-
PDF
- Split View
-
Views
-
Cite
Cite
Sami Sula, Timo Paananen, Ville Tammilehto, Saija Hurme, Anne Mattila, Tuomo Rantanen, Tero Rautio, Tarja Pinta, Suvi Sippola, Jussi M Haijanen, Paulina Salminen, Impact of an appendicolith and its characteristics on the severity of acute appendicitis, BJS Open, Volume 8, Issue 5, October 2024, zrae093, https://doi.org/10.1093/bjsopen/zrae093
Close - Share Icon Share
Abstract
Antibiotics have been reported as an efficient and safe treatment option for uncomplicated acute appendicitis without an appendicolith diagnosed using computed tomography (CT). The aim of this study was to assess the association of a CT-diagnosed appendicolith and its characteristics with appendicitis severity.
A large prospective patient cohort with suspected acute appendicitis enrolled between April 2017 and November 2018 was retrospectively reviewed. The initial analysis evaluated the association of a CT-diagnosed appendicolith with complicated acute appendicitis; then, based on the availability of CT images, a subset of patients was analysed for the correlation of appendicolith characteristics with appendicitis severity. The final appendicitis assessment (uncomplicated or complicated—including perforation, gangrene, an abscess, or a tumour) was determined for all patients.
Out of 3512 eligible patients, 3085 patients with appendicitis were selected and 380 patients with an appendicolith and with a CT image available for reassessment were included. Out of the 3085 patients with CT-diagnosed acute appendicitis, 1101 (35.7%) patients presented with both acute appendicitis and an appendicolith and, out of these, 519 (47.1%) had complicated acute appendicitis. In the patients without an appendicolith (1984 patients), 426 (21.5%) had complicated appendicitis (P < 0.001). Re-evaluation of CT images for 380 patients showed that a larger appendicolith diameter (OR = 1.15 (95% c.i. 1.06 to 1.25); P < 0.001), appendicolith location at the base of the appendix (55.1% versus 44.9%; P = 0.008), and heterogeneous appendiceal wall enhancement around the appendicolith (68.4% versus 31.6%; P < 0.001) were associated with an increased risk of complicated acute appendicitis.
The presence of an appendicolith in patients with acute appendicitis is correlated with the risk of complicated appendicitis. This risk is further increased by a larger appendicolith diameter or appendicolith location at the base of the appendix.
Introduction
Acute appendicitis is one of the most common reasons for emergency department visits and an appendectomy is one of the most common surgical procedures1. However, with the demonstrated feasibility of antibiotic treatment for computed tomography (CT)-diagnosed uncomplicated acute appendicitis, treatment alternatives for acute appendicitis have changed over recent years2–5. With the increasing number of treatment options, the emphasis of pre-interventional diagnostics has shifted from appendicitis confirmation towards differentiating between complicated and uncomplicated appendicitis.
CT is the ‘gold standard’ for acute appendicitis imaging and low-dose CT imaging has reached similar accuracy compared with standard CT imaging, with a significantly decreased radiation dosage6,7. In general, CT has high accuracy with regard to diagnosing appendicitis and, despite its somewhat limited capability to differentiate between uncomplicated and complicated appendicitis, it still has the best negative predictive value for complicated appendicitis compared with other diagnostic imaging modalities7–9.
The presence of an appendicolith in patients with acute appendicitis appears to be a clinically important finding, increasing the risk of failure of non-operative treatment of acute appendicitis and increasing the appendectomy rate5,10–17, suggesting that patients presenting with an appendicolith may not be optimal candidates for antibiotic therapy. In the recent large CODA trial5, assessing the antibiotic treatment of imaging-confirmed acute appendicitis, patients presenting with an appendicolith were found to have a significantly higher risk of appendectomy and complications than those without an appendicolith.
An appendicolith is a calcified faecal deposit in the lumen of an inflamed appendix, present in almost 40% of patients with CT-diagnosed acute appendicitis18, making appendicolith appendicitis the most common presentation of potentially complicated acute appendicitis. The presence of an appendicolith has been considered to drive appendicitis progression in complicated appendicitis demonstrated also at histopathology19–21. However, appendicoliths can also be incidental, clinically irrelevant, findings in asymptomatic patients without acute appendicitis22 and some patients with acute appendicitis and an appendicolith can be safely treated without an appendectomy5. Only a few studies have assessed the effect of appendicolith characteristics on appendicitis severity. In a paediatric study, an appendicolith maximum diameter of 5 mm or more was a significant risk factor for perforated acute appendicitis17. Another study showed that an appendicolith with a diameter of more than 5 mm and an appendicolith with a location at the base of the appendix were associated with gangrenous appendicitis23. A recent study suggested that patients with acute appendicitis presenting with an appendicolith with a diameter of under 5 mm and patients with a low C-reactive protein (CRP) concentration could be treated conservatively, whereas an appendicolith diameter of over 10 mm indicates a high risk of appendiceal perforation, but no conclusions were drawn for the large group of patients with an appendicolith diameter of between 5 and 10 mm24.
However, as all appendicitis cases presenting with an intraluminal appendicolith do not progress to complicated acute appendicitis5, there is a knowledge gap with regard to understanding which appendicolith features are most strongly associated with the failure of antibiotic treatment and increased complications of appendicitis. The aim of this observational study was to investigate the impact of an appendicolith and its characteristics on the severity of appendicitis using the large prospective patient cohort initially assessed for enrolment in the APPAC II2 and APPAC III25 randomized clinical trials (RCTs), both assessing the optimization of non-operative treatment of uncomplicated acute appendicitis. The primary aim was to assess objective CT characteristics of the appendicoliths and their association with appendicitis severity to improve clinical decision-making in patients with acute appendicitis presenting with an appendicolith.
