-
PDF
- Split View
-
Views
-
Cite
Cite
Fatemeh Alavi-Arjas, Michael P Goodman, Masoumeh Simbar, Hamid Alavi Majd, Gemma Sharp, Fatemeh Nahidi, The Effect of Female Genital Cosmetic and Reconstructive Procedures on Body and Genital Self-Image: A Systematic Review and Meta-Analysis, Aesthetic Surgery Journal, Volume 43, Issue 10, October 2023, Pages 1161–1173, https://doi.org/10.1093/asj/sjad109
Close - Share Icon Share
Abstract
Performance of female genital cosmetic and reconstructive procedures (FGCRP) has been increasing over past decades. Appearance and functional concerns are the most common reasons for seeking FGCRP. Poor body and genital self-image may contribute to the increase in demand for surgery. The aim of this systematic review is to explore outcomes of FGCRP in the domains of body and genital self-image. A systematic literature review of PubMed, Web of Science, Scopus, PsycINFO, Embase, and the Cochrane Library was conducted to identify articles that measured body and genital self-image in females after FGCRP. The authors identified 5 articles for a systematic review of body image and 8 studies for a systematic review of genital self-image. The most common procedure performed was labia minora labiaplasty. Instruments for body image evaluation were the Yale–Brown Obsessive-Compulsive Scale Modified for Body Dysmorphic Disorder and the Body Image Quality of Life Inventory. Genital image was assessed with the Female Genital Self-Image Scale and Genital Appearance Satisfaction (GAS) scale. Most of the studies indicated that FGCRP can improve both body image and genital self-image; meta-analysis revealed that FGCRP improved GAS scores by 17.96 (range: 0-33; P < .001). It appears that FGCRP leads to improvements in females’ body and genital self-image. Inconsistencies in study design and measures, however, limit this conclusion. Future research should involve more rigorous study designs (for example randomized clinical trials with large sample sizes) for a more accurate assessment of FGCRP's consequences.

Female genital cosmetic and reconstructive procedures (FGCRP) cover a wide range of procedures, the most common of which are labiaplasty (minora and majora), labia majora augmentation, vaginoplasty/perineoplasty (vaginal reconstruction), hymenoplasty, clitoral hood reduction, and Gräfenberg spot amplification.1 Demand for genital cosmetic procedures is rising. In 2018 (before the start of the COVID-19 pandemic), the American Society for Aesthetic Plastic Surgery declared that labiaplasty was among the fastest growing surgical procedures, up 53% in 5 years. More recent statistics indicated that 30,798 genital surgeries were performed in 2021, which increased by 55% compared to 2020. A total of $109,471,119 was spent on these surgeries.2 It should be noted that these statistics do not include procedures performed by gynecologists, whether cosmetic gynecologists or general obstetricians/gynecologists, for whom statistics are not kept.
In the absence of legal, access, and financial restrictions, people have the right and opportunity to change what concerns them and to resolve their genital-related aesthetic and physical discomfort.3 Females seek FGCRP for aesthetic, sexual, functional, and psychological discomforts.4 Patients may report chafing, itching, personal hygiene issues, dyspareunia, pain with exercise, tugging, exposure in swimwear, recurrent urinary tract infections, and deviation of the urine stream.5 Psychological afflictions include feelings of embarrassment and abnormality of genital appearance and mental preoccupation.6
With past taboos decreasing, people appear to be more open about discussing their sexual organs.7 Medical reality television and talk show hype, viewing of pornography, and the widespread prevalence of pubic hair removal methods have led to increased genital visualization, diminished “padding,” and increased concerns about vulvar appearance.8 Females are influenced to idealize physical “perfection” through social and news media, the Internet, and pornography. This may encourage a certain genital shape (small labia minora and narrow vaginal entrance), and lead to concern over other appearances.9,10 Genital appearance concerns and self-consciousness about vulvar appearance is a primary reason for seeking FGCRP, particularly labiaplasty.11-15
Body image refers to a person's impressions of their own body, including their feelings, ideas, and actions toward their entire body; genital self-image describes one's emotional and psychological perceptions of their own genitalia.16,17 There is a link between positive body image and positive genital self-image.18 Among the most significant precursors are negative self-perceptions and negative emotion. Negative body image consequences include disordered eating, low self-esteem, body surveillance, and a diminished pleasure in daily activities, among others.19
The aim of this systematic review is to answer the question of whether FGCRP can result in self-perceived improvement of body and genital self-image. In our systematic review we included all types of FGCRP, including internally focused procedures, because the way females perceive their genital function can have significant impacts on their sense of body image and genital self-image.
METHODS
Search Strategy
The reporting method of systematic reviews (PRISMA) was applied to recognize and articulate the issues explored in this study, including data gathering and analysis, elucidation of findings, and drawing of conclusions.20 We applied the following tools to search for articles in international databases; PubMed (National Institutes of Health, Bethesda, MD), Web of Science (Clarivate, London, UK), Scopus (Elsevier, Amsterdam, the Netherlands), PsycINFO (American Psychological Association, Washington, DC), Embase (Elsevier, Amsterdam, the Netherlands), and the Cochrane Library (Wiley, Hoboken, NJ). A Google Scholar (Mountain View, CA) search was performed. Proportional articles published from the beginning of 2000 until November 2022 (search date) were searched and extracted by 2 independent researchers (F.A. and F.N.) based on keywords that were combined with Boolean operators to ensure an inclusive and complete search process (Table 1). Inconsistencies were reviewed and resolved by a third reviewer (M.S.). The details of the search strategy are available as Appendices A and B (www.aestheticsurgeryjournal.com).
Keywords of Body and Genital Self-Image After Female Genital Cosmetic and Reconstructive Procedures
| Descriptive specialty terms . | Vaginal caliber . | Labia minora and majora . | Hymenal reconstruction . | Clitoral procedures . | Non-descriptive colloquial terms . | Body/genital image . | Mons pubis . |
|---|---|---|---|---|---|---|---|
| aesthetic genitalia surgery cosmetic genital surgery genital cosmetic surgery cosmetic gynecology cosmetoplastic gynecology cosmetic vaginal vulvo-vaginal rejuvenation genital plastic surgery vulvovaginal aesthetic surgery cosmetic gynecology vulvar laxity | cosmetic vaginoplasty cosmetic vaginal surgery aesthetic vaginal surgery tightening of the vaginal opening tighten vaginal canal designer vagina surgery vaginoplasty vaginal tightening vaginal rejuvenation vaginal support procedures restore the vaginal contour vaginal caliber reduction colpoperineoplasty colporrhaphy perineoplasty vaginal recalibration vaginal re-calibration vaginal laxity | labiaplasty labioplasty labia minora reduction labial hypertrophy labial reduction labia majora reduction labia majora augmentation labia majora lift labia majora-plasty labia majora lipografting | hymenoplasty hymenorrhaphy revirgination | clitoral hood reduction clitoriplasty clitoral hoodectomy clitoral unhooding | intimate operations mommy makeover genital beautification | body/genital image body/genital appreciation body/genital self-image body/genital image acceptance body/genital satisfaction body/genital dissatisfaction body/genital shape body/genital perception | monsplasty mons pubis reconstruction liposuction to the mons pubis mons pubis reduction mons pubis suspension suprapubic lift mons suspension |
