-
PDF
- Split View
-
Views
-
Cite
Cite
Farzad Nahai, Feizollah Niazi, Foad Nahai, Sana Niazi, Jill A Foster, Farideh Doroodgar, Alireza Baradaran-Rafii, Vania Rashidi, An Overview of Surgical Approaches for Lower Eyelid Blepharoplasty, Aesthetic Surgery Journal, Volume 43, Issue 12, December 2023, Pages 1429–1440, https://doi.org/10.1093/asj/sjad245
Close - Share Icon Share
Abstract
Age-related changes in the lower eyelid are noticed by patients as bags or circles under the eye, a tired look, and a flattened face. Lower eyelid blepharoplasty, in which the excess skin and/or orbital fat is excised and repositioned, is mainly performed for aesthetic reasons rather than the correction of functional abnormalities. Favorable outcomes for the combination of these approaches have been reported, but the most suitable surgical technique is still debated. This systematic narrative review deals with the indications, preoperative considerations, operative techniques, and complications of several different surgical approaches to lower eyelid blepharoplasty.

Traditions of Greek and Roman medicine, followed by Avicenna and Ibn Rashid (10th to 11th centuries), described the first removal of the eyelid skin, resulting in improved vision for the patient. The term “blepharoplasty” originated from Latin, and was first coined by Karl Ferdinand Von Gräfe in 1818.1 Blepharoplasty is one of the most common aesthetic procedures performed today.2 Upper eyelid blepharoplasty aims to correct functional abnormalities in conjunction with the aesthetic restoration of the upper eyelid.3 However, the main purpose of the lower lid blepharoplasty (LLB) is to achieve a more youthful or aesthetic improvement; functional abnormalities are rarely observed.4
Age-related lower eyelid changes can result in wrinkles, crepey skin, increased prominence of the orbital fat pads, tear trough deformity, and dark circles around the lower eyelid that create a tired appearance; altogether, in association with the loss of facial soft tissue and osseous atrophy, this results in flattening and sagging of the face.5 These changes, coupled with excessive skin, increased lower eyelid laxity, orbicularis oculi laxity or hypertrophy, herniated orbital fat, and malar festoons, are indications for LLB.6
As Foad Nahai has clearly stated, lower eyelid surgery cannot be considered just a skin surgery.7 Lower eyelid complications, such as ectropion and malposition, can be avoided by properly evaluating risk factors (lax tarsoligamentous system, negative vector, previous procedures, prominent globe, thyroid issues, and so on), mitigating these risk factors (by performing a canthopexy or midface augmentation, for example), and removing a minimum of skin.8 With a better understanding of the eyelid anatomy and advances in medical technology, the techniques of LLB have evolved.5 The first approach was described in 1924 by Bourguet for resection of herniated periorbital fat and popularized by Baylis et al in 1989.9,10 Other techniques, such as “subtractive” blepharoplasty and dermal fillers (hyaluronic acid–based), were also introduced for lower eyelid and infraorbital volumizing.11 Several other techniques have also been introduced for better surgical outcomes; injections of botulinum toxin followed by chemical peels and microdermabrasion, and using cysteamine and methimazole to treat periorbital area melasma (especially in Asian people).12,13-,14 In this paper, we review the indications, methods, and complications of different surgical approaches to LLB.
METHODS
Study Selection
To identify relevant papers published up to January 2023, we thoroughly searched the databases of PubMed (National Institutes of Health, Bethesda, MD), Scopus (Elsevier, Amsterdam, the Netherlands), Web of Science (Clarivate, London, UK), Cochrane (Wiley, Hoboken, NJ), and Embase (Elsevier, Amsterdam, the Netherlands). The review utilized medical subject headings (MeSH) and non-MeSH terms. Both the language and the publication schedule were unrestricted. All of the identified records were imported into EndNote before the screening process, and duplicate citations were removed in EndNote to bring the number of records down (Figure 1). The following MeSH terms (keywords) were in the title of the publications derived from this online search: (1) (blepharoplasty); (2) AND (lower lid*); (3) AND ([transconjunct*] OR [transcutan*] OR [tear trough*]). F.N. and S.N. searched Google Scholar, in addition to the databases previously mentioned, utilizing different combinations of the terms “adipose tissue,” “blepharoplasty,” “cheek,” “eyelids,” “festoon,” “lifting,” “plastic surgery procedures,” “subcutaneous fat,” “rejuvenation,” “tear trough deformity,” and “vector.” Finally, to make sure we did not miss any citations, we inspected the reference lists of the selected papers. The study started on June 1, 2022, and concluded on January 31, 2023.
