-
PDF
- Split View
-
Views
-
Cite
Cite
Giovanni Francesco Marangi, Luca Savani, Marco Gratteri, Lucrezia Arcari, Francesco Segreto, Barbara Cagli, Annalisa Cogliandro, Raffaella Vega, Carlo Mirra, Paolo Persichetti, Main Factors Influencing Patient Satisfaction After Primary Breast Augmentation: A Prospective Study Based on Patient-Reported Outcome Measures, Aesthetic Surgery Journal, Volume 44, Issue 4, April 2024, Pages 375–382, https://doi.org/10.1093/asj/sjad372
Close - Share Icon Share
Abstract
Primary breast augmentation is one of the most sought-after procedures in cosmetic surgery. It is generally related to a high degree of patient satisfaction, but it is not always obvious which factors have greater influence on patient satisfaction.
The aim of this prospective study was to evaluate how anthropometric, psychological, and social parameters, in association with the main surgical variables, influenced patients’ satisfaction with their breasts after surgery.
Patients undergoing primary breast augmentation between October 2018 and February 2022, who completed a 12-month follow-up without complications, were enrolled in the study. For each patient we recorded: BMI, pinch test (upper pole of the breast), surgical access, implant pocket, implant volume, bra size increase, age, smoking habit, civil status, education level, pregnancies, and psychiatric disorders. Each variable was statistically correlated with patient’s satisfaction, assessed by BREAST-Q questionnaire preoperatively and 12 months postoperatively.
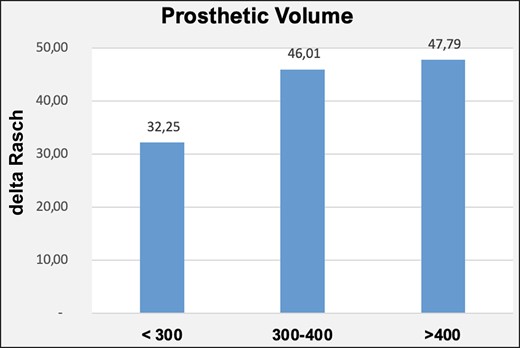
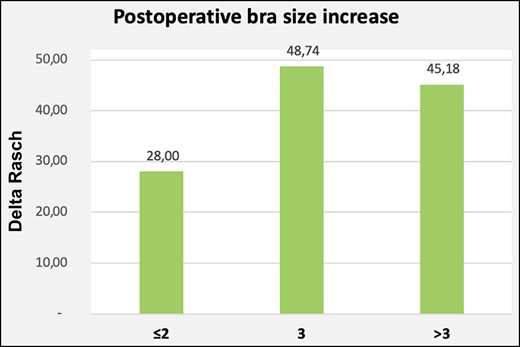
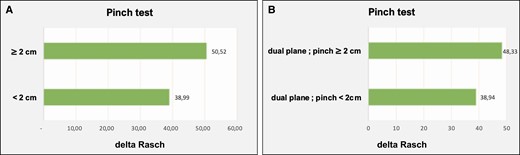
Analyzing the data of the 131 patients, we found 3 factors affecting their satisfaction (P<.05); BMI: underweight patients were less satisfied than normal and overweight patients; pinch test: patients with a pinch test >2 cm were more satisfied; volume of the implant and bra size increase: patients with implant volume <300 cc and a less than 2 bra size increase were less satisfied than patients with larger augmentation.
BMI, pinch test, implant volume, and extent of volumetric enhancement should be taken into careful consideration by the surgeon during preoperative consultation and surgical planning, because they can be critical to patient satisfaction.

The shape and the size of the breasts have always been a primary attribute of feminine attractiveness. For this reason, breast augmentation surgery is generally related to a very high degree of patient satisfaction, and it is one of the most sought-after procedures in cosmetic surgery.1-5
Patient satisfaction is probably our main goal as aesthetic surgeons. This is the result of many factors; patient expectations, analysis of patients’ characteristics, and meticulous planning of the surgery are of paramount importance to achieve a good result. Much effort is made to understand the desires of the patient, such as discussing preoperative and postoperative pictures, trying sizers, or using augmented reality software to simulate the expected result.