| Descriptive specialty terms . | Vaginal caliber . | Labia minora and majora . | Hymenal reconstruction . | Clitoral procedures . | Non-descriptive colloquial terms . | Body/genital image . | Mons pubis . |
|---|---|---|---|---|---|---|---|
| aesthetic genitalia surgery cosmetic genital surgery genital cosmetic surgery cosmetic gynecology cosmetoplastic gynecology cosmetic vaginal vulvo-vaginal rejuvenation genital plastic surgery vulvovaginal aesthetic surgery cosmetic gynecology vulvar laxity | cosmetic vaginoplasty cosmetic vaginal surgery aesthetic vaginal surgery tightening of the vaginal opening tighten vaginal canal designer vagina surgery vaginoplasty vaginal tightening vaginal rejuvenation vaginal support procedures restore the vaginal contour vaginal caliber reduction colpoperineoplasty colporrhaphy perineoplasty vaginal recalibration vaginal re-calibration vaginal laxity | labiaplasty labioplasty labia minora reduction labial hypertrophy labial reduction labia majora reduction labia majora augmentation labia majora lift labia majora-plasty labia majora lipografting | hymenoplasty hymenorrhaphy revirgination | clitoral hood reduction clitoriplasty clitoral hoodectomy clitoral unhooding | intimate operations mommy makeover genital beautification | body/genital image body/genital appreciation body/genital self-image body/genital image acceptance body/genital satisfaction body/genital dissatisfaction body/genital shape body/genital perception | monsplasty mons pubis reconstruction liposuction to the mons pubis mons pubis reduction mons pubis suspension suprapubic lift mons suspension |
Keywords of Body and Genital Self-Image After Female Genital Cosmetic and Reconstructive Procedures
| Descriptive specialty terms . | Vaginal caliber . | Labia minora and majora . | Hymenal reconstruction . | Clitoral procedures . | Non-descriptive colloquial terms . | Body/genital image . | Mons pubis . |
|---|---|---|---|---|---|---|---|
| aesthetic genitalia surgery cosmetic genital surgery genital cosmetic surgery cosmetic gynecology cosmetoplastic gynecology cosmetic vaginal vulvo-vaginal rejuvenation genital plastic surgery vulvovaginal aesthetic surgery cosmetic gynecology vulvar laxity | cosmetic vaginoplasty cosmetic vaginal surgery aesthetic vaginal surgery tightening of the vaginal opening tighten vaginal canal designer vagina surgery vaginoplasty vaginal tightening vaginal rejuvenation vaginal support procedures restore the vaginal contour vaginal caliber reduction colpoperineoplasty colporrhaphy perineoplasty vaginal recalibration vaginal re-calibration vaginal laxity | labiaplasty labioplasty labia minora reduction labial hypertrophy labial reduction labia majora reduction labia majora augmentation labia majora lift labia majora-plasty labia majora lipografting | hymenoplasty hymenorrhaphy revirgination | clitoral hood reduction clitoriplasty clitoral hoodectomy clitoral unhooding | intimate operations mommy makeover genital beautification | body/genital image body/genital appreciation body/genital self-image body/genital image acceptance body/genital satisfaction body/genital dissatisfaction body/genital shape body/genital perception | monsplasty mons pubis reconstruction liposuction to the mons pubis mons pubis reduction mons pubis suspension suprapubic lift mons suspension |
| Descriptive specialty terms . | Vaginal caliber . | Labia minora and majora . | Hymenal reconstruction . | Clitoral procedures . | Non-descriptive colloquial terms . | Body/genital image . | Mons pubis . |
|---|---|---|---|---|---|---|---|
| aesthetic genitalia surgery cosmetic genital surgery genital cosmetic surgery cosmetic gynecology cosmetoplastic gynecology cosmetic vaginal vulvo-vaginal rejuvenation genital plastic surgery vulvovaginal aesthetic surgery cosmetic gynecology vulvar laxity | cosmetic vaginoplasty cosmetic vaginal surgery aesthetic vaginal surgery tightening of the vaginal opening tighten vaginal canal designer vagina surgery vaginoplasty vaginal tightening vaginal rejuvenation vaginal support procedures restore the vaginal contour vaginal caliber reduction colpoperineoplasty colporrhaphy perineoplasty vaginal recalibration vaginal re-calibration vaginal laxity | labiaplasty labioplasty labia minora reduction labial hypertrophy labial reduction labia majora reduction labia majora augmentation labia majora lift labia majora-plasty labia majora lipografting | hymenoplasty hymenorrhaphy revirgination | clitoral hood reduction clitoriplasty clitoral hoodectomy clitoral unhooding | intimate operations mommy makeover genital beautification | body/genital image body/genital appreciation body/genital self-image body/genital image acceptance body/genital satisfaction body/genital dissatisfaction body/genital shape body/genital perception | monsplasty mons pubis reconstruction liposuction to the mons pubis mons pubis reduction mons pubis suspension suprapubic lift mons suspension |
Eligibility Criteria
Original article (not review or letter to editor or commentary article)
Female sex (not transgender)
Female genital surgery is performed only for cosmetic and/or functional reasons (eg, interference in athletic activities, discomfort due to labial friction, poor hygiene, interference with sexual intercourse) and does not refer to procedures performed for medical necessity (eg, previous obstetric or straddle injury, reversing female genital cutting, severe pelvic organs prolapse, incontinence, or gender affirmation surgery)
Must include a postprocedure assessment with a quantitative measure
Not pregnant or breastfeeding
Disagreements were resolved through a discussion between the reviewing authors. If an article's data were incomplete, contact with corresponding authors was attempted for clarity.
Data Extraction
Search results were downloaded to EndNote version 8 (Clarivate, London, UK). A total of 417 articles were retrieved by searching keywords. After removing duplicate studies, the titles and abstracts (after removing the names of journals and authors) of all citations identified were reviewed by 2 researchers (F.A. and F.N.) independently, and discrepancies were reassessed by a third researcher (M.S.) and settled through discussion. After the deletion of irrelevant articles according to the eligibility criteria, 10 articles remained (Figure 1). Then the following information was collected: (1) author names, (2) publication year, (3) study design, (4) sample size, (5) participant mean age, (6) surgery type, (7) follow-up time, (8) body image assessment and result, and (9) genital self-image assessment and finding.
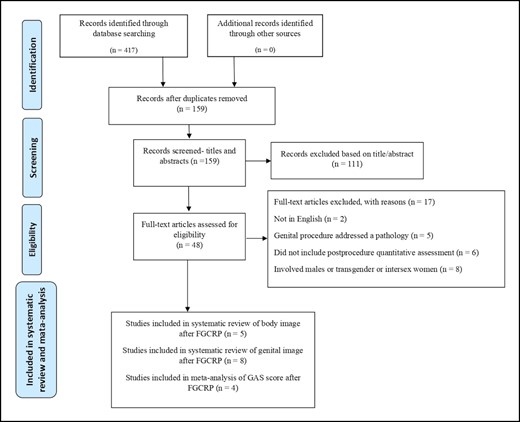
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram showing the search, retrieval, and selection of potentially relevant studies.
Quality Evaluation
The Effective Public Healthcare Practice Project (EPHPP) evaluates the methodological quality of studies by assessing the evidence of efficacy/effectiveness of interventions based on selection bias, study design, confounding variables, blinding, data collection methods, and withdrawal and dropout rates. Ratings for these 6 items of quality are combined to determine a global quality rating of strong (no weak ratings), moderate (1 weak rating), or weak (more than 1 weak rating). The EPHPP was used due to its appropriateness for quality assessment of all quantitative approaches, sufficient content, and construct validity. 21,22
Two reviewers (F.A. and F.N.) assessed the methodological quality of the included studies with the EPHPP.22 The reviewers separately evaluated the methodological qufality of each article with the EPHPP. Ratings were then shared with the other reviewers. Any discrepancies were discussed and a final decision on rating was made. Missing information from a study was requested by an email to the corresponding author.
