line represents 95% clearance.
Determinants of Time to Clearance of N. gonorrhoeae RNA
Univariable Cox regression analysis (Table 3) showed a significant association with sexual risk group (P = .02); clearance was significantly slower for women compared with men (hazard ratio [HR], 0.53 [95% CI, .29–.96]; P = .03). Kaplan–Meier curves and log-rank testing (Figure 2A) showed a significant association with anatomical site (P = .02); clearance was slower for endocervical compared with urethral (P = .01) and rectal infections (P = .03). Because anatomical site, sex, and sexual risk group were either mutually exclusive (men cannot provide a cervical sample) or almost 100% correlated, we could not include >1 of these variables in a multivariable model.
Univariable Cox Regression Analysis of Determinants of Time to Clearance of Neisseria gonorrhoeae
| . | Clearance of RNA (n = 56) . | Clearance of DNA (n = 59) . | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Characteristic . | No. . | PD . | CR . | 95% CI . | HR . | 95% CI . | P Value . | No. . | PD . | CR . | 95% CI . | HR . | 95% CI . | P Value . |
| Sex | .03 | .25 | ||||||||||||
| Male | 38 | 89 | 0.43 | .31–.59 | 1.00 | 39 | 119 | 0.33 | .24–.45 | 1.00 | ||||
| Female | 18 | 65 | 0.28 | .17–.44 | 0.53 | .29–.96 | 20 | 81 | 0.25 | .16–.38 | 0.73 | .42–1.26 | ||
| Age, y | .06 | .45 | ||||||||||||
| ≤23 | 23 | 79 | 0.29 | .19–.44 | 1.00 | 26 | 102 | 0.25 | .17–.37 | 1.00 | ||||
| 24–29 | 13 | 26 | 0.50 | .29–.86 | 2.28 | 1.10–4.72 | 13 | 44 | 0.30 | .17–.51 | 1.19 | .60–2.33 | ||
| ≥30 | 20 | 49 | 0.41 | .26–.63 | 1.77 | .93–3.38 | 20 | 54 | 0.37 | .24–.57 | 1.47 | .81–2.67 | ||
| Ethnicity | .34 | .24 | ||||||||||||
| Dutch | 25 | 76 | 0.33 | .22–.49 | 1.00 | 27 | 77 | 0.35 | .24–.51 | 1.00 | ||||
| Non-Dutch | 31 | 78 | 0.40 | .28–.57 | 1.30 | .76–2.23 | 32 | 123 | 0.26 | .18–.37 | 0.73 | .43–1.23 | ||
| Sexual risk group | .02 | .05 | ||||||||||||
| MSM | 33 | 82 | 0.40 | .29–.57 | 1.00 | 33 | 84 | 0.39 | .28–.55 | 1.00 | ||||
| Heterosexual male | 5 | 7 | 0.71 | .30–1.72 | 2.47 | .93–6.50 | 6 | 35 | 0.17 | .08–.38 | 0.35 | .12–1.03 | ||
| Female | 18 | 65 | 0.28 | .17–.44 | 0.56 | .31–1.04 | 20 | 81 | 0.25 | .16–.38 | 0.61 | .34–1.07 | ||
| HIV | .45 | .26 | ||||||||||||
| Negative | 45 | 127 | 0.35 | .26–.47 | 1.00 | 48 | 173 | 0.28 | .21–.37 | 1.00 | ||||
| Positive | 11 | 27 | 0.41 | .23–.74 | 1.31 | .66–2.58 | 11 | 27 | 0.41 | .23–.74 | 1.50 | .77–2.94 | ||
| Anatomical site | .09 | .004 | ||||||||||||
| Rectum | 21 | 51 | 0.41 | .27–.63 | 1.00 | 20 | 36 | 0.56 | .36–.86 | 1.00 | ||||
| Urethra | 17 | 38 | 0.45 | .28–.72 | 1.13 | .60–2.16 | 19 | 83 | 0.23 | .15–.36 | 0.33 | .16–.67 | ||
| Endocervix | 18 | 65 | 0.28 | .17–.44 | 0.56 | .29–1.07 | 20 | 81 | 0.25 | .16–.38 | 0.36 | .18–.72 | ||
| Chlamydia trachomatis coinfection | .43 | .22 | ||||||||||||
| No | 35 | 91 | 0.38 | .28–.54 | 1.00 | 37 | 110 | 0.34 | .24–.46 | 1.00 | ||||
| Yes | 21 | 63 | 0.33 | .22–.51 | 0.80 | .46–1.39 | 22 | 90 | 0.24 | .16–.37 | 0.72 | .41–1.24 | ||
