-
PDF
- Split View
-
Views
-
Cite
Cite
Jiuzuo Huang, Shouyun Feng, Ruijia Dong, Hefei Wang, Sam T Hamra, Zhigang Liu, Xiao Long, Secondary Upper Blepharoplasty: Converting Static Folds Into Dynamic Folds, Aesthetic Surgery Journal, Volume 41, Issue 5, May 2021, Pages NP188–NP195, https://doi.org/10.1093/asj/sjaa334
Close - Share Icon Share
Abstract
For the patients seeking secondary upper blepharoplasty, a static double-eyelid fold featuring an immobile lower flap and depression of the fold is common.
In this study, the authors propose a novel technique of reconstructing pretarsal tissue defects (PTDs) to converting static folds to dynamic folds.
A total of 203 patients with static folds underwent revision surgery. After complete adhesion release of the lower flap, a PTD was identified, which was defined as an area deficient of orbicularis oculi muscle in front of the tarsal plate. If the width of the PTD was over 2 mm, tissue transfer was performed to reconstruct the PTD, usually with a free retro-orbicularis oculus fat graft or a pretarsal orbicularis oculi flap.
Among the 105 patients with severe static folds, 67 received retro-orbicularis oculus fat grafts and 38 received orbicularis oculi muscle flaps. This technique converted a static fold into a dynamic fold. The surgery satisfaction rate was 86.7%. Complications included partial fold loss (n = 7, 3.4%), complete fold loss (n = 3, 1.5%), sunken upper eyelids (n = 5, 2.5%), multiple folds (n = 3, 1.5%), an unnatural curve of the double fold (n = 5, 2.5%), and asymmetric folds (n = 4, 2.0%).
To convert a static fold to a dynamic fold, we devised a technique that releases adhesion of the lower flap and reconstructs the PTD with retro-orbicularis oculus fat graft or an orbicularis oculi muscle flap. Our study achieved a high patient satisfaction rate, and the resulting fold mimicked the dynamics of the congenital double-eyelid fold.

Upper blepharoplasty is the most common aesthetic procedure in east Asia. The ideal goal of blepharoplasty is to create a dynamic fold without obvious scarring or tension.1 A dynamic fold has the following features: (1) no obvious scar on the upper eyelid when the eyes are closed, (2) the lower flap is mobile during eye opening, and (3) the fold is not too deep when the eyes are fully open or looking downward.2 A number of different techniques have been reported to create a dynamic fold.1-4 However, with the classic tarsal fixation technique,5 because there is too much pretarsal tissue resection, severe and usually high scar adhesion in the lower flap occurs. As a result, static folds are quite common. In contrast with a dynamic fold, a static fold is characterized as follows: (1) a depressed scar when the eyes are closed or gaze downward, (2) immobility of the lower flap during eye movement, (3) a deep fold when the eyes are fully open, and (4) prominent pretarsal fullness regardless of whether the eyes are open or closed.2 Because a static fold has a prominent depressed scar and immobile lower flap during eyelid movement, a dynamic fold is preferable to a static fold.2
To convert a static fold to a dynamic fold, we devised a technique that releases the adhesion and reconstructs the pretarsal tissue defect (PTD) with an orbicularis oculi muscle flap or free retro-orbicularis oculus fat (ROOF) graft. An algorithm for the static fold based on its severity is also proposed.
METHODS
Between January 2015 and February 2018, 203 patients (187 women, 16 men) with static folds underwent revision surgery. The diagnostic criteria of a static fold are as follows: (1) a depressed scar when the eyes are closed or gaze downward, (2) immobility of the lower flap during eye movement, (3) a deep fold when the eyes are fully open, and (4) prominent pretarsal fullness regardless of whether the eyes are open or closed. The patients did not receive incisional upper blepharoplasty, and patients with sunken upper eyelids or multiple upper eyelid folds were excluded.
This study was approved by the Institutional Review Board of Peking Union Medical College Hospital, Chinese Academy of Medical Science, and Peking Union Medical College and adhered to the tenets of the Declaration of Helsinki. Written informed consent was obtained from all patients.
