-
PDF
- Split View
-
Views
-
Cite
Cite
Enrico Tognazzo, Sarah Berndt, Jasmine Abdulcadir, Autologous Platelet-Rich Plasma in Clitoral Reconstructive Surgery After Female Genital Mutilation/Cutting: A Pilot Case Study, Aesthetic Surgery Journal, Volume 43, Issue 3, March 2023, Pages 340–350, https://doi.org/10.1093/asj/sjac265
Close - Share Icon Share
Abstract
Postoperative healing after clitoral reconstruction (CR) for female genital mutilation/cutting can be long and painful due to prolonged clitoral re-epithelialization time (up to 3 months). Autologous platelet-rich plasma (A-PRP) might reduce postoperative clitoral epithelialization time and pain.
The authors assessed postoperative clitoral re-epithelialization time and pain after intraoperative clitoral administration of A-PRP.
Five consecutive women underwent CR (Foldès technique) followed by the administration of A-PRP Regen Lab SA (Le Mont-sur-Lausanne, Switzerland) plasma and glue, injected inside and applied above the re-exposed clitoris, respectively. We recorded surgical complications, postoperative clitoral pain (visual analogue scale), painkiller intake, time to complete re-epithelialization, and the experienced subjective changes in sexual response and perception of their own body image referred by women.
Sexual distress/dysfunction as well as the desire to be physically and symbolically “repaired” were the reasons behind women's requests for surgery. None of the women suffered from chronic vulvar or non-vulvar pain. All women achieved complete clitoral epithelialization by day 80, 3 women between day 54 and 70, and only 1 woman was still taking 1 g of paracetamol twice a day at 2 months postoperative. She had stopped it before the 3-month control. There were no short- or long-term complications. All women described easier access and stimulation of their clitoris as well as improved sexual arousal, lubrication, and pleasure and claimed to be satisfied with their restored body image.
A-PRP could expedite postoperative clitoral epithelialization and reduce postoperative pain after CR after female genital mutilation/cutting.

See the Commentary on this article here.
Female genital mutilation/cutting (FGM/C) is a practice still performed in more than 30 African, Asian, and Middle East countries.1,2 It is estimated that more than 200 million girls and women have undergone it all over the world.1 A total 600,000 women and girls in the European Union and 513,000 women and girls in the United States are estimated to be living with FGM/C.3,4 Recent estimates of the number of women and girls living in Switzerland with or at risk of FGM/C have increased 239% between 2010 and 2018 (from 9059 to 21,706 women) due to increasing migration.5 The World Health Organization classifies FGM/C into 4 types.6 Type I involves the partial or total removal of the clitoral glans and/or the prepuce/clitoral hood. Type II is the partial or total removal of inner labia with or without the cutting of the clitoris and/or the outer labia. Type III, also known as infibulation, is the narrowing of the vaginal opening through the creation of a covering seal, formed by cutting and repositioning the inner or outer labia, with or without excision of the clitoris. Type IV includes all other procedures to the female genitalia for non-medical purposes, for example, pricking, piercing, incising, scraping, and cauterizing the genital area.