| Symptoms or signsa,b | .72 | .12 | ||||||||||||
| No | 23 | 61 | 0.38 | .25–.57 | 1.00 | 24 | 64 | 0.38 | .25–.56 | 1.00 | ||||
| Yes | 33 | 93 | 0.35 | .25–.50 | 0.90 | .53–1.55 | 35 | 136 | 0.26 | .18–.36 | 0.65 | .38–1.12 | ||
| Time to inclusion | .36 | .37 | ||||||||||||
| 0 d | 22 | 53 | 0.42 | .27–.63 | 1.00 | 24 | 92 | 0.26 | .17–.39 | 1.00 | ||||
| ≥1 d | 34 | 101 | 0.34 | .24–.47 | 0.77 | .45–1.34 | 35 | 108 | 0.32 | .23–.45 | 1.28 | .74–2.20 | ||
| Ceftriaxone MIC, mg/Lc | .75 | .22 | ||||||||||||
| ≤0.016 | 37 | 103 | 0.34 | .26–.50 | 1.00 | 40 | 155 | 0.26 | .19–.35 | 1.00 | ||||
| >0.016 | 9 | 27 | 0.33 | .17–.64 | 0.89 | .43–1.85 | 9 | 21 | 0.43 | .22–.82 | 1.64 | .77–3.49 | ||
| Azithromycin MIC, mg/Ld | .72 | .17 | ||||||||||||
| ≤0.25 | 34 | 101 | 0.34 | .24–.47 | 1.00 | 37 | 149 | 0.25 | .18–.34 | 1.00 | ||||
| 0.25–0.5 | 10 | 25 | 0.40 | .22–.74 | 1.29 | .62–2.65 | 10 | 24 | 0.42 | .22–.77 | 1.75 | .84–3.64 | ||
| >0.5 | 2 | 4 | 0.50 | .13–2.00 | 1.54 | .36–6.62 | 2 | 3 | 0.67 | .17–2.67 | 3.18 | .74–13.75 | ||
| Doxycycline MIC, mg/Le | .68 | .25 | ||||||||||||
| ≤0.5 | 9 | 30 | 0.30 | .16–.58 | 1.00 | 11 | 57 | 0.19 | .11–.35 | 1.00 | ||||
| 0.5–1.0 | 16 | 39 | 0.41 | .25–.67 | 1.40 | .61–3.20 | 17 | 52 | 0.33 | .20–.53 | 1.80 | .81–3.98 | ||
| >1.0 | 21 | 61 | 0.34 | .22–.53 | 1.10 | .50–2.46 | 21 | 67 | 0.31 | .20–.48 | 1.77 | .82–3.80 | ||
| Treatment at inclusion | .62 | .03 | ||||||||||||
| Ceftriaxone monotherapy | 21 | 57 | 0.37 | .24–.57 | 1.00 | 21 | 67 | 0.31 | .20–.48 | 1.00 | ||||
| Ceftriaxone + azithromycin | 23 | 69 | 0.33 | .22–.50 | 0.82 | .45–1.49 | 26 | 112 | 0.23 | .16–.34 | 0.71 | .39–1.28 | ||
| Ceftriaxone + doxycycline | 12 | 28 | 0.43 | .24–.75 | 1.14 | .56–2.33 | 12 | 21 | 0.57 | .32–1.01 | 2.01 | .94–4.30 | ||
| . | Clearance of RNA (n = 56) . | Clearance of DNA (n = 59) . | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Characteristic . | No. . | PD . | CR . | 95% CI . | HR . | 95% CI . | P Value . | No. . | PD . | CR . | 95% CI . | HR . | 95% CI . | P Value . |
| Sex | .03 | .25 | ||||||||||||
| Male | 38 | 89 | 0.43 | .31–.59 | 1.00 | 39 | 119 | 0.33 | .24–.45 | 1.00 | ||||
| Female | 18 | 65 | 0.28 | .17–.44 | 0.53 | .29–.96 | 20 | 81 | 0.25 | .16–.38 | 0.73 | .42–1.26 | ||
| Age, y | .06 | .45 | ||||||||||||
| ≤23 | 23 | 79 | 0.29 | .19–.44 | 1.00 | 26 | 102 | 0.25 | .17–.37 | 1.00 | ||||
| 24–29 | 13 | 26 | 0.50 | .29–.86 | 2.28 | 1.10–4.72 | 13 | 44 | 0.30 | .17–.51 | 1.19 | .60–2.33 | ||
| ≥30 | 20 | 49 | 0.41 | .26–.63 | 1.77 | .93–3.38 | 20 | 54 | 0.37 | .24–.57 | 1.47 | .81–2.67 | ||
| Ethnicity | .34 | .24 | ||||||||||||
| Dutch | 25 | 76 | 0.33 | .22–.49 | 1.00 | 27 | 77 | 0.35 | .24–.51 | 1.00 | ||||
| Non-Dutch | 31 | 78 | 0.40 | .28–.57 | 1.30 | .76–2.23 | 32 | 123 | 0.26 | .18–.37 | 0.73 | .43–1.23 | ||
| Sexual risk group | .02 | .05 | ||||||||||||
| MSM | 33 | 82 | 0.40 | .29–.57 | 1.00 | 33 | 84 | 0.39 | .28–.55 | 1.00 | ||||
