-
PDF
- Split View
-
Views
-
Cite
Cite
Gianfranco Frojo, Sameer H Halani, Joel E Pessa, Pat Pazmiño, Simeon Wall, Jeffrey M Kenkel, Daniel A Del Vecchio, Deep Subcutaneous Gluteal Fat Compartments: Anatomy and Clinical Implications, Aesthetic Surgery Journal, Volume 43, Issue 1, January 2023, Pages 76–83, https://doi.org/10.1093/asj/sjac230
Close - Share Icon Share
Abstract
Advances in gluteal fat grafting have resulted in diminished risks through improved understanding of regional anatomy and technical nuances. No anatomic studies identifying the presence or absence of buttock fat compartments have yet been reported.
The aim of this cadaveric study was to identify and characterize the deep subcutaneous gluteal fat compartments to further understand the nuanced differences between deep and superficial subcutaneous fat layers.
A cadaveric study was performed to identify the fat compartments. Latex injection into the iliac artery and vein was used to prepare 4 fresh (N = 8 hemibuttocks) hydrated cadavers for dissection. Preliminary work identified the likely position of deep gluteal fat compartments. The cannula was positioned under ultrasound guidance in between the superficial and deep gluteal layers. Cadaveric buttocks were infiltrated by the static technique with dyed human fat, dyed applesauce, and dyed saline in an attempt to identify the gluteal deep subcutaneous fat compartments.
Dissection identified and characterized 7 discrete deep gluteal fat compartments. These comprise 3 medial fat compartments (superior, middle, and inferior); a central fat compartment; and 3 lateral (superior, middle, and inferior) deep fat compartments.
Seven deep gluteal fat compartments have been identified that have distinct boundaries and maintain injected contents separate from each other above the gluteal muscle fascia. These compartments can be selectively expanded for buttock augmentation. Knowledge of these compartments enables surgeons to perform gluteal augmentation by static infiltration, injecting autologous fat under ultrasound guidance in the deep subcutaneous fat layer, while optimizing aesthetic considerations.
Los avances en el injerto de grasa glútea han dado como resultado una disminución de los riesgos a través de una mejor comprensión de la anatomía regional y los matices técnicos. Aún no se ha informado de estudios anatómicos que identifiquen la presencia o ausencia de compartimentos grasos en los glúteos.
El objetivo de este estudio cadavérico fue identificar y caracterizar los compartimentos profundos de grasa glútea subcutánea a fin de comprender mejor las diferencias detalladas entre las capas de grasa subcutánea profunda y superficial.
Se realizó un estudio cadavérico para identificar los compartimentos de grasa. Se empleó una inyección de látex en la arteria y vena ilíacas para preparar 4 cadáveres hidratados frescos (N=8 hemiglúteos) para su disección. El trabajo preliminar identificó la probable posición de los compartimentos profundos de grasa glútea. Se posicionó la cánula bajo guía de ultrasonido entre las capas glúteas superficial y profunda. Los glúteos cadavéricos se infiltraron con grasa humana teñida, puré de manzana teñido y solución salina teñida usando la técnica estática en un intento por identificar los compartimentos de grasa subcutánea profunda en los glúteos.
La disección identificó y caracterizó 7 compartimentos discretos de grasa glútea profunda. Éstos comprenden 3 compartimentos de grasa medial (superior, medio e inferior), un compartimento de grasa central y 3 compartimentos laterales (superior, medio e inferior) de grasa profunda.
Se han identificado siete compartimentos profundos de grasa glútea que tienen límites distintos y mantienen los contenidos inyectados separados entre sí por encima de la fascia del músculo glúteo. Estos compartimentos se pueden expandir selectivamente para el aumento de glúteos. El conocimiento de estos compartimentos permite a los cirujanos realizar el aumento de glúteos mediante infiltración estática, inyectando grasa autóloga bajo guía de ultrasonido en la capa de grasa subcutánea profunda, al tiempo que se optimizan las consideraciones estéticas.
See the Commentary on this article here.