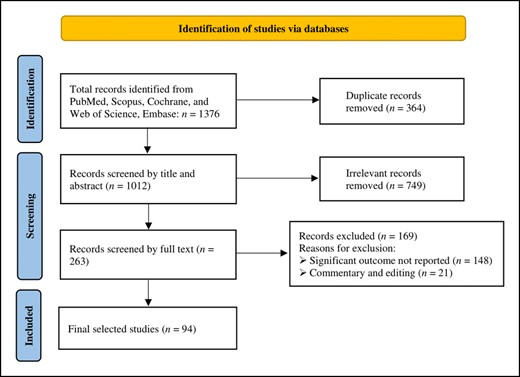
The inclusion and exclusion criteria were as follows. If there were 2 papers published on the same set of patients, only the publication with the higher quality or the greatest number of cases was included. We disregarded the articles not related to the topic and those having the same data sources. Studies that did not report significant outcomes commentaries, and letters to the editor were also excluded. The studies were chosen by 2 independent reviewers (F.N. and S.N.) after applying both the inclusion and exclusion criteria.
RESULTS
Anatomy, Physiopathology, and Aging Changes
The lower eyelid has a moderate S-shaped curve, with the lowest point below the lateral pupil; it contains 2 rows of lashes. The lower eyelid supports lacrimal drainage by pushing tears toward the punctum but plays a minor role in eye closure. Variations in lower lid architecture according to race or ethnicity (such as Asians) should be evaluated before surgery to carefully assess the presence and number of anomalies or changes.15 Two anatomic details important for LLB include, first, the lower eyelid margin positioning, which normally rests at the inferior limbus with no scleral show and with its lowest point slightly lateral to the pupil; and second, the lower eyelid crease, which is approximately 2 mm below the lash line medially and 5 mm below the lash line laterally.
According to Foad Nahai and Farzad Nahai, the lamellae of the lower lid must also be considered.7,16-,20 The anterior lamella of the lower eyelid is made up of a thin layer of skin and pretarsal orbicularis oculi muscle (the orbicularis oculi muscle has 3 subdivisions: pretarsal, preseptal, and orbital parts). The middle lamella includes the orbital septum, orbital fat, and tarsal plate; and the posterior lamella includes the lower eyelid retractors (the inferior tarsal muscle and the capsulopalpebral fascia) and palpebral conjunctiva. The ligaments retain from the bone to the skin, preserving all the elements placed therein, such as the orbicularis oculi.
Lower lid retractors include the capsulopalpebral fascia and the inferior tarsal muscle, which inserts into the tarsal plate. During childhood, the medial and lateral ends of the tarsi fuse at the orbital commissures to the medial and lateral palpebral canthal ligaments or tendons. Most incisions should stop lateral to the punctum; knowledge of anatomy to maintain the neurovascular supply and lymphatic drainage is crucial during LLB.
The marginal arcade, 2 mm from the lid edge, supplies the lower eyelid with blood from the inferior palpebral artery, ophthalmic artery, and lacrimal artery. A maxillary artery branch supplies the lower eyelid; however, the external carotid artery terminal branches vary.21 The lateral half of the lower lid drains into the preauricular lymph node, and the medial half drains into the submandibular nodes.22
The infraorbital nerve, a branch of the maxillary nerve, carries sensory information of the lower lid and the lid–cheek junction from the medial to lateral canthus. Zygomaticofacial nerve branches innervate the lateral canthus. The buccal, zygomatic, and frontal branches of the facial nerve provide motor innervation to the orbicularis oculi muscle, and the oculomotor nerve supplies the lower eyelid retractors.23,24
The lower lid has 3 postseptal fat compartments: nasal (medial), large central, and lateral (temporal). The inferior oblique muscle separates the nasal and central fat pads, and the Lockwood ligament separates the central and lateral fat compartments. The lateral fat pocket includes the retinaculum and canthal tendon.