Women and girls who have had FGM/C are known to possibly suffer from long-term health complications that can be gynecological, obstetrical, urological, infectious, psychological, and sexual.6–11 FGM/C can remove, alter, or injure parts of the erogenous and sexually responsive vascular tissues and cause dyspareunia and sexual dysfunction.11 However, women and girls who have been cut still have most of the anatomic structures to achieve orgasm and experience sexual pleasure. It is in fact the visible and accessible part of the clitoris that can be cut in some types of procedures, while the crura and the body or part of the body of the clitoris remain intact.12 In addition to biological factors, psychological, socio-cultural, experience, and relational factors play a crucial role in female sexual pleasure, response, satisfaction, relationships, and body image as well as in the coping strategies of pain and other eventual psychosexual complications.13,14
Reconstructive surgery after FGM/C aims to remove the scar or scar complications (eg, cysts, adhesions, fibrosis, neuromas of the clitoris, clitoral phimosis, etc) and, in the case of type III FGM/C, to uncover the vaginal introitus, urethral meatus and eventually the clitoris (defibulation). Clitoral reconstruction (CR) or transposition is a surgery that removes the scar above the excised clitoris, the periclitoral fibrosis, and exposes the body of the clitoris previously under the scar.15 It can improve access to the clitoris, facilitating its stimulation and reducing pain.16 CR also has an important psychological and symbolic impact because most patients undergo this surgery with the aim of recovering their female identity and obtaining a psychological and symbolic reparation, even in lack of pain and sexual dysfunction.17–19
Early complications of CR are hematoma, suture failure, infection, and need for hospital readmission.16,20 Long-term complications include worsening in sexual response with hyperesthesia of the clitoris,21 orgasmic dysfunction,22 chronic neuropathic pain,7 recall of the experience of the FGM/C due to postoperative pain, and dissatisfaction with the new genital appearance.23,24
Clear data about postoperative pain assessment, patient experience, and management are missing.25 Little is known, for example, about postoperative pain changes according to different surgical, anesthetic, and dressing techniques. What we know is that, even when uneventful, the postoperative period after CR can be long and painful, with 72.1% of patients reporting pain 7 days after the surgery.26 Most of the available literature reports outcomes of the Foldès technique with pain possibly lasting up to 3 months until full clitoral re-epithelialization is accomplished.27,28 It is usually only after 3 months, when such re-epithelialization is achieved, that sexual, sport, and daily life activities can be fully resumed. Some authors also reported that patients might regret or be afraid and do not opt for surgery because of the painful postoperative days or months.25
Pain after CR can be due to nociceptive/inflammatory causes or to neuropathic causes as well as a combination of the two. Neuropathic pain can be due to an involvement of the dorsal nerve in the surgery or to the resection of the neuromas that are often present in the peri-clitoral tissue removed during surgery.
In addition, postoperative pain might cause patients to recall the experience of FGM/C and/or other sexual or non-sexual traumatic past events, which are frequent in this often vulnerable migrant population.
Reducing the time of re-epithelialization of the clitoris might decrease postoperative pain and decrease the time for healing. This is important for allowing patients to resume earlier their daily and sexual activities.
Autologous Platelet-Rich Plasma (A-PRP; Regen Lab SA [Le Mont-sur-Lausanne, Switzerland]) is a regenerative therapy employed to improve healing in tissues with low healing potential due to low blood supply and slow cell turnover, as in musculoskeletal lesions (tendons, ligaments, and cartilage) and diabetic wounds.29,30 It has also demonstrated a role in reducing neuropathic scar pain in burn scar areas.31 A-PRP consists in autologous plasma enriched in platelets (4-6 times the number of platelets present in normal blood). It is hypothesized to provide a regenerative stimulus due to the release of growth factors (platelet-derived growth factor, transforming growth factor-beta, vascular endothelial growth factor, epidermal growth factor, insulin-like growth factor 1) and cytokines by platelets' alpha granules enhancing a proliferation on adipose-derived stem cells and dermal fibroblasts.32
In gynecological surgery, A-PRP has been utilized with or without lipofilling to treat lichen sclerosus, showing an improved score when symptoms are evaluated.33,34 When applied to treat vaginal dryness in women with a history of breast cancer, intra-mucosal administration of A-PRP seems to lead to a higher Vaginal Health Index, with improved hydration and vaginal epithelial integrity.35 A-PRP gel has also been utilized in women who underwent radical vulvectomies. One retrospective study showed lower rates of necrosis, wound dehiscence, postoperative fever, and time of hospitalization in women who received A-PRP gel compared with those who did not receive it.36 Furthermore, we recently published a case report about a woman with type II FGM/C who had good pain and healing outcomes with epithelialization nearly completed and no need for pain killers at 2 months after CR.37 Finally, A-PRP was recently proposed as a minimally invasive method that could improve female sexuality when administered into the lower anterior vaginal wall in patients with and without FGM/C.38
In this case series, we assessed postoperative pain and time to complete epithelialization after 1 single intraoperative injection of A-PRP Regen Lab and A-PRP Regen Lab glue application in a pilot study on 5 women who underwent clitoral reconstructive surgery and psychosexual therapy after FGM/C. This is a pilot study aimed at informing a future randomized controlled trial.