| Heterosexual male | 5 | 7 | 0.71 | .30–1.72 | 2.47 | .93–6.50 | 6 | 35 | 0.17 | .08–.38 | 0.35 | .12–1.03 | ||
| Female | 18 | 65 | 0.28 | .17–.44 | 0.56 | .31–1.04 | 20 | 81 | 0.25 | .16–.38 | 0.61 | .34–1.07 | ||
| HIV | .45 | .26 | ||||||||||||
| Negative | 45 | 127 | 0.35 | .26–.47 | 1.00 | 48 | 173 | 0.28 | .21–.37 | 1.00 | ||||
| Positive | 11 | 27 | 0.41 | .23–.74 | 1.31 | .66–2.58 | 11 | 27 | 0.41 | .23–.74 | 1.50 | .77–2.94 | ||
| Anatomical site | .09 | .004 | ||||||||||||
| Rectum | 21 | 51 | 0.41 | .27–.63 | 1.00 | 20 | 36 | 0.56 | .36–.86 | 1.00 | ||||
| Urethra | 17 | 38 | 0.45 | .28–.72 | 1.13 | .60–2.16 | 19 | 83 | 0.23 | .15–.36 | 0.33 | .16–.67 | ||
| Endocervix | 18 | 65 | 0.28 | .17–.44 | 0.56 | .29–1.07 | 20 | 81 | 0.25 | .16–.38 | 0.36 | .18–.72 | ||
| Chlamydia trachomatis coinfection | .43 | .22 | ||||||||||||
| No | 35 | 91 | 0.38 | .28–.54 | 1.00 | 37 | 110 | 0.34 | .24–.46 | 1.00 | ||||
| Yes | 21 | 63 | 0.33 | .22–.51 | 0.80 | .46–1.39 | 22 | 90 | 0.24 | .16–.37 | 0.72 | .41–1.24 | ||
| Symptoms or signsa,b | .72 | .12 | ||||||||||||
| No | 23 | 61 | 0.38 | .25–.57 | 1.00 | 24 | 64 | 0.38 | .25–.56 | 1.00 | ||||
| Yes | 33 | 93 | 0.35 | .25–.50 | 0.90 | .53–1.55 | 35 | 136 | 0.26 | .18–.36 | 0.65 | .38–1.12 | ||
| Time to inclusion | .36 | .37 | ||||||||||||
| 0 d | 22 | 53 | 0.42 | .27–.63 | 1.00 | 24 | 92 | 0.26 | .17–.39 | 1.00 | ||||
| ≥1 d | 34 | 101 | 0.34 | .24–.47 | 0.77 | .45–1.34 | 35 | 108 | 0.32 | .23–.45 | 1.28 | .74–2.20 | ||
| Ceftriaxone MIC, mg/Lc | .75 | .22 | ||||||||||||
| ≤0.016 | 37 | 103 | 0.34 | .26–.50 | 1.00 | 40 | 155 | 0.26 | .19–.35 | 1.00 | ||||
| >0.016 | 9 | 27 | 0.33 | .17–.64 | 0.89 | .43–1.85 | 9 | 21 | 0.43 | .22–.82 | 1.64 | .77–3.49 | ||
| Azithromycin MIC, mg/Ld | .72 | .17 | ||||||||||||
| ≤0.25 | 34 | 101 | 0.34 | .24–.47 | 1.00 | 37 | 149 | 0.25 | .18–.34 | 1.00 | ||||
| 0.25–0.5 | 10 | 25 | 0.40 | .22–.74 | 1.29 | .62–2.65 | 10 | 24 | 0.42 | .22–.77 | 1.75 | .84–3.64 | ||
| >0.5 | 2 | 4 | 0.50 | .13–2.00 | 1.54 | .36–6.62 | 2 | 3 | 0.67 | .17–2.67 | 3.18 | .74–13.75 | ||
| Doxycycline MIC, mg/Le | .68 | .25 | ||||||||||||
| ≤0.5 | 9 | 30 | 0.30 | .16–.58 | 1.00 | 11 | 57 | 0.19 | .11–.35 | 1.00 | ||||
| 0.5–1.0 | 16 | 39 | 0.41 | .25–.67 | 1.40 | .61–3.20 | 17 | 52 | 0.33 | .20–.53 | 1.80 | .81–3.98 | ||
| >1.0 | 21 | 61 | 0.34 | .22–.53 | 1.10 | .50–2.46 | 21 | 67 | 0.31 | .20–.48 | 1.77 | .82–3.80 | ||
| Treatment at inclusion | .62 | .03 | ||||||||||||
| Ceftriaxone monotherapy | 21 | 57 | 0.37 | .24–.57 | 1.00 | 21 | 67 | 0.31 | .20–.48 | 1.00 | ||||
| Ceftriaxone + azithromycin | 23 | 69 | 0.33 | .22–.50 | 0.82 | .45–1.49 | 26 | 112 | 0.23 | .16–.34 | 0.71 | .39–1.28 | ||
| Ceftriaxone + doxycycline | 12 | 28 | 0.43 | .24–.75 | 1.14 | .56–2.33 | 12 | 21 | 0.57 | .32–1.01 | 2.01 | .94–4.30 | ||
Abbreviations: CI, confidence interval; CR, clearance rate per days of observation; HIV, human immunodeficiency virus; HR, hazard ratio; MIC, minimal inhibitory concentration; MSM, men who have sex with men; PD, person-days of follow-up.
