-
PDF
- Split View
-
Views
-
Cite
Cite
Alisha B Paranzino, Jason Sims, David S Kirn, Safety and Efficacy of Outpatient Drainless Abdominoplasty: A Single-Surgeon Experience of 454 Consecutive Patients, Aesthetic Surgery Journal, Volume 43, Issue 11, November 2023, Pages 1325–1333, https://doi.org/10.1093/asj/sjad167
Close - Share Icon Share
Abstract
The incidence of seroma after abdominoplasty is accepted as approximately 10% (with a range) in the literature. Progressive tension sutures (PTS) have arisen as a means of reducing seroma, however there are conflicting data regarding their efficacy.
The primary aim of this study was to describe the incidence of postabdominoplasty seroma in the setting of drainless abdominoplasty with PTS.
A retrospective chart review was performed of all abdominoplasties (n = 454) during a 20-year period. At approximately the halfway point of this time frame, the abdominoplasty technique was changed from the use of 2 drains to the use of PTS without drains. Additionally, pulsed electromagnetic field therapy (PEMF) and liposomal bupivacaine (Exparel, Pacira Pharmaceuticals, Inc., Parsippany, NJ) were added as pain control adjuncts.
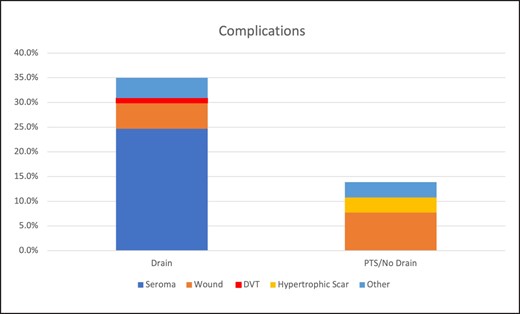
There were 194 patients in the drain group and 260 patients in the PTS/no drains group. The group without drains contained a significantly higher proportion of massive weight loss patients (4.1% vs 9.2%, P = .041). The majority of the group without drains underwent outpatient surgery (89.7% vs 98.8%, P < .001). The overall complication rate was significantly lower in the no drains group (31.4% vs 13.8%, P < .001). The incidence of seroma was dramatically reduced in the group without drains (24.7% vs 0.0%, P < .001).
PTS are highly effective in preventing seroma and can be safely employed as an alternative to drains in abdominoplasty. PEMF may play a role in seroma prevention and is also helpful for pain control. With these techniques to mitigate complications and minimize postoperative pain, abdominoplasty can be performed safely and effectively in a purely outpatient setting.

Abdominoplasty is one of the most frequently performed procedures in aesthetic surgery and is generally regarded as having a favorable risk profile. Although the most devastating complication is often cited as venous thromboembolism (VTE) or pulmonary embolism (PE), the most common is seroma formation. Incidence of seroma after abdominoplasty is accepted as approximately 10% with a large range in the literature.1-4 The sequelae of seroma can vary from a mild asymptomatic fluid collection to infection, wound dehiscence, flap necrosis, and pseudobursa formation.
Previously described mechanisms for preventing seroma formation include tissue sealants, avoiding liposuction, minimizing electrocautery, endoscopy, prolonged drains, sclerotherapy, immobilization, and compression dressings.1,5,6 Progressive tension sutures (PTS) have developed as another means of controlling fluid accumulation, however there are conflicting data regarding their efficacy.1,7-12 The primary aim of this study was to describe the incidence of postabdominoplasty seroma when forgoing traditional closed-suction drains in favor of PTS.
METHODS
A retrospective chart review was performed of all abdominoplasties (n = 454) performed by D. S. K. during a 20-year period (January 1999 through December 2019). At approximately the halfway point of this time frame (May 2010), the abdominoplasty technique changed from the use of 2 drains to the use of PTS without drains. Additionally, pulsed electromagnetic field therapy (PEMF) and liposomal bupivacaine (Exparel, Pacira Pharmaceuticals, Inc., Parsippany, NJ) were added as pain control adjuncts, in November 2010 and March 2013, respectively. There was also a trend toward increased outpatient surgery during this time.
The analyzed data included patient demographics, surgical location, simultaneous procedures, complications, and interventions. Wound complications were defined as any occurrence that required additional intervention, including dressing changes, debridement, or reoperation. Complications were categorized as deep venous thrombosis (DVT), seroma, hypertrophic scar, wound healing complications (dehiscence, fat necrosis, infection, pain) and other (cellulitis, pain, hematoma, fat necrosis, perforated diverticulum). Patients with multiple complications were included in all applicable groups.