On quality assessment, 5 of the articles were categorized as weak, 4 studies as moderate, and 1 as strong (Table 2). Lack of randomization and blinding were a common disadvantage; some important strengths seen in the articles were that all of them employed a standard measure for body and genital image evaluation and evaluated most of the confounders; all but 1 had measurements taken before and after surgery, and except for 3 studies they had a follow-up time of 6 months or more.15,17,23,24
Quality Assessment by Effective Public Healthcare Panacea Project (EPHPP) Quality Assessment Tool for Quantitative Studies
| Author (year) . | Selection bias . | Study design . | Confounders . | Blinding . | Data collection method . | Withdrawals and dropouts . | Global quality rating . |
|---|---|---|---|---|---|---|---|
| Goodman et al (2011) | ** | ** | *** | * | *** | * | * |
| Veale et al (2014) | * | ** | *** | * | *** | ** | * |
| Sharp et al (2016) | ** | ** | *** | * | *** | *** | ** |
| Goodman et al (2016) | ** | ** | *** | * | *** | ** | ** |
| Sharp et al (2017) | ** | ** | *** | * | *** | ** | ** |
| Eftekhar et al (2021) | ** | ** | *** | * | *** | *** | ** |
| Propst et al (2021) | * | ** | *** | * | *** | * | * |
| Jiang et al (2021) | ** | *** | *** | ** | *** | ** | *** |
| Cihantimur et al (2021) | * | ** | * | * | * | * | * |
| Zhou et al (2022) | * | ** | ** | * | *** | * | * |
| Author (year) . | Selection bias . | Study design . | Confounders . | Blinding . | Data collection method . | Withdrawals and dropouts . | Global quality rating . |
|---|---|---|---|---|---|---|---|
| Goodman et al (2011) | ** | ** | *** | * | *** | * | * |
| Veale et al (2014) | * | ** | *** | * | *** | ** | * |
| Sharp et al (2016) | ** | ** | *** | * | *** | *** | ** |
| Goodman et al (2016) | ** | ** | *** | * | *** | ** | ** |
| Sharp et al (2017) | ** | ** | *** | * | *** | ** | ** |
| Eftekhar et al (2021) | ** | ** | *** | * | *** | *** | ** |
| Propst et al (2021) | * | ** | *** | * | *** | * | * |
| Jiang et al (2021) | ** | *** | *** | ** | *** | ** | *** |
| Cihantimur et al (2021) | * | ** | * | * | * | * | * |
| Zhou et al (2022) | * | ** | ** | * | *** | * | * |
*Weak, **Moderate, ***Strong
Quality Assessment by Effective Public Healthcare Panacea Project (EPHPP) Quality Assessment Tool for Quantitative Studies
| Author (year) . | Selection bias . | Study design . | Confounders . | Blinding . | Data collection method . | Withdrawals and dropouts . | Global quality rating . |
|---|---|---|---|---|---|---|---|
| Goodman et al (2011) | ** | ** | *** | * | *** | * | * |
| Veale et al (2014) | * | ** | *** | * | *** | ** | * |
| Sharp et al (2016) | ** | ** | *** | * | *** | *** | ** |
| Goodman et al (2016) | ** | ** | *** | * | *** | ** | ** |
| Sharp et al (2017) | ** | ** | *** | * | *** | ** | ** |
| Eftekhar et al (2021) | ** | ** | *** | * | *** | *** | ** |
| Propst et al (2021) | * | ** | *** | * | *** | * | * |
| Jiang et al (2021) | ** | *** | *** | ** | *** | ** | *** |
| Cihantimur et al (2021) | * | ** | * | * | * | * | * |
| Zhou et al (2022) | * | ** | ** | * | *** | * | * |
| Author (year) . | Selection bias . | Study design . | Confounders . | Blinding . | Data collection method . | Withdrawals and dropouts . | Global quality rating . |
|---|---|---|---|---|---|---|---|
| Goodman et al (2011) | ** | ** | *** | * | *** | * | * |
| Veale et al (2014) | * | ** | *** | * | *** | ** | * |
| Sharp et al (2016) | ** | ** | *** | * | *** | *** | ** |
| Goodman et al (2016) | ** | ** | *** | * | *** | ** | ** |
| Sharp et al (2017) | ** | ** | *** | * | *** | ** | ** |
| Eftekhar et al (2021) | ** | ** | *** | * | *** | *** | ** |
| Propst et al (2021) | * | ** | *** | * | *** | * | * |
| Jiang et al (2021) | ** | *** | *** | ** | *** | ** | *** |
| Cihantimur et al (2021) | * | ** | * | * | * | * | * |
| Zhou et al (2022) | * | ** | ** | * | *** | * | * |
*Weak, **Moderate, ***Strong
Meta-analysis
Forest plots were generated to demonstrate the study-specific pre- to postprocedure strength differences and effect sizes (ESs), within the respective 95% confidence intervals (CIs). Heterogeneity was assessed by I2 statistics. When the heterogeneity index I2 was lower than 50%, the pooled effect size was calculated with a fixed-effects model. When the heterogeneity index I2 was higher than 50%, a random-effects model was used.
For publication bias assessment, a funnel plot was performed. No publication bias was reported, and the funnel plot appeared to be symmetric. The statistical software package STATA 14.0 (Stata Corp., College Station, TX) was utilized to perform the analysis.
RESULTS
This review began by searching through the listed databases using the keywords noted to find relevant articles published from January 2000 to November 2022, initially locating 417 articles (Figure 1). After removal of duplicates, the abstracts of the remaining articles were reviewed and their full texts were obtained as appropriate. After assessing study criteria, 9 articles (5 studies for body image and 8 articles for genital image [3 of which held in common the 2 intended outcomes]) were included. Labia minora labiaplasty was the most common procedure noted in our systematic review.
Results of Systematic Review of Body Image After FGCRP
Body image was evaluated in 5 studies utilizing either the Yale–Brown Obsessive-Compulsive Scale Modified for Body Dysmorphic Disorder (BDD-YBOCS; 2 studies) or the Body Image Quality of Life Inventory (BIQLI; 3 studies) (Table 3).25,26 Goodman et al conducted 2 prospective studies for evaluation of the body image of females after FGCRP (labiaplasty, clitoral hood reduction, and/or aesthetic vaginal tightening) utilizing 3 subdomains of the BDD-YBOCS (Preoccupation, Behaviors, and Avoidance) and the total score.27,28 In the 2011 pilot study, evaluation of 18 females 6 to 9 months after surgery indicated significant improvement in all 3 subdomains and total scores.28 In the 2016 study involving 120 females followed up at 24 months and compared with a control group, there were similar findings for the 3 subdomains and total score.27
Basic Characteristics of Studies Included in the Body Image Systematic Review
| Author, country, year . | Study design . | Sample size . | Mean age ± SD, year (range) . | Procedure type . | Labiaplasty technique . | Follow-up time . | Body image instrument . | Result (Mean ± SD) . |
|---|---|---|---|---|---|---|---|---|
| Goodman et al, USA, 2011 | Prospective study | n = 18 | 35.40 ± 11.73 (Not reported) | Labiaplasty, clitoral hood reduction, vaginoplasty, perineoplasty | Removal of portions of the labia minora and/or labia majora. Modified V-wedge, leading edge, sculpted linear resection techniques | 6-9 months | BDD-YBOCS (Includes 3 subdomains; Preoccupation, Behaviors, Avoidance, and total score) | Preoccupation: Preprocedure: 7.33 ± 3.90 6-9 months: 2.83 ± 2.71 P = .001 Behaviors: Preprocedure: 6.17 ± 3.96 6-9 months: 2.0 ± 2.11 P = .001 Avoidance: Preprocedure: 1.11 ± 1.08 6-9 months: 0.22 ± 0.55 P = .002 Total: Preprocedure: 16.67 ± 8.79 6-9 months: 5.72 ± 4.76 P = .001 |
| Goodman et al, USA, 2016 | Prospective cohort case-control study | Study =120 Control = 50 | Study: 32.74 ± 10.14 (18-63) Control: 33.20 ± 9.58 (18-58) | Labiaplasty, clitoral hood reduction, aesthetic vaginal tightening | N/A | 6, 12, and 24 months | BDD-YBOCS (Includes 3 subdomains; Preoccupation, Behaviors, Avoidance, and total score) | Preprocedure: Preoccupation: Study: 7.62 Control: 1.90 P = .0001 Behaviors: Study: 6.51 Control: 2.50 P = .001 Avoidance: Study: 1.775 Control: 0.32 P = .0001 Total: Study: 15.90 Control: 4.49 P = .0001 24 months: Preoccupation: Study: 2.12 P c/w control =0.625 P c/w pre = 0.0001 Behaviors: Study: 3.91 P c/w control = 0.272 P c/w pre = 0.001 Avoidance: Study: 0.15 P c/w control = 0.370 P c/w pre = 0.0001 Total: Study: 5.96 P c/w control = 0.370 P c/w pre = 0.0001 |
| Veale et al, England, 2014 | Prospective case-control study | Study = 49 Control = 39 | Median (IQR): Study: 34 (25–43) Control: 28 (25–34) | Labiaplasty | Labial trimming, central wedge reduction, de-epithelization technique, superior pedicle flap reconstruction | 3 months | BIQLI | Comparison of median (IQR) scores in study group before and 3 months after surgery; Preprocedure: −0.06 (−1.1 to 1.6) 3 months: 0.5 (−0.3 to 1.9) P = .066 Effect size: d = −0.41 After 3 months: Study: 0.5 (−0.3 to 1.9) Control: 0.0 (−0.6 to 1.7) P = .349 Effect size: d = −0.29 |
| Eftekhar et al, Iran, 2021 | Prospective study | n = 50 | 43.36 ± 8.6 (18-45) | Labiaplasty, clitoral hoodectomy, vaginoplasty, vaginal rejuvenation, anterior and posterior colporrhaphy, perineoplasty, perineorrhaphy | N/A | 3 months | BIQLI | Preprocedure: 29.7 ± 11 3 months: 42 ± 7.8 Effect size: 1.1 P < .001 |
| Propst and Ferrando, USA, 2020 | Cross-sectional study of a retrospective cohort | n= 21 | 30 ± 12 (at least 18 years old) | Labiaplasty | Simple edge resection with a single-layer closure | Median time: 36 months (3-111 months) | BIQLI | 3-111 months: 0.84 ± 1.4 |