a Symptoms included discharge, itch, burning, frequent or painful urination, bleeding, abdominal pain, pain during sex, anal cramps or pain, and changed defecation.
b Signs included red urethra, discharge, bleeding, fragile mucosa, swelling, or anal ulcerations.
c Cutoff based on European Committee on Antimicrobial Susceptibility Testing (EUCAST) epidemiological cutoff.
d Based on EUCAST breakpoints.
e Based on EUCAST breakpoints for tetracycline.
Univariable Cox Regression Analysis of Determinants of Time to Clearance of Neisseria gonorrhoeae
| . | Clearance of RNA (n = 56) . | Clearance of DNA (n = 59) . | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Characteristic . | No. . | PD . | CR . | 95% CI . | HR . | 95% CI . | P Value . | No. . | PD . | CR . | 95% CI . | HR . | 95% CI . | P Value . |
| Sex | .03 | .25 | ||||||||||||
| Male | 38 | 89 | 0.43 | .31–.59 | 1.00 | 39 | 119 | 0.33 | .24–.45 | 1.00 | ||||
| Female | 18 | 65 | 0.28 | .17–.44 | 0.53 | .29–.96 | 20 | 81 | 0.25 | .16–.38 | 0.73 | .42–1.26 | ||
| Age, y | .06 | .45 | ||||||||||||
| ≤23 | 23 | 79 | 0.29 | .19–.44 | 1.00 | 26 | 102 | 0.25 | .17–.37 | 1.00 | ||||
| 24–29 | 13 | 26 | 0.50 | .29–.86 | 2.28 | 1.10–4.72 | 13 | 44 | 0.30 | .17–.51 | 1.19 | .60–2.33 | ||
| ≥30 | 20 | 49 | 0.41 | .26–.63 | 1.77 | .93–3.38 | 20 | 54 | 0.37 | .24–.57 | 1.47 | .81–2.67 | ||
| Ethnicity | .34 | .24 | ||||||||||||
| Dutch | 25 | 76 | 0.33 | .22–.49 | 1.00 | 27 | 77 | 0.35 | .24–.51 | 1.00 | ||||
| Non-Dutch | 31 | 78 | 0.40 | .28–.57 | 1.30 | .76–2.23 | 32 | 123 | 0.26 | .18–.37 | 0.73 | .43–1.23 | ||
| Sexual risk group | .02 | .05 | ||||||||||||
| MSM | 33 | 82 | 0.40 | .29–.57 | 1.00 | 33 | 84 | 0.39 | .28–.55 | 1.00 | ||||
| Heterosexual male | 5 | 7 | 0.71 | .30–1.72 | 2.47 | .93–6.50 | 6 | 35 | 0.17 | .08–.38 | 0.35 | .12–1.03 | ||
| Female | 18 | 65 | 0.28 | .17–.44 | 0.56 | .31–1.04 | 20 | 81 | 0.25 | .16–.38 | 0.61 | .34–1.07 | ||
| HIV | .45 | .26 | ||||||||||||
| Negative | 45 | 127 | 0.35 | .26–.47 | 1.00 | 48 | 173 | 0.28 | .21–.37 | 1.00 | ||||
| Positive | 11 | 27 | 0.41 | .23–.74 | 1.31 | .66–2.58 | 11 | 27 | 0.41 | .23–.74 | 1.50 | .77–2.94 | ||
| Anatomical site | .09 | .004 | ||||||||||||
| Rectum | 21 | 51 | 0.41 | .27–.63 | 1.00 | 20 | 36 | 0.56 | .36–.86 | 1.00 | ||||
| Urethra | 17 | 38 | 0.45 | .28–.72 | 1.13 | .60–2.16 | 19 | 83 | 0.23 | .15–.36 | 0.33 | .16–.67 | ||
| Endocervix | 18 | 65 | 0.28 | .17–.44 | 0.56 | .29–1.07 | 20 | 81 | 0.25 | .16–.38 | 0.36 | .18–.72 | ||
| Chlamydia trachomatis coinfection | .43 | .22 | ||||||||||||
| No | 35 | 91 | 0.38 | .28–.54 | 1.00 | 37 | 110 | 0.34 | .24–.46 | 1.00 | ||||
| Yes | 21 | 63 | 0.33 | .22–.51 | 0.80 | .46–1.39 | 22 | 90 | 0.24 | .16–.37 | 0.72 | .41–1.24 | ||
| Symptoms or signsa,b | .72 | .12 | ||||||||||||
| No | 23 | 61 | 0.38 | .25–.57 | 1.00 | 24 | 64 | 0.38 | .25–.56 | 1.00 | ||||