The factors that, in the surgeon's opinion, may influence the outcome of breast augmentation have been thoroughly discussed in the literature, whereas the patients’ perspective has been relatively less investigated.3,6-9 The aim of this prospective study was to further evaluate how primary breast augmentation can affect patient satisfaction and, in particular, how the anthropometric, psychological, and social parameters of patients undergoing primary breast augmentation, in association with the main surgical variables, influenced patients’ satisfaction with their breasts after the surgery.
METHODS
Study Population
All the patients who underwent primary breast augmentation by the same surgeon at our hospital between February 2019 and February 2022 were enrolled in the study. Patients who received concomitant ancillary procedures (eg, lipofilling to the breast, breast reshaping, etc), or had previous surgeries to the breast, were excluded. For each patient, the following factors were recorded: BMI, pinch test at the upper pole of the breast, surgical access (inframammary fold and lower hemiperiareolar were the 2 methods of access), implant pocket (either dual-plane or subglandular pockets), volume of the implant in cc, breast volume increase by bra size, age, smoking habit, civil status, level of education, pregnancies, and psychiatric disorders.
Patients were reviewed after the surgery at 1, 2, and 4 weeks and 3, 6, and 12 months. We considered 12 months the proper period of time for the healing process to be completed. Patients who did not complete the entire follow-up were excluded, as were those who developed any kind of complication (hematoma, seroma, infection, wound dehiscence, implant malposition, rippling, capsular contracture, waterfall deformity, or implant rupture) during the time of the study. Indeed, our purpose was not to assess the influence of the aforementioned factors on the complication rate, but rather to understand their impact on patient satisfaction after an ideal postoperative course. To evaluate patient satisfaction, an anonymous BREAST-Q 2.0 questionnaire (Augmentation module, Satisfaction with breasts scale) was administered 1 week preoperatively and 12 months after the surgery by a surgeon who did not participate in the surgeries or the follow-up.10-12
Preoperative Planning and Surgical Technique
The choice between anatomical and round implants was mainly left to the patient, despite recommendation by the surgeon in accordance with patient features. Patients could try sizers during the consultation, to visualize the expected increase in breast volume. No 3-dimensional simulation was utilized. According to the breast base and the physical characteristics of the patient, a small range of implants was chosen, and the proper one was selected after trying sizers intraoperatively. MENTOR microtextured breast implants were placed in all cases (MENTOR, Santa Barbara, CA).We utilized inframammary or lower hemiperiareolar access, primarily depending on patient preference, despite recommendation by the surgeon in accordance with patient features; no other types of access were implemented. The dual-plane technique was performed in all the patients with a pinch test at the upper pole of the breast of less than 2 cm; when the pinch test was higher, the choice between dual-plane and subglandular pocket was mainly left to the patient, after explaining all the advantages and drawbacks. Overall, the dual-plane technique was carried out in 87.79% of patients, and the subglandular method in 12.21%. No total submuscular or subfascial planes were employed.
Statistical Analysis
The results of the questionnaire, as well as the demographic data of the sample, were aggregated, made anonymous and imported into an Excel database after each survey. The summation of the scores of each patient was converted to a 0 to 100 point scale (the Rasch scale) to make the data as comparable as possible.10,13
Before analyzing each parameter individually, the preoperative and postoperative scores obtained from the BREAST-Q 2.0 Satisfaction with breasts module of all 131 patients were averaged. We performed a Shapiro-Wilk test to assess normality of the scores. Bivariate analysis was then performed with Prism 9 (GraphPad Software, Boston, MA). Results were presented as delta mean ± standard deviation. Statistical significance of data was assessed with a t test for variables with 2 modalities (ie, smoking habit: yes/no) and with the ANOVA (analysis of variance) test for variables with 3 modalities (ie, BMI: underweight, normal weight, overweight). Differences were considered statistically significant at P < .05. Furthermore, for a significant ANOVA test post hoc analysis was performed.
The study was conducted in accordance with local regulations, international standards of “good clinical practice” in the European Community and the principles of the Declaration of Helsinki. All patients signed a written informed consent. This study was approved by the institutional review board of Campus Bio-Medico University Hospital, Rome, Italy.
RESULTS
One hundred fifty-five patients were enrolled in the study. Six of them were excluded after developing complications during the postoperative period (1 hematoma, 1 delay of wound healing, 2 implant malpositions, 2 rippling, 1 capsular contracture); 17 did not complete the 1-year follow-up. Therefore, data from 131 patients were analyzed. Patients’ ages ranged between 18 and 63 years (<30 years 29%; 30-40 years 59.54%; >40 years 11.45%). All the patients were female.
