-
PDF
- Split View
-
Views
-
Cite
Cite
Emily Erlenbach, Edward McAuley, Neha P Gothe, The Association Between Light Physical Activity and Cognition Among Adults: A Scoping Review, The Journals of Gerontology: Series A, Volume 76, Issue 4, April 2021, Pages 716–724, https://doi.org/10.1093/gerona/glab013
Close - Share Icon Share
Abstract
The physical and cognitive benefits of moderate-vigorous intensity physical activity (MVPA) for adults have been well documented. Recently, there has been increasing interest in the independent health benefits of light-intensity physical activity (LPA). This research has primarily focused on the relationship between LPA and morbidity and mortality risk, with few studies investigating cognitive associations. The purpose of this scoping review was to catalog existing evidence on the association between device-based or technologically measured LPA and cognition among adults, identify trends in the literature, and recommend future areas for research.
Six electronic databases were searched between January and June 2020. Forty published studies met the inclusion criteria, which included both healthy and clinical young and older adult populations. Among the 40 articles were 14 acute exercise studies, 4 randomized control trials (RCTs), 18 cross-sectional studies, and 4 longitudinal studies.
7/14 (50%) acute, 3/4 (75%) RCT, 10/18 (56%) cross-sectional, and 2/4 (50%) longitudinal studies reported a significant, positive relationship between LPA and one or more cognitive outcomes. These heterogeneous findings can largely be attributed to the diverse study designs and populations, as well as the numerous assessments used to test the cognitive domains.
These collective findings suggest LPA may be a potential lifestyle intervention to improve cognition across adulthood. However, the inconsistent approaches used among these studies suggest a more concerted, unified scientific approach is needed to further understand the LPA-cognition relationship.
Physical activity is consistently associated with enhanced physical and mental health across the life span. Moderate-vigorous intensity physical activity (MVPA) has traditionally been promoted as the most effective intensity level to induce the greatest health benefits, with official recommendations to achieve a minimum of 150 minutes per week of moderate-intensity, or 75 minutes per week of vigorous-intensity physical activity (1). However, 31.1% of adults across the globe do not meet these recommendations (2). Intrapersonal factors (such as lack of self-efficacy, motivation, or enjoyment) and environmental factors (such as decreases in occupational physical activity, increased availability of labor-saving technology and increased reliance on passive commuting) have largely contributed to the declines in MVPA engagement and increased sedentary behavior (2–6), which is defined as any waking behavior in a sitting or reclining position with an energy expenditure ≤ 1.5 METs (7). Additionally, the worldwide number of adults ≥ 60 years of age is expected to comprise 22% of the total population by 2050 (8), which will have broad-reaching implications for global health care systems. While physical activity engagement is widely promoted as a lifestyle behavior for healthy aging, this population often faces age-related functional and physical limitations preventing MVPA participation (9). Although the health benefits of MVPA are well-documented, less is known about the health benefits of light physical activity (LPA) across the life span and specifically among aging populations.
LPA, defined as any activity requiring an energy expenditure of 1.6–2.9 METs (10), has become an emerging area of interest for its independent contributions to physical health (11–13). After sedentary behavior, which makes up approximately 9.3 hours or 60% of waking hours, LPA is the most engaged in behavior by making up 6.5 hours or 35% of waking hours among adults (4). Currently, no specific guidelines exist for LPA engagement, but broad recommendations of “move more, sit less” are promoted by the Centers for Disease Control and Prevention (14). More recently, researchers have begun studying the positive health contributions of LPA, especially in the context of cardiometabolic risk and mortality, independent of MVPA engagement (15,16). A systematic review of studies utilizing accelerometer data from the National Health and Nutrition Examination Survey observed LPA’s favorable, significant associations with insulin sensitivity, triglyceride and high-density lipoprotein cholesterol levels, adiposity measures, diabetes, and mortality risk (17). However, the authors noted that of the 40 studies included in the review, only 18 adjusted for MVPA. A more recent systematic review (18) built on these previous findings by only including studies which adjusted for MVPA, and largely corroborated the findings of the preceding review (17). Independent of MVPA participation, Amagasa and colleagues (18) found LPA was inversely associated with metabolic syndrome, waist circumference, triglyceride levels, insulin, and mortality. Notably, the research team included cognitive function as one of the reviewed health-related outcomes. Only 2 cross sectional studies met their inclusion criteria and were reviewed, with inconsistent findings, indicating that the cognitive implications of LPA engagement are less clear and are in need of a more thorough investigation.