| Yes | 33 | 93 | 0.35 | .25–.50 | 0.90 | .53–1.55 | 35 | 136 | 0.26 | .18–.36 | 0.65 | .38–1.12 | ||
| Time to inclusion | .36 | .37 | ||||||||||||
| 0 d | 22 | 53 | 0.42 | .27–.63 | 1.00 | 24 | 92 | 0.26 | .17–.39 | 1.00 | ||||
| ≥1 d | 34 | 101 | 0.34 | .24–.47 | 0.77 | .45–1.34 | 35 | 108 | 0.32 | .23–.45 | 1.28 | .74–2.20 | ||
| Ceftriaxone MIC, mg/Lc | .75 | .22 | ||||||||||||
| ≤0.016 | 37 | 103 | 0.34 | .26–.50 | 1.00 | 40 | 155 | 0.26 | .19–.35 | 1.00 | ||||
| >0.016 | 9 | 27 | 0.33 | .17–.64 | 0.89 | .43–1.85 | 9 | 21 | 0.43 | .22–.82 | 1.64 | .77–3.49 | ||
| Azithromycin MIC, mg/Ld | .72 | .17 | ||||||||||||
| ≤0.25 | 34 | 101 | 0.34 | .24–.47 | 1.00 | 37 | 149 | 0.25 | .18–.34 | 1.00 | ||||
| 0.25–0.5 | 10 | 25 | 0.40 | .22–.74 | 1.29 | .62–2.65 | 10 | 24 | 0.42 | .22–.77 | 1.75 | .84–3.64 | ||
| >0.5 | 2 | 4 | 0.50 | .13–2.00 | 1.54 | .36–6.62 | 2 | 3 | 0.67 | .17–2.67 | 3.18 | .74–13.75 | ||
| Doxycycline MIC, mg/Le | .68 | .25 | ||||||||||||
| ≤0.5 | 9 | 30 | 0.30 | .16–.58 | 1.00 | 11 | 57 | 0.19 | .11–.35 | 1.00 | ||||
| 0.5–1.0 | 16 | 39 | 0.41 | .25–.67 | 1.40 | .61–3.20 | 17 | 52 | 0.33 | .20–.53 | 1.80 | .81–3.98 | ||
| >1.0 | 21 | 61 | 0.34 | .22–.53 | 1.10 | .50–2.46 | 21 | 67 | 0.31 | .20–.48 | 1.77 | .82–3.80 | ||
| Treatment at inclusion | .62 | .03 | ||||||||||||
| Ceftriaxone monotherapy | 21 | 57 | 0.37 | .24–.57 | 1.00 | 21 | 67 | 0.31 | .20–.48 | 1.00 | ||||
| Ceftriaxone + azithromycin | 23 | 69 | 0.33 | .22–.50 | 0.82 | .45–1.49 | 26 | 112 | 0.23 | .16–.34 | 0.71 | .39–1.28 | ||
| Ceftriaxone + doxycycline | 12 | 28 | 0.43 | .24–.75 | 1.14 | .56–2.33 | 12 | 21 | 0.57 | .32–1.01 | 2.01 | .94–4.30 | ||
| . | Clearance of RNA (n = 56) . | Clearance of DNA (n = 59) . | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Characteristic . | No. . | PD . | CR . | 95% CI . | HR . | 95% CI . | P Value . | No. . | PD . | CR . | 95% CI . | HR . | 95% CI . | P Value . |
| Sex | .03 | .25 | ||||||||||||
| Male | 38 | 89 | 0.43 | .31–.59 | 1.00 | 39 | 119 | 0.33 | .24–.45 | 1.00 | ||||
| Female | 18 | 65 | 0.28 | .17–.44 | 0.53 | .29–.96 | 20 | 81 | 0.25 | .16–.38 | 0.73 | .42–1.26 | ||
| Age, y | .06 | .45 | ||||||||||||
| ≤23 | 23 | 79 | 0.29 | .19–.44 | 1.00 | 26 | 102 | 0.25 | .17–.37 | 1.00 | ||||
| 24–29 | 13 | 26 | 0.50 | .29–.86 | 2.28 | 1.10–4.72 | 13 | 44 | 0.30 | .17–.51 | 1.19 | .60–2.33 | ||
| ≥30 | 20 | 49 | 0.41 | .26–.63 | 1.77 | .93–3.38 | 20 | 54 | 0.37 | .24–.57 | 1.47 | .81–2.67 | ||
| Ethnicity | .34 | .24 | ||||||||||||
| Dutch | 25 | 76 | 0.33 | .22–.49 | 1.00 | 27 | 77 | 0.35 | .24–.51 | 1.00 | ||||
| Non-Dutch | 31 | 78 | 0.40 | .28–.57 | 1.30 | .76–2.23 | 32 | 123 | 0.26 | .18–.37 | 0.73 | .43–1.23 | ||
| Sexual risk group | .02 | .05 | ||||||||||||
| MSM | 33 | 82 | 0.40 | .29–.57 | 1.00 | 33 | 84 | 0.39 | .28–.55 | 1.00 | ||||
| Heterosexual male | 5 | 7 | 0.71 | .30–1.72 | 2.47 | .93–6.50 | 6 | 35 | 0.17 | .08–.38 | 0.35 | .12–1.03 | ||