Methods
Study design
This study was a retrospective subgroup analysis of the prospectively collected patient data of patients evaluated for enrolment in two concurrent multicentre RCTs2,25, evaluating non-operative treatment for acute appendicitis (APPAC II2 NCT03236961 and APPAC III25 NCT03234296). The trial protocol for the RCTs, including this substudy, was approved by the ethics committee of the Hospital District of Southwest Finland, and all patients in the main analysis for appendicolith features gave written informed consent; data for the initial analysis of patients were collected only for evaluation for enrolment in the RCTs.
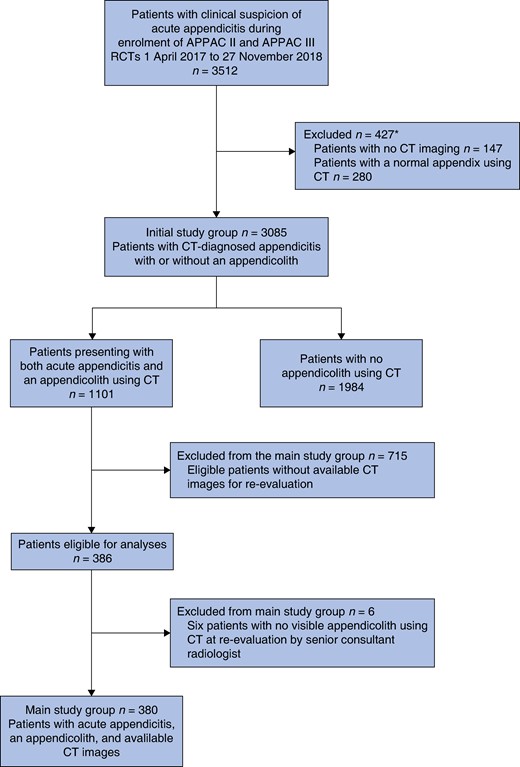
The medical records of all patients evaluated for eligibility in the APPAC II and APPAC III RCTs with suspected acute appendicitis were evaluated for this substudy (Fig. 1). The entire population of patients with appendicitis was first divided into two categories based on the initial CT diagnosis: patients with appendicitis and an appendicolith and patients with appendicitis with no appendicolith. In the initial analysis, the final clinical diagnoses of these two cohorts were assessed and compared to evaluate the overall association of a CT-diagnosed appendicolith with complicated appendicitis among these two patient groups with imaging-diagnosed appendicitis. After patients with an appendicolith using imaging were shown to have a higher risk of complicated appendicitis, more detailed analyses regarding the characteristics of the appendicoliths were performed. The main analysis included all patients with an appendicolith and with an original CT image available, and who gave written informed consent. CT images for these patients were reassessed by one of two abdominal radiologists subspecialized in emergency radiology, with more than 10 years of experience with regard to evaluating appendicolith diameter, appendicolith location, the potential pressure effect of an appendicolith, and possible heterogeneous appendiceal wall enhancement around an appendicolith. Regarding the patients at Turku University Hospital, the maximum diameter was measured using a Philips Carestream PACS MPR (multiplanar reconstruction) tool from venous phase CT images. For patients from other hospitals (Table S1), the maximum diameter was calculated according to the most optimal CT plane available. The association of the CT appendicolith characteristics with the final clinical diagnosis of appendicitis severity, that is complicated or uncomplicated acute appendicitis, was evaluated.
Outcome of interest
The aim of this study was to evaluate the association of an appendicolith and its characteristics with the incidence of complicated acute appendicitis. The primary variables were the diameter and location of the appendicolith. For appendicolith diameter, the aim was to determine a cut-off value potentially predicting a more complicated course of acute appendicitis. As such a cut-off value could not be determined, it was decided to divide the appendicoliths into three diameter categories based on clinical assessment potentially assisting in clinical decision-making. Secondary variables included appendicolith length, the potential pressure effect of an appendicolith on the appendiceal wall (defined as an appendicolith having a wedged appearance; blocking the appendiceal lumen and causing distal stasis), appendiceal diameter, and possible heterogeneous appendiceal wall enhancement around an appendicolith as a potential precursor to perforation. Appendicolith location was classified according to the following four categories (based on the approximate assessment of the radiologist after longitudinal division of the appendix into three parts): located at the base of the appendix, located in the middle part of the appendix, located in the apex of the appendix, or located in the abdominal cavity. Other clinical variables evaluated included sex, age, body mass index (BMI), body temperature, white blood cell count, CRP, and the duration of symptoms.
The final clinical diagnosis for patients undergoing an appendectomy had already been determined by two researchers for the APPAC II2 and APPAC III25 RCTs based on both surgical and histopathological findings. The surgical finding of perforation was evaluated as complicated acute appendicitis, as well as gangrene of the appendix, when supported by both surgery and histopathology. The finding of transmural neutrophil invasion involving the appendiceal muscularis layer of the removed appendix was required for the histopathological diagnosis of acute appendicitis. An appendiceal neoplasm and/or abscess was classified as complicated acute appendicitis. For patients treated with antibiotics, the CT definition of uncomplicated acute appendicitis included an appendiceal diameter of over 6 mm with typical findings of wall thickening and enhancement, and/or peri-appendiceal oedema, and/or a minor amount of fluid around the appendix. For patients with a peri-appendicular abscess using CT who were treated conservatively, the diagnosis was based on the CT finding, when no alternative diagnosis was suggested within a 30-day follow-up interval.
Statistical methods
Continuous variables are described as mean(s.d.) for normally distributed variables and as median (range or interquartile range) for non-normally distributed variables. Categorical variables are described as n (%). Univariable analyses for the association of categorical variables with complicated appendicitis were performed using Pearson’s chi-squared test or Fisher’s exact test when needed. For the continuous explanatory variables binomial logistic regression was used for univariable analyses.
A receiver operating characteristic (ROC) curve was used to determine a possible cut-off value for appendicolith diameter to predict complicated acute appendicitis. The area under the ROC curve (AUC) with 95% confidence intervals is presented as the result of the analysis. Complicated appendicitis was further analysed using multiple binomial logistic regression analysis. All variables that were statistically significant in the univariable analyses were included in the first model and then non-significant variables were excluded from the model one by one. The final model only included the variables that were statistically significant. As the duration of symptoms had many missing values, it was not included in the model selection procedure (first model). Instead, an additional multiple logistic regression analysis was performed to evaluate the association of appendicolith diameter and duration of symptoms with complicated appendicitis. This additional model also included the interaction of appendicolith diameter and duration of symptoms. The results of logistic analyses were quantified using ORs with 95% confidence intervals.