Therefore, the purpose of this review was to detail the current evidence regarding the association of LPA and cognition among adults in order to understand if any clinically meaningful associations exist. Given the vast number of research designs, populations studied, and cognitive outcomes investigated across the studies, a scoping review was identified as the most appropriate approach to examine the current status of research activity and catalog the existing evidence examining LPA and cognition (19). Scoping reviews are generally used as a first step to “map the literature” of an emerging research field where there is a paucity of synthesized information in order to gauge the necessity of an in-depth systematic review, identify gaps in the literature and provide informed recommendations for further research in the area (20).
Method
This scoping review was conducted following the 5-stage methodological framework for conducting transparent, rigorous scoping reviews suggested by Arksey and O’Malley (20) and updated by Levac and colleagues (19). The 5 stages below follow along with the methodological steps suggested by the aforementioned authors.
Identify the Research Question
The guiding research question for this review was “what is the current evidence regarding the association between LPA and cognition among adults?” The intentional breadth of this question allowed for a broader scope of this field to be surveyed. Furthermore, given LPA is a health behavior which is widely engaged in by populations of all abilities, both clinical (individuals diagnosed with a physical or mental disease) and nonclinical (individuals who do not have any physical or mental clinical diagnoses) adult populations were included in an effort to avoid overlooking relevant studies which may hold clinically meaningful implications. The operational definition of “cognition” was defined as “the set of mental processes that contribute to perception, memory, intellect and action” (21). Therefore, the primary cognitive domains of focus for this scoping review were memory, executive function, attention and processing speed. The additional parameter of “overall cognitive function” was also included to account for studies which assessed global cognitive status (typically in aging studies).
Identify Relevant Studies
A search string was developed by the study author (E.E.), with the assistance of a health sciences librarian, and was based off previously published search strings used in systematic reviews pertaining to cognition (21) and light physical activity (18). In an effort to broadly capture studies examining LPA as a concept, specific physical activity modalities which can performed at light intensities (such as yoga, walking, dance, tai chi, balance, and flexibility training) were not intentionally included in the search string. However, if a study’s primary aim was to study the effects of LPA and utilized one of these modalities in the design, it was eligible for inclusion. The search parameters for cognition included broad terms (ie, cognition, cognitive function, neurocognition, and brain function) as well as specific functions (ie, memory, executive function, attention, and processing speed). The following medical subject headings were specified in the search string: exercise, executive function, cognition, mental processes, memory, attention, and problem solving (22). The list of search terms used can be found in Table 1. Databases searched included CINHAL, PubMed, SPORTDiscus, Scopus, Web of Science, and PsycINFO. All citations were exported to Mendeley Desktop (Version 1.19.4) and Excel, where duplicates were identified and removed.