| Female | 18 | 65 | 0.28 | .17–.44 | 0.56 | .31–1.04 | 20 | 81 | 0.25 | .16–.38 | 0.61 | .34–1.07 | ||
| HIV | .45 | .26 | ||||||||||||
| Negative | 45 | 127 | 0.35 | .26–.47 | 1.00 | 48 | 173 | 0.28 | .21–.37 | 1.00 | ||||
| Positive | 11 | 27 | 0.41 | .23–.74 | 1.31 | .66–2.58 | 11 | 27 | 0.41 | .23–.74 | 1.50 | .77–2.94 | ||
| Anatomical site | .09 | .004 | ||||||||||||
| Rectum | 21 | 51 | 0.41 | .27–.63 | 1.00 | 20 | 36 | 0.56 | .36–.86 | 1.00 | ||||
| Urethra | 17 | 38 | 0.45 | .28–.72 | 1.13 | .60–2.16 | 19 | 83 | 0.23 | .15–.36 | 0.33 | .16–.67 | ||
| Endocervix | 18 | 65 | 0.28 | .17–.44 | 0.56 | .29–1.07 | 20 | 81 | 0.25 | .16–.38 | 0.36 | .18–.72 | ||
| Chlamydia trachomatis coinfection | .43 | .22 | ||||||||||||
| No | 35 | 91 | 0.38 | .28–.54 | 1.00 | 37 | 110 | 0.34 | .24–.46 | 1.00 | ||||
| Yes | 21 | 63 | 0.33 | .22–.51 | 0.80 | .46–1.39 | 22 | 90 | 0.24 | .16–.37 | 0.72 | .41–1.24 | ||
| Symptoms or signsa,b | .72 | .12 | ||||||||||||
| No | 23 | 61 | 0.38 | .25–.57 | 1.00 | 24 | 64 | 0.38 | .25–.56 | 1.00 | ||||
| Yes | 33 | 93 | 0.35 | .25–.50 | 0.90 | .53–1.55 | 35 | 136 | 0.26 | .18–.36 | 0.65 | .38–1.12 | ||
| Time to inclusion | .36 | .37 | ||||||||||||
| 0 d | 22 | 53 | 0.42 | .27–.63 | 1.00 | 24 | 92 | 0.26 | .17–.39 | 1.00 | ||||
| ≥1 d | 34 | 101 | 0.34 | .24–.47 | 0.77 | .45–1.34 | 35 | 108 | 0.32 | .23–.45 | 1.28 | .74–2.20 | ||
| Ceftriaxone MIC, mg/Lc | .75 | .22 | ||||||||||||
| ≤0.016 | 37 | 103 | 0.34 | .26–.50 | 1.00 | 40 | 155 | 0.26 | .19–.35 | 1.00 | ||||
| >0.016 | 9 | 27 | 0.33 | .17–.64 | 0.89 | .43–1.85 | 9 | 21 | 0.43 | .22–.82 | 1.64 | .77–3.49 | ||
| Azithromycin MIC, mg/Ld | .72 | .17 | ||||||||||||
| ≤0.25 | 34 | 101 | 0.34 | .24–.47 | 1.00 | 37 | 149 | 0.25 | .18–.34 | 1.00 | ||||
| 0.25–0.5 | 10 | 25 | 0.40 | .22–.74 | 1.29 | .62–2.65 | 10 | 24 | 0.42 | .22–.77 | 1.75 | .84–3.64 | ||
| >0.5 | 2 | 4 | 0.50 | .13–2.00 | 1.54 | .36–6.62 | 2 | 3 | 0.67 | .17–2.67 | 3.18 | .74–13.75 | ||
| Doxycycline MIC, mg/Le | .68 | .25 | ||||||||||||
| ≤0.5 | 9 | 30 | 0.30 | .16–.58 | 1.00 | 11 | 57 | 0.19 | .11–.35 | 1.00 | ||||
| 0.5–1.0 | 16 | 39 | 0.41 | .25–.67 | 1.40 | .61–3.20 | 17 | 52 | 0.33 | .20–.53 | 1.80 | .81–3.98 | ||
| >1.0 | 21 | 61 | 0.34 | .22–.53 | 1.10 | .50–2.46 | 21 | 67 | 0.31 | .20–.48 | 1.77 | .82–3.80 | ||
| Treatment at inclusion | .62 | .03 | ||||||||||||
| Ceftriaxone monotherapy | 21 | 57 | 0.37 | .24–.57 | 1.00 | 21 | 67 | 0.31 | .20–.48 | 1.00 | ||||
| Ceftriaxone + azithromycin | 23 | 69 | 0.33 | .22–.50 | 0.82 | .45–1.49 | 26 | 112 | 0.23 | .16–.34 | 0.71 | .39–1.28 | ||
| Ceftriaxone + doxycycline | 12 | 28 | 0.43 | .24–.75 | 1.14 | .56–2.33 | 12 | 21 | 0.57 | .32–1.01 | 2.01 | .94–4.30 | ||
Abbreviations: CI, confidence interval; CR, clearance rate per days of observation; HIV, human immunodeficiency virus; HR, hazard ratio; MIC, minimal inhibitory concentration; MSM, men who have sex with men; PD, person-days of follow-up.