Our understanding of safe practices in gluteal fat grafting has evolved rapidly over the past several years.1–14 Dynamic cadaver studies have shown that fat graft placed under the deep gluteal fascia (DGF) can easily migrate through the gluteus maximus muscle. When this intramuscular fat graft enters an injured gluteal vein, the fat can travel to the heart and lungs, resulting in a fat pulmonary embolism with potentially fatal results. These findings led to the evolution of a “subcutaneous-only” gluteal fat grafting technique now advocated by many surgeons3,15 and by a number of plastic surgery societies.16–19 Additionally, a publication titled “Practice Advisory on Gluteal Fat Grafting” was released in April 2022, promoting safety guidelines for gluteal fat grafting.4 These guidelines focus on ensuring correct anatomic placement and eliminating distraction and fatigue. The 10 main principles of the Advisory include restriction of fat placement to the subcutaneous plane, the use of ultrasound guidance to correctly identify and document the layer of fat placement, avoiding the use of Luer-Lock syringes, the use of roller pump techniques for graft volumes >200 mL, using cannulas 4 mm or greater for inserting fat, minimizing distraction and operator fatigue during transplantation, utilizing a “single-surgeon” approach, and performing no more than 3 gluteal fat grafting cases per day.
Although subcutaneous-only gluteal fat grafting is safe, surgeons still need a technique to confirm the subcutaneous placement of fat graft in every case. Intraoperative ultrasound filled this unmet clinical need by enabling surgeons to confirm their subcutaneous placement of fat graft. Ultrasound visualization also revealed 2 distinct subcutaneous fascial layers: the DGF (ie, gluteal muscle fascia) which encases the exterior surface of the gluteus maximus muscle; and the superficial gluteal fascia (SGF), which is analogous to Scarpa’s fascia (ie, superficial fascial system [SFS]) and lies under the dermis and above the DGF. There are also 2 distinct fat subcutaneous layers, the superficial fat subcutaneous space, which is below the dermis and above the SGF, and the deep fat subcutaneous space, which is below the SGF and above the DGF (Figure 1).
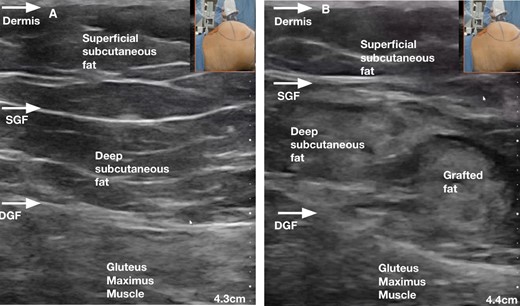
(A) Ultrasound image demonstrating the anatomic layers of the gluteal region prior to any infiltration of fat graft. (B) Ultrasound image demonstrating the anatomic layers of the gluteal region after injection of fat graft below the SGF into the “deep subcutaneous fat layer”, with preservation of the DGF (bottom arrow). DGF, deep gluteal fascia (ie, gluteus maximus muscle fascia); SGF, superficial gluteal fascia (ie, superficial fascial system).
Intraoperative ultrasound enables the surgeon: (1) to confirm their fat graft remains subcutaneous; (2) to avoid injury to the SGF and DGF; and (3) to specifically target either the superficial or deep subcutaneous spaces.4,15 As described by Pazmino and Del Vecchio, static injection, migration, and equalization (SIME) appears to be a safe and effective way to augment the gluteal region by confirming the placement of fat graft in the deep subcutaneous space with a static cannula, allowing the migration of fat through the deep subcutaneous space compartments, and then utilizing a moving cannula to equalize the fat graft as needed.4
During the evolution of the SIME approach, it was noted that fat migrated within the deep subcutaneous space but radial expansion appeared to halt, suggesting a clear demarcation of the deposition of fat.20 The clear divide seen clinically led to the theory that there may be anatomic compartments in the deep subcutaneous space (beneath the superficial or Scarpa’s fascia) fat layer that consisted of fibroseptal portioning membranes, similar to those seen in the face.20 Knowledge of the anatomy of facial fat compartments improved our understanding and enabled more precise control when treating the aging face.20 The purpose of this study was to investigate and potentially demonstrate evidence of deep gluteal fat compartments in a cadaveric model.
METHODS
A total of 8 (N = 8) hemibuttock dissections were performed in 4 fresh female human cadaver specimens (age range, 47-68 years) with permission from both the University of Texas Southwestern Medical Center IRB (IRB Plastic Surgery Tissue Bank STU 062011-113) and the Willed Body Program at the University of Texas Southwestern Medical Center. The study was conducted from March 24 to March 27, 2022. All specimens were prepared as follows. An anterior transabdominal (Pfannenstiel) approach was used to identify and cannulate the bilateral internal iliac arteries and veins. Next, the vessels were flushed with normal saline to clear the vessels and their respective angiosomes of pooled, dependent, and clotted blood to enhance visualization of both the topographic buttock anatomy and the subcutaneous tissues. Arterial and venous latex injection was then performed to facilitate identification of the gluteal vessels and more superficial septocutaneous perforators. The specimens were stored in the prone position prior to infiltration and dissection. A series of 3 injections were performed to evaluate the different compartments of the buttock: dyed human fat, (water-soluble) dyed saline, and dyed applesauce.
