-
PDF
- Split View
-
Views
-
Cite
Cite
Farhad Hafezi, Sholeh Jahanshahi, Commentary on: Concha-Type Microtia: New Surgical Incision, Aesthetic Surgery Journal, Volume 43, Issue 11, November 2023, Pages NP823–NP824, https://doi.org/10.1093/asj/sjad241
Close - Share Icon Share
See the Original Article here.
Successful reconstruction of concha-type microtia requires meticulous carving of a cartilaginous framework and the creation of a thin, stable, and smooth skin coverage. The texture and quality of the skin are of prime importance in determining the final shape and contour of the 3-dimensional framework and a sufficient amount of intact skin is a crucial factor in achieving the ideal result.
When reconstructing congenital concha-type microtia, excess skin is typically available which can be used for the framework envelope; however, in traumatic cases, and particularly in burn patients, this is less pliable due to scarring. These limitations affect the size and the type of incision for framework insertion.
In this article,1 a 2-phase Nagata approach was presented for the reconstruction of the deficient helix, anti-helix, and scapha. The procedure was implemented in a total of 33 patients, consisting of 23 concha losses and 10 congenital cases. Two scalp incisions were executed for the insertion of the cartilaginous framework and it was rationalized that this procedure is superior to the Nagata W-incision.
Dr Satoru Nagata first introduced this 2-stage method in 1990.2,3 The procedure gradually gained popularity and was eventually accepted as an alternative to the Brent 4-stage method. Nagata divided microtia into 3 subgroups: lobule type, small concha type, and concha type.2,4 In the Nagata small concha type, concha is lacking, and instead, a vestigial cartilage is present. In these, as well as in congenital cases, the skin incision is first made along the margin of the cartilage remnants to remove the vestigial cartilage and then the incision is continued as a W-plasty which provides a larger pocket for the insertion of the new framework.
Concha-type microtia is typically found in trauma or burn patients for whom the covering skin is insufficient and not intact and often contains unfavorable scars. It is desirable to avoid the scar area and preferably make the incision at a distance from the scar and camouflage it in the hair-bearing scalp.
In this manuscript,1 the authors selected congenital and secondary microtia cases that were originally classified by Nagata as concha type. Nagata in 1994 described the skin incision for these deformities as a Z-plasty with a posterior V-shaped incision.4 He recently changed the posterior V-shaped incision to a W-shaped incision.5
Although the authors constructed a perfect framework, their 2 incisions were visible and extended over the framework as shown in Video 61 of their manuscript. The result, therefore, is not desirable and contradicts the goals of the authors. Also, the pressure and ischemia of the covering skin with overlaying scar makes the cartilage prone to exposure, infection, and resorption, leading to suboptimal results. In another report of 230 autologous auricular reconstructions, 15 cases with cartilaginous exposure were reported.6
In our experience, in concha-type microtia, when there is no need to construct the tragus or rotate the lobule to a new position, 1 scalp incision is usually adequate for insertion and adjustment of the cartilaginous framework. This can in particular be executed in both traumatic and burn patients in whom the covering skin is not of ideal quality (Figure 1).
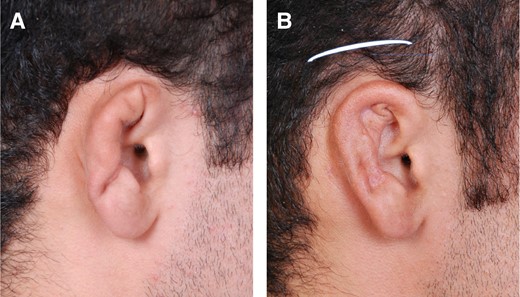
(A) Concha-type ear deformity. (B) Single incision used to insert and adjust framework in place.
In conclusion, it seems that the cartilaginous framework in concha-type microtia, either congenital or traumatic, can be inserted through 1 incision in the superior hair-bearing area of the scalp. This incision is usually sufficient for both safe framework insertion and adjustment. It is also safer to keep the incision away from the pocket and to avoid extending it over the framework to achieve a better aesthetic result and reduce the chance of visibility, dehiscence, and framework exposure.
Disclosures
The authors declared no potential conflicts of interest with respect to the research, authorship, and publication of this article.
Funding
The authors received no financial support for the research, authorship, and publication of this article, including payment of the article processing charge.
REFERENCES
Author notes
Dr Hafezi is a professor of plastic surgery, Iran University of Medical Sciences, St Fatima Hospital and Burn Research Center, Tehran, Iran.
Dr Jahanshahi is a surgical and clinical pathologist, Jahan Koodak Laboratory, Tehran, Iran.