a Symptoms included discharge, itch, burning, frequent or painful urination, bleeding, abdominal pain, pain during sex, anal cramps or pain, and changed defecation.
b Signs included red urethra, discharge, bleeding, fragile mucosa, swelling, or anal ulcerations.
c Cutoff based on European Committee on Antimicrobial Susceptibility Testing (EUCAST) epidemiological cutoff.
d Based on EUCAST breakpoints.
e Based on EUCAST breakpoints for tetracycline.
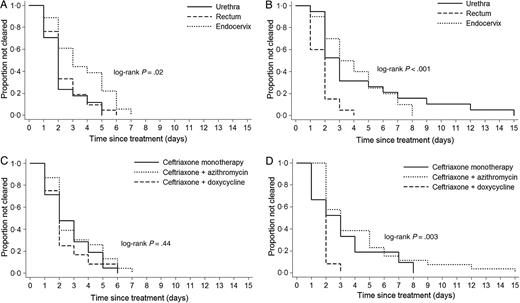
Time to clearance of Neisseria gonorrhoeae RNA (left column: A and C) and DNA (right column: B and D), by anatomical site (top row) and treatment (bottom row). The differences between groups were analyzed using the log-rank test.
Blips After Clearance of N. gonorrhoeae RNA
Six patients experienced 11 blips (Table 2). Three of them reported sexual contact after clearance (Supplementary Figure 2A), of whom 1 reported unprotected sex. RLU values of blips positive for N. gonorrhoeae only were significantly lower (mean, 220.6 RLUs [range, 91–463]) compared with pretreatment samples (mean, 1226.2 RLUs [range, 567–1350]; P = .0001). Results were identical when using the alternative definition of clearance (data not shown).
Predictors of blips were determined using 1308 samples at risk from 61 patients (Supplementary Table 1). The median number of days at risk was 24 (range, 4–25). The overall risk of finding a blip after clearance was 0.8%. No blips were observed within 48 hours of reported sex or rectal/vaginal douching. We found a significant univariable association between blips and coinfection with C. trachomatis (odds ratio [OR], 16.26 [95% CI, 1.42–186.37]) and dual treatment with doxycycline (OR, 8.20 [95% CI, 1.39–48.47]). These variables were highly correlated and multivariable analysis was not possible.
Clearance of N. gonorrhoeae DNA
One patient was excluded due to a negative pretreatment DNA result for N. gonorrhoeae. No patients experienced a treatment failure, and 1 patient experienced a reinfection (same patient as in the RNA analysis, day 13 Ct value, 31.6). For 59 patients (97%), we could determine the exact day of clearance (Table 2). The median time to clearance was 2 days (range, 1–15 days). After 9 days, 95% of patients had cleared DNA (Figure 1B); by anatomical site, this was reached after 15 days (urethra), 4 days (rectum), and 8 days (endocervix). With the alternative definition of clearance, the median time to clearance was identical, but the range was narrower (1–9 days), and 95% cleared after 8 days.
Determinants of Time to Clearance of N. gonorrhoeae DNA
Univariable Cox regression analysis showed a significant association with anatomical location (P = .004) and treatment (P = .03) (Table 3). Clearance rate was slower in endocervical and urethral infections compared with rectal infections (HRs, 0.36 [95% CI, .18–.72] and 0.33 [95% CI, .16–.67], respectively). This was also seen in Kaplan–Meier curves and log-rank testing (Figure 2B). Patients receiving dual therapy with azithromycin had a slower clearance rate (HR, 0.71 [95% CI, .39–1.28]), whereas those receiving dual therapy with doxycycline had a faster clearance rate compared with ceftriaxone monotherapy (HR, 2.01 [95% CI, .94–4.30]). Because of nonoverlap or almost 100% overlap in categories of anatomical site and treatment, including these variables in the same multivariable model was not possible.
Blips After Clearance of N. gonorrhoeae DNA
Ten patients experienced 19 blips (median per patient, 1.5 [range, 1–5]; Table 2). Seven of them reported sexual contact after clearance (Supplementary Figure 2B), of whom 4 reported unprotected sex. Blips had significantly higher Ct values (mean, 37.9 [range, 35.4–39.5]) compared to pretreatment samples (mean, 28.5 [range, 23.5–37.9]; P = .0001). When using the alternative definition of clearance, 15 patients had 29 blips (mean Ct value, 37.9).
