-
PDF
- Split View
-
Views
-
Cite
Cite
Bart Lutters, Peter J Koehler, Cerebral pneumography and the 20th century localization of brain tumours, Brain, Volume 141, Issue 3, March 2018, Pages 927–933, https://doi.org/10.1093/brain/awy031
Close - Share Icon Share
Introduction
In 1918, the American neurosurgeon Walter Dandy (1886–1946) first described the injection of air into the cerebral ventricles as an aid to clinical diagnostics (Dandy, 1918). By revealing alterations in the shape, size or position of the ventricles on the radiogram, ventriculography provided a valuable tool to indirectly predict the presence and localization of brain tumours. The following year, Dandy introduced a method for the ‘intraspinous’ injection of air, pneumoencephalography, which allowed for the radiological visualization of tumour-induced changes of both the ventricular system and the cerebral subarachnoid space (Dandy, 1919). With the invention of ventriculography and pneumoencephalography—jointly referred to as cerebral pneumography—Dandy laid the groundwork for subsequent methods to directly or indirectly visualize lesions of the CNS with radiopaque substances, including contrast myelography, arterial encephalography and isotope encephalography (Moniz, 1927; Moore, 1948). The value of cerebral pneumography was, however, not undisputed, as the technique was not devoid of danger and often challenging to interpret. Hence, there was a feeling that to depend on radiography was to renounce oneself as a neurologist, by exposing patients to dangerous procedures, while thorough clinical examination performed by a skilful neurologist, would, in many cases, be sufficient for the diagnosis and localization of brain tumours. In this article, we wish to celebrate the centenary of Walter Dandy’s inventions of ventriculography and pneumoencephalography, procedures that, despite their dangers and shortcomings, significantly contributed to the diagnosis and localization of brain tumours during the 20th century.
The age of cerebral localization
Prior to the introduction of ventriculography, the diagnosis and localization of brain tumours depended almost entirely on patient history and neurological examination. During the second half of the 19th century, the discovery of the (left) frontal speech centre by Paul Broca (1824–80) and the excitability of the cerebral cortex by Gustav Fritsch (1838–1927) and Eduard Hitzig (1838–1907) had inaugurated the age of cerebral localization, while the introduction of antiseptic surgery by Joseph Lister (1827–1912) and advances in anaesthesiology had paved the way for the development of neurological surgery, providing an incentive for the earlier diagnosis and localization of brain tumours. By the beginning of 20th century, the diagnosis of brain tumours consisted of two subsequent steps. First, the general diagnosis of a brain tumour was to be made, mostly based on signs of increased intracranial pressure, such as headache, nausea, and papilledema. After the general diagnosis had been made, the next step was to make a local diagnosis, based on localizing signs such as unilateral sensorimotor disturbances, visual field defects and language disturbances (Redlich, 1912).
During this period, meticulous neurological examination was estimated by some to provide accurate tumour localization in 75% of cases, still leaving a considerable percentage of brain tumours that could not be localized by clinical means (Redlich, 1912). In these cases, skull radiography—pioneered by the Austrian neuropsychiatrist Arthur Schüller (1874–1957) in his 1912 monograph Röntgen-diagnostik der Erkankungen des Kopfes—provided a modest aid to clinical diagnostics. By visualizing tumour-induced cranial and intracranial changes, such as destruction of the sella turcica in case of pituitary tumours and focal skull erosion in hemispheric tumours, indirect cues could be gained regarding the presence and localization of brain tumours; direct signs of brain tumour were only present in cases of tumour calcification. Moreover, several authors were already experimenting with the introduction of air into the cerebral ventricles and subarachnoid space—Schüller supposedly attempted to inject air into dog ventricles for radiographic purposes just a few years after the invention of X-ray by Wilhelm Röntgen (1845–1923) in 1895 and the American neurologist Edward Affleck Sharp sought to resolve subarachnoid adhesions in acute meningitis by producing an ‘artificial pneumorachis’ through lumbar injections of oxygen—and several cases of head trauma were reported, in which air had entered the cerebral ventricles through fractures of the skull, allowing for radiographic visualization of the ventricular system (Guttmann, 1936).