| Author, country, year . | Study design . | Sample size . | Mean age ± SD, year (range) . | Procedure type . | Labiaplasty technique . | Follow-up time . | Body image instrument . | Result (Mean ± SD) . |
|---|---|---|---|---|---|---|---|---|
| Goodman et al, USA, 2011 | Prospective study | n = 18 | 35.40 ± 11.73 (Not reported) | Labiaplasty, clitoral hood reduction, vaginoplasty, perineoplasty | Removal of portions of the labia minora and/or labia majora. Modified V-wedge, leading edge, sculpted linear resection techniques | 6-9 months | BDD-YBOCS (Includes 3 subdomains; Preoccupation, Behaviors, Avoidance, and total score) | Preoccupation: Preprocedure: 7.33 ± 3.90 6-9 months: 2.83 ± 2.71 P = .001 Behaviors: Preprocedure: 6.17 ± 3.96 6-9 months: 2.0 ± 2.11 P = .001 Avoidance: Preprocedure: 1.11 ± 1.08 6-9 months: 0.22 ± 0.55 P = .002 Total: Preprocedure: 16.67 ± 8.79 6-9 months: 5.72 ± 4.76 P = .001 |
| Goodman et al, USA, 2016 | Prospective cohort case-control study | Study =120 Control = 50 | Study: 32.74 ± 10.14 (18-63) Control: 33.20 ± 9.58 (18-58) | Labiaplasty, clitoral hood reduction, aesthetic vaginal tightening | N/A | 6, 12, and 24 months | BDD-YBOCS (Includes 3 subdomains; Preoccupation, Behaviors, Avoidance, and total score) | Preprocedure: Preoccupation: Study: 7.62 Control: 1.90 P = .0001 Behaviors: Study: 6.51 Control: 2.50 P = .001 Avoidance: Study: 1.775 Control: 0.32 P = .0001 Total: Study: 15.90 Control: 4.49 P = .0001 24 months: Preoccupation: Study: 2.12 P c/w control =0.625 P c/w pre = 0.0001 Behaviors: Study: 3.91 P c/w control = 0.272 P c/w pre = 0.001 Avoidance: Study: 0.15 P c/w control = 0.370 P c/w pre = 0.0001 Total: Study: 5.96 P c/w control = 0.370 P c/w pre = 0.0001 |
| Veale et al, England, 2014 | Prospective case-control study | Study = 49 Control = 39 | Median (IQR): Study: 34 (25–43) Control: 28 (25–34) | Labiaplasty | Labial trimming, central wedge reduction, de-epithelization technique, superior pedicle flap reconstruction | 3 months | BIQLI | Comparison of median (IQR) scores in study group before and 3 months after surgery; Preprocedure: −0.06 (−1.1 to 1.6) 3 months: 0.5 (−0.3 to 1.9) P = .066 Effect size: d = −0.41 After 3 months: Study: 0.5 (−0.3 to 1.9) Control: 0.0 (−0.6 to 1.7) P = .349 Effect size: d = −0.29 |
| Eftekhar et al, Iran, 2021 | Prospective study | n = 50 | 43.36 ± 8.6 (18-45) | Labiaplasty, clitoral hoodectomy, vaginoplasty, vaginal rejuvenation, anterior and posterior colporrhaphy, perineoplasty, perineorrhaphy | N/A | 3 months | BIQLI | Preprocedure: 29.7 ± 11 3 months: 42 ± 7.8 Effect size: 1.1 P < .001 |
| Propst and Ferrando, USA, 2020 | Cross-sectional study of a retrospective cohort | n= 21 | 30 ± 12 (at least 18 years old) | Labiaplasty | Simple edge resection with a single-layer closure | Median time: 36 months (3-111 months) | BIQLI | 3-111 months: 0.84 ± 1.4 |
BIQLI, Body Image Quality of Life Inventory; BDD-YBOCS, Yale–Brown Obsessive-Compulsive Scale Modified for Body Dysmorphic Disorder; c/w, compared with; IQR, interquartile range; N/A, not applicable; pre, preprocedure; SD, standard deviation.
Basic Characteristics of Studies Included in the Body Image Systematic Review
| Author, country, year . | Study design . | Sample size . | Mean age ± SD, year (range) . | Procedure type . | Labiaplasty technique . | Follow-up time . | Body image instrument . | Result (Mean ± SD) . |
|---|---|---|---|---|---|---|---|---|
| Goodman et al, USA, 2011 | Prospective study | n = 18 | 35.40 ± 11.73 (Not reported) | Labiaplasty, clitoral hood reduction, vaginoplasty, perineoplasty | Removal of portions of the labia minora and/or labia majora. Modified V-wedge, leading edge, sculpted linear resection techniques | 6-9 months | BDD-YBOCS (Includes 3 subdomains; Preoccupation, Behaviors, Avoidance, and total score) | Preoccupation: Preprocedure: 7.33 ± 3.90 6-9 months: 2.83 ± 2.71 P = .001 Behaviors: Preprocedure: 6.17 ± 3.96 6-9 months: 2.0 ± 2.11 P = .001 Avoidance: Preprocedure: 1.11 ± 1.08 6-9 months: 0.22 ± 0.55 P = .002 Total: Preprocedure: 16.67 ± 8.79 6-9 months: 5.72 ± 4.76 P = .001 |
| Goodman et al, USA, 2016 | Prospective cohort case-control study | Study =120 Control = 50 | Study: 32.74 ± 10.14 (18-63) Control: 33.20 ± 9.58 (18-58) | Labiaplasty, clitoral hood reduction, aesthetic vaginal tightening | N/A | 6, 12, and 24 months | BDD-YBOCS (Includes 3 subdomains; Preoccupation, Behaviors, Avoidance, and total score) | Preprocedure: Preoccupation: Study: 7.62 Control: 1.90 P = .0001 Behaviors: Study: 6.51 Control: 2.50 P = .001 Avoidance: Study: 1.775 Control: 0.32 P = .0001 Total: Study: 15.90 Control: 4.49 P = .0001 24 months: Preoccupation: Study: 2.12 P c/w control =0.625 P c/w pre = 0.0001 Behaviors: Study: 3.91 P c/w control = 0.272 P c/w pre = 0.001 Avoidance: Study: 0.15 P c/w control = 0.370 P c/w pre = 0.0001 Total: Study: 5.96 P c/w control = 0.370 P c/w pre = 0.0001 |
| Veale et al, England, 2014 | Prospective case-control study | Study = 49 Control = 39 | Median (IQR): Study: 34 (25–43) Control: 28 (25–34) | Labiaplasty | Labial trimming, central wedge reduction, de-epithelization technique, superior pedicle flap reconstruction | 3 months | BIQLI | Comparison of median (IQR) scores in study group before and 3 months after surgery; Preprocedure: −0.06 (−1.1 to 1.6) 3 months: 0.5 (−0.3 to 1.9) P = .066 Effect size: d = −0.41 After 3 months: Study: 0.5 (−0.3 to 1.9) Control: 0.0 (−0.6 to 1.7) P = .349 Effect size: d = −0.29 |
| Eftekhar et al, Iran, 2021 | Prospective study | n = 50 | 43.36 ± 8.6 (18-45) | Labiaplasty, clitoral hoodectomy, vaginoplasty, vaginal rejuvenation, anterior and posterior colporrhaphy, perineoplasty, perineorrhaphy | N/A | 3 months | BIQLI | Preprocedure: 29.7 ± 11 3 months: 42 ± 7.8 Effect size: 1.1 P < .001 |
| Propst and Ferrando, USA, 2020 | Cross-sectional study of a retrospective cohort | n= 21 | 30 ± 12 (at least 18 years old) | Labiaplasty | Simple edge resection with a single-layer closure | Median time: 36 months (3-111 months) | BIQLI | 3-111 months: 0.84 ± 1.4 |
| Author, country, year . | Study design . | Sample size . | Mean age ± SD, year (range) . | Procedure type . | Labiaplasty technique . | Follow-up time . | Body image instrument . | Result (Mean ± SD) . |
|---|---|---|---|---|---|---|---|---|
| Goodman et al, USA, 2011 | Prospective study | n = 18 | 35.40 ± 11.73 (Not reported) | Labiaplasty, clitoral hood reduction, vaginoplasty, perineoplasty | Removal of portions of the labia minora and/or labia majora. Modified V-wedge, leading edge, sculpted linear resection techniques | 6-9 months | BDD-YBOCS (Includes 3 subdomains; Preoccupation, Behaviors, Avoidance, and total score) | Preoccupation: Preprocedure: 7.33 ± 3.90 6-9 months: 2.83 ± 2.71 P = .001 Behaviors: Preprocedure: 6.17 ± 3.96 6-9 months: 2.0 ± 2.11 P = .001 Avoidance: Preprocedure: 1.11 ± 1.08 6-9 months: 0.22 ± 0.55 P = .002 Total: Preprocedure: 16.67 ± 8.79 6-9 months: 5.72 ± 4.76 P = .001 |
| Goodman et al, USA, 2016 | Prospective cohort case-control study | Study =120 Control = 50 | Study: 32.74 ± 10.14 (18-63) Control: 33.20 ± 9.58 (18-58) | Labiaplasty, clitoral hood reduction, aesthetic vaginal tightening | N/A | 6, 12, and 24 months | BDD-YBOCS (Includes 3 subdomains; Preoccupation, Behaviors, Avoidance, and total score) | Preprocedure: Preoccupation: Study: 7.62 Control: 1.90 P = .0001 Behaviors: Study: 6.51 Control: 2.50 P = .001 Avoidance: Study: 1.775 Control: 0.32 P = .0001 Total: Study: 15.90 Control: 4.49 P = .0001 24 months: Preoccupation: Study: 2.12 P c/w control =0.625 P c/w pre = 0.0001 Behaviors: Study: 3.91 P c/w control = 0.272 P c/w pre = 0.001 Avoidance: Study: 0.15 P c/w control = 0.370 P c/w pre = 0.0001 Total: Study: 5.96 P c/w control = 0.370 P c/w pre = 0.0001 |
| Veale et al, England, 2014 | Prospective case-control study | Study = 49 Control = 39 | Median (IQR): Study: 34 (25–43) Control: 28 (25–34) | Labiaplasty | Labial trimming, central wedge reduction, de-epithelization technique, superior pedicle flap reconstruction | 3 months | BIQLI | Comparison of median (IQR) scores in study group before and 3 months after surgery; Preprocedure: −0.06 (−1.1 to 1.6) 3 months: 0.5 (−0.3 to 1.9) P = .066 Effect size: d = −0.41 After 3 months: Study: 0.5 (−0.3 to 1.9) Control: 0.0 (−0.6 to 1.7) P = .349 Effect size: d = −0.29 |
| Eftekhar et al, Iran, 2021 | Prospective study | n = 50 | 43.36 ± 8.6 (18-45) | Labiaplasty, clitoral hoodectomy, vaginoplasty, vaginal rejuvenation, anterior and posterior colporrhaphy, perineoplasty, perineorrhaphy | N/A | 3 months | BIQLI | Preprocedure: 29.7 ± 11 3 months: 42 ± 7.8 Effect size: 1.1 P < .001 |
| Propst and Ferrando, USA, 2020 | Cross-sectional study of a retrospective cohort | n= 21 | 30 ± 12 (at least 18 years old) | Labiaplasty | Simple edge resection with a single-layer closure | Median time: 36 months (3-111 months) | BIQLI | 3-111 months: 0.84 ± 1.4 |
BIQLI, Body Image Quality of Life Inventory; BDD-YBOCS, Yale–Brown Obsessive-Compulsive Scale Modified for Body Dysmorphic Disorder; c/w, compared with; IQR, interquartile range; N/A, not applicable; pre, preprocedure; SD, standard deviation.