Predictors of blips were determined using 1285 samples at risk from 61 patients (Supplementary Table 1). The median number of days at risk was 24 (range, 4–25). The risk of finding a blip after clearance was 1.5%. Four blips were observed within 48 hours of reported sexual contact, but the association was not statistically significant.
DISCUSSION
We assessed the appropriate timing of TOC for N. gonorrhoeae using modern-type RNA- and DNA-based NAATs. The median time to clearance was 2 days when using either NAAT. Clearance rates of 95% were reached after 6 and 9 days, respectively. Time to clearance was associated with sexual risk group, anatomical site, and treatment in unadjusted analysis. Because of multicollinearity, we could not use multivariable analysis to identify the most important correlate of time to clearance. We therefore cannot be sure which treatment regimen results in the fastest clearance.
Few previous studies reported time to clearance of N. gonorrhoeae using molecular tests [15–18]. A strength of the current study is the testing on 28 consecutive days. The only previous study evaluating results on consecutive days described the dynamics of DNA clearance in 130 patients using ligase chain reaction, which has not been available for many years [15]. The median time to clearance was 1 day (men) and 2 days (women) in 21 days of follow-up. This is similar to our results with a median of 2 days for both RNA and DNA. Another strength of the current study is the use of modern commercially available NAATs. The only study using a modern NAAT described RNA clearance after 21 days, using the Aptima Combo 2 assay in 194 MSM [17]. Clearance was 100% for urethral and 92% for rectal samples. The latter is lower compared to our results (100% clearance after 7 days). The 10 positive samples might represent reinfections or blips, which could explain the lower clearance [17]. Hjelmevoll et al reported 84% DNA clearance after 7 days and 100% after 14 days, using an in-house porA pseudogene PCR in 29 patients [16]. Bissessor et al reported 92% DNA clearance after 14 days, using 2 PCRs targeting the porA and opa genes in 190 MSM [18]. Our study has further detailed the clearance of both RNA and DNA using modern NAATs.
Bachmann et al previously described intermittent shedding of DNA after clearance in 18% of their population [15]. In our study, 10% of patients had RNA blips and 16% had DNA blips. However, the overall risk of finding a blip in all samples at risk was only 0.8% and 1.5%, respectively. In addition, only 1 patient experienced a total of 4 blips in both RNA and DNA on the same day. Some blips could represent a test artefact, which is suggested by the stronger univariable association of blips and C. trachomatis coinfection in RNA compared with DNA blips. Differentiation between N. gonorrhoeae and C. trachomatis RNA in the Aptima Combo 2 assay only depends on the kinetic zone and is therefore possibly more difficult than in the DNA assay. Ongoing subclinical infection appears unlikely as we showed that blips were preceded by at least 3 negative samples. More likely would be deposition of genetic material by a sex partner. However, we found no significant association between blips and sexual contact in the 48 hours before sampling. Finally, blips could be caused by the release of genetic material from degrading epithelial or submucosal cells or biofilm [21].
Our study has potential limitations. As a single-center study with a high-risk population, our results might not be generalizable to other settings. We did not include pharyngeal infections, as self-collection was deemed too challenging for participants. Because of multicollinearity, multivariable analysis of associations with clearance or blips was not possible. Last, as a positive NAAT result gives no information about viability of the microorganism, there is no corroborated definition of clearance. When a more lenient definition was used, time to clearance was shorter, but more blips were observed.
Future research should include pharyngeal infections and focus on a combined timing of TOC for gonorrhoea and chlamydia, and the interpretation of positive NAAT results, preferably with higher power to detect associations with clearance and blips.
In conclusion, if indicated, we recommend performing a TOC for anogenital gonorrhoea at least 7 or 14 days after administering therapy, when using modern-type RNA- or DNA-based NAATs, respectively. When interpreting TOC results for possible treatment failures, both the occurrence of blips and a possible reinfection need to be taken into account. The risk of finding a blip was around 1%, and the difference of RLU or Ct values in pretreatment samples and blips was significant. Therefore, a low-positive TOC result could indicate a blip. If a blip cannot be excluded, we recommend obtaining a new sample for retesting.
Notes
Acknowledgments. We are grateful to all participants. We thank Myra van Leeuwen, Claudia Owusu, and Princella Felipa for their help in recruiting the participants. We thank Fred Zethof for performing the Aptima Combo 2 assays, Davy Janssen for performing the Cobas 4800 assays, and Paul Smits for performing the Abbott NG/CT assays. Statistician Nan van Geloven advised on the sample size calculations.
Financial support. This work was supported by the Public Health Service Amsterdam. Hologic provided Aptima test materials and kits in-kind. Roche provided Cobas test materials and kits in-kind.
Potential conflicts of interest. All authors: No potential conflicts of interest. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References