Inferior displacement of the zygomatico-cutaneous ligament causes lower lid laxity. Atrophic subcutaneous tissue and adjacent fat, including the suborbicularis oculi fat (SOOF) and malar fat pads, cause orbital hollowing, tear trough deformity, and a flattened midface. The SOOF is positioned below the lateral half of the infraorbital rim (at the inferolateral side of the orbit), located beneath the orbital septum and superficial to the periosteum, and deep to the orbicularis oculi muscle above the zygoma.25
The pseudoherniated fat pads of the orbit, caused by the weakened septum, cause the “eye-bag” prominence and herniation of the orbital fat in the lower eyelids (also known as steatoblepharon). It is managed by effacing the lower lid–cheek junction and recreating a smooth transition of the lower lid–cheek interface.20,26
Preoperative Assessment
Ten steps were introduced for the preoperative assessment of candidates for LLB.
Lower lid position and symmetry in primary gaze should be assessed at the limbus.
The lower lid margin should be evaluated for active blepharitis or meibomian gland dysfunction.
The snap-back test should be performed to evaluate lid laxity by pulling the lid inferiorly.
Distraction of the lower lid from the globe should be tested utilizing the thumb and index finger (>2 mm is considered abnormal).
Laxity of the canthal tendons should be tested by pulling the lower lid medially away from the lateral canthus (>2 mm is considered abnormal). Canthal anchoring is recommended if there is even the slightest indication of laxity, despite the remarkably low rate of lower eyelid malposition or retraction following transconjunctival blepharoplasty.
Medial canthal laxity, punctal inversion or eversion, and punctal patency should also be checked.
Lower-lid fat pads (medial, central, and lateral) should be assessed. The presence of the tear trough and lid-cheek junction should be noted.
The relation of eyeball to cheek (orbital vector) should be noted
Skin type (Fitzpatrick score) and changes such as thinning, the position of wrinkles, crow's feet, pigmentation, and festoons also should be distinguished.
A pinch test should be performed.27
Surgical Techniques
Traditional lower blepharoplasty procedures focus on removing skin, muscle, and fat that can result in hollowing and retraction of the eyelids. A paradigm change that favors orbicularis oculi muscle suspension, canthopexy, transposition, septal reset, preservation, or judicious fat excision has recently taken place. As shown in Figure 2, the excess skin and muscle are utilized for choosing between the transconjunctival and transcutaneous approaches. Fat transposition or conservative excision or another adjunct is selected based on the presence of a tear trough deformity and excess skin, as well as the result of the snap-back, malar vector, and lid distraction tests.27
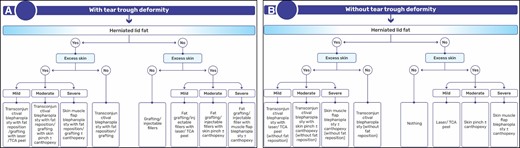
Algorithms for lower lid blepharoplasty based on the presence and extent of the herniated orbital fat pad and excess skin, with (A) and without (B) tear trough deformity.
Transconjunctival Approach
The transconjunctival technique starts with an incision that is made approximately 3 to 5 mm below the inferior tarsal plate and allows direct access to all 3 compartments of the lower eyelid fat pads (by the detachment of the lower lid retractors from the inferior tarsal plate) without the anterior lamella being damaged (Figure 3).28-30 The transconjunctival incision can also be performed through a preseptal or retroseptal approach.