METHODS
Five consecutive women who consulted at our FGM/C outpatient clinic—Gynecological and Obstetrical Service of the University Hospitals of Geneva—requesting CR between April 2019 and July 2020 received the usual multidisciplinary care, including psychosexual therapy and follow-up, and were offered and agreed to a single intraoperative intra-clitoral injection of A-PRP Regen Lab SA and A-PRP Regen Lab SA glue clitoral application with the aim to possibly reduce time of healing, time to complete epithelialization and pain.
Data on reasons for requesting surgery and expectations regarding the intervention were collected with sociodemographic and clinical information, including type of FGM/C, age when the FGM/C was performed, short- and long-term (genitourinary, psychological, and sexual) complications of the practice, and memories of the cutting. As usual, all women received interdisciplinary care with sexual counseling, psychosexual evaluation and were referred for psychosexual therapy with our psychologist sex therapist with information on their sexual anatomy, physiology, and response. Detailed information, including drawings and/or pictures of their vulva, CR, outcomes, and risks, were provided. During the preoperative discussion, we routinely employed 3-dimensional models of the clitoris with and without FGM/C and of the pelvis to explain the sexual anatomy and response as well as the surgical technique.39
Information about a possible A-PRP administration and its risks were given. Although there are still no studies, to our knowledge, about injections of A-PRP after CR, women were informed of the available literature and the known general risks linked to A-PRP injections in other sites, such as local bleeding, infection, pain and uncomfortable feeling, and allergy. All women did not present with other vulvar conditions than the FGM/C and signed a written informed-consent to agree with the surgery, the utilization of A-PRP, and the publication of this case series. Following Swiss Association of Research Ethics Committee directives, there was no need for an ethics committee approval for a 5-case series.40 The study was conducted in the respect of the ethical principles for medical research involving human patients of the Declaration of Helsinki.41
The A-PRP was provided with no additional costs by Regen Lab SA. Regen Lab SA did not interfere with the care of the patients or with the development of the study design and data analysis. The costs of the clitoral surgery and non-surgical care after FGM/C is refunded by health insurance in Switzerland.42
In all women, CR was performed according to Foldès technique, in gynecological position, in day care, under general anesthesia with laryngeal mask and 2 g of cefazolin as antibioprophylaxis.28 According to our protocol, patients were discharged with a prescription of paracetamol 1 g 4 times a day, ibuprofen 400 mg 3 times a day, and tramadol 50 mg 4 times a day. In our experience, tramadol is regularly utilized, in general, during the first postoperative 30 to 40 days.
A-PRP plasma and glue were produced during the surgery by centrifuging two 8-mL tubes (RegenBCT® tubes) of the patient's blood to separate the different blood components and extract the PRP. The blood was taken at the moment of the intravenous line placement. The tubes underwent a 5-minute centrifugation at a centrifugal force of 1500 g. The obtained plasma was collected from the tubes. For each tube of 8 mL of blood, 4.5 mL of A-PRP was obtained. The obtained A-PRP has a platelet concentration 1.6 times over the whole-body value. Red blood cells are removed at 99.7%, and white blood cells are removed at 96.5% (among white blood cells, granulocytes are preferentially removed, leaving mostly lymphocytes and monocytes in A-PRP). Platelets in RegenLab PRP have been shown to be functionally active if utilized within 4 hours after the blood sampling.43
A-PRP glue was also produced from women's blood during the intervention. In this case, the blood was collected in an 8-mL tube without anti-coagulants (RegenATS®). The tube underwent 2 cycles of 5-minute centrifugation at a centrifugal force of 1500 g. After the centrifugation, the plasma is coagulated and it is possible to extract a serum rich in activated thrombin. The serum with the activated thrombin is then employed to activate A-PRP coagulation in the A-PRP glue.