Categorical and binary variables were reported as counts and percentages of groups. Variables between groups were compared with chi-square or Fisher's exact test as appropriate. Continuous variables were reported as means and standard deviations and compared between groups with analysis of variance (ANOVA) or t tests. Significance was set at P < .05. All statistics were calculated with SPSS statistical software version 28 (IBM Corp., Armonk, NY).
Surgical Technique
All patients were marked in the preoperative holding area in a standing position. The inferior incision was generally designed below the abdominal skin crease, at the superior border of the pubic hairline and extended laterally (Figure 1). When performed concomitantly, power-assisted liposuction was performed with a superwet technique before flap elevation and was generally limited to the flanks and hips. No liposuction of the flap was conducted in any case. Dissection was carried out with electrocautery in the prefascial plane. Lateral dissection was limited to preserve intercostal perforators. Above the umbilicus, dissection was performed centrally to the level of the xiphoid process. Plication was performed to address diastasis recti with running nonabsorbable suture (Figure 2). During the first portion of the series, closed-suction 15-French Blake drains (Medline Industries, Inc., Northfield, IL) were placed through separate stab incisions.

Typical preoperative abdominoplasty markings demonstrated on a 66-year-old female patient. Inferior incision designed below the abdominal skin crease at the superior border of the pubic hairline and extended laterally.
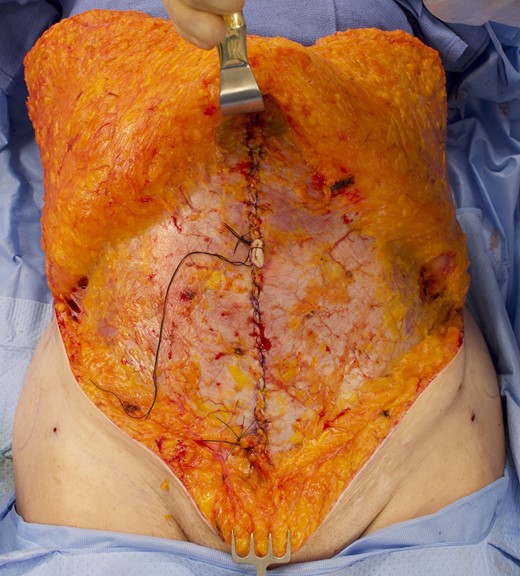
Intraoperative photograph of the same 66-year-old female patient shown in Figure 1. Prefascial dissection performed centrally to the level of the xiphoid process. Plication to address diastasis recti utilized running nonabsorbable suture.
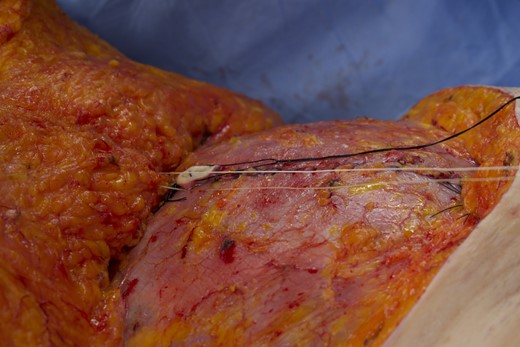
During the second portion of the series, progressive tension sutures were placed to obliterate the space typically evacuated by drains. With interrupted no. 1 Vicryl (Ethicon, Somerville, NJ) suture, Scarpa's fascia was anchored to the rectus fascia. The surgeon's nondominant hand provided tension while the dominant hand directed the suture needle according to the method described by Pollock.7 Approximately 10 to 15 sutures were placed sequentially, beginning in the subxiphoid region and proceeding caudally. A series of 4 PTS sutures were placed to anchor Scarpa's fascia to the abdominal wall fascia at the base of the umbilicus (Figure 3). The umbilical stalk was only anchored to the flap skin. Sutures in the midline were placed under controlled tension to advance the flap caudally and spaced at 2- to 3-cm intervals (Figure 4). Sutures placed lateral to the midline were under minimal to no tension and spaced at 2- to 3-cm intervals. The hallmark of a PTS suture correctly placed through Scarpa's fascia was that the suture alone would advance the flap, without need for the surgeon or assistant to push the flap down.