The invention of air contrast
In 1916, Walter Dandy—who was just finishing his surgical training at Johns Hopkins University—and his senior colleague George Heuer (1882–1950) published two consecutive articles on the value of skull radiography in the localization of brain tumours, demonstrating that only in about 45% of the cases the radiographs provided valuable diagnostic cues (Dandy, 1918). As a result of inaccurate diagnostics and localization, tumours could often not be found upon surgical exploration. Dandy clearly recognized the need for a faster and more accurate way to diagnose and localize brain tumours, which would save patients from the horror of undergoing a useless and dangerous operation under local anaesthesia, and would naturally improve the surgical results and patient outcome:
‘The crux of the whole matter is that no brain tumor can be cured without operative removal; and that the earlier the diagnosis and localization is made the better the chances for a cure. The future outlook in the treatment of brain tumors is dependent almost entirely upon early recognition and localization of the tumor’ (Dandy, 1920).
For some time, Dandy had considered introducing a contrast agent into the cerebral ventricles, hoping that it would allow for the detection of cerebral tumours by visualizing tumour-induced alterations in the shape and size of the lateral ventricles. For this purpose, he had injected various substances into the ventricles of experimental animals (dogs)—including thorium, potassium iodide and other solutions then used in pyelography—all with fatal results (Dandy, 1918). Largely inspired by the remarkable gas shadows outlining the stomach and intestines in abdominal radiograms and the observation that brain tumours invading the paranasal sinuses could be detected by skull radiography due to the displacement of the normally contained air, Dandy eventually conceived of injecting air into the cerebral ventricles, a technique referred to as pneumoventriculography or simply ventriculography (Dandy, 1918).
The procedure consisted of performing a ventricular puncture through a burr hole in the skull (in young children through the anterior fontanel). CSF was then withdrawn from the ventricles, using a record syringe with a two-way valve attachment, allowing for the introduction of an equal amount or air. This process was continued as long as CSF could be readily obtained, a maximum amount of CSF being replaced by air while the patient was lying face-down with the head slightly rotated and the puncture was made in the anterior part of the lowermost lateral ventricle (Fig. 1) (Dandy, 1918). Radiograms were then obtained in lateral and anteroposterior directions with the patient being verticalized; by manipulating the head in such a way that the air would displace to either one of the ventricles, it was possible to visualize each lateral ventricle separately (Dandy, 1920).
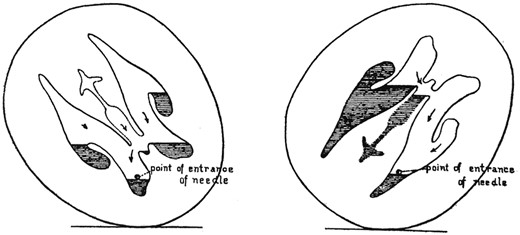
Diagram showing the positions of the head for optimal withdrawal of CSF from a single ventricular puncture. From Dandy (1918).
For his first study on ventriculography, Dandy injected air into the cerebral ventricles of several children (6 months to 12 years of age) clinically suspected of internal hydrocephalus. In these cases, ventriculography proved to be of tremendous value, providing an absolute diagnosis by direct visualization of the enlarged ventricular system. He then moved on to investigate the value of ventriculography in diagnosis and localization of brain tumours in a series of over 75 paediatric and adult patients (Dandy, 1920). As Dandy had predicted, many suspected tumours of the cerebral hemispheres could readily be demonstrated by ventriculography, based on alterations in the shape, size and position of the lateral ventricles (Fig. 2). Alternatively, bilateral enlargement of the lateral ventricles was indicative of hydrocephalus, making the presence of a cerebellar tumour more likely.
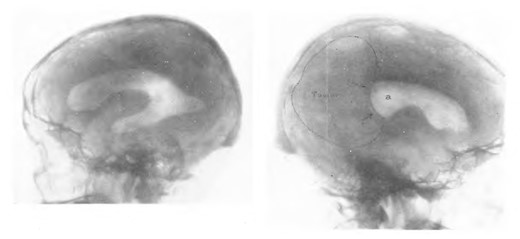
Ventriculogram showing a relatively unaffected right lateral ventricle (left) and a left lateral ventricle (right) in which the posterior horn has been compressed by a tumour. From Dandy (1920).