| Terms Related to Light Physical Activity . | Terms Related to Cognition . | Terms Related to Population of Interest . |
|---|---|---|
| Light-intensity physical activity* | Cognition | Adult* |
| Low-intensity physical activity* | Cognitive function | |
| Light-intensity lifestyle | Brain function | |
| Light-intensity exercise | Executive function | |
| Low-intensity exercise | Executive control | |
| Light-intensity activity* | Memory | |
| Low-intensity activity* | Mental processes | |
| Light-intensity physical activity* | Reaction time | |
| Low-intensity physical activity* | Response latency | |
| Light-intensity lifestyle | Accuracy | |
| Light-intensity exercise | Attention | |
| Low-intensity exercise | Task switching | |
| Problem solving | ||
| Decision making | ||
| Multitasking | ||
| Planning | ||
| Reasoning | ||
| Comprehension | ||
| Spatial memory | ||
| Episodic memory | ||
| Long-term memory | ||
| Declarative memory | ||
| Intelligence | ||
| Neurocognition | ||
| Neurocognitive | ||
| Neuro-cognition | ||
| Neuro-cognitive | ||
| Attentiveness | ||
| Concentration | ||
| Concentrate | ||
| Information retrieval | ||
| Information processing | ||
| Perceptual skills |
| Terms Related to Light Physical Activity . | Terms Related to Cognition . | Terms Related to Population of Interest . |
|---|---|---|
| Light-intensity physical activity* | Cognition | Adult* |
| Low-intensity physical activity* | Cognitive function | |
| Light-intensity lifestyle | Brain function | |
| Light-intensity exercise | Executive function | |
| Low-intensity exercise | Executive control | |
| Light-intensity activity* | Memory | |
| Low-intensity activity* | Mental processes | |
| Light-intensity physical activity* | Reaction time | |
| Low-intensity physical activity* | Response latency | |
| Light-intensity lifestyle | Accuracy | |
| Light-intensity exercise | Attention | |
| Low-intensity exercise | Task switching | |
| Problem solving | ||
| Decision making | ||
| Multitasking | ||
| Planning | ||
| Reasoning | ||
| Comprehension | ||
| Spatial memory | ||
| Episodic memory | ||
| Long-term memory | ||
| Declarative memory | ||
| Intelligence | ||
| Neurocognition | ||
| Neurocognitive | ||
| Neuro-cognition | ||
| Neuro-cognitive | ||
| Attentiveness | ||
| Concentration | ||
| Concentrate | ||
| Information retrieval | ||
| Information processing | ||
| Perceptual skills |
Note: “*” used as wildcard character to search for all phrases which included the truncated term.
| Terms Related to Light Physical Activity . | Terms Related to Cognition . | Terms Related to Population of Interest . |
|---|---|---|
| Light-intensity physical activity* | Cognition | Adult* |
| Low-intensity physical activity* | Cognitive function | |
| Light-intensity lifestyle | Brain function | |
| Light-intensity exercise | Executive function | |
| Low-intensity exercise | Executive control | |
| Light-intensity activity* | Memory | |
| Low-intensity activity* | Mental processes | |
| Light-intensity physical activity* | Reaction time | |
| Low-intensity physical activity* | Response latency | |
| Light-intensity lifestyle | Accuracy | |
| Light-intensity exercise | Attention | |
| Low-intensity exercise | Task switching | |
| Problem solving | ||
| Decision making | ||
| Multitasking | ||
| Planning | ||
| Reasoning | ||
| Comprehension | ||
| Spatial memory | ||
| Episodic memory | ||
| Long-term memory | ||
| Declarative memory | ||
| Intelligence | ||
| Neurocognition | ||
| Neurocognitive | ||
| Neuro-cognition | ||
| Neuro-cognitive | ||
| Attentiveness | ||
| Concentration | ||
| Concentrate | ||
| Information retrieval | ||
| Information processing | ||
| Perceptual skills |
| Terms Related to Light Physical Activity . | Terms Related to Cognition . | Terms Related to Population of Interest . |
|---|---|---|
| Light-intensity physical activity* | Cognition | Adult* |
| Low-intensity physical activity* | Cognitive function | |
| Light-intensity lifestyle | Brain function | |
| Light-intensity exercise | Executive function | |
| Low-intensity exercise | Executive control | |
| Light-intensity activity* | Memory | |
| Low-intensity activity* | Mental processes | |
| Light-intensity physical activity* | Reaction time | |
| Low-intensity physical activity* | Response latency | |
| Light-intensity lifestyle | Accuracy | |
| Light-intensity exercise | Attention | |
| Low-intensity exercise | Task switching | |
| Problem solving | ||
| Decision making | ||
| Multitasking | ||
| Planning | ||
| Reasoning | ||
| Comprehension | ||
| Spatial memory | ||
| Episodic memory | ||
| Long-term memory | ||
| Declarative memory | ||
| Intelligence | ||
| Neurocognition | ||
| Neurocognitive | ||
| Neuro-cognition | ||
| Neuro-cognitive | ||
| Attentiveness | ||
| Concentration | ||
| Concentrate | ||
| Information retrieval | ||
| Information processing | ||
| Perceptual skills |
Note: “*” used as wildcard character to search for all phrases which included the truncated term.