The preoperative mean value of satisfaction with the breasts was 33.62 ± 14.52, the postoperative value was 77.98 ± 14.12; the difference between these was statistically significant (P<.0001).
Results are shown in Table 1. Age, smoking habit, previous pregnancies, marital status, education, psychological disorders, surgical access, and type of implants did not show a statistically significant correlation with the delta between the postoperative Rasch values and the preoperative values (P > .05).
| Variables . | Delta mean . | Delta SD . | P value . |
|---|---|---|---|
| BMI | |||
| Underweight | 35.27 | ± 18.42 | .009340733 |
| Normal range | 45.48 | ± 17.37 | |
| Overweight | 52.05 | ± 23.58 | |
| Pinch test | |||
| <2 cm | 38.99 | ± 17.29 | .00043106 |
| ≥2 cm | 50.52 | ± 19.26 | |
| Age | |||
| <30y | 47.29 | ± 20.81 | .458315582 |
| 30-40y | 42.68 | ± 17.01 | |
| ≥40y | 45.67 | ± 24.40 | |
| Smoking habit | |||
| No | 42.72 | ± 19.99 | .174808939 |
| Yes | 47.49 | ± 16.90 | |
| Access site | |||
| Inframammary | 46.97 | ± 18.72 | .364843832 |
| Hemiperiareolar | 43.48 | ± 20.09 | |
| Previous pregnancies | |||
| No | 43.18 | ± 21.09 | .400682422 |
| Yes | 46.04 | ± 15.75 | |
| Marital Status | |||
| Single | 42.6 | ± 21.37 | .243977757 |
| Married | 46.51 | ± 15.70 | |
| Higher education | |||
| Yes | 44.33 | ± 19.18 | .952490373 |
| No | 44.75 | ± 18.30 | |
| Psychological disorder | |||
| No | 44.92 | ± 19.53 | .217501903 |
| Yes | 36.78 | ± 7.87 | |
| Type of Prosthesis | |||
| Round | 42.75 | ± 19.18 | .234164182 |
| Anatomical | 46.81 | ± 18.78 | |
| Prosthetic Volume, cc | |||
| <300 | 32.25 | ± 17.62 | .006876244 |
| 300-400 | 47.79 | ± 19.68 | |
| >400 | 46.01 | ± 18.16 | |
| Delta bra size | |||
| ≤1 | 28 | ± 16.35 | .007778351 |
| >1-2 | 48.74 | ± 19.52 | |
| >2 | 45.18 | ± 18.46 | |
| Dual plane + pinch < 2cm | 38.94 | ± 17.27 | .007101555 |
| Dual plane + pinch ≥ 2 cm | 48.33 | ± 18.89 | .128187307 |
| Subglandular | 56.87 | ± 19.38 |
| Variables . | Delta mean . | Delta SD . | P value . |
|---|---|---|---|
| BMI | |||
| Underweight | 35.27 | ± 18.42 | .009340733 |
| Normal range | 45.48 | ± 17.37 | |
| Overweight | 52.05 | ± 23.58 | |
| Pinch test | |||
| <2 cm | 38.99 | ± 17.29 | .00043106 |
| ≥2 cm | 50.52 | ± 19.26 | |
| Age | |||
| <30y | 47.29 | ± 20.81 | .458315582 |
| 30-40y | 42.68 | ± 17.01 | |
| ≥40y | 45.67 | ± 24.40 | |
| Smoking habit | |||
| No | 42.72 | ± 19.99 | .174808939 |
| Yes | 47.49 | ± 16.90 | |
| Access site | |||
| Inframammary | 46.97 | ± 18.72 | .364843832 |
| Hemiperiareolar | 43.48 | ± 20.09 | |
| Previous pregnancies | |||
| No | 43.18 | ± 21.09 | .400682422 |
| Yes | 46.04 | ± 15.75 | |
| Marital Status | |||
| Single | 42.6 | ± 21.37 | .243977757 |
| Married | 46.51 | ± 15.70 | |
| Higher education | |||
| Yes | 44.33 | ± 19.18 | .952490373 |
| No | 44.75 | ± 18.30 | |
| Psychological disorder | |||
| No | 44.92 | ± 19.53 | .217501903 |
| Yes | 36.78 | ± 7.87 | |
| Type of Prosthesis | |||
| Round | 42.75 | ± 19.18 | .234164182 |
| Anatomical | 46.81 | ± 18.78 | |
| Prosthetic Volume, cc | |||
| <300 | 32.25 | ± 17.62 | .006876244 |
| 300-400 | 47.79 | ± 19.68 | |
| >400 | 46.01 | ± 18.16 | |
| Delta bra size | |||
| ≤1 | 28 | ± 16.35 | .007778351 |
| >1-2 | 48.74 | ± 19.52 | |
| >2 | 45.18 | ± 18.46 | |
| Dual plane + pinch < 2cm | 38.94 | ± 17.27 | .007101555 |
| Dual plane + pinch ≥ 2 cm | 48.33 | ± 18.89 | .128187307 |
| Subglandular | 56.87 | ± 19.38 |
BMI, body mass index; SD, standard deviation.