A-PRP plasma was injected immediately after preparation inside the reconstructed clitoris. The aim of the injection was to enhance a proliferation on adipose-derived stem cells and on dermal fibroblasts to help epithelialization of the clitoral body tissue and expedite healing of nerve endings, reducing neuropathic scar pain. Volumes injected ranged from 2.6 to 5 mL, depending on the size of the re-exposed clitoral body. The injection was performed directly inside the clitoral body in 2 different points (superior and inferior). The volume of A-PRP injected was related to the size of the “neo” clitoris. The injection was stopped when some resistance was felt. For each patient, A-PRP glue was then applied above the clitoris at the end of the surgery with the aim to cover the non-epithelialized clitoris and expedite healing.
We chose A-PRP Regen Lab because it has a platelet concentration factor of 1.6-fold, one- to threefold being the concentration that has been shown to be the most beneficial for clinical utilization concentrations.44 Moreover, the amount of white blood cells is deeply reduced (>85% depletion), particularly granulocytes (>96%) releasing antimicrobial substances and protease delaying healing.45 Postoperative follow-up was scheduled at 1, 3, 6, 8, and 12 weeks.
We assessed the intake of pain killers and clitoral pain using the pain visual analogue scale (VAS). We also clinically evaluated and documented time to complete re-epithelialization. We recorded eventual, immediate, or late complications and subjective changes in sexual response, genital appearance, and body image. In this pilot study, patient satisfaction in sexual response and body image was recorded as a subjective appreciation without a specific questionnaire.
A photographic documentation of the pre-, intra, and postoperative clitoral appearance was collected. Patients gave their informed written consent for the procedure, for personal data utilization in this case series, and for photographs to be taken and published in this manuscript.
RESULTS
All women were originally from Africa (Guinea, Senegal, Somalia, and Mali), between 27 and 51 years old (average, 39 ± 8 years old), and with FGM/C type III. Three had FGM/C type IIIa; the remaining 2 women had type IIIb and had been previously defibulated.
All women had self-referred to the clinic. They spontaneously asked for CR with no previous proposition by the doctor of the clinic or other health professionals. They had heard about the surgery from friends or the media. All desired to both physically and symbolically repair the genital cutting. Some of them were also willing to improve their sexual functioning (Table 1). None suffered from chronic vulvar or non-vulvar pain.
| Age, y . | Original country . | FGM/C type . | Reason for requesting CR . |
|---|---|---|---|
| 35 | Guinea | IIb (previous IIIb) | Physical and symbolic repair, improvement of sexual desire and pleasure |
| 51 | Senegal | IIIa | Physical and symbolic repair, improvement of sexual desire, arousal, and pleasure. Decrease superficial dyspareunia |
| 27 | Somalia | IIb (previous IIIb) | Physical and symbolic repair, restoring body image |
| 39 | Senegal | IIIa | Physical and symbolic repair, restoring body image, improvement of sexual desire and arousal |
| 43 | Mali | IIIa | Physical and symbolic repair, restoring body image, decrease superficial dyspareunia |
| Age, y . | Original country . | FGM/C type . | Reason for requesting CR . |
|---|---|---|---|
| 35 | Guinea | IIb (previous IIIb) | Physical and symbolic repair, improvement of sexual desire and pleasure |
| 51 | Senegal | IIIa | Physical and symbolic repair, improvement of sexual desire, arousal, and pleasure. Decrease superficial dyspareunia |
| 27 | Somalia | IIb (previous IIIb) | Physical and symbolic repair, restoring body image |
| 39 | Senegal | IIIa | Physical and symbolic repair, restoring body image, improvement of sexual desire and arousal |
| 43 | Mali | IIIa | Physical and symbolic repair, restoring body image, decrease superficial dyspareunia |
CR, clitoral reconstruction; FGM/C, female genital mutilation/cutting;
| Age, y . | Original country . | FGM/C type . | Reason for requesting CR . |
|---|---|---|---|
| 35 | Guinea | IIb (previous IIIb) | Physical and symbolic repair, improvement of sexual desire and pleasure |