Design and Anesthesia
Because the lower flap was too tight, the upper margin of the lower flap was lowered after adhesion release. The designed incision line was approximately 1 mm higher than the expected height of the supratarsal crease. If there was skin redundancy, an appropriate amount of skin was resected. The surgical technique is illustrated in Figures 1 through 3.
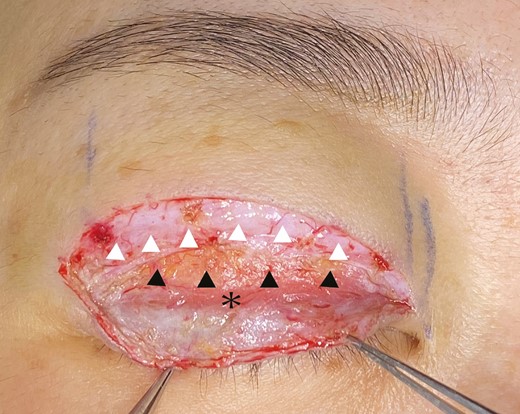
Lower flap dissection was completed, and a pretarsal tissue defect (black arrowhead) was evaluated (3 mm), indicating a severe static fold. The orbicularis oculi muscle of the upper flap (white arrowhead) was employed to prevent multiple folds. The remnant orbicularis oculi muscle of the lower flap is marked with an asterisk.
Lower Flap Dissection and PTD Evaluation
The skin incision was created as planned, and a strip of redundant skin was excised. For a static fold, the lower flap was under tension. The dissection was performed in a caudal direction between the skin and the pretarsal fascia until the remnant orbicularis oculi muscle was seen and no tension was observed on the lower flap. The PTD was defined as the area deficient of orbicularis oculi muscle in front of the tarsal plate after lower flap dissection (Figure 1). If the width of the PTD was over 2 mm, tissue transfer was performed to reconstruct the PTD, usually with a free ROOF graft or a pretarsal orbicularis oculi flap. If the width of the PTD was less than 2 mm (defined as a mild static fold), no tissue transfer was performed.
Upper Flap Dissection and Levator Manipulation
The orbital septum was opened laterally, and dual plane dissection was performed.6 All the scar adhesions were released across the whole incision, from lateral to medial. With the classic tarsal fixation technique, a considerable amount of preaponeurotic fat and orbital septum is removed, so there are scar adhesions in this plane to replace the orbital septum. The first plane was the dissection of scar tissue between the levator aponeurosis and the preaponeurotic fat. Afterwards, adhesions were released between the postorbicularis fascia and the septal layer (the second plane).
After dual plane dissection, the patient was evaluated in a sitting position. Most patients with a high fold and/or blepharoptosis were corrected successfully. However, in some patients, blepharoptosis was still evident. For residual ptosis correction, levator aponeurosis advancement was performed.
PTD Reconstruction
If the width of the PTD was no less than 2 mm, especially if there was a PTD below the upper margin of the lower flap, tissue transfer was performed. If more than 2 mm of redundant skin was resected above the old incision line, the pretarsal orbicularis oculi muscle flap was pulled down to reconstruct the PTD. If there was no sufficient pretarsal orbicularis oculi muscle, a piece of the lateral one-third of the ROOF was harvested. Care should be taken to reserve a thin layer of ROOF under the orbicularis oculi muscle to avoid multiple upper eyelid folds postoperatively. The ROOF graft was trimmed to fit the full length of the PTD. The width of the ROOF graft was approximately 1 mm more than the width of the PTD (Figure 2). Before suture fixation, it was ensured that the contour of the lower flap with the ROOF graft was flat. The ROOF graft or pretarsal orbicularis oculi muscle flap was then sutured with the remnant orbicularis oculi muscle of the lower flap with 8-0 nylon. In patients for whom the pretarsal orbicularis oculi muscle flap was not utilized for PTD reconstruction, the pretarsal orbicularis oculi muscle under the incised skin was employed for the upper flap to prevent multiple eyelid creases.