| Variables . | Delta mean . | Delta SD . | P value . |
|---|---|---|---|
| BMI | |||
| Underweight | 35.27 | ± 18.42 | .009340733 |
| Normal range | 45.48 | ± 17.37 | |
| Overweight | 52.05 | ± 23.58 | |
| Pinch test | |||
| <2 cm | 38.99 | ± 17.29 | .00043106 |
| ≥2 cm | 50.52 | ± 19.26 | |
| Age | |||
| <30y | 47.29 | ± 20.81 | .458315582 |
| 30-40y | 42.68 | ± 17.01 | |
| ≥40y | 45.67 | ± 24.40 | |
| Smoking habit | |||
| No | 42.72 | ± 19.99 | .174808939 |
| Yes | 47.49 | ± 16.90 | |
| Access site | |||
| Inframammary | 46.97 | ± 18.72 | .364843832 |
| Hemiperiareolar | 43.48 | ± 20.09 | |
| Previous pregnancies | |||
| No | 43.18 | ± 21.09 | .400682422 |
| Yes | 46.04 | ± 15.75 | |
| Marital Status | |||
| Single | 42.6 | ± 21.37 | .243977757 |
| Married | 46.51 | ± 15.70 | |
| Higher education | |||
| Yes | 44.33 | ± 19.18 | .952490373 |
| No | 44.75 | ± 18.30 | |
| Psychological disorder | |||
| No | 44.92 | ± 19.53 | .217501903 |
| Yes | 36.78 | ± 7.87 | |
| Type of Prosthesis | |||
| Round | 42.75 | ± 19.18 | .234164182 |
| Anatomical | 46.81 | ± 18.78 | |
| Prosthetic Volume, cc | |||
| <300 | 32.25 | ± 17.62 | .006876244 |
| 300-400 | 47.79 | ± 19.68 | |
| >400 | 46.01 | ± 18.16 | |
| Delta bra size | |||
| ≤1 | 28 | ± 16.35 | .007778351 |
| >1-2 | 48.74 | ± 19.52 | |
| >2 | 45.18 | ± 18.46 | |
| Dual plane + pinch < 2cm | 38.94 | ± 17.27 | .007101555 |
| Dual plane + pinch ≥ 2 cm | 48.33 | ± 18.89 | .128187307 |
| Subglandular | 56.87 | ± 19.38 |
| Variables . | Delta mean . | Delta SD . | P value . |
|---|---|---|---|
| BMI | |||
| Underweight | 35.27 | ± 18.42 | .009340733 |
| Normal range | 45.48 | ± 17.37 | |
| Overweight | 52.05 | ± 23.58 | |
| Pinch test | |||
| <2 cm | 38.99 | ± 17.29 | .00043106 |
| ≥2 cm | 50.52 | ± 19.26 | |
| Age | |||
| <30y | 47.29 | ± 20.81 | .458315582 |
| 30-40y | 42.68 | ± 17.01 | |
| ≥40y | 45.67 | ± 24.40 | |
| Smoking habit | |||
| No | 42.72 | ± 19.99 | .174808939 |
| Yes | 47.49 | ± 16.90 | |
| Access site | |||
| Inframammary | 46.97 | ± 18.72 | .364843832 |
| Hemiperiareolar | 43.48 | ± 20.09 | |
| Previous pregnancies | |||
| No | 43.18 | ± 21.09 | .400682422 |
| Yes | 46.04 | ± 15.75 | |
| Marital Status | |||
| Single | 42.6 | ± 21.37 | .243977757 |
| Married | 46.51 | ± 15.70 | |
| Higher education | |||
| Yes | 44.33 | ± 19.18 | .952490373 |
| No | 44.75 | ± 18.30 | |
| Psychological disorder | |||
| No | 44.92 | ± 19.53 | .217501903 |
| Yes | 36.78 | ± 7.87 | |
| Type of Prosthesis | |||
| Round | 42.75 | ± 19.18 | .234164182 |
| Anatomical | 46.81 | ± 18.78 | |
| Prosthetic Volume, cc | |||
| <300 | 32.25 | ± 17.62 | .006876244 |
| 300-400 | 47.79 | ± 19.68 | |
| >400 | 46.01 | ± 18.16 | |
| Delta bra size | |||
| ≤1 | 28 | ± 16.35 | .007778351 |
| >1-2 | 48.74 | ± 19.52 | |