Two-sided tests were used and P < 0.05 was considered statistically significant. Statistical analyses were performed using SAS System for Windows, version 9.4 (SAS Institute Inc., Cary, NC, USA) and Figs 2 and 3 were drawn using R 3.0.2 (R Foundation for Statistical Computing, Vienna, Austria).
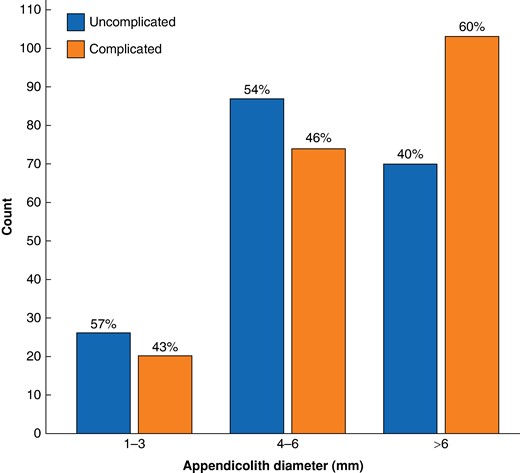
Effect of appendicolith diameter (categorized into three groups) on the risk of complicated appendicitis
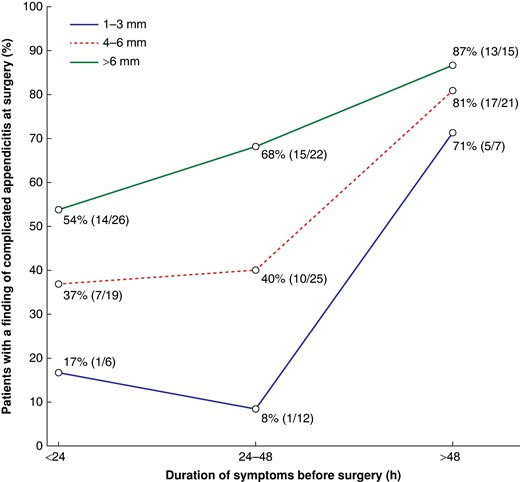
Subgroup analysis of the association between duration of symptoms and complicated acute appendicitis with an appendicolith
Results
Altogether, 3512 patients with suspected acute appendicitis in 9 different Finnish hospitals prospectively collected between 1 April 2017 and 27 November 2018 at evaluation for enrolment in APPAC II2 and III25 RCTs were reviewed for this substudy. Of these, 3085 patients were diagnosed with acute appendicitis using CT and included in the initial analysis assessing the association of a CT-diagnosed appendicolith with complicated appendicitis. Out of these, 1101 patients (35.7%) presented with an appendicolith using CT and 1984 patients had appendicitis with no appendicolith. Out of the 1101 patients with an appendicolith, 519 (47.1% (95% c.i. 44.2% to 50.1%)) had complicated acute appendicitis and, in the 1984 patients with no appendicolith, 426 (21.5% (95% c.i. 19.7% to 23.3%)) had complicated appendicitis (P < 0.001). The study flow chart is presented in Fig. 1. Out of the 1101 patients, there were 380 patients (34.5%) available for the main analysis, having appendicitis, an appendicolith, and a CT image available for re-evaluation. Of these 380 patients from 7 different hospitals (Table S1), 51.8% (95% c.i. 46.8% to 56.9%) had complicated acute appendicitis (197 patients). Patient demographics and baseline characteristics are presented in Table 1. All 274 patients evaluated at Turku University Hospital and an additional 112 patients from other study hospitals with available CT images were eligible for analyses; 715 patients evaluated in other study hospitals were excluded due to the unavailability of original CT images based on the lack of written informed consent. Out of the 380 patients with appendicitis and an appendicolith, 367 underwent an appendectomy and 13 patients were initially treated with antibiotics. Of these 13 patients treated with antibiotics, 7 patients had a peri-appendicular abscess and 6 patients had acute appendicitis with an appendicolith; 8 patients underwent an interval appendectomy and 5 patients were treated with antibiotics only.