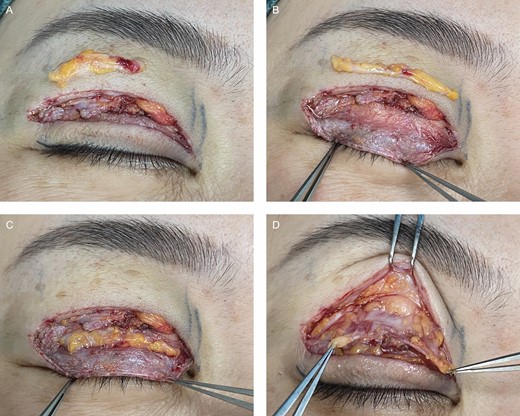
Retro-orbicularis oculus fat (ROOF) graft and orbital fat manipulation. (A) The lateral one-third of the ROOF was harvested for tissue transfer. Care was taken to reserve a thin layer of ROOF under the orbicularis oculi muscle to avoid multiple upper eyelid folds postoperatively. (B) The ROOF graft was trimmed to fit the full length of the pretarsal tissue defect. (C) The ROOF graft was sutured with the remnant orbicularis oculi muscle of the lower flap with 8-0 nylon. (D) The lower flap appeared flat after the ROOF graft. The orbital fat and posterior orbital fascia were pulled down to prevent multiple folds.
Double-Eyelid Crease Fixation
Before the suture for double-eyelid crease fixation, the PTD was first corrected. The first suture point was placed at the midpupillary point, and 7-0 nylon suture was started with horizontal stitching through the pretarsal levator aponeurosis. Then the suture was passed through the ROOF graft or the pretarsal orbicularis oculi muscle flap, followed by the dermis. The suture points on the pretarsal levator aponeurosis and the ROOF graft/pretarsal orbicularis oculi muscle flap were at the same height as the upper margin of the lower flap. Three to 6 sutures were required to create a stable supratarsal fold.
Adhesion Prevention and Skin Suture
Adhesion was prevented by pulling down the orbital fat together with orbital septum, and skin-orbital fat-skin–interrupted sutures were performed with 8-0 nylon. For many patients, the orbital septum had been destroyed in previous blepharoplasty procedures, and the posterior orbital fascia was pulled down instead of the orbital septum together with orbital fat.7 The posterior orbital fascia differs from the orbital septum; the orbital septum is relatively thick and white, whereas the posterior orbital fascia is a thin layer of transparent fascia tissue immediately surrounding the orbital fat. For patients with too much orbital fat resection in previous operations, the remaining orbital fat was not long enough to cover the pretarsal area. In this case, the orbital fat was divided meticulously to increase its length and could then be utilized for skin-orbital fat-skin–interrupted sutures without tension.
To prevent unwanted tissue adhesion higher than the planned upper eyelid crease, a 3M skin tape (St. Paul, MN) was applied on the skin above the incision line after skin closure with interrupted 7-0 nylon. The tape kept the skin taut and helped to avoid the unwanted adhesion between the skin above the incision line and the levator aponeurosis.6
Postoperative Care and Evaluation
Sutures and skin tape removal were performed on the fifth postoperative day. Patients in this study were followed-up from 6 to 24 months. The evaluation was based on patient feedback, including the height and symmetry of the upper eyelid folds, patient satisfaction, and scar formation; each item was graded as poor, fair, good, or excellent.8 The final result was determined by the lowest grade in the questionnaire. Postoperative complications, such as partial or complete loss of the double-eyelid line, a deep fold, multiple folds, an unnatural curve of the double fold, depressed or hypertrophic scar formation, a sunken upper eyelid, and asymmetric folds, were also recorded.
RESULTS
Between January 2015 and February 2018, 203 patients (187 women, 16 men) with static folds underwent revision surgery. The average age was 31 years (range, 25-61 years). There were 108 patients with high folds, 21 patients with blepharoptosis, 98 patients with mild static folds, and 105 patients with severe static folds. Among the 105 patients with severe static folds, ROOF grafts were performed in 67 patients, and orbicularis oculi muscle flaps were performed in 38 patients. For the patients with blepharoptosis, ptosis resolved in 16 patients after adhesion lysis, and only 5 patients underwent levator advancement. The patients were followed up for 6 to 36 months, with an average follow-up duration of 15.3 months. Typical cases are presented in Figures 4, 5 (Video, available online at www.aestheticsurgeryjournal.com, shows the front and quarter views of the patient in Figure 4 with dynamic folds 12 months after she received revisional blepharoplasty for her static folds).