Three studies included the BIQLI.17,23,29 In the prospective case-control study conducted by Veale et al, 4 methods for altering the labia minora were investigated, and it was found that labiaplasty did not significantly improve body image.29 However, the change tended toward significant (P = .066) with a moderate effect size (d = −0.41) on the BIQLI. Eftekhar et al also found that FGCRP led to improved body image after 3 months.23 Propst and Ferrando only reported a cross-sectional retrospective study of 21 patients with a (wide) 3- to 111-month follow-up.17 The number of studies including the BDD-YBOCS or BIQLI was insufficient for a meta-analysis.
Results of Systematic Review of Genital Self-Image After FGCRP
Genital self-image was evaluated in 8 studies utilizing either the Female Genital Self-Image Scale (FGSIS; 3 studies) or the Genital Appearance Satisfaction (GAS; 5 studies) (Table 4).30,31 Goodman et al utilized the FGSIS and indicated that 24 months after surgery the study group (n = 120) showed significantly improved genital self-image compared with baseline, with no difference in the control group n = 50).27 Additionally, in the study by Cihantimur et al in which the FGSIS was implemented, 97 females underwent labia majora augmentation by autologous fat injection; at 6- and 12-month follow-up, genital self-image compared with preoperation self-image had significantly improved.32 Zhou et al's study employed the FGSIS for 136 females, and 3 months after the surgery they showed significantly improved genital self-image compared with baseline.24 Studies that utilized FGSIS were not sufficient for meta-analysis.
Basic Characteristics of Studies Included in the Genital Self-Image Systematic Review
| Author, country, year . | Study design . | Sample size . | Mean age ± SD, year (range) . | Procedure type . | Labiaplasty technique . | Follow-up time . | Genital body image instrument . | Result (Mean ± SD) . |
|---|---|---|---|---|---|---|---|---|
| Goodman et al, USA, 2016 | Prospective cohort case-control study | Study = 120 Control = 50 | Study: 32.74 ± 10.14 (18-63) Control: 33.20 ± 9.58 (18-58) | Labiaplasty, clitoral hood reduction, and/or aesthetic vaginal tightening | Not reported | 6,12, and 24 months | FGSIS | Preprocedure: Study: 15.58 Control: 22.10 P = .0001 6 months: Study: 21.02 Control: 22.50 P = .104 12 months: Study: 23.5 c/w entry: P <0.0001 c/w control: P = .192 24 months: Study: 23.94 c/w entry: P < .0001 c/w control: P = .192 |
| Cihantimur et al, Turkey, 2021 | Prospective | 97 | 33.4 ± 4.2 (Not reported) | Labia majora augmentation (360 genital fat transfer) | 6 and 12 months | FGSIS | Preprocedure: 17.7 ± 1.6 6 months: 20.9 ± 1.4 c/w pre: P < .0001 12 months: 22.2 ± 1.8 c/w pre: P = .013 | |
| Zhou et al, China, 2022 | Retrospective | 136 | 31.6 ± 8.82 (21-53) | Labiaplasty with Clitoral Hood Reduction | Trilobal labiaplasty using edge excision labiaplasty, wedge labiaplasty, and clitoral hood reduction | 3 months | FGSIS | Preprocedure: 10.81 ± 2.67 3 months: 24.84 ± 3.47 P < .001 |
| Veale et al, England, 2014 | Prospective case-control study | Study = 49 Control = 39 | Median (IQR): Study: 34 (25-43) Control: 28 (25-34) | Labiaplasty | Labial trimming, central wedge reduction, de-epithelization technique, superior pedicle flap reconstruction | 3 months | GAS | Median scores (IQR) Preprocedure: Study: 23.5 (20-27) Control: 7 (6-8) P < .0005 3 months: Study: 4 (1-11.5) Control: 2 (0-6) P = .084 |
| Propst et al, USA, 2020 | Cross-sectional study of a retrospective cohort | 21 | 30 ± 12 (at least 18 years old) | Labiaplasty | Simple edge resection with single-layer closure | Median time: 36 months (3-111 months) | GAS | 3-111 months: 7.9 ± 3.6 |
| Jiang et al, China, 2021 | Clinical trial | Study (modified labiaplasty) = 29 Control (traditional labiaplasty) = 14 | Study: 31.8 ± 7.1 (22-50) Control: 26.6 ± 4.1 (20-35) | Labiaplasty | 1. Combination of central wedge de-epithelialization on the medial side with edge resection 2. Central wedge resection | 6 months | GAS | Preprocedure; Study: 22.5 ± 7.1 Control (mLP): 21.9 ± 4.5 P = .78 6 months: Study: 4.0 ± 3.6 Control (mLP): 4.6 ± 3.7 c/w Control: P = .63 c/w pre: P < .001 |
| Sharp et al, Australia, 2016 | Prospective controlled design | Study: 29 Control: 22 | Study: 32.0 ± 9.5 (18-56) Control: 35.9 ± 9.8 (21-55) | Labiaplasty | Not reported | 6 months | GAS | Baseline: Study: 25.4 ± 4.9 Control: 6.6 ± 7.3 P < .001 6 months: Study: 6.6 ± 6.5 Control: 6.4 ± 7.3 P > .05 |
| Sharp et al, Australia, 2017 | Retrospective | 48 | 39.4 ± 11.6 (19-60) | Labiaplasty | Not reported | Mean time: 44.4 months (3-204 months) | GAS | Baseline: 22.81 ± 6.59 3-204 months: 5.69 ± 5.41 P < .001 |
| Author, country, year . | Study design . | Sample size . | Mean age ± SD, year (range) . | Procedure type . | Labiaplasty technique . | Follow-up time . | Genital body image instrument . | Result (Mean ± SD) . |
|---|---|---|---|---|---|---|---|---|
| Goodman et al, USA, 2016 | Prospective cohort case-control study | Study = 120 Control = 50 | Study: 32.74 ± 10.14 (18-63) Control: 33.20 ± 9.58 (18-58) | Labiaplasty, clitoral hood reduction, and/or aesthetic vaginal tightening | Not reported | 6,12, and 24 months | FGSIS | Preprocedure: Study: 15.58 Control: 22.10 P = .0001 6 months: Study: 21.02 Control: 22.50 P = .104 12 months: Study: 23.5 c/w entry: P <0.0001 c/w control: P = .192 24 months: Study: 23.94 c/w entry: P < .0001 c/w control: P = .192 |
| Cihantimur et al, Turkey, 2021 | Prospective | 97 | 33.4 ± 4.2 (Not reported) | Labia majora augmentation (360 genital fat transfer) | 6 and 12 months | FGSIS | Preprocedure: 17.7 ± 1.6 6 months: 20.9 ± 1.4 c/w pre: P < .0001 12 months: 22.2 ± 1.8 c/w pre: P = .013 | |
| Zhou et al, China, 2022 | Retrospective | 136 | 31.6 ± 8.82 (21-53) | Labiaplasty with Clitoral Hood Reduction | Trilobal labiaplasty using edge excision labiaplasty, wedge labiaplasty, and clitoral hood reduction | 3 months | FGSIS | Preprocedure: 10.81 ± 2.67 3 months: 24.84 ± 3.47 P < .001 |
| Veale et al, England, 2014 | Prospective case-control study | Study = 49 Control = 39 | Median (IQR): Study: 34 (25-43) Control: 28 (25-34) | Labiaplasty | Labial trimming, central wedge reduction, de-epithelization technique, superior pedicle flap reconstruction | 3 months | GAS | Median scores (IQR) Preprocedure: Study: 23.5 (20-27) Control: 7 (6-8) P < .0005 3 months: Study: 4 (1-11.5) Control: 2 (0-6) P = .084 |
| Propst et al, USA, 2020 | Cross-sectional study of a retrospective cohort | 21 | 30 ± 12 (at least 18 years old) | Labiaplasty | Simple edge resection with single-layer closure | Median time: 36 months (3-111 months) | GAS | 3-111 months: 7.9 ± 3.6 |
| Jiang et al, China, 2021 | Clinical trial | Study (modified labiaplasty) = 29 Control (traditional labiaplasty) = 14 | Study: 31.8 ± 7.1 (22-50) Control: 26.6 ± 4.1 (20-35) | Labiaplasty | 1. Combination of central wedge de-epithelialization on the medial side with edge resection 2. Central wedge resection | 6 months | GAS | Preprocedure; Study: 22.5 ± 7.1 Control (mLP): 21.9 ± 4.5 P = .78 6 months: Study: 4.0 ± 3.6 Control (mLP): 4.6 ± 3.7 c/w Control: P = .63 c/w pre: P < .001 |