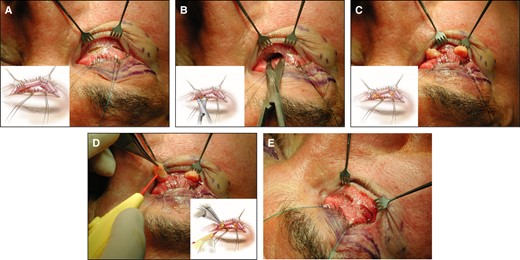
Surgical techniques of transconjunctival approach, dissection, fat exposure, and excision in a 71-year-old male patient. (A) Subtarsal incision and proper exposure (with a sulcus suture and retractor). (B) Access to fat compartment. (C) Orbital fat exposure. (D) Fat resection. (E) Procedure ending with uncovered wound.
For the preseptal technique, a conjunctival incision 2 to 3 mm under the inferior edge of the tarsus is performed, allowing access to the posterior of the septum with a 6 to 7.5 mm cut inferior to the tarsus.31 This approach provides access to the ocular fat pads without visible external scarring.6 The procedure is appropriate for individuals who have restricted lid flexibility and pseudoherniated infraorbital fat, which can render the transcutaneous approach difficult. 28,32
In the retroseptal approach, the dissection plane is accessed by a lower conjunctival incision, 5 mm under the inferior edge of the tarsus.
The preseptal and retroseptal approaches have the advantage of minimal bleeding and fat extrusion into the operating field, and direct access to the inferior orbital fat without wounding the septum, respectively.31,33 However, the 2 approaches have similar risk profiles in practice.34 The number of incisions also is a factor. Yamashita and colleagues reported approximately 5 times higher complication rates with the transconjunctival approach, with repeated incisions as compared to single incisions.35
To protect the cornea and maximize the fat pad exposure (Figure 3), the posterior conjunctival flap is secured cephalad with a traction suture, and the anterior edge of the divided conjunctiva is retracted caudally with a small retractor. The percutaneous or buried absorbable sutures (with similar clinical outcomes and high patient satisfaction) can be used to create a subperiosteal or supraperiosteal pocket for fat repositioning.36 During fat repositioning of the medial and central fat compartments, an elevator is utilized to raise the periosteum over the upper maxilla for approximately 15 mm without injuring the infraorbital nerve. Dissection may be carried out laterally to release the orbital retaining ligament (ORL), based on the extent of fat repositioning, and the lateral fat compartment should be debulked to the level of the orbital rim. The conjunctival incision can be left to heal secondarily or closed loosely with buried 6–0 fast absorbable gut sutures.
After performing the transconjunctival LLB, there are several procedures that can be performed as secondary procedures to maximize results.37
Facial fillers and autologous fat grafting: ideal for patients with tear trough deformity, midfacial lipoatrophy, malar fat pad descent, or malar bony atrophy, with admirable results and minimal complications.38,39
Suture canthopexy: utilized to correct the lateral canthal depression and prevent ectropion, in cases with mild to moderate lid laxity.40 Patients with severe lid laxity (poor snap-back test or >6 mm distraction of lid from the globe) and/or preoperative ectropion should undergo ectropion repair through lateral tarsal strip canthoplasty or canthopexy, a lid-shortening technique.41
Malar/cheek lateral suspension: utilized for the suspension of the preseptal orbicularis, lifting the SOOF and the subperiosteal midface.
Skin resurfacing (chemical peeling or CO2 and erbium YAG laser): mainly utilized to improve thin and wrinkled skin appearance and dark pigmentation of the lower lid; applicable for patients with Fitzpatrick skin types I to III.8,13
The pinch technique:27,42 utilized for wrinkles and skin redundancy when resurfacing is contraindicated, ie, in patients with moderate skin excess and Fitzpatrick types IV to VI. This procedure is applied after the transconjunctival portion is completed. After defining the horizontal fold of skin in the pretarsal area with the Brown-Adson forceps, approximately 1 to 2 mm below the lash line, which can extend from the medial canthus to the lateral orbital rim, the fold (containing skin and little or no muscle) is crushed with a straight hemostat and excised with Westcott scissors (Acme United Corp., Fairfield, CT), and the skin is closed with 6–0 Prolene (Ethicon, Cornelia, GA) in a running fashion. High patient satisfaction (94%) is reported when the pinch technique is combined with fat excision, laser resurfacing, and sometimes fat transfer.