Intraoperative photograph of the same 66-year-old female patient. A series of 4 PTS sutures were placed to anchor Scarpa's fascia to the abdominal wall fascia at the base of the umbilicus. The umbilical stalk was only anchored to the flap skin.

Intraoperative photograph of the same 66-year-old female patient. Sutures in the midline were placed under controlled tension to advance the flap caudally and obliterate the space typically evacuated by drains. A hallmark of a PTS suture correctly placed through Scarpa's fascia is that the suture alone advances the flap, without the need for the surgeon or assistant to push the flap down.
Before placement of progressive tension sutures, liposomal bupivacaine (Exparel) was infiltrated locally for long-acting pain control. Exparel was placed around the entire perimeter of the zone of dissection at 1-cm interval injection points into the fascia, along the zone of midline plication at 1-cm intervals, and laterally at the border of the external oblique muscle. Additionally, Exparel was infiltrated into the fascia at each progressive tension suture point.
A stirrup-shaped incision was created for the umbilicus at the level of the iliac crest. The Scarpa's fascia around the perimeter of the umbilical tunnel was attached to the abdominal wall fascia with 4 sutures of 2-0 Vicryl. At the skin, the umbilicus was inset with buried dermal sutures of 4-0 Monocryl (Ethicon, Somerville, NJ) and running subcuticular 5-0 Monocryl. The final umbilical inset is demonstrated in Figure 5.
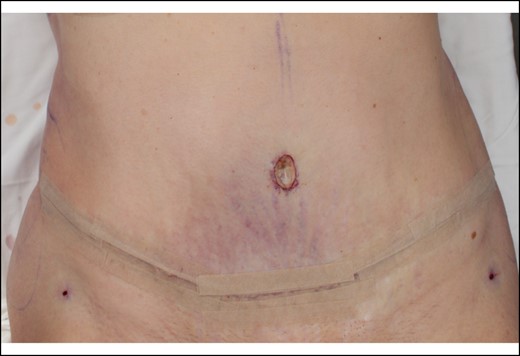
Intraoperative photograph of the same 66-year-old female patient. Umbilicus inset with a stirrup-shaped incision at the level of the iliac crest. Scarpa's fascia around the perimeter of the umbilical tunnel was attached to the abdominal wall fascia.
Ultimately the incisional closure was performed under minimal tension with a multilayered approach with absorbable suture. Deep closure involved the use of 0 Vicryl to place 3-point sutures between Scarpa's fascia on each side of the incision and the deep fascia. The skin was closed with running subcuticular 2-0 Monocryl. No buried dermal sutures were utilized.
Dressings included an abdominal binder (Dale Medical Products, Franklin, MA) and a pulsed electromagnetic field therapy device (SofPulse; Endonovo Therapeutics, Woodland Hills, CA), as seen in Figure 6. SofPulse applies targeted microcurrents to tissue to help reduce edema and recovery time. The levels of microcurrent are 1000 times lower than those emitted by a mobile phone.13 The device costs approximately $200 and consists of a noninvasive disposable coil applicator which is placed external to the abdominal binder.14 The treatment depth is approximately 12 cm and works through dressings and clothing without skin contact. The lightweight battery-powered applicator employs a programmed mode to deliver 15 minutes of pulsed electromagnetic field therapy every 2 hours for a total of 100 treatments; therefore patients receive approximately 8 days of postoperative therapy. The PEMF signal consists of a 2-millisecond burst of 27.12-MHz radiofrequency sinusoidal waves repeating at 2 bursts/second.

Intraoperative photograph of the same 66-year-old female patient. Dressings included a pulsed electromagnetic field therapy device (SofPulse) applied external to the binder.
D. S. K.'s practice has evolved to comprise primarily outpatient surgery with early ambulation and prompt return to activity. Chemoprophylaxis for thromboembolism prevention was not utilized before release of the American Society of Plastic Surgeons (ASPS) consensus recommendations in 2011.15 Following release of those guidelines, indications for chemoprophylaxis were determined according to the 2005 Caprini risk assessment model, with chemoprophylaxis being administered for those with a score of 7 or higher.