Study Selection
Original research studies using any research design (ie, intervention or observational) were eligible for inclusion. The inclusion criteria were the following: (i) include device-based or technologically measured LPA categorized by one of the following American College of Sports Medicine (ACSM) definitions of “very light” or “light” relative intensity: <37–45% maximal oxygen uptake (VO2max); <30–39% heart rate reserve (HRR) or % VO2 reserve; <57–63% HRR (23) OR accelerometer-classified LPA, (ii) include at least one validated behavioral cognitive performance measure, (iii) directly examine an association between LPA and cognitive outcomes, (iv) use an adult (18+) sample, and (v) an original research study of either acute (defined as a single isolated bout of LPA), randomized control trial (RCT), cross-sectional or longitudinal design.
Exclusion criteria included the following: (i) cognitive function used as a screening measure and not an outcome variable, (ii) structural or functional brain outcomes (measured via MRI, fMRI, ECG, PET scans, etc.) as the only outcomes reported, (iii) use of self-report LPA as the exposure variable, (iv) not a full peer-reviewed article (ie, conference abstract, thesis), (v) clinical psychological conditions (ie, depression, anxiety) as cognitive outcomes, (vi) LPA designated as a control condition, and (vii) use of animal models. Arksey and O’Malley (20) suggested that search criteria in scoping reviews be amendable to allow for additional criteria to be added once greater familiarity with the field was reached.
The first author (E.E.) conducted the searches and, after duplicates were removed, eliminated articles based on irrelevance of titles and abstracts. Full texts were then retrieved and read to determine basis for inclusion. For articles that did not clearly fit within, or outside of, the search criteria, E.E. and N.G. met to discuss their eligibility. If a consensus could not be reached regarding their status for inclusion, E.M. was consulted to resolve the disagreement. After reviewing all the potentially eligible articles, an additional eighth exclusion criterion of “LPA assessed in experimental/extraordinary conditions” was added. This was to ensure that the only articles included in the review reflected LPA which is engaged in during routine, everyday life. The study selection process is detailed in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram found in Figure 1.
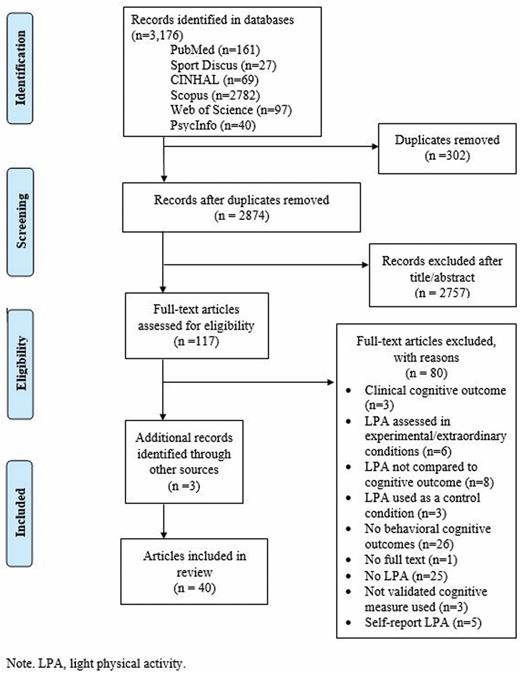
PRISMA flow diagram of study selection process. LPA = light physical activity.
Charting the Data
Data from all identified studies were extracted using Mendeley Desktop (Version 1.19.4) and Excel. The following data were extracted from each article: first author, year, study design, sample characteristics (mean sample age, gender percentage breakdown, and population characteristics), how LPA was monitored during study period, definition of LPA, cognitive domain(s) assessed, cognitive assessments used, and LPA-specific study findings. The following data were also extracted from relevant studies: time point(s) of data collection (intervention, longitudinal); accelerometer data reduction details (cross-sectional, longitudinal), length/frequency of LPA bouts (acute, intervention); population metrics of LPA, MVPA, and sedentary time (cross-sectional, longitudinal). Reported covariates used in analysis were also recorded.
The fifth and final step of the 5-stage methodological framework, “collating, summarizing, and reporting the results” (20) is detailed in the following sections.