| Sharp et al, Australia, 2016 | Prospective controlled design | Study: 29 Control: 22 | Study: 32.0 ± 9.5 (18-56) Control: 35.9 ± 9.8 (21-55) | Labiaplasty | Not reported | 6 months | GAS | Baseline: Study: 25.4 ± 4.9 Control: 6.6 ± 7.3 P < .001 6 months: Study: 6.6 ± 6.5 Control: 6.4 ± 7.3 P > .05 |
| Sharp et al, Australia, 2017 | Retrospective | 48 | 39.4 ± 11.6 (19-60) | Labiaplasty | Not reported | Mean time: 44.4 months (3-204 months) | GAS | Baseline: 22.81 ± 6.59 3-204 months: 5.69 ± 5.41 P < .001 |
c/w, compared with; FGSIS, Female Genital Self-Image Scale; GAS, Genital Appearance Satisfaction; IQR, interquartile range; mLP, modified labiaplasty; pre, preprocedure; SD, standard deviation.
Basic Characteristics of Studies Included in the Genital Self-Image Systematic Review
| Author, country, year . | Study design . | Sample size . | Mean age ± SD, year (range) . | Procedure type . | Labiaplasty technique . | Follow-up time . | Genital body image instrument . | Result (Mean ± SD) . |
|---|---|---|---|---|---|---|---|---|
| Goodman et al, USA, 2016 | Prospective cohort case-control study | Study = 120 Control = 50 | Study: 32.74 ± 10.14 (18-63) Control: 33.20 ± 9.58 (18-58) | Labiaplasty, clitoral hood reduction, and/or aesthetic vaginal tightening | Not reported | 6,12, and 24 months | FGSIS | Preprocedure: Study: 15.58 Control: 22.10 P = .0001 6 months: Study: 21.02 Control: 22.50 P = .104 12 months: Study: 23.5 c/w entry: P <0.0001 c/w control: P = .192 24 months: Study: 23.94 c/w entry: P < .0001 c/w control: P = .192 |
| Cihantimur et al, Turkey, 2021 | Prospective | 97 | 33.4 ± 4.2 (Not reported) | Labia majora augmentation (360 genital fat transfer) | 6 and 12 months | FGSIS | Preprocedure: 17.7 ± 1.6 6 months: 20.9 ± 1.4 c/w pre: P < .0001 12 months: 22.2 ± 1.8 c/w pre: P = .013 | |
| Zhou et al, China, 2022 | Retrospective | 136 | 31.6 ± 8.82 (21-53) | Labiaplasty with Clitoral Hood Reduction | Trilobal labiaplasty using edge excision labiaplasty, wedge labiaplasty, and clitoral hood reduction | 3 months | FGSIS | Preprocedure: 10.81 ± 2.67 3 months: 24.84 ± 3.47 P < .001 |
| Veale et al, England, 2014 | Prospective case-control study | Study = 49 Control = 39 | Median (IQR): Study: 34 (25-43) Control: 28 (25-34) | Labiaplasty | Labial trimming, central wedge reduction, de-epithelization technique, superior pedicle flap reconstruction | 3 months | GAS | Median scores (IQR) Preprocedure: Study: 23.5 (20-27) Control: 7 (6-8) P < .0005 3 months: Study: 4 (1-11.5) Control: 2 (0-6) P = .084 |
| Propst et al, USA, 2020 | Cross-sectional study of a retrospective cohort | 21 | 30 ± 12 (at least 18 years old) | Labiaplasty | Simple edge resection with single-layer closure | Median time: 36 months (3-111 months) | GAS | 3-111 months: 7.9 ± 3.6 |
| Jiang et al, China, 2021 | Clinical trial | Study (modified labiaplasty) = 29 Control (traditional labiaplasty) = 14 | Study: 31.8 ± 7.1 (22-50) Control: 26.6 ± 4.1 (20-35) | Labiaplasty | 1. Combination of central wedge de-epithelialization on the medial side with edge resection 2. Central wedge resection | 6 months | GAS | Preprocedure; Study: 22.5 ± 7.1 Control (mLP): 21.9 ± 4.5 P = .78 6 months: Study: 4.0 ± 3.6 Control (mLP): 4.6 ± 3.7 c/w Control: P = .63 c/w pre: P < .001 |
| Sharp et al, Australia, 2016 | Prospective controlled design | Study: 29 Control: 22 | Study: 32.0 ± 9.5 (18-56) Control: 35.9 ± 9.8 (21-55) | Labiaplasty | Not reported | 6 months | GAS | Baseline: Study: 25.4 ± 4.9 Control: 6.6 ± 7.3 P < .001 6 months: Study: 6.6 ± 6.5 Control: 6.4 ± 7.3 P > .05 |
| Sharp et al, Australia, 2017 | Retrospective | 48 | 39.4 ± 11.6 (19-60) | Labiaplasty | Not reported | Mean time: 44.4 months (3-204 months) | GAS | Baseline: 22.81 ± 6.59 3-204 months: 5.69 ± 5.41 P < .001 |
| Author, country, year . | Study design . | Sample size . | Mean age ± SD, year (range) . | Procedure type . | Labiaplasty technique . | Follow-up time . | Genital body image instrument . | Result (Mean ± SD) . |
|---|---|---|---|---|---|---|---|---|
| Goodman et al, USA, 2016 | Prospective cohort case-control study | Study = 120 Control = 50 | Study: 32.74 ± 10.14 (18-63) Control: 33.20 ± 9.58 (18-58) | Labiaplasty, clitoral hood reduction, and/or aesthetic vaginal tightening | Not reported | 6,12, and 24 months | FGSIS | Preprocedure: Study: 15.58 Control: 22.10 P = .0001 6 months: Study: 21.02 Control: 22.50 P = .104 12 months: Study: 23.5 c/w entry: P <0.0001 c/w control: P = .192 24 months: Study: 23.94 c/w entry: P < .0001 c/w control: P = .192 |
| Cihantimur et al, Turkey, 2021 | Prospective | 97 | 33.4 ± 4.2 (Not reported) | Labia majora augmentation (360 genital fat transfer) | 6 and 12 months | FGSIS | Preprocedure: 17.7 ± 1.6 6 months: 20.9 ± 1.4 c/w pre: P < .0001 12 months: 22.2 ± 1.8 c/w pre: P = .013 | |
| Zhou et al, China, 2022 | Retrospective | 136 | 31.6 ± 8.82 (21-53) | Labiaplasty with Clitoral Hood Reduction | Trilobal labiaplasty using edge excision labiaplasty, wedge labiaplasty, and clitoral hood reduction | 3 months | FGSIS | Preprocedure: 10.81 ± 2.67 3 months: 24.84 ± 3.47 P < .001 |
| Veale et al, England, 2014 | Prospective case-control study | Study = 49 Control = 39 | Median (IQR): Study: 34 (25-43) Control: 28 (25-34) | Labiaplasty | Labial trimming, central wedge reduction, de-epithelization technique, superior pedicle flap reconstruction | 3 months | GAS | Median scores (IQR) Preprocedure: Study: 23.5 (20-27) Control: 7 (6-8) P < .0005 3 months: Study: 4 (1-11.5) Control: 2 (0-6) P = .084 |
| Propst et al, USA, 2020 | Cross-sectional study of a retrospective cohort | 21 | 30 ± 12 (at least 18 years old) | Labiaplasty | Simple edge resection with single-layer closure | Median time: 36 months (3-111 months) | GAS | 3-111 months: 7.9 ± 3.6 |
| Jiang et al, China, 2021 | Clinical trial | Study (modified labiaplasty) = 29 Control (traditional labiaplasty) = 14 | Study: 31.8 ± 7.1 (22-50) Control: 26.6 ± 4.1 (20-35) | Labiaplasty | 1. Combination of central wedge de-epithelialization on the medial side with edge resection 2. Central wedge resection | 6 months | GAS | Preprocedure; Study: 22.5 ± 7.1 Control (mLP): 21.9 ± 4.5 P = .78 6 months: Study: 4.0 ± 3.6 Control (mLP): 4.6 ± 3.7 c/w Control: P = .63 c/w pre: P < .001 |
| Sharp et al, Australia, 2016 | Prospective controlled design | Study: 29 Control: 22 | Study: 32.0 ± 9.5 (18-56) Control: 35.9 ± 9.8 (21-55) | Labiaplasty | Not reported | 6 months | GAS | Baseline: Study: 25.4 ± 4.9 Control: 6.6 ± 7.3 P < .001 6 months: Study: 6.6 ± 6.5 Control: 6.4 ± 7.3 P > .05 |
| Sharp et al, Australia, 2017 | Retrospective | 48 | 39.4 ± 11.6 (19-60) | Labiaplasty | Not reported | Mean time: 44.4 months (3-204 months) | GAS | Baseline: 22.81 ± 6.59 3-204 months: 5.69 ± 5.41 P < .001 |
c/w, compared with; FGSIS, Female Genital Self-Image Scale; GAS, Genital Appearance Satisfaction; IQR, interquartile range; mLP, modified labiaplasty; pre, preprocedure; SD, standard deviation.