| 51 | Senegal | IIIa | Physical and symbolic repair, improvement of sexual desire, arousal, and pleasure. Decrease superficial dyspareunia |
| 27 | Somalia | IIb (previous IIIb) | Physical and symbolic repair, restoring body image |
| 39 | Senegal | IIIa | Physical and symbolic repair, restoring body image, improvement of sexual desire and arousal |
| 43 | Mali | IIIa | Physical and symbolic repair, restoring body image, decrease superficial dyspareunia |
| Age, y . | Original country . | FGM/C type . | Reason for requesting CR . |
|---|---|---|---|
| 35 | Guinea | IIb (previous IIIb) | Physical and symbolic repair, improvement of sexual desire and pleasure |
| 51 | Senegal | IIIa | Physical and symbolic repair, improvement of sexual desire, arousal, and pleasure. Decrease superficial dyspareunia |
| 27 | Somalia | IIb (previous IIIb) | Physical and symbolic repair, restoring body image |
| 39 | Senegal | IIIa | Physical and symbolic repair, restoring body image, improvement of sexual desire and arousal |
| 43 | Mali | IIIa | Physical and symbolic repair, restoring body image, decrease superficial dyspareunia |
CR, clitoral reconstruction; FGM/C, female genital mutilation/cutting;
Sexual dysfunction included subjective complaining of low desire (both spontaneous and after stimulation), lack of or rare orgasm, and low lubrication with consequent superficial dyspareunia. One woman reported low desire, low pleasure, and lack of orgasm during sexual intercourse with her previous partner but could currently experience sexual pleasure, arousal, and orgasm with masturbation.
All women already had at least 1 child. Four had had vaginal deliveries. Only 1 had a history of a cesarean birth for pathologic cardiotocography, with a second child born via vaginal birth 3 years after. None of the women smoked.
All women underwent CR according to the Foldes' technique between April 2019 and July 2020. The 3 women with FGM/C type IIIa were defibulated at the same time as CR.
The median of the operation time was 65 minutes (interquartile range [IQR] = 15 minutes). All operations were uneventful. Periclitoral fibrosis removed during CR was analyzed as usually for all women. Four out of 5 presented a neuroma within the scar removed. One had a fibro-scar remodelling. Four out of 5 patients had a complete follow-up at 6 months. One woman lived far away and had a follow-up in person at 3 months and by phone at 6 months.
Pain and Intake of Painkillers
None of the women presented preoperative pain and particularly clitoral pain. Postoperative pain results are summarized in Table 2. Eight weeks after the operation, only 1 patient was still taking paracetamol twice a day, which was the only painkiller treatment (median 0 g/d, IQR = 1 g). All patients reported a VAS score at 0.
Pain Evaluated With VAS and Need of Painkillers During Postoperative Follow-up at Day 7, 21, 42, and 84 After CR
| Postoperative time . | VAS scale . | Median use of paracetamol . | Median use of ibuprofen . | Median use of tramadol . |
|---|---|---|---|---|
| 7 d | Between 0 and 6 (median 4 [IQR = 5]) | 4 g/d (IQR = 3 g) | 1200 mg/d (IQR = 800 mg) | 0 mg/d (IQR = 100 mg) |
| 21 d | Between 0 and 3 (median 0 [IQR = 1.5]) | 2 g/d (IQR = 2 g) | 800 mg/d (IQR = 1000 mg) | 100 mg/d (IQR = 125 mg)a |
| 42 d | Between 0 and 3 (median 0 [IQR = 1.5]) | 2 g/d (IQR = 2.5 g) | 800 mg/d (IQR = 1000 mg) | 0 mg/d (IQR = 25 mg)b |
| 84 d | 0 | None | None | None |
| Postoperative time . | VAS scale . | Median use of paracetamol . | Median use of ibuprofen . | Median use of tramadol . |
|---|---|---|---|---|
| 7 d | Between 0 and 6 (median 4 [IQR = 5]) | 4 g/d (IQR = 3 g) | 1200 mg/d (IQR = 800 mg) | 0 mg/d (IQR = 100 mg) |
| 21 d | Between 0 and 3 (median 0 [IQR = 1.5]) | 2 g/d (IQR = 2 g) | 800 mg/d (IQR = 1000 mg) | 100 mg/d (IQR = 125 mg)a |
| 42 d | Between 0 and 3 (median 0 [IQR = 1.5]) | 2 g/d (IQR = 2.5 g) | 800 mg/d (IQR = 1000 mg) | 0 mg/d (IQR = 25 mg)b |
| 84 d | 0 | None | None | None |
VAS, Visual Analog Scale. aTramadol was taken because of severe pain when moving and clitoral rubbing. Two women referred occasional sensations of short intermittent painful clitoral electric shocks. bOnly 1 woman who took tramadol once a day since the early postoperative period still needed to take tramadol once a day because of persistence of not painful but distressing small clitoral electric shocks.