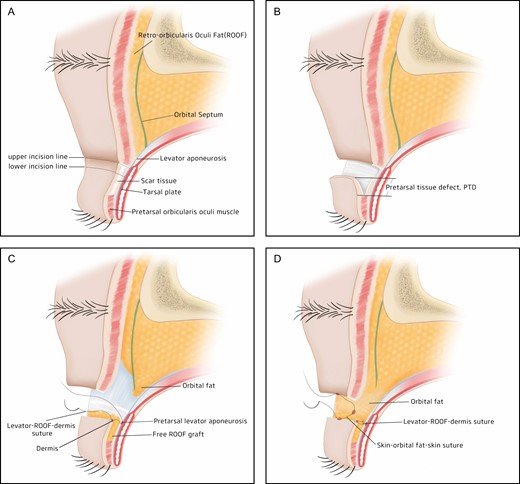
Surgical technique. (A) Preoperative design. The incision lines were drawn, and the skin between the 2 incision lines was resected. The lower flap was found to be deficient of orbicularis oculi muscle, only containing white scar tissue. Scar adhesion between the lower flap skin and tarsal plate was so tight that the lower flap was immobile during eyelid movement. (B) Lower flap dissection. The dissection was made in a caudal direction between the skin and the pretarsal fascia until the remnant orbicularis oculi muscle was seen and no tension was observed on the lower flap. The pretarsal tissue defect (PTD) was defined as the area deficient of orbicularis oculi muscle in front of the tarsal plate. It was a severe static fold with a PTD > 2 mm. (C) PTD reconstruction. Free retro-orbicularis oculus fat grafts were transferred to the lower flap with PTD, and 3 to 6 internal suture fixations were performed between the dermis and pretarsal levator aponeurosis to create a supratarsal crease. (D) Glide zone reconstruction. The orbital septum was pulled down together with orbital fat, and skin-orbital fat-skin–interrupted sutures were performed.

(A-C) This 37-year-old female patient before static fold revision blepharoplasty with eyes open, gazing downward, and closed. (D-F) Twelve months after revision blepharoplasty with eyes open, gazing downward, and closed.

(A-C) This 35-year-old female patient before static fold revision blepharoplasty with eyes open, gazing downward, and closed. (D, E, F) Twelve months after revision, blepharoplasty with eyes open, gazing downward, and closed.
Postoperative evaluation was administered by both the patients and the doctors. The patient evaluation was performed with questionnaires as previously reported.8 Of the 203 patients, 131 (64.5%) had excellent results, 45 (22.1%) had good results, 12 (5.9%) had fair results, and 15 (7.4%) had poor results. According to the postoperative evaluation, 176 (86.7%) patients were satisfied with the results. Postoperative complication was evaluated by the doctors. Complications included partial fold loss (n = 7, 3.4%), complete fold loss (n = 3, 1.5%), sunken upper eyelids (n = 5, 2.5%), multiple folds (n = 3, 1.5%), an unnatural curve of the double fold (n = 5, 2.5%), and asymmetric folds (n = 4, 2.0%).
DISCUSSION
Inborn double-eyelid folds appear when the levator aponeurosis inserts into the subcutaneous tissue9 or the intramuscular septum.10 The inborn fold is a natural and dynamic fold. However, with the classic tarsal fixation technique,5 it is important to dissect away a considerable amount of tissue lying between the lower skin flap and the tarsal plate. Afterwards, the skin edges were sutured with the tarsal plate to create the superior palpebral fold. Because a considerable amount of tissue (mainly pretarsal orbicularis oculi muscle) was dissected away between the lower skin flap and the tarsal plate, a PTD occurs. Therefore, a static fold is a common result. When the eyes were looking downward, pretarsal fullness and a depressed scar could be seen in the patients with a static fold.11 Therefore, in addition to routine pictures with eyes open and closed, a picture with the patient looking downward12 is necessary for a patient with a static fold.