Results
Articles Retrieved
All searches were conducted between January and June 2020 by E.E. with assistance from the college librarian. The initial search yielded 3176 hits, with 2874 titles remaining after duplicates were removed. Next, all titles and abstracts were examined for relevance. After removing 2757 irrelevant hits, 117 articles were reviewed in their entirety and screened for inclusion and exclusion criteria. Eighty articles were excluded for reasons listed in the PRISMA flow (Figure 1). The reference lists of the remaining articles were scanned, yielding 3 more articles.
Article Characteristics
Among the reviewed articles, study designs ranged from: n = 14 acute LPA; n = 4 RCTs; n = 18 cross-sectional; and n = 4 longitudinal. Overall, 32.5% (n = 13) studies examined LPA among young adults (age range 19.1–27.8 years), 25% (n = 10) examined middle-aged adults (age range 35.7–64.78 years), and 45% (n = 18) examined older adults (aged 65 years and older). N = 1 study was comprised of both young and older adults. N = 32 (80%) studies utilized nonclinical, healthy populations. All studies examined either memory (episodic, semantic, and working subdomains), attention/processing speed, executive functioning and/or global cognitive status. The cognitive assessments used are listed in Supplementary Table 1.
Acute Studies Examining LPA
A summary of the 14 acute studies can be found in the Supplementary Material (Supplementary Table 2). Overall, 7 (50%) of studies reported at least one significant outcome between the LPA condition and a cognitive domain (24–30). Among these 7 studies, 5 reported associations with executive function (24,26–28,30), 1 reported an association with memory (25), and 1 reported an association with attention (29).
Across all 14 acute studies, 4 measured cognitive performance immediately after the LPA bout. Only 2 found significant pre–post improvements in attention and task-switching performance (27,28). Notably, the 2 studies which reported insignificant associations also measured attention and executive functioning performance (24,31). Among the 5 studies which administered cognitive assessments after a delayed period, 4 reported significant associations among the LPA groups with executive function (24,26,30) and episodic memory (25). Among the 6 studies which administered cognitive assessments during the exercise bout, only 1 study reported significant, positive associations with selective and sustained attention (29).
Overall, 11 studies used young adult samples (mean age range 20.01–27.8; 24–28,32–37), 2 used middle-aged adults (mean age range 35.7–40.2; 29,30) and 1 study included a sample of both young and older adults (mean age 21.8 and 65.5 years, respectively; 31). Two studies were randomized trials (24,35), and the rest utilized a repeated measures study design.
Randomized Control Trials
Four RCTs met the inclusion criteria and are summarized in Supplementary Table 3. Overall, 3 studies (75%) observed that the LPA experimental group significantly increased in at least one cognitive outcome score, including increased processing speed (38), short-term memory (39) and improvements among the attention/concentration, short-term memory and higher cognitive functioning subscales on the Strub and Black Mental status test (40).
The mean age of the study samples was between 60 and 64 years. Two studies included healthy populations (40,41) and the other 2 studied stroke survivors (38,39). Three studies were composed of group-based exercise classes (39–41); 1 study did not clearly distinguish the intervention delivery (38). Only 2 studies reported controlling for covariates in analyses (40,41), which included age, sex, marital status, years of education, and depression.
Cross-sectional Studies
Eighteen cross-sectional studies were included in this review and are summarized in Supplementary Table 4. Overall, 10 studies (55.55%) found LPA to be significantly associated with one or more cognitive outcomes. Six studies found LPA to be significantly, positively associated with executive functioning (42–47); 2 studies found significant, positive associations with attention/processing speed (45,48); 1 study found significant, positive associations with working memory (42); and 3 studies found significant, positive associations with global cognitive status (49–51).
Study sample sizes varied from 72 to 7098 participants. Fourteen included healthy adult samples (42–44,46–56) and 5 studied clinical populations including adults diagnosed with peripheral arterial disease (57), adults diagnosed with schizophrenia (48), older adults with cognitive impairments (45,58) and postmenopausal breast cancer survivors (59). One study included both clinical and nonclinical populations (48). Only one study sampled young adults (mean age 19.1 years; 46), with the remaining studies examining middle aged to older adult populations (mean age range 41.1–88.0). All studies reported LPA and MVPA metrics obtained from accelerometers. The average amount of LPA was 264.22 minutes/day (SD = 119.87), and values ranged from 47.5 to 550.6 minutes/day. The average minutes of MVPA per day was 41.98 (SD = 33.75). Only 10 studies reported sedentary time (42,43,49–54,56,59), which averaged 583.27 minutes/day (SD = 100.49). Sixteen studies reported covariates incorporated into analyses (42–46,48–52,54–59) including demographics, health behaviors, health status, and accelerometer wear time. Twelve studies specifically included covariates of physical activity and/or cognitive status in their analyses (42–44,49–52,54–56,59,60).