| . | n . | Missing values (n) . | All . | Appendicolith and complicated acute appendicitis . | Appendicolith and uncomplicated acute appendicitis . | P* . |
|---|---|---|---|---|---|---|
| Patients | 380 | 0 | 380 | 197† (51.8) | 183 (48.2) | – |
| Sex‡ | ||||||
| Male | 226 | 0 | 226 | 115 (50.9) | 111 (49.1) | – |
| Female | 154 | 0 | 154 | 82 (53.2) | 72 (46.8) | – |
| Age (years), mean(s.d.) | 380 | 0 | 43.2(17.0) | 47.0(17.6) | 39.1(15.4) | <0.001 |
| BMI (kg/m2), median (range) | 372 | 8 | 26.1 (16.9–53.3) | 26.1 (18.8–50.8) | 26.1 (16.9–53.3) | 0.82 |
| Body temperature (°C), mean(s.d.) | 364 | 16 | 37.6(0.7) | 37.8(0.7) | 37.4(0.6) | <0.001 |
| White blood cell count (×109/l), median (i.q.r. or range) | 380 | 0 | 14.1 (i.q.r. 11.4–16.6) | 14.3 (range 12.2–17.2) | 13.6 (range 10.9–16.3) | 0.013 |
| C-reactive protein (mg/l), median (i.q.r.) | 380 | 0 | 37 (12–111) | 73 (25–158) | 18 (6–47) | <0.001 |
| Duration of symptoms before surgery§ (h), median (i.q.r.) | 153 | 227 | 33.5 (20.7–54.9) | 37.6 (22.0–62.3) | 26.1 (17.8–40.0) | <0.001 |
| . | n . | Missing values (n) . | All . | Appendicolith and complicated acute appendicitis . | Appendicolith and uncomplicated acute appendicitis . | P* . |
|---|---|---|---|---|---|---|
| Patients | 380 | 0 | 380 | 197† (51.8) | 183 (48.2) | – |
| Sex‡ | ||||||
| Male | 226 | 0 | 226 | 115 (50.9) | 111 (49.1) | – |
| Female | 154 | 0 | 154 | 82 (53.2) | 72 (46.8) | – |
| Age (years), mean(s.d.) | 380 | 0 | 43.2(17.0) | 47.0(17.6) | 39.1(15.4) | <0.001 |
| BMI (kg/m2), median (range) | 372 | 8 | 26.1 (16.9–53.3) | 26.1 (18.8–50.8) | 26.1 (16.9–53.3) | 0.82 |
| Body temperature (°C), mean(s.d.) | 364 | 16 | 37.6(0.7) | 37.8(0.7) | 37.4(0.6) | <0.001 |
| White blood cell count (×109/l), median (i.q.r. or range) | 380 | 0 | 14.1 (i.q.r. 11.4–16.6) | 14.3 (range 12.2–17.2) | 13.6 (range 10.9–16.3) | 0.013 |
| C-reactive protein (mg/l), median (i.q.r.) | 380 | 0 | 37 (12–111) | 73 (25–158) | 18 (6–47) | <0.001 |
| Duration of symptoms before surgery§ (h), median (i.q.r.) | 153 | 227 | 33.5 (20.7–54.9) | 37.6 (22.0–62.3) | 26.1 (17.8–40.0) | <0.001 |
Values are n (%) unless otherwise indicated. *Logistic regression analysis. †Of these 197 patients with complicated acute appendicitis, there were 138 patients with gangrenous appendicitis, 29 patients with a peri-appendicular abscess, 121 patients with perforation of the appendix, and 7 patients with a tumour; these findings are not mutually exclusive, such that one patient may have had several of the findings mentioned above. ‡The sex of the patient had no association with complicated acute appendicitis (P = 0.637; chi-squared test). §The duration of symptoms before surgery was the time from the onset of the first symptom (pain, nausea, or vomiting) to surgery. i.q.r., interquartile range.
| . | n . | Missing values (n) . | All . | Appendicolith and complicated acute appendicitis . | Appendicolith and uncomplicated acute appendicitis . | P* . |
|---|---|---|---|---|---|---|
| Patients | 380 | 0 | 380 | 197† (51.8) | 183 (48.2) | – |
| Sex‡ | ||||||
| Male | 226 | 0 | 226 | 115 (50.9) | 111 (49.1) | – |
| Female | 154 | 0 | 154 | 82 (53.2) | 72 (46.8) | – |
| Age (years), mean(s.d.) | 380 | 0 | 43.2(17.0) | 47.0(17.6) | 39.1(15.4) | <0.001 |
| BMI (kg/m2), median (range) | 372 | 8 | 26.1 (16.9–53.3) | 26.1 (18.8–50.8) | 26.1 (16.9–53.3) | 0.82 |
| Body temperature (°C), mean(s.d.) | 364 | 16 | 37.6(0.7) | 37.8(0.7) | 37.4(0.6) | <0.001 |
| White blood cell count (×109/l), median (i.q.r. or range) | 380 | 0 | 14.1 (i.q.r. 11.4–16.6) | 14.3 (range 12.2–17.2) | 13.6 (range 10.9–16.3) | 0.013 |
| C-reactive protein (mg/l), median (i.q.r.) | 380 | 0 | 37 (12–111) | 73 (25–158) | 18 (6–47) | <0.001 |
| Duration of symptoms before surgery§ (h), median (i.q.r.) | 153 | 227 | 33.5 (20.7–54.9) | 37.6 (22.0–62.3) | 26.1 (17.8–40.0) | <0.001 |
| . | n . | Missing values (n) . | All . | Appendicolith and complicated acute appendicitis . | Appendicolith and uncomplicated acute appendicitis . | P* . |
|---|---|---|---|---|---|---|
| Patients | 380 | 0 | 380 | 197† (51.8) | 183 (48.2) | – |
| Sex‡ | ||||||
| Male | 226 | 0 | 226 | 115 (50.9) | 111 (49.1) | – |
| Female | 154 | 0 | 154 | 82 (53.2) | 72 (46.8) | – |
| Age (years), mean(s.d.) | 380 | 0 | 43.2(17.0) | 47.0(17.6) | 39.1(15.4) | <0.001 |
| BMI (kg/m2), median (range) | 372 | 8 | 26.1 (16.9–53.3) | 26.1 (18.8–50.8) | 26.1 (16.9–53.3) | 0.82 |
| Body temperature (°C), mean(s.d.) | 364 | 16 | 37.6(0.7) | 37.8(0.7) | 37.4(0.6) | <0.001 |
| White blood cell count (×109/l), median (i.q.r. or range) | 380 | 0 | 14.1 (i.q.r. 11.4–16.6) | 14.3 (range 12.2–17.2) | 13.6 (range 10.9–16.3) | 0.013 |
| C-reactive protein (mg/l), median (i.q.r.) | 380 | 0 | 37 (12–111) | 73 (25–158) | 18 (6–47) | <0.001 |
| Duration of symptoms before surgery§ (h), median (i.q.r.) | 153 | 227 | 33.5 (20.7–54.9) | 37.6 (22.0–62.3) | 26.1 (17.8–40.0) | <0.001 |
Values are n (%) unless otherwise indicated. *Logistic regression analysis. †Of these 197 patients with complicated acute appendicitis, there were 138 patients with gangrenous appendicitis, 29 patients with a peri-appendicular abscess, 121 patients with perforation of the appendix, and 7 patients with a tumour; these findings are not mutually exclusive, such that one patient may have had several of the findings mentioned above. ‡The sex of the patient had no association with complicated acute appendicitis (P = 0.637; chi-squared test). §The duration of symptoms before surgery was the time from the onset of the first symptom (pain, nausea, or vomiting) to surgery. i.q.r., interquartile range.