During his work with ventriculography, Dandy noticed that, in some cases, the air injected into the cerebral ventricles would pass from the ventricular system into the subarachnoid space, outlining the subarachnoid cisterns and cerebral sulci on the radiogram (Fig. 3) (Dandy, 1919). Dandy realized the diagnostic potential of introducing subarachnoid air contrast, conceiving that many tumours would directly or indirectly affect the subarachnoid space. For this purpose, he started injecting air into the lumbar spinal canal, which, with the patients in supine or upright position, would quickly pass to the cerebral subarachnoid space. The air would frequently enter the cerebral ventricles as well, allowing for the radiological visualization of both the ventricular and the subarachnoid system. Similar to ventriculography, CSF was gradually withdrawn and replaced by an equal amount of air to minimize intracranial pressure changes. In Dandy’s initial series, alterations of the subarachnoid space were found in three of eight patients, in one case enabling the localization of a midbrain tumour due to obstruction of the pontine cistern (Dandy, 1919). For Dandy, this clearly indicated the practical value of lumbar intraspinous air injections, whether or not in combination with ventriculography:
‘As a matter of fact, we shall often be able to localize a tumor from either a ventriculogram or from an X-ray of the subarachnoid space alone, an analysis of the signs and symptoms of the individual case enabling us to determine which should be tried first. From the data obtainable from the combination of intraventricular and intraspinous injections it is difficult to see how intracranial tumors can escape localization’ (Dandy, 1919).

Ventriculogram in which the air has passed from the ventricular system into the subarachnoid system, outlining the subarachnoid cisterns and cerebral sulci. From Dandy (1919).
Initial doubts: the dangers of cerebral pneumography
Dandy’s intraventricular and intraspinous air injections were not readily accepted among the neurological community. In North America, eminent neurosurgeons such as Harvey Cushing (1869–1939), Charles Frazier (1870–1936) and the young Wilder Penfield (1891–1976) feared the complications associated with the procedure—including convulsions, infections, bradycardia, apnoea and death—which they regarded frequent enough to consider their use contraindicated when a diagnosis could be made by other means. In Europe too, particularly in the UK, a nation with a strong tradition in clinical medicine and localization, there was a certain resilience against cerebral pneumography, and it was not until 1924 that its potential value was first discussed among the members of the section of neurology of the Royal Society of Medicine (Collier, 1924). By that time, German internist Adolf Bingel (1879–1953) had, independently from Dandy, discovered lumbar injections of air to detect tumour-induced alterations of the subarachnoid space on the radiogram, effectively introducing Dandy’s technique, which he named ‘pneumoencephalography’, in Europe (Guttmann, 1936). Moreover, the French physicians Jean-Athanase Sicard (1872–1929) and Jacques Forestier (1890–1978) had introduced contrast myelography—in which the radiopaque substance lipiodol was injected into the spine for the localization of spinal tumours—thereby drawing attention to the potential value of radiology in neurological diagnosis.
During the meeting of the Royal Society of Medicine, most participants expressed themselves positively of Sicard’s lipiodol injections, which were well tolerated by patients and allowed for more precise localization of spinal lesions (Collier, 1924). Ventriculography and pneumoencephalography were viewed less favourably; the procedures were considered far more dangerous than its pioneers had suggested, with some authors reporting a fairly high mortality rate. Sure enough, ventriculography could occasionally provide useful information in differentiating between brain tumours and other conditions presenting with increased intracranial pressure symptoms and in cases of unco-operative or blind patients inaccessible to neurological examination. But, as the eminent neurological surgeon Sir Geoffrey Jefferson (1886–1961) argued, a skilful clinician would certainly refrain from exposing his patients to risky procedures when a diagnosis could be provided by less invasive methods:
‘I am inclined to use the method sparingly; obviously, the better the neurologist the less the need for ventriculography. The upholders of the method have harmed their cause by claiming too much for it, and by publishing photographs of tumours which should have been localized easily enough by less dangerous means’ (Collier, 1924).
These concerns were shared by Portuguese neurologist Egas Moniz (1874–1955) and—in combination with the promising results of Sicard’s lipiodol injections—stimulated him to find an alternative (Moniz, 1927). Moniz came to the idea of injecting a radiopaque substance (initially strontium bromide, later sodium iodide) into the internal carotid arteries, potentially allowing for the localization of cerebral tumours by visualizing tumour-induced alterations in the cerebral arteries on the radiogram. After extensive experimentation on human cadavers, experimental animals and patients, Moniz eventually succeeded in radiologically visualizing the modified cerebral arteries of a 20-year-old patient with a pituitary tumour on the radiogram (Moniz, 1927). It is emblematic of Moniz’ objective to develop a novel diagnostic tool for the localization brain tumours, rather than for the detection of cerebral vascular abnormalities for which the procedure is still in use today, that he initially referred to his invention as ‘arterial encephalography’ rather than the currently used ‘cerebral arteriography’.