Human Fat Injection
The fat was harvested from 2 patients by separation, aspiration, and fat equalization technique (SAFE)21 liposuction and then immediately stored at 4°C in a refrigerator for use the following day. One gram of water-soluble Eosin Y (S119830; Sigma-Aldrich, Saint Louis, MO) was utilized for each 200 mL of fat. The fat was stained with a specific process that permits extracellular and intracellular staining. Then, 2 mL of a 10% solution of Oil Red O (00625; Sigma-Aldrich) was dissolved in 100 mL of 91% isopropyl alcohol and strained through a 20-micron filter. Fat was then rinsed with 200 mL of normal saline. Incisions (4 mm) in the superior aspect of the natal gluteal cleft, posterior superior iliac crest centrally, and inferior gluteal cleft were used to approach the buttock from the cranial and caudal directions, respectively. The fat was injected with a 4 mm angled basket cannula attached to a power-assisted handpiece (Microaire Surgical Instruments, Charlottesville, VA), using a roller infusion pump at a rate of 750 mL/minute. All infiltration was performed under ultrasound guidance (Clarius, Vancouver, Canada) and done statically. Full-thickness, cross-sectional cuts were made through the skin to the gluteus maximus muscle to visualize partitioning of injected fat within discrete compartments.
Dyed Applesauce Injection
Dyed applesauce, in a similar color schema as above, was used as a proxy for fat graft, to further delineate the anatomic boundaries of the gluteal fat compartments.6 Infiltration and dissection were performed as described above.
Dyed Saline Injection
Water-soluble dyes were used in various colors, including orange, purple, blue, green, and black. Preliminary work was performed on multiple specimens to identify the optimal staining techniques and colors for capturing the fat compartments, as previously described.20 The dyes were mixed with normal saline in concentrations high enough to ensure adequate staining of the fat in the buttocks. The dyed saline was then drawn into 60-mL Luer-Lock syringes and infiltrated into the buttock with an 18-gauge spinal needle. All infiltration was performed under ultrasound guidance where the dermis, SFS or SGF, the gluteus maximus fascia or deep muscle fascia, and the gluteus maximus muscle were visualized. Infiltration of the dye was restricted to the deep subcutaneous fat layer (ie, below the SFS and above the deep gluteus muscle fascia) and was visualized for the entire time of infiltration (Figure 1, Video 19. Move Video 1 to the top of the page, left column.). Volumes of infiltrated dye varied depending on the body habitus of the specimens, with an endpoint of localized turgor in the tissue with minimal peau d’orange of the skin. Total volumes per area ranged from 60 to 180 mL to the predetermined injection sites (Figure 2).

Marked injection sites of dye mixed with saline into the deep subcutaneous layer (below the superficial gluteal fascia), with their respective colors, in the cadaver hemibuttock (above).
After 10 minutes had elapsed, the skin and subcutaneous fat were sharply elevated off the cadaveric specimen at the level of the SGF. Full-thickness longitudinal and transverse cross-sectional cuts were made down to muscle at 8-cm intervals. The depth and extent of dye infiltration was assessed to verify the presence of discrete anatomic boundaries between fat compartments. This was repeated for a total of 4 hemibuttocks, injecting at different sites to assess the diffusion of the dye. Gravity as a factor in dye migration was ruled out by infiltrating 1 specimen in the lateral decubitus position.
RESULTS
Expansion Vibration Lipofilling of the Buttock
Ultrasound-guided static infiltration of human fat into the deep subcutaneous space of the hemibuttocks of the cadavers initially demonstrated isolated expansion radially, which then transitioned into an outward direction, improving projection in the buttock in the area of injection (Video 2). The infiltration of proxy fat (applesauce) demonstrated similar behavior to the identification without overlap (Video 3). Additionally, no fat was found to have migrated below the gluteal muscle fascia and there was no tearing or violation of the gluteal vessels after submuscular space exploration and identification of the vasculature. Finally, despite the static nature of the injections of fat into the deep subcutaneous space, no discrete boluses of fat were observed in the deep subcutaneous space in any of the specimens.