Longitudinal Studies
Four longitudinal studies, summarized in Supplementary Table 5, were eligible for inclusion and were composed of sample sizes ranging from 15 to 6452 participants. Overall, 2 studies (50%) found significant associations between accelerometer-measured LPA and cognitive outcomes. One study reported that baseline LPA was predictive of reduced rate of cognitive decline 2 years later (61). The second study reported LPA, which was assessed every month for 4 months, to be significantly correlated with general intelligence and attention (62). Additionally, average LPA engaged in over the 4-month observation period was significantly correlated with attention performance scores at the final, fourth month assessment period.
Three studies included healthy, older adult populations (mean age range 66–74.52; 60–63) and one study examined a small sample (n = 15, mean age 78 years) of older adults diagnosed with cerebrovascular disease (62). All studies assessed LPA at baseline, with average LPA engagement at 199.25 minutes/day (SD = 104.16) and average MVPA engagement at 15.75 minutes/day (SD = 18.17). Follow-up time points ranged from 4 months to 5 years; however, only 2 studies administered accelerometers at both baseline and follow-up (60,62). Average LPA measured at final follow-up time points among the 2 studies was 208.07 minutes/day (SD = 44.14) and average MVPA was 14.87 minutes/day (SD = 10.71). Only 2 studies reported daily sedentary time (62,63) with one study (62) including sleep time in this metric. Notably, only one study included MVPA in analyses as a simultaneous predictor of cognitive outcomes (61).
Discussion
To our knowledge, this is the first scoping review to document the existing evidence from studies examining the direct associations between LPA and cognition. Overall, there is no consistent trend among the 40 reviewed studies, with mixed results for both acute and long-term LPA engagement and its effects on cognitive functions.
Acute exercise has been widely recognized for its short-term improvements on cognitive performance (64). Across the reviewed studies the length of LPA bout ranged between 5.5 and 30 minutes. This in addition to the design parameters such as intensity, mode of exercise, type, and timing of cognitive task administration may have influenced the results (65), making it difficult to compare studies and ascertain acute LPA’s influence on cognition. A previous meta-analysis (65) on the cognitive benefits of acute exercise found that when cognition was assessed during exercise, exercise intensity did not have a significant effect on performance. This was echoed in the current review, where 5 out of 6 studies administering assessments during the LPA bout reported no significant associations with cognitive outcomes. However, among studies where cognition was tested after an acute LPA bout the findings were mixed. The aforementioned meta-analysis (65) suggested that lighter intensity exercise may show cognitive associations when assessments are administered immediately after exercise, possibly due to activation of the “appropriate level of physiological mechanism[s]” (65) to facilitate improved cognitive performance. The study authors also reported significant effect sizes for the effects of an acute bout of LPA on cognition during exercise (d = 0.092), immediately after exercise (d = 0.169), and after a delay (d = 0.245; 65). These small effect sizes provide one possibility for the discrepancy among the results of our current studies, suggesting some studies may have been underpowered.
While a majority (3 out of 4) of the reviewed RCTs reported positive, significant associations between the LPA arm and one or more cognitive outcomes, there were several significant shortcomings in the study designs. None of the studies controlled for participants’ fitness levels or physical activity engagement prior to the study, one had an ambiguous classification of the light-intensity exercise arm (41), and all studies were composed of smaller sample sizes (ranging from 35–72 participants). Additionally, only 4 RCTs were eligible for inclusion, as these studies reported the specific intensity set for their LPA-arm. Previous systematic reviews and meta-analyses of RCTs have noted a consistent lack of intensity dosage reporting among exercise RCTs (66,67). Thus, it is possible more RCTs have been conducted utilizing LPA-based intervention arms. However, by failing to accurately document the intensity of exercise, independent effects of LPA and MVPA cannot be distinguished and thereby potential LPA effects may go undetected.