Careful optimism: the first International Neurological Congress
In 1931, the first International Neurological Congress was held in Berne, Switzerland, which was attended by some of the world’s most renowned neurologists and neurological surgeons and proved to be instrumental for the establishment of neurology as an independent specialty in medicine (Fig. 4). During the congress, there was a specific session devoted to brain tumours, with several contributions on the diagnostic value of skull radiography, ventriculography, pneumoencephalography and arterial encephalography. The attitude towards the use of radiography was considerably more positive, with participants recognizing that, in some cases, brain tumours could simply not be localized or even diagnosed by clinical means. Nevertheless, as the American neurosurgeon Ernest Sachs (1879–1958) emphasized, the interpretation of radiological results remained challenging, especially when they did not match the clinical findings. Sachs gave several examples related to the use of skull radiography—including a case in which radiological and clinical findings suggested a different tumour localization, and a case with abnormalities on the skull radiogram (for example convolutional atrophy) in the absence of objective neurological symptoms—stressing that in most of these cases the clinical findings should ultimately prevail (Brouwer et al., 1932).

Representatives of the various countries participating in the preparation of the first International Neurological Congress in Berne (1931). Identifiable participants: Max Nonne (front row; second from left), Charles Sherrington (front row; third from left), Bernard Sachs (front row; fourth from left), Robert Bing (back row; second from left), Otto Marburg (back row; third from left); Ottorino Rossi (back row; fourth from left), C.U. Ariëns Kappers (back row; fifth from left), George Guillain (back row; seventh from left) and Henry Alsop Riley (back row, second from right). From Henry Alsop Riley Papers, Archives and Special Collections, Columbia University.
Following Sachs, the renowned German neurologist and neurosurgeon Otfrid Foerster (1873–1941), his Breslau colleague Ludwig Guttmann (1899–1980) and the American neurosurgeon Francis Grant (1891–1967) discussed the value of cerebral pneumography. Foerster and Grant both emphasized the value of ventriculography in the diagnosis and localization of brain tumours, even though its use had to be restricted to cases in which clinical symptomatology alone could not provide a definite localization (because of the risk of sudden intracranial pressure changes and diffuse parenchymal bleeding). However, they strongly favoured ventriculography over pneumoencephalography in cases of suspected brain tumour, as in the presence of intracranial hypertension, the latter could result in herniation of the cerebellum into the foramen magnum:
‘In brain tumours, the dangers and downsides of lumbar air injections outweigh the benefits. Hence, I believe that the procedure should in principal not be used, and, if used at all, should only be resorted to when it can supplement the results obtained from ventriculography performed by means of ventricular puncture’ (Foerster in Brouwer et al., 1932).
Guttmann was more optimistic towards the use of pneumoencephalography in cases of suspected brain tumours; while recognizing the dangers associated with the procedure, he considered its use sufficiently safe in the presence of only mild increased intracranial pressure symptoms (e.g. isolated headache, nausea, mild papilloedema). Moreover, besides being much easier to perform, the procedure had the significant advantage of allowing for the radiological visualization of both the ventricular system and the subarachnoid space, thereby providing more diagnostic information than could be obtained from ventriculography. Interestingly, Guttmann considered pneumoencephalography not only useful in cases when clinical localization was inconclusive, but also in determining the exact site and extent of the tumour in the presence of focal neurological symptoms, and to monitor postoperative tumour recurrence, thereby indirectly propagating a more indiscriminate use of radiography in brain tumour patients (Guttmann, 1936).
In the decades following the first International Neurological congress, significant advances were made to the technique of pneumoencephalography, most notably by the American neurosurgeon Leo Davidoff (1898–1975) and neuroradiologist Cornelius Dyke (1900–43), who managed to carry out the entire procedure under carefully controlled conditions at the radiology department, thereby reducing the risks and discomfort associated with the procedure. This stimulated the increased use pneumoencephalography over subsequent decades, and while ventriculography remained to be used in case of severe intracranial hypertension, pneumoencephalography came to be regarded as the preferred method for the diagnosis and localization of brain tumours (Guttmann, 1936). Moreover, the combined use of cross-sectional imaging or tomography and cerebral pneumography—suggested by the Dutch neurologist Bernard Ziedses des Plantes (1902–93) during the first half of the 20th century and further refined during the 1960s—greatly improved the quality of the cerebral pneumogram by eliminating shadows resulting from overprojection. Tomography could either be accomplished by simultaneously moving the X-ray tube and film in various directions while the patient remained still, or by moving the patient while the tube and film remained still. The latter ultimately led to the invention of the ‘somersaulting chairs’ in the early 1960s, which rotated patients 360° around their horizontal axis (Amplatz, 1963). During this period, the development of transfemoral catheterization, image subtraction methods and film changers also improved the technique of arterial encephalography, which proved useful in the localization of brain tumours by revealing tumour-induced shifts in the cerebral arteries and predicting the presence of certain types of tumours based on their vascular pattern. In addition, various other diagnostic techniques, such as ultrasonography and electroencephalography, were used in the localization of brain tumours, but these applications never gained widespread acceptance.