In univariable analysis, appendicolith diameter was associated with complicated acute appendicitis, even though a clear cut-off value could not be determined (AUC 0.60 (95% c.i. 0.54 to 0.65); P < 0.001). See Table 2. The association was also statistically significant (P = 0.022) when appendicolith diameter was categorized into three groups (1–3 mm, 4–6 mm, and over 6 mm). See Fig. 2. When comparing an appendicolith diameter of 4–6 mm with an appendicolith diameter of 1–3 mm, the OR for complicated appendicitis was 1.11 (95% c.i. 0.57 to 2.14); when comparing an appendicolith diameter of over 6 mm with an appendicolith diameter of 1–3 mm, the OR was 1.91 (95% c.i. 0.99 to 3.69); and when comparing an appendicolith diameter of over 6 mm with an appendicolith diameter of 3–6 mm, the OR was 1.17 (95% c.i. 1.12 to 2.67). Appendicolith location at the base of the appendix was associated with complicated acute appendicitis (P = 0.008). Of the other assessed CT variables, appendicolith-induced pressure (P = 0.003) and heterogeneous appendiceal wall enhancement around the appendicolith (P < 0.001) were associated with complicated acute appendicitis. See Table 2.
Characteristics of intraluminal appendicoliths in patients with acute appendicitis
| . | n . | Missing values (n) . | Appendicolith and complicated acute appendicitis . | Appendicolith and uncomplicated acute appendicitis . | P . | OR* (95% c.i.) . |
|---|---|---|---|---|---|---|
| Appendicolith length (mm), median (i.q.r.) | 380 | 0 | 9.0 (7.0–12.0) | 8.0 (6.0–11.0) | 0.767† | 1.006 (0.969,1.043) |
| Appendicolith diameter (mm), median (i.q.r.) | 380 | 0 | 7.0 (5.0–8.0) | 6.0 (4.0–7.0) | 0.001† | 1.153 (1.061,1.253) |
| Appendicolith location‡ | 374 | 6 | 195 (52.1) | 179 (47.9) | 0.0076§ | – |
| Base of the appendix | 287 | 158 (55.1) | 129 (44.9) | |||
| Middle part and apex of the appendix | 60 + 21 = 81 | 24 + 7 = 31 (38.3) | 36 + 14 = 50 (61.7) | |||
| Abdominal cavity | 6 | 6 | 0 | |||
| Appendicolith-induced pressure on the wall of the appendix | 276 | 13 | 155 (56.2) | 121 (43.8) | 0.003§ | – |
| No pressure effect on the wall of the appendix | 91 | 35 (38.5) | 56 (61.5) | |||
| Heterogeneous appendiceal wall enhancement around the appendicolith | 212 | 6 | 145 (68.4) | 67 (31.6) | <0.001§ | – |
| No unenhanced areas in the appendix wall around the appendicolith | 162 | 49 (30.2) | 113 (69.8) | |||
| Appendiceal diameter (mm), median (i.q.r.) | 366 | 14 | 14 (12–16) | 12 (10–15) | <0.001§ | 1.14 (1.06,1.22) |
| . | n . | Missing values (n) . | Appendicolith and complicated acute appendicitis . | Appendicolith and uncomplicated acute appendicitis . | P . | OR* (95% c.i.) . |
|---|---|---|---|---|---|---|
| Appendicolith length (mm), median (i.q.r.) | 380 | 0 | 9.0 (7.0–12.0) | 8.0 (6.0–11.0) | 0.767† | 1.006 (0.969,1.043) |
| Appendicolith diameter (mm), median (i.q.r.) | 380 | 0 | 7.0 (5.0–8.0) | 6.0 (4.0–7.0) | 0.001† | 1.153 (1.061,1.253) |
| Appendicolith location‡ | 374 | 6 | 195 (52.1) | 179 (47.9) | 0.0076§ | – |
| Base of the appendix | 287 | 158 (55.1) | 129 (44.9) | |||
| Middle part and apex of the appendix | 60 + 21 = 81 | 24 + 7 = 31 (38.3) | 36 + 14 = 50 (61.7) | |||
| Abdominal cavity | 6 | 6 | 0 | |||
| Appendicolith-induced pressure on the wall of the appendix | 276 | 13 | 155 (56.2) | 121 (43.8) | 0.003§ | – |
| No pressure effect on the wall of the appendix | 91 | 35 (38.5) | 56 (61.5) | |||
| Heterogeneous appendiceal wall enhancement around the appendicolith | 212 | 6 | 145 (68.4) | 67 (31.6) | <0.001§ | – |
| No unenhanced areas in the appendix wall around the appendicolith | 162 | 49 (30.2) | 113 (69.8) | |||
| Appendiceal diameter (mm), median (i.q.r.) | 366 | 14 | 14 (12–16) | 12 (10–15) | <0.001§ | 1.14 (1.06,1.22) |
Values are n (%) unless otherwise indicated. *OR for one-unit increases in continuous variables (appendicolith length, 1 mm; appendicolith diameter, 1 mm; and appendiceal diameter, 1 mm). †Logistic regression analyses. ‡Appendicoliths located at the base of the appendix were compared with appendicoliths located in the middle part and apex of the appendix; extraluminal appendicoliths located in the abdominal cavity were excluded. All three groups of appendicoliths located within the appendiceal lumen were initially analysed separately, but as only the appendicoliths located at the base of the appendix were associated with complicated appendicitis, the other locations were combined for the final analysis. §Chi-squared test. i.q.r., interquartile range.