Botulinum toxin injection: treats the crow's feet area.43-45
In various studies, surgeons have utilized the combination of 1 or more of these techniques in addition to the transconjunctival approach, and they have reported different patient satisfaction and complication rates. For example, Rohrich and colleagues (2011) described the results of 5 combinations for LLB, which included fat injection for augmentation of the deep malar fat, transconjunctival fat excision, and release of the trough ligament, lateral canthopexy, and skin pinch/flap.46 Rohrich and Mohan (2020) also characterized a 6-step method that included deep malar fat augmentation, transconjunctival removal of lower postseptal fat, ORL release, lateral retinacular canthopexy, skin pinch resection, and fractionated fat injection.47
Overall, the transconjunctival approach is preferred for young patients with isolated fat prolapse (no skin excess).7 In patients with excess skin, a minimal transcutaneous approach or pinch technique can be combined with the transconjunctival approach to achieve a better result.33
Transcutaneous Approach
Skin flap and skin-muscle flap are two of the most widely utilized approaches in the transcutaneous technique. Skin-muscle flap is a time-tested technique, with approved safety and effectiveness over 30 years, and is considered optimal for redraping lower eyelids with significant excess skin and muscle tissue.48 This technique, originally described by Castanares (1951), is performed by creating a skin-muscle flap below the lash line through a subciliary incision, preserving the underlying pretarsal orbicularis muscle.11 The orbicularis is resuspended along the lateral orbital rim; excess skin is excised conservatively, and the incision is closed carefully.27,49 Various modifications have been recommended for this traditional method of transcutaneous LLB, such as the placement of a skin incision inferior to the tarsal margin to preserve a pretarsal orbicularis oculi muscle cuff, which can improve blinking and tear drainage.50 The advantage of the transcutaneous skin-muscle flap approach is the selective subperiosteal release of the orbicularis retaining ligament, and/or a simultaneous midface lift for improved appearance of the lid-cheek junction, debulking, or repositioning fat pads.
An alternative to this method is the skin-flap method, a conservative removal of excess skin without disruption to the underlying orbicularis, for which the dissection goes between the lower eyelid skin and the orbicularis muscle. The fat-preserving technique is another technique for strengthening the herniated fat by pushing it back into orbit and suturing the capsulopalpebral fascia to the inferior orbital rim.51
For a comprehensive review, Table 1 presents the indications, contraindications, and complications of transcutaneous and transconjunctival LLB procedures.6,8,48,52-66 To date, no randomized clinical trials have been published comparing the outcomes and complications of different techniques, which limits evidence-based comparison for definitive conclusions about the surgical techniques of LLB.53
Transcutaneous and Transconjunctival Lower Lid Blepharoplasty (LLB): Comparison of Indications, Contraindications, and Complications
| LLB Technique . | Transconjunctival LLB . | Transcutaneous LLB . |
|---|---|---|
| Indications |
|
|
| Contraindications | Similar to other elective and/or aesthetic surgical procedures54 | |
| Complications |
|
|
| LLB Technique . | Transconjunctival LLB . | Transcutaneous LLB . |
|---|---|---|
| Indications |
|
|
| Contraindications | Similar to other elective and/or aesthetic surgical procedures54 | |
| Complications |
|
|
Transcutaneous and Transconjunctival Lower Lid Blepharoplasty (LLB): Comparison of Indications, Contraindications, and Complications
| LLB Technique . | Transconjunctival LLB . | Transcutaneous LLB . |
|---|---|---|
| Indications |
|
|
| Contraindications | Similar to other elective and/or aesthetic surgical procedures54 | |
| Complications |
|
|
| LLB Technique . | Transconjunctival LLB . | Transcutaneous LLB . |
|---|---|---|
| Indications |
|
|
| Contraindications | Similar to other elective and/or aesthetic surgical procedures54 | |
| Complications |
|
|
In the study by Rancati and colleagues on 117 patients, approximately half receiving each method and followed for 24 months, the surgeons reported that the transconjunctival technique was faster and easier, with lower complication rates and higher patient satisfaction than the transcutaneous technique.