| >2 | 45.18 | ± 18.46 | |
| Dual plane + pinch < 2cm | 38.94 | ± 17.27 | .007101555 |
| Dual plane + pinch ≥ 2 cm | 48.33 | ± 18.89 | .128187307 |
| Subglandular | 56.87 | ± 19.38 |
BMI, body mass index; SD, standard deviation.
Statistically significant correlations were observed for the modalities related to BMI, prosthetic volume, delta bra size, and pinch test (P < .05). Data regarding statistically significant changes are shown in Figures 1-4.
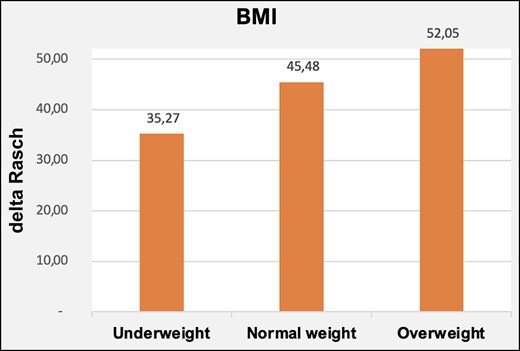
The average value of the delta of BREAST-Q was 35.27 for underweight patients, 45.48 for normal weight patients, and 52.05 for overweight patients. The post hoc results showed that the statistical significance was related to the variation of preoperative and postoperative BREAST-Q values obtained from underweight patients, while no significant differences were found between normal weight and overweight patients.
By studying the results of the ANOVA test relating to the delta bra size, the average delta Rasch value was 28 for an increase in size less than or equal to 2; 48.74 for an increase of 3 sizes; and 45.18 for an increase of more than 3 sizes. The statistical significance was related to the delta Rasch value obtained from patients who obtained a volumetric increase of the breast ≤ 2 sizes, as shown by the post hoc analysis. On the other hand, no significant differences were found between patients with volumetric increase between 2 and 3 sizes and patients with an increase > 3 sizes.
For volume of the implant, an average delta Rasch value of 32.25 was obtained for patients with a volume less than 300 cc, 46.01 for a volume between 300 and 400 cc, and 47.79 for a volume greater than 400 cc. The post hoc results showed that the delta Rasch value obtained from patients with a volume of less than 300 cc was significantly different from the respective values of the remaining study population. When comparing patients with a volume between 300 and 400 cc and patients with a volume greater than 400 cc, however, no statistically significant differences emerged in the delta Rasch value. Post hoc analysis results are shown in Table 2.
| BMI . | Underweight-normal weight . | Underweight-overweight . | Normal weight-overweight . |
|---|---|---|---|
| P value | .011 | .011 | .174 |
| Delta bra size | ≤2 | >2-3 | >3 |
| P value | .005 | .004 | .412 |
| Prosthetic volume, cc | <300 | 300-400 | >400 |
| P value | .003033 | .005562 | .64703 |
| BMI . | Underweight-normal weight . | Underweight-overweight . | Normal weight-overweight . |
|---|---|---|---|
| P value | .011 | .011 | .174 |
| Delta bra size | ≤2 | >2-3 | >3 |
| P value | .005 | .004 | .412 |
| Prosthetic volume, cc | <300 | 300-400 | >400 |
| P value | .003033 | .005562 | .64703 |
BMI, body mass index.