The remainder of the included studies (5 articles) employed the GAS measure, but 1 of them did not measure baseline genital image; therefore, 4 studies (with 5 study groups) were included in the next step for meta-analysis.17 In addition, it should be noted that Jiang et al conducted a clinical trial with 2 groups.33 In the study group a modified labiaplasty was performed and in the second group a traditional labiaplasty technique (central wedge resection) was performed. After 6 months, evaluation of genital image with the GAS showed no significant difference between groups; both methods led to improved genital self-image compared with baseline scores.
Meta-analysis of Evaluation of Genital Image After FGCRP by GAS Measure
Four articles were included in the meta-analysis. Jiang et al compared 2 interventional groups with 2 different labia minora labiaplasty techniques (linear edge resection and a modified lateral edge wedge with medial edge resection).33 Outcomes from each group were included separately (as 2 independent studies) in the meta-analysis along with the 3 other studies that utilized GAS measures and reported presurgical and postsurgical assessments; 4 articles with 5 study groups were included in the final meta-analysis.29,34,35
The results of the final analysis of 5 studies, with 146 participants, showed that the mean GAS score after FGCRP had increased by 17.96 points (95% CI, 16.96-18.95), which was statistically significant; the range of the measure was 0 to 33. The studies had admissible homogeneity and I2 was 0.0% (variation in ES attributable to heterogeneity; test of ES = 0: z = 35.51, P < .001); see Table 5 and Figure 2. For publication bias assessment, a funnel plot was generated. In the current study, no publication bias was reported for genital self-image, and the funnel plot appeared to be symmetric (Figure 3).
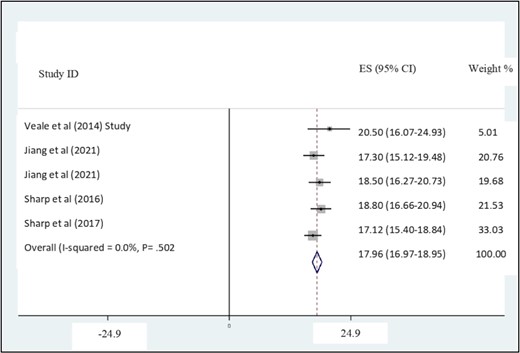
Forest plot for Genital Appearance Satisfaction (GAS) studies. CI, confidence interval; ES, effect size.
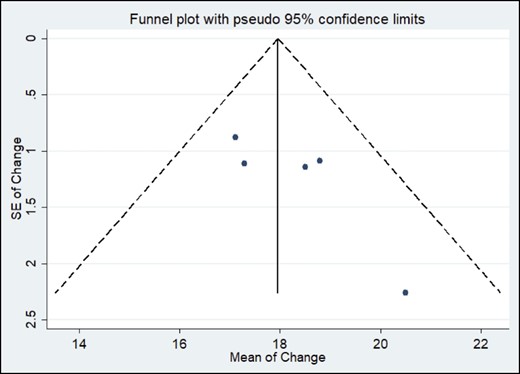
Funnel plot of the logit-transformed standard error (SE) of Genital Appearance Satisfaction (GAS) studies.
Meta-analysis of Genital Appearance Satisfaction (GAS) Change Scores After Female Genital Cosmetic and Reconstructive Procedure
| Study ID . | Sample size . | ES . | Lower limit 95% CI . | Upper limit 95% CI . | % Weight . |
|---|---|---|---|---|---|
| Veale et al (2014)a | 26 | 20.500 | 16.070 | 24.930 | 5.01 |
| Jiang et al (2021) (traditional method) | 14 | 17.300 | 15.124 | 19.476 | 20.76 |
| Jiang et al (2021) (modified method) | 29 | 18.500 | 16.266 | 20.734 | 19.68 |
| Sharp et al (2016) | 29 | 18.800 | 16.664 | 20.936 | 21.53 |
| Sharp et al (2017) | 48 | 17.120 | 15.395 | 18.845 | 33.03 |
| I-V pooled ES | N/A | 17.960 | 16.969 | 18.951 | 100.00 |
| Study ID . | Sample size . | ES . | Lower limit 95% CI . | Upper limit 95% CI . | % Weight . |
|---|---|---|---|---|---|
| Veale et al (2014)a | 26 | 20.500 | 16.070 | 24.930 | 5.01 |
| Jiang et al (2021) (traditional method) | 14 | 17.300 | 15.124 | 19.476 | 20.76 |
| Jiang et al (2021) (modified method) | 29 | 18.500 | 16.266 | 20.734 | 19.68 |
| Sharp et al (2016) | 29 | 18.800 | 16.664 | 20.936 | 21.53 |
| Sharp et al (2017) | 48 | 17.120 | 15.395 | 18.845 | 33.03 |
| I-V pooled ES | N/A | 17.960 | 16.969 | 18.951 | 100.00 |
The standard deviation before surgery was not reported, but it was estimated according to the corresponding author's comment. For the estimation, assuming the same variance before and after the intervention, the standard deviation after the intervention was considered to be 11.5, as was estimate of the standard deviation before the intervention. Heterogeneity chi-squared = 3.35 (d.f. = 4), P = .502. I2 (variation [I-V] in ES attributable to heterogeneity) = 0.0%. Test of ES = 0: z = 35.51, P = .000. CI, confidence interval; ES, effect size; N/A, not applicable; df, degree of freedom.
Meta-analysis of Genital Appearance Satisfaction (GAS) Change Scores After Female Genital Cosmetic and Reconstructive Procedure
| Study ID . | Sample size . | ES . | Lower limit 95% CI . | Upper limit 95% CI . | % Weight . |
|---|---|---|---|---|---|
| Veale et al (2014)a | 26 | 20.500 | 16.070 | 24.930 | 5.01 |
| Jiang et al (2021) (traditional method) | 14 | 17.300 | 15.124 | 19.476 | 20.76 |
| Jiang et al (2021) (modified method) | 29 | 18.500 | 16.266 | 20.734 | 19.68 |
| Sharp et al (2016) | 29 | 18.800 | 16.664 | 20.936 | 21.53 |
| Sharp et al (2017) | 48 | 17.120 | 15.395 | 18.845 | 33.03 |
| I-V pooled ES | N/A | 17.960 | 16.969 | 18.951 | 100.00 |
| Study ID . | Sample size . | ES . | Lower limit 95% CI . | Upper limit 95% CI . | % Weight . |
|---|---|---|---|---|---|
| Veale et al (2014)a | 26 | 20.500 | 16.070 | 24.930 | 5.01 |
| Jiang et al (2021) (traditional method) | 14 | 17.300 | 15.124 | 19.476 | 20.76 |
| Jiang et al (2021) (modified method) | 29 | 18.500 | 16.266 | 20.734 | 19.68 |
| Sharp et al (2016) | 29 | 18.800 | 16.664 | 20.936 | 21.53 |
| Sharp et al (2017) | 48 | 17.120 | 15.395 | 18.845 | 33.03 |
| I-V pooled ES | N/A | 17.960 | 16.969 | 18.951 | 100.00 |
The standard deviation before surgery was not reported, but it was estimated according to the corresponding author's comment. For the estimation, assuming the same variance before and after the intervention, the standard deviation after the intervention was considered to be 11.5, as was estimate of the standard deviation before the intervention. Heterogeneity chi-squared = 3.35 (d.f. = 4), P = .502. I2 (variation [I-V] in ES attributable to heterogeneity) = 0.0%. Test of ES = 0: z = 35.51, P = .000. CI, confidence interval; ES, effect size; N/A, not applicable; df, degree of freedom.
