-
Views
-
Cite
Cite
Kenta Yamaguchi, Masaaki Konishi, Nobuyuki Kagiyama, Takatoshi Kasai, Kentaro Kamiya, Hiroshi Saito, Kazuya Saito, Emi Maekawa, Takeshi Kitai, Kentaro Iwata, Kentaro Jujo, Hiroshi Wada, Satoru Shinoda, Eiichi Akiyama, Shin-Ichi Momomura, Kiyoshi Hibi, Yuya Matsue, Association of Low Muscle Strength With Incident Pneumonia in Older Patients With Heart Failure, The Journals of Gerontology: Series A, Volume 80, Issue 1, January 2025, glae266, https://doi.org/10.1093/gerona/glae266
Close - Share Icon Share
Abstract
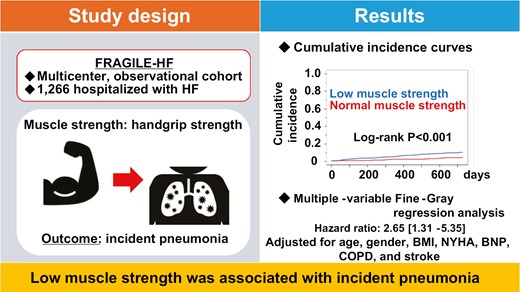
Patients with heart failure (HF) are at an increased risk of developing pneumonia, leading to a high mortality. A decrease in muscle strength due to aging or concomitant disease may contribute to the development of pneumonia in older adults. We sought to investigate the relationship between low muscle strength and pneumonia incidence in older patients hospitalized for worsening HF.
We carried out a subanalysis of the FRAGILE-HF, a prospective multicenter observational study, including 1 266 consecutive older (≥65 years) patients hospitalized with HF (mean age 80.2 ± 7.8 years; 57.4% male; left ventricular ejection fraction 46% ± 17%) and information of incident pneumonia observed after discharge. Patients were followed up for 2 years post-discharge.
A total of 88 patients (7.0%) developed pneumonia after discharge, with an incidence of 42.7 per 1 000 person-years. A total of 893 patients with low muscle strength, defined as handgrip strength <28 kg for men and <18 kg for women according to international criteria, were more likely to develop pneumonia than those with normal muscle strength (p < .001; log-rank test). Low muscle strength was a significant predictor of incident pneumonia (adjusted hazard ratio with 95% confidence interval: 2.65 [1.31–5.35], p = .007). Furthermore, the mortality rates were 43.2% in patients who developed pneumonia and 19.3% in those who did not, indicating a heightened risk of death following the onset of pneumonia (adjusted hazard ratio: 4.25 [2.91–6.19], p < .001).
In older patients hospitalized for HF, low muscle strength was associated with incident pneumonia after discharge.