RESULTS
The total number of patients included was 454. As shown in Table 1, there were 194 patients in the drain group and 260 patients in the progressive tension suture/no drains group. In the drain cohort, no patients received Exparel or PEMF therapy. These adjuncts were added shortly after the transition to drainless technique. In the PTS/no drains cohort, 189 patients (72.7%) received Exparel. The remaining patients received no local anesthetic. In the PTS/no drains cohort, 252 patients (96.9%) received PEMF therapy.
| . | Drains . | . | PTS/no drains . | . | All patients . | . | P value . |
|---|---|---|---|---|---|---|---|
| No. of patients | 194 | 260 | 454 | ||||
| Dates | 3/29/1999–5/20/2010 | 6/15/2010–11/14/2019 | 3/29/1999–11/14/2019 | ||||
| Patients: | |||||||
| Average age | 40.2 | SD 9.4 | 43.7 | SD 10.2 | 42.2 | SD 10.0 | <.001 |
| Average BMI | 25.5 | SD 4.5 | 26.0 | SD 4.6 | 25.8 | SD 4.6 | .331 |
| Massive weight loss (>100 lb) | 8 | 4.1% | 24 | 9.2% | 32 | 7.0% | .041 |
| Males | 7 | 3.6% | 4 | 1.5% | 11 | 2.4% | .218 |
| Type of procedure: | .319 | ||||||
| Full | 159 | 82.0% | 212 | 81.5% | 371 | 81.7% | |
| Modified | 23 | 11.9% | 33 | 12.7% | 56 | 12.3% | |
| Mini | 9 | 4.6% | 12 | 4.6% | 21 | 4.6% | |
| Fleur-de-lis | 0 | 0.0% | 3 | 1.2% | 3 | 0.7% | |
| Belt lipectomy | 2 | 1.0% | 0 | 0.0% | 2 | 0.4% | |
| Revision | 1 | 0.5% | 0 | 0.0% | 1 | 0.2% | |
| Liposuction | 146 | 75.3% | 220 | 84.6% | 366 | 80.6% | .016 |
| Additional procedures | 113 | 58.2% | 159 | 61.2% | 272 | 59.9% | .562 |
| Liposomal bupivacaine (Exparel) | 0 | 0.0% | 189 | 72.7% | 189 | 41.6% | <.001 |
| PEMF | 0 | 0.0% | 252 | 96.9% | 252 | 55.5% | <.001 |
| PTS | 1 | 0.5% | 260 | 100.0% | 261 | 57.5% | <.001 |
| Surgical setting: | <.001 | ||||||
| Full admission | 17 | 8.8% | 3 | 1.2% | 20 | 4.4% | |
| Observation | 3 | 1.5% | 0 | 0.0% | 3 | 0.7% | |
| Outpatient | 174 | 89.7% | 257 | 98.8% | 431 | 94.9% | |
| Complications: | 61 | 31.4% | 36 | 13.8% | 97 | 21.4% | <.001 |
| DVT | 2 | 1.0% | 0 | 0.0% | 2 | 0.4% | .182 |
| Seroma | 48 | 24.7% | 0 | 0.0% | 48 | 10.6% | <.001 |
| Wound | 10 | 5.2% | 20 | 7.7% | 30 | 6.6% | .342 |
| Hypertrophic scar | 0 | 0.0% | 8 | 3.1% | 8 | 1.8% | .012 |
| Other | 8 | 4.1% | 8 | 3.1% | 16 | 3.5% | .612 |
| Average visits to resolve | 4.1 | SD 3.8 | 2.6 | SD 2.8 | 3.6 | SD 3.5 | .041 |
| . | Drains . | . | PTS/no drains . | . | All patients . | . | P value . |
|---|---|---|---|---|---|---|---|
| No. of patients | 194 | 260 | 454 | ||||
| Dates | 3/29/1999–5/20/2010 | 6/15/2010–11/14/2019 | 3/29/1999–11/14/2019 | ||||
| Patients: | |||||||
| Average age | 40.2 | SD 9.4 | 43.7 | SD 10.2 | 42.2 | SD 10.0 | <.001 |
| Average BMI | 25.5 | SD 4.5 | 26.0 | SD 4.6 | 25.8 | SD 4.6 | .331 |
| Massive weight loss (>100 lb) | 8 | 4.1% | 24 | 9.2% | 32 | 7.0% | .041 |
| Males | 7 | 3.6% | 4 | 1.5% | 11 | 2.4% | .218 |