Several studies have reported the outcome of the combined methods. Jung and colleagues have reported no complications, no recurrence, and favorable aesthetic outcomes in 453 patients who underwent LLB with a septo-capsulopalpebral fascial recession flap, which included skin incision, maintenance of pretarsal muscular roll, skin-muscle flap elevation, orbital septum release, orbital fat removal, septo-capsulopalpebral recession flap, skin excision, and closure.67
Adjuncts that can enhance the outcome of lower blepharoplasty and prevent complications should be individualized (canthal suspension; canthoplasty or canthopexy, ie, eyelid tightening; and fat repositioning, preservation, or resection.)37
Approach to Tear Trough Deformity
In elder patients with herniated orbital fat pads, the presence and extent of infraorbital rim hollowing, caused by age-related subcutaneous volume loss, should be evaluated. A hollow undereye is caused by orbital and malar rim retrusion, whereas fat herniation may make the lid-cheek junction worse.39
The medial infraorbital rim hollowing, also known as a tear trough deformity, is a result of subcutaneous thinning of the eyelid skin. The lateral plane, called the palpebromalar or lid-cheek junction, may also have infraorbital rim hollowing, causing hollowing of the entire lower lid rim.
The tear trough deformity, as defined by Loeb (1993), has 3 components: (1) a fixed orbital septum and arcus marginalis medially below the orbicularis oculi muscle; (2) the “triangular gap” formed by the junction of the orbicularis oculi muscle and the lateral nasal musculature; and (3) the absence of fat and soft tissue, resulting in a hollow sunken medial lower eyelid.68
The septal reset is recommended for patients with severe tear trough deformity, because the fibrous tissue layer of the septum acts as a barrier for orbital fat, allowing better sutures and more secure repositioning below the infraorbital rim.69 In the septal reset approach (as described by Hamra), a transcanthal canthopexy (which will be discussed further) stabilizes the lid margin and momentarily sets the orbital septum at the arcus marginalis level free, and the septum is subsequently fixed to the inferior orbital rim.40
DISCUSSION
Meticulous Fat Management
Fat management plays an important role in the rejuvenation of the lower lid. The fat pads of the lower lid enlarge with increasing age. Figure 2 describes the algorithmic approach for patients with herniated orbital fat pads. Fat pads that herniated anterior to the orbital rim need debulking and/or repositioning, depending on fat and volume loss along the infraorbital rim.
In patients with significant pseudoherniation of the lower-lid fat pads, because the risk of denervation of the orbicularis muscle and insufficient anterior lamella is higher in the skin-muscle flap transcutaneous approach, isolated transconjunctival LLB is considered an appropriate method, resulting in reduced double convexity and smoother lower eyelid contour.
The preservation of fat is a recent modification (developed in the past decades) to the early LLB, which utilized fat debulking and removal. Loeb and later Hamra introduced fat transposition for the correction of tear trough deformity, untoward lid-cheek junction, and/or palpebromalar sulcus by releasing the ORL and medial orbicularis oculi attachments.70,71
Fat transposition can be also performed through a transconjunctival approach, during which the pseudoherniated fat is blended into the malar-cheek mound. Comparative studies have also shown the appropriateness of ORL release in patients with tear trough deformity, utilizing the transconjunctival approach.72,73
To determine where and how much fat should be removed, the surgeon’s judgment and expertise are essential.11,39,68,70,71,74-81 To smooth the lid-cheek junction during lower blepharoplasty, fat grafting is frequently employed.