Pain Evaluated With VAS and Need of Painkillers During Postoperative Follow-up at Day 7, 21, 42, and 84 After CR
| Postoperative time . | VAS scale . | Median use of paracetamol . | Median use of ibuprofen . | Median use of tramadol . |
|---|---|---|---|---|
| 7 d | Between 0 and 6 (median 4 [IQR = 5]) | 4 g/d (IQR = 3 g) | 1200 mg/d (IQR = 800 mg) | 0 mg/d (IQR = 100 mg) |
| 21 d | Between 0 and 3 (median 0 [IQR = 1.5]) | 2 g/d (IQR = 2 g) | 800 mg/d (IQR = 1000 mg) | 100 mg/d (IQR = 125 mg)a |
| 42 d | Between 0 and 3 (median 0 [IQR = 1.5]) | 2 g/d (IQR = 2.5 g) | 800 mg/d (IQR = 1000 mg) | 0 mg/d (IQR = 25 mg)b |
| 84 d | 0 | None | None | None |
| Postoperative time . | VAS scale . | Median use of paracetamol . | Median use of ibuprofen . | Median use of tramadol . |
|---|---|---|---|---|
| 7 d | Between 0 and 6 (median 4 [IQR = 5]) | 4 g/d (IQR = 3 g) | 1200 mg/d (IQR = 800 mg) | 0 mg/d (IQR = 100 mg) |
| 21 d | Between 0 and 3 (median 0 [IQR = 1.5]) | 2 g/d (IQR = 2 g) | 800 mg/d (IQR = 1000 mg) | 100 mg/d (IQR = 125 mg)a |
| 42 d | Between 0 and 3 (median 0 [IQR = 1.5]) | 2 g/d (IQR = 2.5 g) | 800 mg/d (IQR = 1000 mg) | 0 mg/d (IQR = 25 mg)b |
| 84 d | 0 | None | None | None |
VAS, Visual Analog Scale. aTramadol was taken because of severe pain when moving and clitoral rubbing. Two women referred occasional sensations of short intermittent painful clitoral electric shocks. bOnly 1 woman who took tramadol once a day since the early postoperative period still needed to take tramadol once a day because of persistence of not painful but distressing small clitoral electric shocks.
Re-epithelialization
Two women presented with a starting of the epithelialization of the clitoris at day 30. Median time-to full epithelialization was 60 days (IQR = 20 days). Figures 1, 2 show the preoperative appearance and the re-epithelialization process in 2 women with FGM/C who underwent CR with A-PRP.

This 51-year-old female presented with type IIIa female genital mutilation/cutting. (A) Before surgery. (B) Postoperative check at day 67: starting of re-epithelialization, there was no need of pain killers. (C) Postoperative check at 3 months: re-epithelialization completed; masturbation resumed. (D) Postoperative check at 6 months.