| Type of procedure: | .319 | ||||||
| Full | 159 | 82.0% | 212 | 81.5% | 371 | 81.7% | |
| Modified | 23 | 11.9% | 33 | 12.7% | 56 | 12.3% | |
| Mini | 9 | 4.6% | 12 | 4.6% | 21 | 4.6% | |
| Fleur-de-lis | 0 | 0.0% | 3 | 1.2% | 3 | 0.7% | |
| Belt lipectomy | 2 | 1.0% | 0 | 0.0% | 2 | 0.4% | |
| Revision | 1 | 0.5% | 0 | 0.0% | 1 | 0.2% | |
| Liposuction | 146 | 75.3% | 220 | 84.6% | 366 | 80.6% | .016 |
| Additional procedures | 113 | 58.2% | 159 | 61.2% | 272 | 59.9% | .562 |
| Liposomal bupivacaine (Exparel) | 0 | 0.0% | 189 | 72.7% | 189 | 41.6% | <.001 |
| PEMF | 0 | 0.0% | 252 | 96.9% | 252 | 55.5% | <.001 |
| PTS | 1 | 0.5% | 260 | 100.0% | 261 | 57.5% | <.001 |
| Surgical setting: | <.001 | ||||||
| Full admission | 17 | 8.8% | 3 | 1.2% | 20 | 4.4% | |
| Observation | 3 | 1.5% | 0 | 0.0% | 3 | 0.7% | |
| Outpatient | 174 | 89.7% | 257 | 98.8% | 431 | 94.9% | |
| Complications: | 61 | 31.4% | 36 | 13.8% | 97 | 21.4% | <.001 |
| DVT | 2 | 1.0% | 0 | 0.0% | 2 | 0.4% | .182 |
| Seroma | 48 | 24.7% | 0 | 0.0% | 48 | 10.6% | <.001 |
| Wound | 10 | 5.2% | 20 | 7.7% | 30 | 6.6% | .342 |
| Hypertrophic scar | 0 | 0.0% | 8 | 3.1% | 8 | 1.8% | .012 |
| Other | 8 | 4.1% | 8 | 3.1% | 16 | 3.5% | .612 |
| Average visits to resolve | 4.1 | SD 3.8 | 2.6 | SD 2.8 | 3.6 | SD 3.5 | .041 |
BMI, body mass index; DVT, deep venous thrombosis; PEMF, pulsed electromagnetic field therapy; PTS, progressive tension sutures; SD, standard deviation.
| . | Drains . | . | PTS/no drains . | . | All patients . | . | P value . |
|---|---|---|---|---|---|---|---|
| No. of patients | 194 | 260 | 454 | ||||
| Dates | 3/29/1999–5/20/2010 | 6/15/2010–11/14/2019 | 3/29/1999–11/14/2019 | ||||
| Patients: | |||||||
| Average age | 40.2 | SD 9.4 | 43.7 | SD 10.2 | 42.2 | SD 10.0 | <.001 |
| Average BMI | 25.5 | SD 4.5 | 26.0 | SD 4.6 | 25.8 | SD 4.6 | .331 |
| Massive weight loss (>100 lb) | 8 | 4.1% | 24 | 9.2% | 32 | 7.0% | .041 |
| Males | 7 | 3.6% | 4 | 1.5% | 11 | 2.4% | .218 |
| Type of procedure: | .319 | ||||||
| Full | 159 | 82.0% | 212 | 81.5% | 371 | 81.7% | |
| Modified | 23 | 11.9% | 33 | 12.7% | 56 | 12.3% | |
| Mini | 9 | 4.6% | 12 | 4.6% | 21 | 4.6% | |
| Fleur-de-lis | 0 | 0.0% | 3 | 1.2% | 3 | 0.7% | |
| Belt lipectomy | 2 | 1.0% | 0 | 0.0% | 2 | 0.4% | |
| Revision | 1 | 0.5% | 0 | 0.0% | 1 | 0.2% | |
| Liposuction | 146 | 75.3% | 220 | 84.6% | 366 | 80.6% | .016 |
| Additional procedures | 113 | 58.2% | 159 | 61.2% | 272 | 59.9% | .562 |
| Liposomal bupivacaine (Exparel) | 0 | 0.0% | 189 | 72.7% | 189 | 41.6% | <.001 |
| PEMF | 0 | 0.0% | 252 | 96.9% | 252 | 55.5% | <.001 |
| PTS | 1 | 0.5% | 260 | 100.0% | 261 | 57.5% | <.001 |
| Surgical setting: | <.001 | ||||||
| Full admission | 17 | 8.8% | 3 | 1.2% | 20 | 4.4% | |
| Observation | 3 | 1.5% | 0 | 0.0% | 3 | 0.7% | |
| Outpatient | 174 | 89.7% | 257 | 98.8% | 431 | 94.9% | |
| Complications: | 61 | 31.4% | 36 | 13.8% | 97 | 21.4% | <.001 |