Characteristics of intraluminal appendicoliths in patients with acute appendicitis
| . | n . | Missing values (n) . | Appendicolith and complicated acute appendicitis . | Appendicolith and uncomplicated acute appendicitis . | P . | OR* (95% c.i.) . |
|---|---|---|---|---|---|---|
| Appendicolith length (mm), median (i.q.r.) | 380 | 0 | 9.0 (7.0–12.0) | 8.0 (6.0–11.0) | 0.767† | 1.006 (0.969,1.043) |
| Appendicolith diameter (mm), median (i.q.r.) | 380 | 0 | 7.0 (5.0–8.0) | 6.0 (4.0–7.0) | 0.001† | 1.153 (1.061,1.253) |
| Appendicolith location‡ | 374 | 6 | 195 (52.1) | 179 (47.9) | 0.0076§ | – |
| Base of the appendix | 287 | 158 (55.1) | 129 (44.9) | |||
| Middle part and apex of the appendix | 60 + 21 = 81 | 24 + 7 = 31 (38.3) | 36 + 14 = 50 (61.7) | |||
| Abdominal cavity | 6 | 6 | 0 | |||
| Appendicolith-induced pressure on the wall of the appendix | 276 | 13 | 155 (56.2) | 121 (43.8) | 0.003§ | – |
| No pressure effect on the wall of the appendix | 91 | 35 (38.5) | 56 (61.5) | |||
| Heterogeneous appendiceal wall enhancement around the appendicolith | 212 | 6 | 145 (68.4) | 67 (31.6) | <0.001§ | – |
| No unenhanced areas in the appendix wall around the appendicolith | 162 | 49 (30.2) | 113 (69.8) | |||
| Appendiceal diameter (mm), median (i.q.r.) | 366 | 14 | 14 (12–16) | 12 (10–15) | <0.001§ | 1.14 (1.06,1.22) |
| . | n . | Missing values (n) . | Appendicolith and complicated acute appendicitis . | Appendicolith and uncomplicated acute appendicitis . | P . | OR* (95% c.i.) . |
|---|---|---|---|---|---|---|
| Appendicolith length (mm), median (i.q.r.) | 380 | 0 | 9.0 (7.0–12.0) | 8.0 (6.0–11.0) | 0.767† | 1.006 (0.969,1.043) |
| Appendicolith diameter (mm), median (i.q.r.) | 380 | 0 | 7.0 (5.0–8.0) | 6.0 (4.0–7.0) | 0.001† | 1.153 (1.061,1.253) |
| Appendicolith location‡ | 374 | 6 | 195 (52.1) | 179 (47.9) | 0.0076§ | – |
| Base of the appendix | 287 | 158 (55.1) | 129 (44.9) | |||
| Middle part and apex of the appendix | 60 + 21 = 81 | 24 + 7 = 31 (38.3) | 36 + 14 = 50 (61.7) | |||
| Abdominal cavity | 6 | 6 | 0 | |||
| Appendicolith-induced pressure on the wall of the appendix | 276 | 13 | 155 (56.2) | 121 (43.8) | 0.003§ | – |
| No pressure effect on the wall of the appendix | 91 | 35 (38.5) | 56 (61.5) | |||
| Heterogeneous appendiceal wall enhancement around the appendicolith | 212 | 6 | 145 (68.4) | 67 (31.6) | <0.001§ | – |
| No unenhanced areas in the appendix wall around the appendicolith | 162 | 49 (30.2) | 113 (69.8) | |||
| Appendiceal diameter (mm), median (i.q.r.) | 366 | 14 | 14 (12–16) | 12 (10–15) | <0.001§ | 1.14 (1.06,1.22) |
Values are n (%) unless otherwise indicated. *OR for one-unit increases in continuous variables (appendicolith length, 1 mm; appendicolith diameter, 1 mm; and appendiceal diameter, 1 mm). †Logistic regression analyses. ‡Appendicoliths located at the base of the appendix were compared with appendicoliths located in the middle part and apex of the appendix; extraluminal appendicoliths located in the abdominal cavity were excluded. All three groups of appendicoliths located within the appendiceal lumen were initially analysed separately, but as only the appendicoliths located at the base of the appendix were associated with complicated appendicitis, the other locations were combined for the final analysis. §Chi-squared test. i.q.r., interquartile range.
Of the patient-related variables, older age (P < 0.001), higher body temperature (P < 0.001), higher white blood cell count (P = 0.013) or CRP (P < 0.001), longer duration of symptoms (P = 0.004), and wider appendiceal diameter (P < 0.001) were associated with complicated acute appendicitis. Sex (P = 0.637) and BMI (P = 0.825) were not associated with complicated acute appendicitis. See Tables 1–3.
Univariable logistic regression analysis of the association of patient characteristics with complicated acute appendicitis in patients with acute appendicitis and an appendicolith
| . | n . | OR* (95% c.i.) . | P† . |
|---|---|---|---|
| Age | 380 | 1.03 (1.02,1.04) | <0.001 |
| BMI | 372 | 1.00 (0.96,1.03) | 0.825 |
| Body temperature | 364 | 2.67 (1.90,3.76) | <0.001 |
| White blood cell count | 380 | 1.07 (1.01,1.13) | 0.013 |
| C-reactive protein | 380 | 1.02 (1.01,1.02) | <0.001 |
| Duration of symptoms before surgery‡ | 153 | 1.03 (1.01,1.04) | <0.001 |
| . | n . | OR* (95% c.i.) . | P† . |
|---|---|---|---|
| Age | 380 | 1.03 (1.02,1.04) | <0.001 |
| BMI | 372 | 1.00 (0.96,1.03) | 0.825 |
| Body temperature | 364 | 2.67 (1.90,3.76) | <0.001 |
| White blood cell count | 380 | 1.07 (1.01,1.13) | 0.013 |
| C-reactive protein | 380 | 1.02 (1.01,1.02) | <0.001 |
| Duration of symptoms before surgery‡ | 153 | 1.03 (1.01,1.04) | <0.001 |
*OR for one-unit increases in continuous variables (age, 1 year; BMI, 1 kg/m2; body temperature 1°C; white blood cell count, 1×109/l; C-reactive protein, 1 mg/l; and duration of symptoms before surgery, 1 h). †Logistic regression analysis. ‡The duration of symptoms before surgery was the time from the onset of the first symptom (pain, nausea, or vomiting) to surgery. BMI, body mass index.