The Deep Gluteal Fat Compartments
Dyed saline characterized the anatomic boundaries of the deep fat compartments of the buttock. Dissection identified 7 distinct deep subcutaneous gluteal fat compartments, separated by a fibroseptal network. These compartments are as follows: 3 medial compartments (superior, middle, inferior); a central compartment; and 3 lateral (superior, middle, inferior) deep fat compartments (Figure 3).
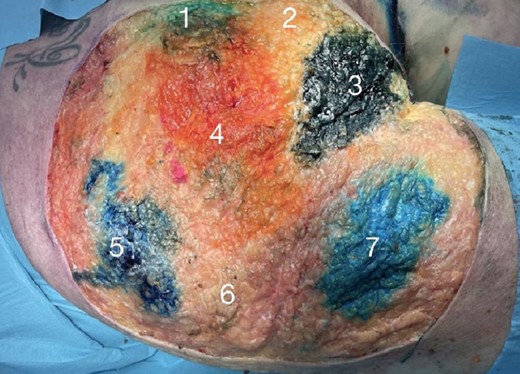
The distinct deep fat compartments of the buttocks after removal of the skin and superficial layer of fascia. These comprise: 3 medial compartments (1, superior-medial; 2, middle-medial; 3, inferior-medial); a central compartment (4); and 3 lateral (5, superior-lateral; 6, middle-lateral; 7, inferior-lateral) deep fat compartments.
The superior-medial compartment is bordered medially by the gluteal cleft, cranially by the posterior superior iliac spine and crest, and caudally by the sacrocutaneous ligament.
The middle-medial compartment is bordered medially by the gluteal cleft and the cleft adhesion, cranially by the central compartment, and caudally by the ischiocutaneous ligament and the lower medial compartment.
The inferior-medial compartment is encased by the ischiocutaneous ligament and is triangular in shape.8 It is bordered cranially by the middle-medial compartment, and caudally by the gluteal crease and the gluteal cleft adhesion. The superior-lateral compartment is bounded anteriorly by the iliotibial tract, cranially by the iliac crest, inferiorly by the middle-lateral compartment, and medially by the superior-medial and central compartments. The middle-lateral compartment lies at Mendieta’s C-point22 at the lateral mid-buttock area. This area is bound cranially by the superior-lateral compartment, medially by the central compartment, and inferior by the inferior-lateral compartment. The inferior-lateral is the most inferior of compartments and sits along the gluteal crease adhesion and extends laterally. Its boundaries include the lateral extent of the central compartment, the middle-lateral compartment, and the inferior-medial compartment.
The central compartment is the most critical and relevant for achieving adequate projection of the buttock, and is always expanded in autologous gluteal fat grafting. The central compartment is found at the most projecting point of a youthful buttock and is encircled by the other compartments. Upon repeating the experiment in the lateral decubitus position, the same distribution of dye within the 7 fat compartments was replicated.
DISCUSSION
The Aesthetic Surgery Education and Research Foundation (ASERF) Gluteal Fat Grafting Task Force released specific recommendations that have contributed to a reduction in morbidity and mortality when performing gluteal fat grafting.16,18,23 Furthermore, there have been significant contributions to the literature with respect to the understanding of the relevant anatomy and danger zones, including ligaments, gluteal vasculature location and depth, dimensional analysis of the gluteal subcutaneous spaces, and important landmarks.1,2,8,9,24,25 The increased awareness of the potential risks related to the procedure and high patient demand have led to refinements in gluteal fat grafting techniques that have improved patient safety and overall outcomes.5,26–28 It has become evident that the critical technical points are controlling cannula24 position at all times to prevent gluteal vascular injury and precisely determining the depth of fat insertion to prevent potential entry of fat under the DGF and subjecting the potentially traumatized vasculature to fat under pressure.3,26 Cadaveric studies have shown that fat injected below the gluteal fascia has the potential to migrate through the muscle belly to the deep undersurface of the gluteus maximus directly adjacent to the gluteal veins, which may contribute to the potentially fatal entry of fat into the gluteal vein and ultimately to the inferior vena cava.6 The safety recommendations from national societies further reinforced the importance of cannula position, which spurred the Florida Board of Medicine to enact their 2019 mandate that gluteal fat grafting could only be performed in the subcutaneous spaces above the DGF.12 In addition, gluteal fat grafting should only be performed by experienced board-eligible or board-certified plastic surgeons in licensed or accredited surgical facilities.