| DVT | 2 | 1.0% | 0 | 0.0% | 2 | 0.4% | .182 |
| Seroma | 48 | 24.7% | 0 | 0.0% | 48 | 10.6% | <.001 |
| Wound | 10 | 5.2% | 20 | 7.7% | 30 | 6.6% | .342 |
| Hypertrophic scar | 0 | 0.0% | 8 | 3.1% | 8 | 1.8% | .012 |
| Other | 8 | 4.1% | 8 | 3.1% | 16 | 3.5% | .612 |
| Average visits to resolve | 4.1 | SD 3.8 | 2.6 | SD 2.8 | 3.6 | SD 3.5 | .041 |
| . | Drains . | . | PTS/no drains . | . | All patients . | . | P value . |
|---|---|---|---|---|---|---|---|
| No. of patients | 194 | 260 | 454 | ||||
| Dates | 3/29/1999–5/20/2010 | 6/15/2010–11/14/2019 | 3/29/1999–11/14/2019 | ||||
| Patients: | |||||||
| Average age | 40.2 | SD 9.4 | 43.7 | SD 10.2 | 42.2 | SD 10.0 | <.001 |
| Average BMI | 25.5 | SD 4.5 | 26.0 | SD 4.6 | 25.8 | SD 4.6 | .331 |
| Massive weight loss (>100 lb) | 8 | 4.1% | 24 | 9.2% | 32 | 7.0% | .041 |
| Males | 7 | 3.6% | 4 | 1.5% | 11 | 2.4% | .218 |
| Type of procedure: | .319 | ||||||
| Full | 159 | 82.0% | 212 | 81.5% | 371 | 81.7% | |
| Modified | 23 | 11.9% | 33 | 12.7% | 56 | 12.3% | |
| Mini | 9 | 4.6% | 12 | 4.6% | 21 | 4.6% | |
| Fleur-de-lis | 0 | 0.0% | 3 | 1.2% | 3 | 0.7% | |
| Belt lipectomy | 2 | 1.0% | 0 | 0.0% | 2 | 0.4% | |
| Revision | 1 | 0.5% | 0 | 0.0% | 1 | 0.2% | |
| Liposuction | 146 | 75.3% | 220 | 84.6% | 366 | 80.6% | .016 |
| Additional procedures | 113 | 58.2% | 159 | 61.2% | 272 | 59.9% | .562 |
| Liposomal bupivacaine (Exparel) | 0 | 0.0% | 189 | 72.7% | 189 | 41.6% | <.001 |
| PEMF | 0 | 0.0% | 252 | 96.9% | 252 | 55.5% | <.001 |
| PTS | 1 | 0.5% | 260 | 100.0% | 261 | 57.5% | <.001 |
| Surgical setting: | <.001 | ||||||
| Full admission | 17 | 8.8% | 3 | 1.2% | 20 | 4.4% | |
| Observation | 3 | 1.5% | 0 | 0.0% | 3 | 0.7% | |
| Outpatient | 174 | 89.7% | 257 | 98.8% | 431 | 94.9% | |
| Complications: | 61 | 31.4% | 36 | 13.8% | 97 | 21.4% | <.001 |
| DVT | 2 | 1.0% | 0 | 0.0% | 2 | 0.4% | .182 |
| Seroma | 48 | 24.7% | 0 | 0.0% | 48 | 10.6% | <.001 |
| Wound | 10 | 5.2% | 20 | 7.7% | 30 | 6.6% | .342 |
| Hypertrophic scar | 0 | 0.0% | 8 | 3.1% | 8 | 1.8% | .012 |
| Other | 8 | 4.1% | 8 | 3.1% | 16 | 3.5% | .612 |
| Average visits to resolve | 4.1 | SD 3.8 | 2.6 | SD 2.8 | 3.6 | SD 3.5 | .041 |
BMI, body mass index; DVT, deep venous thrombosis; PEMF, pulsed electromagnetic field therapy; PTS, progressive tension sutures; SD, standard deviation.
In the drain group, there were 7 males and 187 females. In the PTS/no drains group, there were 4 males and 256 females. The average patient age was 40.2 years (range 19–68 years) in the drain group and 42.2 years (range 18–77 years) in the group without drains (P < .001). The no drains group contained a significantly higher proportion of massive weight loss patients, defined as a greater than 100-pound weight loss over any time frame (4.1% vs 9.2%, P = .041). BMI and gender were not statistically different between the 2 groups.