| BMI . | Underweight-normal weight . | Underweight-overweight . | Normal weight-overweight . |
|---|---|---|---|
| P value | .011 | .011 | .174 |
| Delta bra size | ≤2 | >2-3 | >3 |
| P value | .005 | .004 | .412 |
| Prosthetic volume, cc | <300 | 300-400 | >400 |
| P value | .003033 | .005562 | .64703 |
| BMI . | Underweight-normal weight . | Underweight-overweight . | Normal weight-overweight . |
|---|---|---|---|
| P value | .011 | .011 | .174 |
| Delta bra size | ≤2 | >2-3 | >3 |
| P value | .005 | .004 | .412 |
| Prosthetic volume, cc | <300 | 300-400 | >400 |
| P value | .003033 | .005562 | .64703 |
BMI, body mass index.
Finally, patients with a pinch test ≥2 cm related to a greater improvement in breast satisfaction postoperatively than patients who had a pinch test value <2 cm. The comparison of the delta between patients who underwent dual-plane technique with a pinch test ≥ 2 cm and patients with subglandular placement did not show a statistically significant correlation with patient satisfaction. On the other hand, when comparing the delta Rasch of patients undergoing the dual-plane technique with a pinch test < 2 cm with patients who had the same technique performed but with higher pinch test, a statistically significant difference was found, with greater satisfaction in the latter. The preoperative and postoperative changes are shown in Figures 5-9.
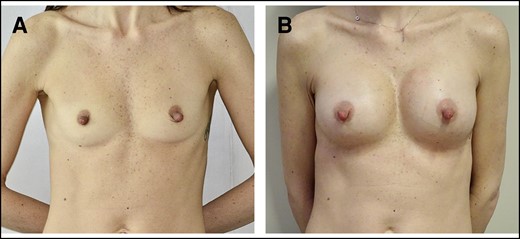
(A) Preoperative underweight 38-year-old patient, BMI = 18.3 kg/m2, pinch test <2 cm. (B) One year post operation, anatomical prosthesis of 322 cc, dual-plane technique, inframammary access site; delta Rasch 24 (preoperative score 28; postoperative score 52). BMI, body mass index.

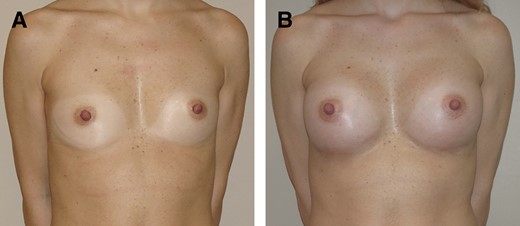
(A) Preoperative overweight 22-year-old patient, BMI = 25.8 kg/m2, pinch test ≥2 cm. (B) One year post operation, anatomical prosthesis of 390 cc, subglandular plane, inframammary access; delta Rasch 77 (preoperative score 23; postoperative score 100). BMI, body mass index.
(A) Preoperative 34-year-old patient of normal weight, BMI = 20.2 kg/m2, pinch test < 2 cm. (B) One year post operation, anatomical prosthesis of 295 cc, dual-plane technique, inframammary access; delta Rasch 56 (preoperative score 35; postoperative score 91). BMI, body mass index.
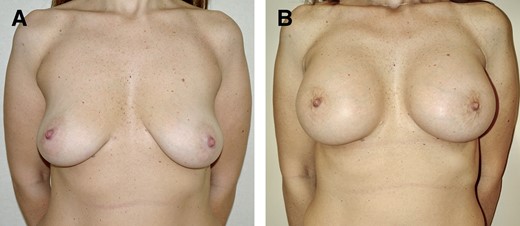
(A) Preoperative 38-year-old patient of normal weight, BMI = 23.8 kg/m2, pinch test ≥2 cm. (B) One year post operation, anatomical prosthesis of 400 cc, dual-plane technique, inframammary access; delta Rasch 83 (preoperative score 17; postoperative score 100). BMI, body mass index.