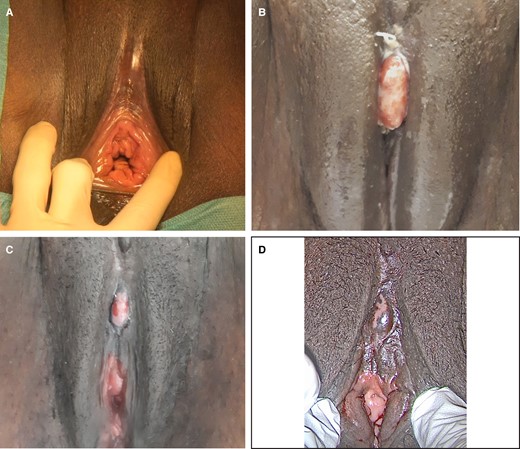
This 35-year-old female presented with type IIb female genital mutilation/cutting. (A) Before surgery. (B) Postoperative check at day 22: not yet re-epithelialized, the pain was successfully managed with pain killers. (C) Postoperative check at day 46: an advanced state of re-epithelialization, no pain killer intake. (D) Postoperative check at day 70: re-epithelialization almost completed, no pain (menstruation).37
Subjective Report of Sexual Response
Women were able to resume masturbation between 2 and 3 months after surgery and sexual intercourse at 2 to 4 months. All women described easier access and stimulation of their clitoris that they found more accessible and more sensitive. They all referred to experiencing easier and improved sexual arousal, lubrication, and pleasure with easier orgasm.
Subjective Aesthetic Result
All women noticed a change in the appearance of the re-exposed clitoris during the postoperative follow-up, particularly a decreased size of the clitoris starting from 2 months after the surgery when comparing it with their immediate postoperative appearance. All said they felt restored/repaired in their body and genital image and sexuality and felt the experience of surgery and psychosexual care as “a journey” of repair.
DISCUSSION
We describe a 5-case series on the intraoperative utilization of A-PRP in CR in women with FGM/C for reducing epithelialization time and consequently postoperative pain.
Complications
There were no short- or long-term complications after CR with A-PRP injection. To our knowledge, there is no evidence of long-term adverse outcomes after A-PRP injections; short-term risks include local subcutaneous bleeding, local infections, acute local pain, and an uncomfortable feeling.45 Among others, Gibran et al described A-PRP as safe and effective for treatment of burn wounds with autologous sheet grafts.46 Similarly, Gupta et al described it as biocompatible, safe, and effective in a case-control study among 200 patients treated with skin grafts for resurfacing wound burns.47 In gynecology, A-PRP has been employed by King et al to treat vulvar lichen sclerosus. These authors reviewed the published literature showing that autologous PRP has minimal risk of scar tissue formation or serious adverse events.34 Future studies could assess if a faster healing can be associated with a higher risk of retraction or fibrosis of the clitoris and if A-PRP is safe in women who might have or did have a vulvar dysplasia.
Pain and Intake of Painkillers
Postoperative pain is known to be frequent after CR, reducing women's quality of life during the first months after the operation and potentially leading to a posttraumatic stress disorder relapse.9,10,23,25,26 Postoperative pain can be difficult to evaluate in women with FGM/C who experience baseline preoperative moderate to severe pain with or without sexual intercourse, and most studies on CR did not study and report postoperative pain assessment, limiting our knowledge on the subject.25,48
Previous authors have tried to propose different solutions to decrease the healing time and postoperative pain, which often starts at day 7, for instance modifying the Foldès surgical technique with the resurfacing of the re-exposed clitoris with a graft of vaginal wall, a minor labial flap, a mucosal buccal graft, or a local flap such as the Omega-Domed flap and micro-surgery.19,49–51 There is also increasing and new interest from the plastic and regenerative medicine field in the surgical and postsurgical care of women with FGM/C.19
In our sample, painkiller intake and VAS scale progressively declined in the first 6 weeks after the operation. Only 1 woman was still taking paracetamol 1 g twice a day at the 8-week check and stopped it before the 12-week control. Validated questionnaires could be utilized in further studies to compare and evaluate preoperative and postoperative pain after CR and the impact and experience of such pain.