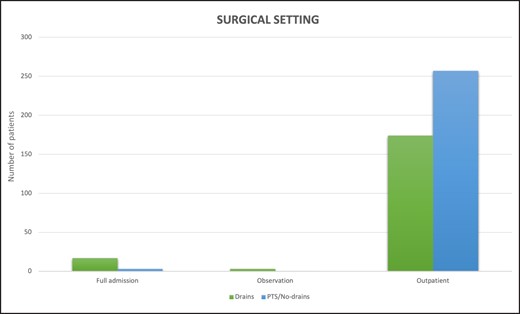
Liposuction was performed with higher frequency in the no drains group (75.3% vs 84.6%, P = .016); however there was no statistical difference in performance of concomitant procedures (58.2% vs 61.2%, P = .562). In accordance with the aforementioned changes to surgical technique, there was a statistically significant difference in the utilization of progressive tension sutures, liposomal bupivacaine, and PEMF between the 2 groups. As demonstrated in Figure 7, the majority of the group without drains underwent outpatient surgery, and this was statistically significant when compared to the drain group (89.7% vs 98.8%, P < .001).
The overall complication rate was statistically reduced in the no drains group (31.4% vs 13.8%, P < .001). Two patients in the drain group were found to have DVTs, but this was not statistically significant (1.0% vs 0.0%, P = .182). The incidence of seroma was dramatically reduced in the group without drains (24.7% vs 0.0%, P < .001). The presence or absence of seroma was clinically determined by palpation only. Complications took less time to resolve in the no drains group (4.1 vs 2.6 visits, P < .041).
The complication profile of each group is illustrated in Figure 8. Of note, a 63-year-old patient in the group without drains suffered a perforated diverticulum in the postoperative interval. The diverticulum was located distally in the descending colon. Upon laparotomy, extensive previously unrecognized diverticulosis was identified in the left colon. The authors believe that transient ileus and constipation from even the minimal narcotic use led to the perforation.
Patients were routinely seen at 3 to 4 days, 1 week, 2 weeks, 6 weeks, 6 months, and 1 year postoperatively. The average duration of follow-up was 9 months.
DISCUSSION
Surgical goals of abdominoplasty include maximizing contour improvement of the abdomen, removing dermatochalasis, repairing diastasis recti, contouring zones of localized adiposity, repairing umbilical and ventral hernias, controlling postoperative pain and morbidity, minimizing risk of complications, avoiding need for hospitalization, and early return to activity. As body contouring continues to become more prominent in plastic surgery, so too have advances in safety and outcomes. The demographic data of our cohort reflected national trends over the past 2 decades. The average age of the no drains group was significantly higher, consistent with patients undergoing plastic surgery at later ages.16 Similarly, there was a higher proportion of massive weight loss patients in the no drains group. This can be linked directly to national trends in bariatric surgery.17
Pressures for reducing costs and decreasing length of stay coupled with improvements in postoperative pain control have allowed abdominoplasty to evolve into a primarily outpatient procedure.6,12,18 This was certainly reflected in our data, because only 1.2% of the PTS/no drains group were admitted postoperatively. Admission was primarily due to medical comorbidities. D. S. K.’s preference is to avoid abdominoplasty combined with hysterectomy or other gynecologic procedures. Although the safety of abdominoplasty in an outpatient setting has been demonstrated, complications are inevitable in any surgical procedure and mitigation becomes crucial when patients are being discharged home.