Loeb et al suggested employing fat grafting to manage lower eyelid depression as well as pushing the postseptal fat pads into the face.68,70 Some cosmetic surgeons favor utilizing diluted fat (70% fat mixed with saline and infranatant fluid as diluent) to boost volume and address undereye hollowing.82
Huang et al suggested employing microautologous fat grafts in the tear trough and medial canthus to replace the excision of all 3 postseptal fat pads.83 Despite having outstanding cosmetic results, grafting may take some time, needs a donor location and, combined with other blepharoplasty methods, can be challenging.82
In many situations, lower blepharoplasty is performed as a subsequent operation because the lower eyelids continue to droop, most often in the lateral fat compartment. Because of the arcuate expansion, the lower eyelid's lateral fat pad is higher up and separate from its medial and central sections. As a result, both subciliary (a transcutaneous incision in the subciliary crease) and transconjunctival blepharoplasty techniques tend to disregard this compartment, despite the fact that it is one of the bigger contributors to fat herniation. As a solution, Tran et al installed a “septal window” for fat management during lower blepharoplasty that makes it easier to remove more fat (especially lateral fat pad) during septal reset, resulting in a clean lid-cheek junction without impairing arcuate extension.84
As fat is resected or repositioned care must be taken to evaluate bulging and/or hollowing by applying gentle pressure on the upper eyelid over the globe. External sutures or tension-free internal fixation with absorbable sutures can be utilized for the periosteum below the orbital rim. The key to successful surgery is selective removal, repositioning, or redraping of deep, periorbital fat into areas of volume deficiency.36 To determine the type of procedure and method of fat management, it is necessary to examine the changes in the periorbital region. In the majority of cases, the results are enhanced when these procedures are performed concurrently.
Suborbicularis Oculifat Lift
Freeman introduced the combination of a SOOF lift with transconjunctival LLB on 64 patients (cadavers) and reported excellent results, with high safety and reliability.85 His dissection was performed on a preseptal plane inferior to the infraorbital rim bone. He incised the exposed arcus marginalis along the medial half of the rim, which released the ORL and enabled a supraperiosteal dissection beyond the inferior border of the tear trough deformity. The exposed SOOF pad was suspended to the infraorbital periosteum utilizing a horizontal mattress suture. However, in this technique, the bulk of the SOOF below the lateral half of the bony infraorbital rim, which can result in an unfavorable aesthetic outcome, is not considered.
Further refinements of midface lift methods over the past decade have suggested fat repositioning of the midface on the infra-SOOF line.86,87 Therefore, this technique was not widely utilized. After the introduction and popularization of the transcutaneous technique for LLB, the SOOF lift is preferably performed through the open skin-muscle flap approach.
Management of Involutional Ectropion
Orbicularis and horizontal lid tightening are frequently used to treat lid laxity, regardless of the transcutaneous or transconjunctival technique. Evidence showed that patients with a negative vector (a posterior positioning of the orbital rim related to the corneal surface) are at a higher risk for lower lid malposition after LLB.88 Cases with lid laxity should undergo skin excision with great caution. A combination of the procedure with canthal adjustment is recommended in such patients, depending on the amount of lid laxity.
If there is little (1-2 mm) lid laxity, the lateral canthus can be raised by suture canthopexy. A lateral retinacular canthopexy may be more appropriate to lift the lateral canthal tendon over the upper lateral rim if there is evidence of moderate (3-6 mm) laxity.89 For improved mobility, lateral canthoplasty with lateral cantholysis may be required for excessive lower lid laxity (>6 mm).89,90 A lateral tarsal strip is an additional option in the these groups.
A 5- to 7-mm cut is created in the lateral canthal tissue opening 5 mm lateral to the lateral commissure in the simplified technique for lateral canthal tendon canthopexy.91 The interior segment of the orbital rim periosteum may be seen when cutting along the path of the lateral orbital rim to Whitnall's tubercle, and a 4.0 polydioxanone suture (PDS) with a P2 needle passing through the periosteum, underneath the orbital rim, and above the tubercle results in the proper height. Refraining from damaging the eyelid margin or lateral canthal angle, it is then vertically passed between the lateral margin of the lower eyelid tarsus and medial tip of the lateral canthal tendon. The lower eyelid can be raised to the appropriate level to seal the skin after the interrupted, embedded 6-0 poliglecaprone suture has sealed the orbicularis layer.
During inferior retinacular lateral canthoplasty (transcantho-canthopexy), an upper blepharoplasty incision is created on the lateral canthus throughout the lower retinacular lateral canthoplasty, and the lower crux on the lateral canthal tendon is then relocated. The tendon is then attached to the lateral orbital rim periosteum. However, this method includes an extensive incision behind the lateral canthal tendon, and poses the potential of intraoperative overcorrection and protracted edema, resulting in reduced tightness and longevity in the lower eyelids.