Epithelialization Time
Re-epithelialization time generally shows a high heterogeneity, making it difficult to assess a normal time to full re-epithelialization. The usual reported length after CR is 3 months, which is also what we have noticed in our clinical experience.15
Our pilot study shows a time of complete clitoral epithelialization occurring between 8 and 12 weeks after the operation, particularly between day 54 and 80, with a median of 60 days (IQR = 20 days). This delay seems to be shorter than the usually reported period of 3 months, but the low number of patients and absence of a control group limit our conclusions. The role of A-PRP in hastening the healing process has been investigated and demonstrated in skin grafts and in the treatment of chronic wounds.52,53 Such accelerated healing can be due to angiogenic and mitogenic properties of PRP. The degranulation of growth factors such as platelet-derived growth factor, vascular endothelial growth factor, epidermal growth factor, hepatocyte growth factor, fibroblast growth factor, and insulin-like growth factor 1 induces fibroblast activation, blood vessel formation, and adipose tissue formation, promoting soft-tissue healing.47,54
How to Utilize A-PRP
We administered only 1 intraoperative and intraclitoral injection of A-PRP and applied above the re-exposed clitoris the A-PRP glue. The long-term impact of a single PRP dose is yet to be proven because PRP can easily be drained from the site of injection. As in the treatment of vulvar lichen sclerosus and of cartilage pathology and osteoarthritis (with intra-articular injections), multiple clitoral injections of A-PRP could be proposed as a treatment to hasten the healing process of the clitoris. For the treatment of vulvar lichen sclerosus, 2 injections separated by 6 weeks have been utilized, whereas for osteo-articular diseases, injections have been administrated at 1- to 2-week intervals.34,55–57 In case multiple A-PRP injections are administered during the follow-up, if non-steroidal anti-inflammatory drugs are contemporarily employed to treat pain, these can inhibit platelet aggregation; questions have been raised about PRP’s final therapeutic effect.30,58 Eventually following non-intraoperative clitoral injections without general or spinal anesthesia, however, could be painful, and the acceptability and tolerability should be evaluated in this specific population with a history of genital cutting. Due to the design of the pilot study and the small sample, we cannot determine if the effect of A-PRP and the A-PRP glue differed. However, we think that the applied A-PRP glue might be less useful or not useful at all compared with the injection of A-PRP because the genitals are a site that is frequently washed and rubbed, and the glue might be worn off in a few hours. Since this pilot study, we have performed other CRs without the glue, applying only the A-PRP plasma in the clitoris.
Limits of the Study
The limits of our study are the small size of the group of patients and the lack of a control group, thus limiting the possibility to assess with certitude the role of A-PRP in hastening the healing process. Known confounding factors of scarring should also be considered when analyzing larger groups of patients. Moreover, the utilization of validated questionnaires and methods to assess pre- and postoperative symptoms and clitoral sensitivity as well as the utilization of objective outcomes of healing would help provide more objective and comparable results.
Larger randomized prospective studies are needed to assess if A-PRP can expedite healing and reduce pain after CR, together with other possible outcomes such as infection rate, aesthetic result, sexual functioning result, and clitoral sensitivity. If real clinical benefits are shown, the utilization of A-PRP in CR could also have socio-economic benefits. The costs of a tube of A-PRP is approximately 65 Swiss francs. PRP utilization in burn treatment reduced the cost of hospitalization by 25% compared with people with burns who did not receive PRP.59 Currently, A-PRP production and utilization are not often refunded for gynecological treatments.
CONCLUSIONS
A-PRP clitoral injection appears to be a safe procedure when utilized in CR. Our experience suggests a possible role in expediting healing and reducing pain for CR after FGM/C, which needs to be further investigated with larger randomized prospective studies.
Acknowledgments
The authors thank Regen Lab SA (Le Mont-sur-Lausanne, Switzerland) for providing A-PRP and Eric Wenger from Regen Lab SA, who assisted each A-PRP preparation.
Disclosures
Regen Lab SA (Le Mont-sur-Lausanne, Switzerland) provided the Autologous Platelet-Rich Plasma (A-PRP production). Dr Sarah Berndt is an employee of Regen Lab SA and provided information about the product and conceptualized how it could be employed for the authors' aim. Regen Lab SA did not influence the development of the study design, data analysis, and manuscript production.
Funding
The authors received no financial support for the research, authorship, and publication of this article.