Univariable logistic regression analysis of the association of patient characteristics with complicated acute appendicitis in patients with acute appendicitis and an appendicolith
| . | n . | OR* (95% c.i.) . | P† . |
|---|---|---|---|
| Age | 380 | 1.03 (1.02,1.04) | <0.001 |
| BMI | 372 | 1.00 (0.96,1.03) | 0.825 |
| Body temperature | 364 | 2.67 (1.90,3.76) | <0.001 |
| White blood cell count | 380 | 1.07 (1.01,1.13) | 0.013 |
| C-reactive protein | 380 | 1.02 (1.01,1.02) | <0.001 |
| Duration of symptoms before surgery‡ | 153 | 1.03 (1.01,1.04) | <0.001 |
| . | n . | OR* (95% c.i.) . | P† . |
|---|---|---|---|
| Age | 380 | 1.03 (1.02,1.04) | <0.001 |
| BMI | 372 | 1.00 (0.96,1.03) | 0.825 |
| Body temperature | 364 | 2.67 (1.90,3.76) | <0.001 |
| White blood cell count | 380 | 1.07 (1.01,1.13) | 0.013 |
| C-reactive protein | 380 | 1.02 (1.01,1.02) | <0.001 |
| Duration of symptoms before surgery‡ | 153 | 1.03 (1.01,1.04) | <0.001 |
*OR for one-unit increases in continuous variables (age, 1 year; BMI, 1 kg/m2; body temperature 1°C; white blood cell count, 1×109/l; C-reactive protein, 1 mg/l; and duration of symptoms before surgery, 1 h). †Logistic regression analysis. ‡The duration of symptoms before surgery was the time from the onset of the first symptom (pain, nausea, or vomiting) to surgery. BMI, body mass index.
After univariable analyses, a multiple logistic regression analysis was performed including the most significant variables associated with complicated appendicitis. See Table 4. The final model included appendicolith diameter (P = 0.002), age (P = 0.012), body temperature (P = 0.003), CRP (P < 0.001), and heterogeneous appendiceal wall enhancement around the appendicolith (P < 0.001). These variables had the strongest association with complicated acute appendicitis, with higher values increasing the odds of complicated acute appendicitis.
Multiple logistic regression analysis including the most significant variables associated with complicated appendicitis
| . | OR* (95% c.i.) . | P† . |
|---|---|---|
| Appendicolith diameter | 1.18 (1.06,1.31) | 0.002 |
| Age | 1.02 (1.01,1.04) | 0.012 |
| Body temperature | 1.87 (1.24,2.83) | 0.003 |
| C-reactive protein | 1.01 (1.01,1.02) | <0.001 |
| Heterogeneous appendiceal wall enhancement around the appendicolith | 2.57‡ (1.53,4.32) | <0.001 |
| . | OR* (95% c.i.) . | P† . |
|---|---|---|
| Appendicolith diameter | 1.18 (1.06,1.31) | 0.002 |
| Age | 1.02 (1.01,1.04) | 0.012 |
| Body temperature | 1.87 (1.24,2.83) | 0.003 |
| C-reactive protein | 1.01 (1.01,1.02) | <0.001 |
| Heterogeneous appendiceal wall enhancement around the appendicolith | 2.57‡ (1.53,4.32) | <0.001 |
*OR for one-unit increases in continuous variables (appendicolith diameter, 1 mm; age, 1 year; body temperature, 1°C; and C-reactive protein, 1 mg/l). †Logistic regression analyses. ‡OR for categorical variable.
Multiple logistic regression analysis including the most significant variables associated with complicated appendicitis
| . | OR* (95% c.i.) . | P† . |
|---|---|---|
| Appendicolith diameter | 1.18 (1.06,1.31) | 0.002 |
| Age | 1.02 (1.01,1.04) | 0.012 |
| Body temperature | 1.87 (1.24,2.83) | 0.003 |
| C-reactive protein | 1.01 (1.01,1.02) | <0.001 |
| Heterogeneous appendiceal wall enhancement around the appendicolith | 2.57‡ (1.53,4.32) | <0.001 |
| . | OR* (95% c.i.) . | P† . |
|---|---|---|
| Appendicolith diameter | 1.18 (1.06,1.31) | 0.002 |
| Age | 1.02 (1.01,1.04) | 0.012 |
| Body temperature | 1.87 (1.24,2.83) | 0.003 |
| C-reactive protein | 1.01 (1.01,1.02) | <0.001 |
| Heterogeneous appendiceal wall enhancement around the appendicolith | 2.57‡ (1.53,4.32) | <0.001 |
*OR for one-unit increases in continuous variables (appendicolith diameter, 1 mm; age, 1 year; body temperature, 1°C; and C-reactive protein, 1 mg/l). †Logistic regression analyses. ‡OR for categorical variable.
A subgroup analysis was conducted combining the appendicolith diameter groups (1–3 mm, 4–6 mm, and over 6 mm) and the duration of symptoms before surgery to assess the association of these two variables with the severity of appendicitis. See Fig. 3. The duration of symptoms before surgery was the time from the onset of the first symptom to surgery. There were 153 patients with data available for duration of symptoms and appendicolith diameter who were included in this subgroup analysis. In logistic regression analysis, the interaction of appendicolith diameter and duration of symptoms was not statistically significant (P = 0.732). Instead, a longer duration of symptoms before surgery had a statistically significant effect (P < 0.001) on complicated appendicitis, regardless of appendicolith diameter. Compared with patients operated on within 24 h after symptom onset, the OR of having complicated appendicitis was 1.30 (95% c.i. 0.58 to 2.90) for patients operated on between 24 and 48 h after symptom onset and 8.51 (95% c.i. 3.01 to 24.07) for patients operated on over 48 h after symptom onset.