For inferior retinacular suspension a 1-mm lower eyelid incision is performed in addition to the blepharoplasty incision, and sutures are inserted beneath the lateral canthal tendon. The lateral canthus tendon (LCT), orbicularis oculi muscle, and skin are lifted in the dermal orbicular pennant procedure before an opening in the skin is made to see the tendon. The structures are rejoined at the height of the upper pupillary margin when the LCT separates from the orbital rim. The method decreases the length gap and drop of the upper eyelid; however, the original anatomy is irregular due to the extensive cut and innate laxity of the orbicularis oculi muscle.
The orbicularis oculi muscle is elevated near the lateral orbital rim during lateral canthal resuspension sine canthotomy, and Stevens scissors (Integra LifeSciences, Plainsboro, NJ) are put beneath the muscle. The next step is a vertical spreading, which releases the superficial lateral palpebral, zygomatic malar, and orbitomalar ligaments. A 4.0 PDS stitch is then used to secure the periosteum and lateral canthal tendon inside the orbital rim. Even though the upper and lower eyelids are not imbricated, due to extensive cutting and disturbance of surrounding anatomy this technique is not recommended for individuals with facial nerve palsy or floppy eyelid syndrome.
In the locking-Y lateral canthopexy with osseous integration technique, a 5-0 monofilament polypropylene stitch is positioned below the superficial lateral canthal tendon alongside a second inferior needle placed across the inferior crus. Two drill holes are made into the zygomatic bone, and sutures are passed under the inferior and superior lateral canthal tendons. This method prevents the cheese-wiring effect because the stitches are inserted into bone instead of periosteum, despite being more invasive and requiring drilling of the zygomatic bone.92
Canthotomy is the first step in the lateral tarsal strip (LTS) procedure. After the epithelium is removed to create a tarsal strip, the tarsus is connected to the lateral orbital periosteum. Although this method has increased correction and durability, it also reduces the horizontal palpebral aperture in a cosmetically undesirable way, requires more surgical alteration, takes longer to complete, and raises the chance of imbrication.
CONCLUSIONS
The anatomic landmarks and approaches of the LLB were reviewed, with consideration of the incision site, tear trough deformity, desired vector, dissection planes, and fixation method. Furthermore, the different aspects of the two most utilized techniques for LLB were explained thoroughly, including their indications and contraindications, surgical techniques, adjunct techniques, complications, and management. Several adjunct methods have been proposed for various indications with proven safety and efficacy in interventional studies; however, most studies lack comparison groups and randomization. More research is needed to determine the advantages and disadvantages of transcutaneous vs transconjunctival surgery and the benefits and risks of various fat repositioning and augmentation techniques.
Acknowledgments
Thanks to Glenn Floyd for his expertise and assistance throughout editing of the manuscript. Drs Farzad Nahai and Feizollah Niazi made an equal contribution to this work as first coauthors.
Disclosures
The authors declared no potential conflicts of interest with respect to the research, authorship, and publication of this article.
Funding
The authors received no financial support for the research, authorship, and publication of this article.
REFERENCES
Author notes
Dr Farzad Nahai is a plastic surgeon in private practice in Atlanta, GA.
Dr F. Niazi is an associate professor, Department of Plastic and Reconstructive Surgery, Research Center of Modarres Hospital, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
Dr Foad Nahai is a professor, Division of Plastic and Reconstructive Surgery, Emory University School of Medicine, Atlanta, GA and is the editor in chief of Aesthetic Surgery Journal.
Dr S. Niazi is a researcher, Ophthalmic Research Center, Research Institute for Ophthalmology and Vision Science, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
Dr Foster is a professor, Ophthalmic Surgeons and Consultants of Ohio, Columbus, OH.
Dr Doroodgar is an adjunct professor, Negah Aref Ophthalmic Research Center, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
Dr Baradaran-Rafii is a professor, Department of Ophthalmology, University of South Florida Morsani College of Medicine, Tampa, FL.
Dr Rashidi is a professor, Department of Ophthalmology and Visual Neurosciences, University of Minnesota, Minneapolis, MN.