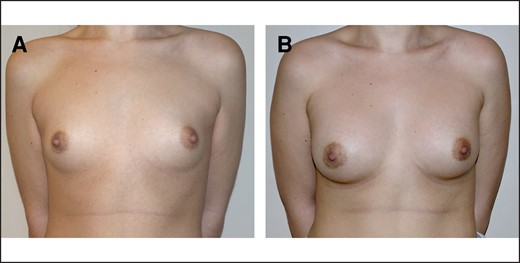
(A) Preoperative 26-year-old patient of normal weight, BMI = 21.3 kg/m2, pinch test < 2 cm. (B) One year post operation, 275-cc round prosthesis, dual-plane technique, lower hemiperiareolar access, 1 bra size increase; delta Rasch 27 (preoperative score 44; postoperative score 71). BMI, body mass index.
DISCUSSION
Over the years, more and more attention has been paid to the patient's point of view, and the advent of validated questionnaires such as BREAST-Q has made it possible to investigate this field in a more accurate and reliable way.10-12 Patient satisfaction is, ultimately, the most important aspect and the main goal of cosmetic surgery, and therefore deserves to be investigated and studied in detail, together with the aspects that can affect it.
Various studies, including ours, have shown that breast augmentation is generally correlated with a high degree of patient satisfaction and increases a woman's quality of life by enhancing sexual attraction, self-esteem, and social relationships.1-4 However, it is not always obvious which factors have a greater influence on patient satisfaction. The aim of this study was to evaluate how the main aspects related to the patient and the surgery influenced the degree of patient satisfaction, regardless of the surgeon's opinion.
A large study by Alderman et al identified patients’ age as the only element having a statistically significant impact on their satisfaction after submuscular breast augmentation: in fact, older patients were less satisfied with the result of the surgery.3 Contrary to this, analyzing the data of the 131 patients in our study, we found 3 main factors affecting their satisfaction (P<.05):
BMI: underweight patients were less satisfied than normal and overweight patients.
Pinch test: patients with a pinch test of ≥2 cm were more satisfied.
Volume of implant and bra size increase: patients with an implant volume of <300 cc and an increase of <2 bra sizes were less satisfied than patients with larger augmentation.
BMI and pinch test are often partially related, because the latter measures the thickness of the subcutaneous tissue, which is normally less represented in underweight patients.14 It is well known that patients with poor subcutaneous tissue are at higher risk of complications related to the visibility of the implant, such as rippling; we excluded from this study patients who developed this issue, as well as those with other complications, to determine whether the subcutaneous tissue thickness affected the satisfaction of patients with a straightforward postoperative course. It is our hypothesis that patients with thinner subcutaneous tissues are less satisfied because the implants are less camouflaged and more obvious, despite being not clearly visible, and therefore the result may be more artificial to the eye and touch. Our data showed that the dual-plane technique in underweight patients and in females with a pinch test of <2 cm led to a lower degree of satisfaction than the same technique in patients with a higher BMI and pinch test; at the same time, patients who were normal or overweight and had pinch tests greater than 2 cm were equally satisfied, regardless of whether dual-plane or subglandular technique was performed. Because the dual-plane technique was implemented in all patients with a pinch test of <2 cm, we were unable to quantify the advantage of this approach over others in providing better implant coverage and patient satisfaction. However, in our opinion, and also reported in the literature, the dual-plane pocket remains particularly well suited for this kind of patients; the subglandular approach might lead more easily to implant visibility.
Lipofilling can play an important role in increasing the thickness of breast subcutaneous tissue; underweight patients are often the ones who would benefit the most from this ancillary procedure, but at the same time they have very little or no fat deposits from which to harvest the necessary tissue.15,16 Even in underweight females, however, it is often possible to find small amounts, possibly by harvesting minimal volumes from multiple body areas in the same surgery; in our experience, even small amounts of adipose tissue are often able to improve the final result. Beyond careful preoperative assessment and technical arrangements for mitigating the visibility of the implants, it is of paramount importance to thoroughly discuss the details with the patient, who must be fully aware of how the breast may appear after implantation.