Seroma is the most common complication after abdominoplasty and can have a range of effects, from multiple outpatient visits to secondary surgical revision. Multiple etiologies of seroma have been proposed, including vascular and lymphatic channel disruption, dead space formation, shearing forces between the flap and fascia, and release of inflammatory mediators.1 Addressing the etiology of seroma through directed suture placement was initially popularized by Pollock and Pollock in 2000 and has since been modified by multiple different authors.7,19 The proposed benefits of progressive tension sutures include not only decreased seroma formation, but also reduced tension on the abdominal skin flap, resulting in decreased wound complications and accurate umbilical placement.20 The disadvantages of progressive tension sutures include increased operative time, difficulty of placement, a significant learning curve, skin dimpling, and possibly increased pain. Previous authors have estimated 30 to 50 minutes of additional operative time.1,21 D. S. K. routinely spends 25 to 30 minutes placing progressive tension sutures, which includes inset around the umbilicus at the deep layer. Use of progressive tension sutures to reduce seroma formation has been successfully described in other disciplines of plastic surgery, including facelift and reconstructive breast surgery.8,22-24
The literature regarding progressive tension sutures in aesthetic abdominoplasty is conflicting, likely as a result of the wide variation of technique in practice. The number of sutures and their placement differ among authors, however most agree that sutures must be placed between Scarpa's fascia and the deep abdominal fascia to truly be effective. Our data suggest that placement of progressive tension sutures in this manner without drains is an effective technique for reducing postoperative seroma. The incidence was dramatically reduced, to the extent that seroma was not clinically apparent in the progressive tension sutures/no drains group. The overall complication rate was also significantly reduced in this group, suggesting that this technique is both efficacious and safe. Other authors have suggested that when seromas do form in the setting of progressive tension sutures, they may be less complex and more readily treated.12
The major limitation of our study was the presence of multiple variables between cohorts due to evolving practice patterns. In addition to the discontinuation of drains in favor of progressive tension sutures, liposomal bupivacaine and PEMF were also initiated. Exparel has now become the gold standard for long-acting local anesthetic in many plastic surgery procedures.25 PEMF is less commonly employed but has been developed as a noninvasive intervention to enhance tissue healing.26,27
PEMF is the local application of moving electric charges to influence tissue physiology. By delivering the field in a pulsed nature, as opposed to continuously, there is no heat generated. PEMF has been studied extensively and has been found to modulate cytokines, growth factors, and molecular markers of inflammation. A recent meta-analysis found statistically significant improvement in pain, edema, and wound healing.28 The direct anti-inflammatory mechanism of PEMF is proposed to be the modulation of calcium binding to calmodulin, which subsequently activates nitric oxide synthase (NOS). There are several different isoforms of NOS that produce nitric oxide and create various effects impacting multiple phases of pain, swelling, tissue regeneration, and remodeling.29
In vitro, PEMF has been shown to increase angiogenesis and reepithelialization.30,31 In vivo, PEMF has demonstrated efficacy in treating bony nonunion and postoperative edema.32-35 Specifically, PEMF has been found to decrease inflammatory mediators such as IL-1β in breast reduction and transverse rectus abdominis myocutaneous (TRAM) flap patients.36,37 In addition to its wound healing effects, recent evidence suggests that PEMF may be a useful adjunct for postoperative pain control. Studies have shown decreased pain scores and narcotic use in multiple types of aesthetic and reconstructive breast surgery.13,14,38-40 Previous authors have shown that the effects of PEMF on pain are of higher magnitude than those reported for pain pumps.37 PEMF devices are also relatively inexpensive and have no known side effects.29
Previous studies with PTS alone have demonstrated seroma rates ranging from 0.1% to 6.1%.2,9,10,12,20,41-43 Given that seroma fluid demonstrates inflammatory mediators and that PEMF studies have demonstrated a decrease in inflammatory mediators, the authors postulate that the 0% incidence of seroma in the PTS portion of this series may be at least in part related to the combined utilization of PTS and PEMF. Additional study dedicated to comparing drainless abdominoplasty with and without PEMF would be needed to support or refute this theory. Although the authors can only postulate on the contribution of PEMF, the results are compelling regarding the efficacy of this combination of techniques in mitigating complications and minimizing postoperative pain.
Limitations
This study may have been affected by selection bias due to its retrospective nature. Additionally, aesthetic outcomes were not assessed. As mentioned, the progressive tension sutures group included variables related to postoperative pain control.
CONCLUSION
Progressive tension sutures are highly effective in preventing seroma and can be safely employed as an alternative to drains in abdominoplasty. PEMF may play a role in seroma prevention and is also helpful for pain control. By employing these techniques to mitigate complications and minimize postoperative pain, abdominoplasty can be performed safely and effectively in a purely outpatient setting.
Disclosures
The authors declared no potential conflicts of interest with respect to the research, authorship, and publication of this article.
Funding
The authors received no financial support for the research, authorship, and publication of this article.
REFERENCES
Author notes
Dr Paranzino is a fellow, Division of Plastic and Reconstructive Surgery, Brigham and Women's Hospital, Boston, MA, USA.
Mr Sims is a registered nurse first assistant in private practice in Lexington, KY, USA.
Dr Kirn is a plastic surgeon in private practice in Lexington, KY, USA.