The nature of cross-sectional study designs likely contributed to these inconsistent findings reported among the reviewed studies, due to the inability to infer causality and establish temporality between the outcome and exposure. Such limitations can only be overcome via more rigorous interventions and RCTs. Additionally, numerous inconsistent study designs and measurements were present among the reviewed studies, including health status of participants (4 studies included clinical populations), varied sample sizes, accelerometer data processing approaches, cognitive assessments administered and outcomes reported, covariates included in analyses, and statistical approaches.
While 2 of the 4 included longitudinal studies observed positive, significant associations between LPA engagement (at one or more time points) and cognitive functioning, all studies had notable limitations. These included high attrition rates (60), small sample sizes (62), and potential practice effects on cognitive assessments (62). Additionally, 2 studies (61,63) only collected physical activity at baseline, and these activity levels were regressed onto changes in cognitive scores from baseline to follow-up. Thus, it is uncertain if participants experienced any changes in physical activity over the observation period and how these changes may have impacted their cognitive scores.
Need to Account for Aerobic Fitness and MVPA Engagement
No studies in the present review included participants’ aerobic fitness as a covariate. This is surprising given the strong and consistent association of aerobic fitness with cognitive function (68,69). Controlling for this variable is especially important in acute and cross-sectional studies which conduct between-subject analyses. Including and controlling for aerobic fitness is important to establish with certainty that any significant differences observed in cognitive function are a result of participants’ LPA participation and not due to unaccounted internal factors (ie, aerobic fitness level).
Only 10 observational studies (9 cross-sectional and 1 longitudinal) included MVPA as a simultaneous predictor in their statistical models. While MVPA is not a validated direct proxy for aerobic fitness, this variable provides insight into LPA’s association with cognition after controlling for engagement in higher intensity activities. The fact that only 53% of the included observational studies accounted for MVPA engagement suggests that the current state of the field may not be fully capturing, and controlling for, all the significant physical activity and subsequent aerobic fitness cognitive predictors. This inconsistency may partly explain the heterogeneous findings of LPA’s association with cognition. It is worth noting, however, that no clear trends emerged between studies which did and did not control for MVPA among their results.
LPA Measurement Methodologies and Reporting
Despite the formal classification of LPA as activity with an energy expenditure between 1.6 and 2.9 METs and methods of estimating this intensity recommended by ACSM (23), operationalization of “light-intensity” activity in physical activity research has widely varied (70). As greater interest continues to emerge regarding the overall independent health benefits of LPA, this inconsistent classification may lead to studies being incorrectly excluded or included in future analyses and reviews. Norton and colleagues (70) have emphasized a need for more consistent terminology regarding exercise intensity, and this is evident across studies which have inaccurately used the term “light-intensity” (71,72).
Additionally, among cross-sectional and longitudinal studies which utilized accelerometers, the data collection and processing methods varied greatly. Some of this variation is due to the selection of cut points validated for specific populations, age groups, or device placement; however, all but 2 of studies included in this review used a waist-based wear protocol. Additionally, even among studies which examined similar populations the selected cut points varied. The most frequently used device cut-off to classify LPA across the reviewed observational studies was by Freedson and colleagues (≤1951 counts/min; 73). However, all studies reported using validated cut-offs to classify LPA. Counts-based classification was most widely used (16 studies), followed by device-calculated MET cutoffs (3 studies) and device-based intensity level classification (2 studies). It has been recently emphasized that due to the variety of decision points researchers face when using accelerometers and the frequent reliance on proprietary intensity-calculation algorithms produced by commercially available devices, the research community is limited in the extent to which accelerometer data for LPA can be compared and reproduced between studies (74).
Hypothesized Underlying Mechanisms
The acute and long-term physiological mechanisms underpinning LPA’s influence on cognitive function have not been widely investigated. Soya and colleagues (75) previously found that rodents who ran at a “mild intensity” (defined as sub-lactic threshold) for 30 minutes exhibited greater activation in the CA1 and dentate gyrus regions of the hippocampus and greater levels of brain-derived neurotrophic factor mRNA across hippocampal sub regions. Brain-derived neurotrophic factor plays a significant role in upregulating synaptic plasticity (76) and neurogenesis (77), especially in the hippocampal region, which can translate to improved cognitive functioning (76). Another study (25) found that healthy young adults who completed a 10-minute bout of light intensity cycling exhibited increased functional connectivity between hippocampal (dentate gyrus/CA3 regions) and cortical (para-hippocampal, angular, and fusiform gyri) regions, and this increase was predictive of increased episodic memory performance.