Discussion
This study reports a statistically significant association between a larger appendicolith diameter and complicated acute appendicitis, but no cut-off value for appendiceal diameter for the increased risk of complicated appendicitis could be determined and even in the group of patients with appendicoliths having a diameter of 1–3 mm almost half of the patients had complicated appendicitis. There was a statistically significant difference in the prevalence of complicated acute appendicitis between patients who presented with both acute appendicitis with an appendicolith and patients without an appendicolith (47.1% versus 21.5% respectively). Other appendicolith- and patient-related findings predictive of having complicated acute appendicitis in patients with appendicitis and an appendicolith included appendicolith location at the base of the appendix and heterogeneous appendiceal wall enhancement around the appendicolith, older age, higher body temperature, and higher CRP. In clinical practice, these factors may be used to assist decision-making and patient information as patients with appendicitis and an appendicolith may not be optimal for non-operative treatment and these results do steer the clinical thinking towards favouring an appendectomy.
International definitions of complicated appendicitis are not standardized. The criteria balance between the clinical idea of ruling out complicated acute appendicitis resulting in an optimized and more selected patient population of uncomplicated acute appendicitis and the other perspective of aiming to extend the non-operative treatment option to a larger patient population with a potentially higher risk of complicated acute appendicitis. Although in the CODA trial5 half of the patients with appendicolith appendicitis initially treated with antibiotics avoided surgical treatment in the first 2 years, the majority of complications were found in patients with appendicoliths, supporting the view that all appendicoliths present a risk factor for complicated acute appendicitis, corroborated by the present study.
This study was unable to determine a clear cut-off value for appendicolith diameter, in contrast to the findings of many other studies, reporting an appendicolith diameter of 5 mm to be a cut-off value for increased risk of complicated appendicitis17,23,24. However, these studies have methodological limitations (including only selected appendicolith patients undergoing an appendectomy and lack of histopathology of the removed appendix)17,23. Appendicolith diameter was associated with complicated acute appendicitis, even though a clear cut-off value could not be determined.
This study has several limitations. First, there were 1101 patients presenting with an appendicolith using CT, but only 386 patients had CT images that were available for retrospective review, because of both a lack of written informed consent from some of the non-randomized patients to re-evaluate their CT images and the unavailability of CT images from some of the study hospitals. However, despite the suboptimal availability of the CT images, to the authors’ knowledge, this is so far the largest data set assessing specific CT features of appendicoliths in a prospective patient cohort. In addition, the prevalence of complicated acute appendicitis in the 380 study patients was very similar to the prevalence of complicated acute appendicitis in all of the appendicolith patients in the cohort, adding to the generalizability of the results of this selected cohort. Second, some of the assessed variables, such as appendicolith-induced pressure and appendicolith-induced heterogeneous appendiceal wall enhancement are naturally subjective and radiologist dependent, and the interobserver variability was not assessed. However, the radiologists used standardized uniform criteria when assessing these variables. Third, the suboptimal recording of the duration of symptoms is a clear limitation of this study. Fourth, for some patients who were treated with antibiotics the final diagnosis was based on the CT finding and uneventful recovery, and thus the reference standard could be considered suboptimal. The main strengths of this study include the large prospective patient cohort and the clinical diagnosis of acute appendicitis severity that was as accurate as possible, using evaluation of CT images by two radiologists and clinical evaluation by two researchers based on both surgical and histopathological findings.
In conclusion, it is generally thought that an appendicolith is a complicating factor in acute appendicitis. The results of the present study corroborate the previous findings, showing that the presence of an appendicolith is associated with a significantly increased risk of complicated acute appendicitis compared with the absence of an appendicolith. This risk was further increased by a larger appendicolith diameter, appendicolith location at the base of the appendix, and heterogeneous appendiceal wall enhancement around the appendicolith. In addition, no appendicolith subgroup or feature was found that did not have an increased risk of complicated acute appendicitis. For patients presenting with both acute appendicitis and an appendicolith, an appendectomy remains the best treatment option. When antibiotic treatment is considered for a patient with an appendicolith, the patient needs to be informed of the increased risk of complicated acute appendicitis and appendectomy, and the surgeon should exclude the appendicolith CT features prognostic of non-responsiveness to antibiotics.
Funding
This study was supported by the Academy of Finland, the Sigrid Jusélius Foundation, the Finnish Medical Foundation, and the Orion Research Foundation. The funders had no role in the design and conduct of this study.
Acknowledgements
The authors thank Eeva-Liisa Sävelä (Satasairaala Central Hospital), Imre Ilves (Mikkeli Central Hospital), and the whole APPAC study group for their contribution to patient recruitment. The authors would also like to thank the Academy of Finland (Paulina Salminen), the Sigrid Jusélius Foundation (Paulina Salminen), the Finnish Medical Foundation (Sami Sula), and the Orion Research Foundation (Sami Sula) for providing research grants. Timo Paananen and Ville Tammilehto contributed equally as second authors and Jussi M. Haijanen and Paulina Salminen contributed equally as last authors.
Author contributions
Sami Sula (Data curation, Formal analysis, Investigation, Methodology, Writing—original draft), Timo Paananen (Data curation, Formal analysis, Investigation), Ville Tammilehto (Data curation, Formal analysis, Investigation), Saija Hurme (Data curation, Formal analysis, Methodology, Software), Anne Mattila (Data curation, Writing—review & editing), Tuomo Rantanen (Data curation, Writing—review & editing), Tero Rautio (Data curation, Writing—review & editing), Tarja Pinta (Data curation, Writing—review & editing), Suvi Sippola (Data curation, Writing—review & editing), Jussi M. Haijanen (Conceptualization, Data curation, Investigation, Methodology, Supervision, Writing—review & editing), and Paulina Salminen (Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Supervision, Writing—review & editing)
Disclosure
Paulina Salminen declares lecture fees from Novo Nordisk. All other authors declare no conflicts of interest.
Supplementary material
Supplementary material is available at BJS Open online.
Data availability
A complete deidentified patient data set will be made available to researchers on request. Individuals wishing to access the data should send a request to the corresponding author.