DISCUSSION
This appears to be the first systematic review and meta-analysis of body and genital self-image after FGCRP. A highly inclusive approach was adopted and encompassed all types of surgical FGCRP to improve the aesthetic appearance and/or function of the female genitalia (excluding FGCRP for medical indications), and any type of research method that employed quantitative methods to measure body or genital self-image. Labiaplasty was the most common procedure in our systematic review, referring to surgical reduction of “larger-sized” labia, with the understanding that no criteria exist to support a description of labia minora hypertrophy, and the idea of normal labia minora size varies between females, healthcare professionals, and cultures.36
Body image appraisal was performed in 5 studies, and 2 standardized instruments were applied. One of them, the BDD-YBOCS, was utilized in 2 studies.25,27,28 Large sample size (120 females in the intervention group) and significant follow-up (24 months) were 2 strengths of Goodman and colleagues’ study.27 The findings of this study showed that, at baseline, the surgical patients had higher (more dysmorphic) scores than the control group, in a range considered mildly to moderately dysmorphic according to Phillips’s criteria and the Diagnostic and Statistical Manual of Mental Disorders Text Revision (DSM-IV-TR).25,37 In this study, at 6 months after surgery positive effects of FGCRP on body image were minimal, but at 12 and 24 months following surgery body image scores of the FGCRP group had improved to mirror or exceed the control group's scores.
Another body image tool in our review was the BIQLI, implemented in 3 studies.17,23,26,29 The pilot study, small sample size (21 people), only postoperative evaluation, and lack of a control group limited interpretation of Propst and Ferrando's study.17 Veale et al's and Eftekhar et al's studies were concordant with respect to the outcome of positive effects of FGCRP on body image, but Eftekhar et al's results must be interpreted with caution, because follow-up was limited to 3 months. A follow-up time of at least 6 months is recommended for evaluating psychological outcomes of FGCRP to limit the impact of cognitive dissonance.38,39 All of the articles that were included in the systematic review of body image after FGCRP revealed a positive effect of procedures.23,27,28
Seven studies were included in the systematic review of genital self-image after FGCRP. The most common measures (in 5 of the studies), was the GAS scale. Veale et al validated the GAS in females seeking labiaplasty and recommended this scale for audit and outcome monitoring of interventions for females distressed by the appearance or function of their genitalia.40
All included studies showed that FGCRP improved genital self-image. Follow-up time was varied but most commonly 6 months, although Goodman et al's study reported a 24-month follow-up.27 The meta-analysis indicated a 17.96 improvement in GAS score after FGCRP, which was a substantial and significant increase, particularly considering the range of the measure's score (0 to 33).
All included articles demonstrated the positive effect of genital cosmetic and reconstructive procedures on body and genital self-image. Regardless of the methodological differences, the benefits are undeniable. FGCRP appears to have a positive impact on psychological health and self-esteem, and, according to several of the studies reported here, a salutary effect on sexual function and satisfaction.15,23,27,29,34,39,41
A female’s comfort with her body directly influences her sexual satisfaction. Pujols and colleagues revealed by performing multiple regression analysis that sexual satisfaction was predicted by high body esteem and low frequency of appearance-based distracting thoughts during sexual activity, even after controlling for sexual function status.18
Chronic attentiveness to one's own body may interfere with sexual activity and hinder females’ sexual function.42 It has been reported that in females experiencing pelvic organ prolapse (POP) sexual function appears to be more affected by body image than the topographical changes of POP.43
The detrimental impact of negative genital perceptions on young females’ sexual well-being was described by the study of Schick et al, which indicated that poor genital image was associated with higher genital self-consciousness during sexual activities and, in turn, associated with lower sexual esteem and sexual satisfaction.44 Body dissatisfaction has been associated with sexual avoidance, engaging in sexual behaviors that are not of one's choosing, less sexual agency, and more acceptance of risky sexual behaviors.45,46
Additionally, it may be concluded that self-objectification and mental self-occupation is a key to the connection of poor body/genital image to poor psychological and sexual consequences.47,48 Overall, this novel review provides an important platform for future research regarding FGCRP. It helps to answer one of the most fundamental questions in labiaplasty research in a rigorous and systematic manner: “Do females who undergo labiaplasty surgery feel better about their genital appearance afterward?” The answer appears to be “yes” based on the limited research currently available. With multiple studies indicating that genital self-image concerns are the primary motivator for females to seek labiaplasty, the findings of this review can be discussed by surgeons with their patients in their initial consultations and assist with clinical decision-making.
Study Limitations
This review has several limitations. Attention to the limitations of this research will help evaluate the strength of the results. The extant research is heterogenous and the methodology varied. None of the studies separated cases based on severity, despite the subjectivity of this measure. Due to the impossibility of blinding participants, the effect of suggestion and inculcation on the results is unknown. Due to the limitations of the literature included, it also was not possible to examine whether the seemingly positive impacts of FGCRP on body image and genital self-image differ by demographic characteristics of the patient (eg, age, cultural background). This should be explored in future research.
Furthermore, because the articles were mainly written by or with the participation of experienced and skilled surgeons, their outcomes may be more aesthetic and their complication rates lower than those of their less experienced colleagues. Additionally, the income of cosmetic and reconstructive surgeons depends largely upon cosmetic procedures, presenting an incentive to report positive outcomes.
Finally, there also were not enough papers that utilized the same instruments to conduct more extensive meta-analyses. Future research should employ a standard battery of measures such as the GAS for genital self-image and BIQLI for body image to allow for higher quality reviews and meta-analyses.49
CONCLUSIONS
Female genital cosmetic and reconstructive procedures have become more widespread and popular. The present study is the first systematic review of body perception after FGCRP and indicates that these surgeries, predominantly labiaplasties, improved females’ body image and genital self-image. Stronger research protocols, however, are needed to obtain more accuracy and certainty regarding these findings. Additionally, long-term effects and the costs and benefits of these surgeries have not been assessed. Future research should focus on conducting prospective controlled studies in which standard batteries of outcome measures are employed with longer-term follow-up. This will enrich our knowledge and allow for the conduct of larger higher quality meta-analyses to be performed.
Supplemental Material
This article contains supplemental material located online at www.aestheticsurgeryjournal.com.
Acknowledgments
This study is related to project NO 1401/4674 from the Student Research Committee, Shahid Beheshti University of Medical Sciences, Tehran, Iran. The authors also thank the Student Research Committee and the Research and Technology Chancellor at Shahid Beheshti University of Medical Sciences for their financial support of this study. Drs Sharp and Nahidi contributed equally and are senior coauthors.
Disclosures
The authors declared no potential conflicts of interest with respect to the research, authorship, and publication of this article.
Funding
This study is related to project NO 1401/59298 from the Student Research Committee, Shahid Beheshti University of Medical Sciences, Tehran, Iran. The funding body had no input on the design, conduct, or analysis of the systematic review and meta-analysis.
REFERENCES
Author notes
Ms Alavi-Arjas is a PhD student of reproductive health at the Student Research Committee, Department of Midwifery and Reproductive Health, School of Nursing and Midwifery, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
Dr Goodman is an assistant clinical professor, Department of Ob/Gyn, California Northstate University College of Medicine, Sacramento, CA, USA.
Dr Simbar is a professor of Reproductive Health at the Department of Midwifery and Reproductive Health, Midwifery and Reproductive Health Research Center, School of Nursing and Midwifery, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
Dr Majd is a professor of biostatistics, Department of Biostatistics, School of Paramedicine, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
Dr Sharp is an associate professor of research, Department of Neuroscience, Monash University, Melbourne, Victoria, Australia, and an interspecialty consulting editor for Aesthetic Surgery Journal.
Dr Nahidi is an associate professor of health education and promotion at the Department of Midwifery and Reproductive Health, Midwifery and Reproductive Health Research Center, School of Nursing and Midwifery, Shahid Beheshti University of Medical Sciences, Tehran, Iran.