It is also possible LPA may indirectly affect cognition via upregulating peripheral metabolic pathways. For example, a previous study (78) found that an 8-week low-intensity walking program improved plasma lipid metabolism among sedentary, middle-aged adults. Impaired lipid metabolism has been associated with cognitive decline and increased risk for neurodegenerative diseases (79). LPA has also been suggested to help regulate blood glucose levels (11). Elevated blood glucose levels are linked to risk of Type 2 diabetes and cardiovascular disease, both of which are significant predictors of impaired cognitive function and risk of neurodegenerative diseases (80,81).
LPA may also affect cognition via displacement of sedentary behavior, which has been previously investigated for its own independent, detrimental cognitive associations (82). High levels of prolonged sedentary behavior may reduce cerebral blood flow (83), disrupt glucose and lipid metabolism (84,85) and increase risk for metabolic syndrome (86)—all factors associated with compromised cognitive functioning. A previous study (83) found that disrupting prolonged (4 hours) sitting with short, frequent light-intensity walking breaks (2-minute breaks every 30 minutes) attenuated decreases in cerebral blood flow observed in the uninterrupted sitting group. Additional intervention studies have demonstrated physiological benefits of breaking up prolonged sitting with light-intensity walking breaks (87–89), albeit most have been conducted on overweight/obese participants.
Lastly, Iso-Markku and colleagues (49) found significant, independent associations between both sedentary behavior and LPA with cognition among a twin cohort. However, these associations were only observed in between-family linear analyses (ie, between different sets of twins), leading the authors to hypothesize that the influence of LPA and sedentary behavior on cognition may be due to “genetic selection and environmental similarity between siblings” (49).
Limitations
Given that this was a scoping review, the literature selection and review process was not subjected to the extensively rigorous methodology that is a typical component of systematic reviews or meta-analyses. However, systematic reviews are typically conducted after such “scoping endeavors” have already mapped out the general trends of the field to date, in order to answer specific questions using studies selected from a very narrow search criteria (20). Thus, the intent of the present work was to capture all LPA-cognition related studies to better understand the current state of the field and which direction(s) may be the most promising to pursue. Thus, not adhering to the “systematic” approach is not particularly a limitation. That being said, because scoping reviews are intended to be broad and all-encompassing, we did not dissect differences of association among populations, age groups or cognitive domains. These specific research questions would be more appropriate for a future systematic review or a meta-analysis.
Conclusion
In order to further our understanding of the potential independent health contributions of LPA, especially in the context of cognitive function, the following considerations are recommended for future research studies:
More rigorous RCTs using LPA as the primary intervention arm. This also includes clearly defined intensity parameters for LPA and fidelity checks during the interventions to ensure participants are adhering to the prescribed intensity.
Incorporate aerobic fitness and MVPA engagement as a covariate in analyses, to understand if individuals of varying aerobic fitness levels and physical activity habits respond differently to LPA.
Design studies with greater power (ie, larger sample sizes) to detect potential small effect sizes.
Determine whether displacing sedentary behavior with LPA results in significant cognitive gains.
Currently, the research supporting the association between LPA and cognition is equivocal and future research in this area will necessitate studies of sufficient methodological rigor to determine the efficacy of this relationship. In this scoping review, we have detailed the existing evidence, identified gaps and issues that must be addressed in order to further our knowledge, and provided suggestions for future research. Given that most individuals can easily engage in LPA, determining its potential as an independent behavior to maintain or improve cognitive functions becomes an important public health goal.
Acknowledgment
The authors would like to thank the UIUC Applied Health Sciences librarian for assistance with search string development.
Funding
None declared.
Author Contributions
E.E.: scoping review conception, search string development, assessment of articles for eligibility, data extraction, and manuscript writing; E.M.: manuscript writing and review; N.G.: scoping review conception, assessment of full-text articles for eligibility, and manuscript writing and review.
Conflict of Interest
None declared.