New possibilities: the rise of modern brain imaging
In 1948, the American surgeon George Moore (1920–2008) revolutionized the field of neuroradiology by introducing the use of radioactive diiodofluorescein, thereby allowing for the direct visualization of brain tumours (Moore, 1948). Moore, still in his 20s, had accurately postulated that fluorescein—a substance known to be selectively taken up by certain eye tumours—would also be taken up by brain tumours. Inspired by the introduction of radioactive iodine in the diagnosis of thyroid disease, he then conceived of attaching a radioactive isotope to fluorescein. Following intravenous injection, this radioactive diiodofluorescein was selectively taken up by the brain tumour, from there emitting gamma rays that could subsequently be detected by means of a Geiger-Müller tube. Using this method, Moore was able to predict the presence of brain tumours with far more accuracy than could be achieved by clinical examination, revealing the presence of a tumour when clinical examination was suggestive of a different type of lesion (e.g. subdural haematoma) and vice versa (Moore, 1948). In addition, isotope encephalography was well tolerated by patients and involved relatively little risk; a significant advantage over cerebral pneumography. Nevertheless, it would take more than a decade before the method became established, as the initial optimism was tempered by subsequent studies yielding less promising results.
By the 1970s, according to the authoritative multivolume Handbook of Clinical Neurology, the use of radioactive contrast agents in the diagnosis and localization of brain tumours had become completely accepted (Mealey, 1974). Moreover, the procedure was routinely used in surgical planning and postoperative follow-up, illustrating its role as an accessible screening instrument in the diagnosis and management of brain tumours. Yet, the Handbook still contained chapters on skull radiography and pneumoencephalography, even though the author of the latter chapter admitted that its use had declined since the advent of isotope encephalography. Clearly, the introduction of the new imaging modality had dismissed the fundamental argument against the use of neuroradiology, namely, it being dangerous to patients. This came at the expense of clinical localization, which inevitably lost some practical significance in the diagnosis and localization of brain tumours. Interestingly, cerebral pneumography continued to be important to the field of stereotactic neurosurgery, as the human stereotaxic apparatus, devised by Ernest Spiegel (1895–1980) and Henry Wycis (1911–71) in 1947, made use of intracranial anatomical landmarks, some of which were visible on plain radiograms (calcified pineal glands), but also those that could only be visualized using air contrast (Spiegel et al., 1947).
The 1970s also witnessed the invention of the two most commonly used brain imaging modalities today: computed tomography (CT), invented by the computer engineer Godfrey Hounsfield (1919–2004) in 1971 (even though the South African physicist Allen Cormack had previously worked out the algorithm that provided the basis for CT independently), and MRI, which reached the clinic in the 1980s. Even though initial CT methods were relatively crude and results challenging to interpret, imaging modalities continued to improve during the late 20th and early 21st century, and have undoubtedly resulted in earlier tumour detection and improved patient outcome. With the increasing use of brain imaging, however, problems regarding the management of incidental brain findings are becoming more apparent, revolving around the dilemma whether or not to treat patients that do not display objective neurological symptoms. These concerns are not unlike issues raised during the first half of the 20th century, when the neurological community first became aware of the occasional disagreement between clinical and radiological findings, which still confronts neurologists and neurosurgeons today.
Conclusion
One century has passed since Walter Dandy invented the techniques of ventriculography and pneumoencephalography, which provided an invaluable aid to the 20th century diagnosis and localization of brain tumours. The procedures were, however, not readily accepted by the neurological community, which initially regarded them as dangerous and often unnecessary additions to clinical diagnostics. But as the procedures improved and the right indications were established, a more positive attitude emerged, even though cerebral pneumography remained mostly restricted to cases in which clinical examination could not provide a definite diagnosis. Cerebral pneumography also inspired the development of several valuable diagnostic procedures, including positive contrast myelography and arterial encephalography. During the second half of the 20th century, the development of novel imaging modalities allowed for the direct visualization of tumours without exposing patients dangerous procedures, resulting in a more indiscriminate use of radiology in the diagnosis and management of brain tumours. While this has led to earlier diagnosis and improved patient outcome, the occasional disagreement between clinical and radiological findings continues to pose a problem to modern neurologists.
Funding
No funding was received towards this work.