Despite these significant advances in anatomic knowledge, technique innovation, and safety warnings, there have been continued reported deaths from fat embolism, with the most recent in Miami, Florida in April 2022.10,29 Despite their best intentions, the fundamental challenge surgeons face is their inability to consistently confirm a subcutaneous-only fat graft placement with a blind injection technique. These observations have prompted surgeons to develop safer injection techniques, including 2-surgeon techniques where the surveilling surgeon uses an ultrasound probe to follow the moving cannula of the injecting surgeon, as described by Cansancao et al.15,30
As surgeons became more limited in their gluteal recipient site options, they were forced to inject more superficially. The superficial subcutaneous fat space, unlike the deep subcutaneous fat space, exhibits a regular and consistent palisading of dermofascial attachments. This more confined space is compact with fibrous septae, and overgrafting in this area may lead to flattening and contour irregularities, dermal thinning, and “blowout” deformities of the buttock.3,15 Three of the senior authors have adopted ultrasound-guided gluteal fat grafting characterized by intraoperative ultrasound-guided visualization of fat graft injection into the deep subcutaneous space directly above the DGF. This SIME concept of static injection migration equalization, as described by Pazmino and Del Vecchio, appears to be a safe and effective way to augment the gluteal region.31 The ultrasound confirms the accurate fat graft deposit via a static cannula in the deep subcutaneous space and utilizes the dynamic migration of fat to fill the deep subcutaneous space compartments. Ultrasound has filled the need of surgeons to accurately and consistently stay in the subcutaneous space and avoid injury to the muscle or deep venous system. Utilizing this technique, the authors noted distinct demarcated areas of volumization as the fat graft migrated through each deep subcutaneous compartment. Importantly, and similar to the facial fat compartments,32 the deep subcutaneous fat space allows for the flow and distribution of fat graft within each compartment. The superficial fat subcutaneous space with its increased fibroseptal network does not permit easy migration of fat graft. Applying the knowledge of the superficial and deep fat compartments of the face to the buttock and the observation that fat graft within the deep subcutaneous space is demarcated, the authors hypothesized that the buttock must also have deep fat compartments that limit the migration of injected fat. As demonstrated by Rohrich and Pessa, there is a system of fascial condensations between superficial and deep fascia that divides the superficial and deep fat facial layers into distinct compartments.20 These spaces or compartments have distinct boundaries that limit the migration of injected dye between compartments.20,32 These same vertical fascial boundaries to dye and dyed fat migration were noted in our injections of the buttock (Figure 4). The use of ultrasound-guided fat injection into the buttocks targets these distinct compartments for equal distribution of the fat and permits predictable expansion of these deep subcutaneous fat compartments to achieve a more uniform and safer gluteal augmentation without disruption of the gluteal vasculature (Figure 5).31

The distinct demarcation (white arrows) between compartments at one of the boundaries between the inferior-medial (3) and inferior-lateral (7) deep fat compartments.

Inferior gluteal arteries (pink highlight) and veins (blue highlight) unviolated after infiltration and expansion of the central deep fat compartment.