The volume of the implant and the increase of breast volume appeared to be decisive factors for patient satisfaction in our sample. During preoperative counseling, we investigated the desired volume by trying sizers and having a thorough discussion with the patient. At the end of the evaluation, all patients were satisfied with the chosen volume. Anecdotally, during the follow-up many of these patients stated that, given another chance, they would have chosen a bigger implant. Moreover, in our experience, despite efforts to help patients understand that the implant volume is not the main aspect to consider, the size of implant by cc remains psychologically significant for some of them. Some studies reported that big implants, especially those larger than 400 cc, seem to be related to a higher complication rate in the long term; on the other hand, small implants might deliver fewer benefits of satisfaction to the patient.17 What to privilege then? Bearing in mind that the breast base and the anthropometric features of the patient should definitely lead the choice of the implant, we believe that, when possible and desired by the patient, it might be wise to choose larger implants, in particular when considering volumes around 300 cc. In our experience, intraoperative sizers are a great help in this regard. Nonetheless, it is essential to make the patient understand that the choice of implant must follow certain criteria, and that the volume should be the result of a careful evaluation, rather than the starting point. Preoperative sizers are our preferred method for demonstrating to the patient what to expect in terms of volumetric increase. Once again, proper preoperative assessment is crucial and, at the same time, it is important to help patients understand what is realistically achievable and to manage their expectations before the surgery.
The main surgical factors, namely pocket plane, surgical access, and shape of the implant, did not show a significant influence on patients’ satisfaction. We could hypothesize that, if the specific indications for each of them is properly followed, it will lead to good results from the patient’s point of view.
Limitations of this study included the fact that it was carried out in a single center, and all patients were operated on by the same surgeon, making the results less generalizable. Geographical, cultural, and local aesthetic trends may have strongly influenced the patients’ opinions, which may be a potential explanation for the differences in results from results of previous studies from other countries.3 In addition, we could not evaluate the influence of some factors, such as the subfascial and total submuscular techniques, because they were not normally employed in the practice of the main surgeon. It would be interesting to extend this study to a multicenter design with a higher number of patients of different ethnicities, also taking into consideration other surgical techniques.
On the other hand, this prospective study took into consideration a large number of factors, related to either the patient or the surgery, and assessed patient satisfaction with a validated questionnaire. The results of this study underline that some parameters may consistently correlate to patients’ satisfaction. Knowing the factors that primarily influence patients’ point of view, the surgeon can focus on them during the preoperative consultation, making the patient aware of the impact of certain features on the postoperative result. In our opinion, these results do not change the operative technique radically, but they could lead the surgeons to place implants with slightly larger volumes where possible in accordance with patient features; in this regard, an intraoperative sizer may be particularly helpful in evaluating the larger volume suitable for that particular patient.
Furthermore, it may be worth considering an ancillary procedure such as lipofilling, especially in patients with a low BMI and poor representation of subcutaneous tissue. The data from this study may help with analysis of patients’ point of view in more detail, and the particular aspects that may influence their satisfaction, emphasizing to the surgeon the importance of those factors in preoperative and intraoperative management. By understanding the patient's perspective in more depth, the surgeon may have additional tools to discuss with her, and be able to better guide her wishes and expectations in the most appropriate way for both patient and surgeon.
CONCLUSIONS
Underweight patients, or those who had a breast pinch test of less than 2 cm, had less benefit in terms of satisfaction with their breasts following primary augmentation; likely, poor representation of the subcutaneous tissue leads to greater evidence of the presence of the implant, which is subjectively perceived by the patient herself. At the same time, implant size and the extent of volumetric increase remained key elements in determining the degree of satisfaction of many patients who decided to undergo surgery. A proper preoperative evaluation and some technical refinements are essential to better managing these aspects, and a thorough consultation with the patient is of paramount importance. Knowing the elements that may influence her perception of the postoperative result can be of great help to the surgeon in guiding the discussion with the patient, understanding her wishes, and managing her expectations.
Disclosures
The authors declared no potential conflicts of interest with respect to the research, authorship, and publication of this article.
Funding
The authors received no financial support for the research, authorship, and publication of this article.
REFERENCES
Author notes
Drs Marangi, Segreto, Cagli, and Cogliandro are plastic surgeons; Dr Savani, Gratteri, Arcari, and Mirra are residents; Dr Vega is a resident, Department of Plastic, Reconstructive, and Cosmetic Surgery, Pisa University Hospital, Pisa, Italy
Dr Persichetti is the department chair, Department of Plastic, Reconstructive, and Cosmetic Surgery, Campus Bio-Medico University Hospital, Rome, Italy.
- client satisfaction
- pregnancy
- smoking
- body mass index procedure
- consultation
- educational status
- follow-up
- habits
- mental disorders
- preoperative care
- surgical procedures, operative
- breast
- plastic surgery procedures
- augmentation mammoplasty
- underweight
- levels of evidence
- overweight
- patient self-report
- implants
- chief complaint