The distinct fat compartments in the buttock contribute to our understanding of optimal ways to fill these fat compartments while prioritizing patient safety. As demonstrated in our cadaveric study, the fat distributed evenly within each deep subcutaneous fat compartment while obtaining optimal fill. This was felt to be due to the paucity of connective tissue within the deep subcutaneous space, relative to the superficial subcutaneous space, allowing for migration and pressure equilibrium of grafted fat into its “like tissue” recipient site below the corresponding layer of superficial fascia.4,31 We identified 7 deep subcutaneous gluteal fat compartments that appear to correlate with clinical areas where fat graft may be utilized to augment and enhance the gluteal region. We have named these deep subcutaneous fat compartments according to anatomic position and associated clinical relevance: superior-medial, middle-medial, inferior-medial, central, inferior-lateral, superior-lateral, and medial-lateral. The superior-medial compartment is responsible for the upper buttock cleavage. Augmentation in this area accomplishes a critical attribute of an aesthetically pleasing buttocks and safe expansion can be accomplished here. The superior-lateral is responsible for the “square shape” buttock as described by Mendieta, and is also responsible for the iatrogenically caused “tombstone” deformity, as described by Del Vecchio and Wall.5,22,33 The middle-lateral compartment is located at the lateral mid-buttock area (Mendieta’s C-point); depressions in this area vary in severity and its expansion is responsible for defining a round buttock.22 The inferior-lateral is the most inferior of compartments and sits along the gluteal crease adhesion and extends laterally; this area is responsible for the “banana roll” and must be approached with caution with liposuction as it can lead to unnatural buttock aesthetics.34 The central compartment is found at the most projecting point of the youthful buttock and is encircled by the other compartments. The central compartment should always be expanded in autologous gluteal fat grafting as it is the most relevant for achieving adequate central projection. Inadvertent deep cannula placement in this central area is most likely to lead to injuries of the gluteal veins.35 The middle-medial and inferior-medial are seldom grafted. The idea of fat compartments in the gluteal region was inspired by Rohrich and Pessa’s description of the facial fat compartments, and the clinical observation of gluteal fat migration with abrupt demarcation was supported by the work of Ghavami et al, who first described a distinct subcutaneous gluteal ligament.8,20 The findings in this study suggest that there are distinct deep subcutaneous gluteal fat compartments that can be targeted for ultrasound-guided fat expansion in autologous gluteal fat grafting.
Study Limitations
There are certainly limitations to any cadaveric study, including the inability to simulate live tissue dynamics and to accurately simulate live surgery conditions for the surgeon and patient. One main concern is the possibility that the compartments identified may have been influenced by the volume of infiltrate, and its subsequent filling pressures. Although this may be possible, our reproducible results in the lateral decubitus position make this less likely. We did not attempt to identify if there were separate compartments in the superficial subcutaneous fat plane or investigate if the deep subcutaneous fat compartments extend in a similar fashion to the more superficial subcutaneous tissue plane. Other limitations include positioning, in that the specimens were not in the standard jackknife position because cadaveric specimens are only available on standardized anatomic dissection tables, a situation that does not recreate how the authors prefer to position live patients to inject fat into their buttocks. There are limitations related to each part of the methodology, specifically the inability to reproduce the same consistent color scheme in the figures and videos as we did not initially anticipate how many total compartments and dyes were required for the staining.
CONCLUSIONS
We demonstrate here the presence of 7 distinct, deep gluteal fat compartments that are separated from each other and from the gluteal muscle fascia. These compartments can be selectively expanded for buttock augmentation safely while allowing for optimal buttock aesthetics and projection—most notably the central, mid-lateral, and upper medial compartments. With knowledge of these compartments, surgeons can safely perform gluteal augmentation with autologous fat, optimizing shape aesthetics, while avoiding violation of deeper structures and improving the procedure’s safety profile.
Acknowledgments
Drs Frojo and Halani contributed equally as co-first authors.
Disclosures
Dr Wall holds patents on fat transplantation devices which are not currently commercially available. Dr Kenkel receives research grants from Bellus Medical (Dallas, TX), Venus Concept (Toronto, Canada), Allergan (Irvine, CA), and Brijjit Medical (Marietta, GA). Dr Del Vecchio receives royalties from Microaire (Charlottesville, VA) and from Wells Johnson (Tucson, AZ) for cannula designs and holds patents on fat transplantation devices which are not currently commercially available. The remaining authors declared no potential conflicts of interest with respect to the research, authorship, and publication of this article.
Funding
Funding for this investigation was provided by the University of Texas Southwestern Department of Plastic Surgery, Dallas, TX.
REFERENCES
Author notes
Dr Frojo is an aesthetic plastic surgery fellow and Dr Halani is a plastic surgery resident, Department of Plastic Surgery, University of Texas Southwestern Medical Center, Dallas, TX, USA. Dr Pessa is a plastic surgeon in private practice, Arlington, MA, USA. Dr Pazmiño is a plastic surgeon in private practice, Miami, FL, USA. Dr Wall is a plastic surgeon in private practice, Shreveport, LA, USA. Dr Kenkel is chairman and professor, Department of Plastic Surgery, University of Texas Southwestern Medical Center, Dallas, TX, USA; editor-in-chief of ASJ Open Forum; and associate editor for Aesthetic Surgery Journal. Dr Del Vecchio is a plastic surgeon, Massachusetts General Hospital, Boston, MA, USA.