Publications have reported the creation of dynamic double-eyelid folds that are similar with the movement of congenital folds, such as techniques with septoaponeurosis junctional thickening,2 levator aponeurosis,13 or septal extension.1 However, no studies to our knowledge have investigated secondary blepharoplasty for static fold correction.
To the best of our knowledge, this is the first study detailing the conversion of a static fold into a dynamic fold. Adhesion release and PTD reconstruction of the lower flap are 2 key elements. In this study, we devised PTDs as a new concept to imply the severity of the static fold. After releasing the adhesion of the lower flap, the width of the PTD is evaluated. The severity of a static fold can only be determined intraoperatively. A mild static fold is defined as PTD < 2 mm. A PTD ≥ 2 mm is defined as a severe static fold, which requires tissue transfer. Without appropriate tissue transfer, there will be scar adhesion between the skin and pretarsal tissue on the lower flap, and the static fold recurs.
In our series, pretarsal tissue transfer was mainly performed with ROOF grafts. This is because in secondary blepharoplasty, usually not too much skin redundancy exists above the old incision line, so orbicularis oculi muscle is not sufficient for tissue transfer. Another reason is that if the excised skin is below the old incision line, there is too much fibrotic scar tissue and not so much orbicularis oculi muscle under the skin. For tissue transfer, the ROOF graft is better than fibrotic scar tissue.14 Unipedicled and bipedicled ROOF flaps were also tried for PTD reconstruction. Although a pedicled ROOF flap had the advantage of better blood supply, the existence of the pedicle (medially or laterally) caused a local bulge and sometimes an additional crease above the local bulge, which had a negative impact on the result. We therefore abandoned the pedicled ROOF because of those shortcomings. A management algorithm for the static fold based on its severity is also proposed in Table 1.
| Severity of static fold . | Width of PTD (mm) . | Width of skin excision (mm) . | PTD reconstruction . |
|---|---|---|---|
| Mild | <2 | Any | No |
| Severe | ≥2 | >2 | ROOF/OOM |
| ≤2 | ROOF |
| Severity of static fold . | Width of PTD (mm) . | Width of skin excision (mm) . | PTD reconstruction . |
|---|---|---|---|
| Mild | <2 | Any | No |
| Severe | ≥2 | >2 | ROOF/OOM |
| ≤2 | ROOF |
OOM, orbicularis oculi muscle; PTD, pretarsal tissue defect; ROOF, retro-orbicularis oculus fat.
| Severity of static fold . | Width of PTD (mm) . | Width of skin excision (mm) . | PTD reconstruction . |
|---|---|---|---|
| Mild | <2 | Any | No |
| Severe | ≥2 | >2 | ROOF/OOM |
| ≤2 | ROOF |
| Severity of static fold . | Width of PTD (mm) . | Width of skin excision (mm) . | PTD reconstruction . |
|---|---|---|---|
| Mild | <2 | Any | No |
| Severe | ≥2 | >2 | ROOF/OOM |
| ≤2 | ROOF |
OOM, orbicularis oculi muscle; PTD, pretarsal tissue defect; ROOF, retro-orbicularis oculus fat.
In a dynamic fold, the glide zone is very important and acts like a frictionless lubricating layer that allows the posterior layer to glide upward.15 During our operation, the posterior orbital fascia/orbital septum is pulled along with the orbital fat not only to prevent multiple folds but also to reconstruct the glide zone.
In a person with a congenital double eyelid, because there is orbicularis oculi muscle and no scar adhesion in the lower skin flap, the lower flap is mobile during eyelid movement. However, in a patient with a static fold, because of the tight scar adhesion between the lower skin flap and the tarsal plate, the lower flap becomes an immobile zone. PTD reconstruction can prevent direct scar adhesion between the skin and tarsal plate, facilitating the mobility of the lower flap. With our technique, the lower skin flap is converted from an immobile zone into a mobile zone, which looks natural and dynamic during eyelid movement. Preoperatively, many patients reported symptoms such as tightness and dry eyes. After operation, those symptoms resolve because the tight and high scar adhesion of the lower flap has been released.
In most patients of our series, ptosis resolved with meticulous dissection or freeing of scar. As described previously,6 a high fold induces a greater weight load on the levator muscle compared with a low fold. Therefore, high double-eyelid folds can induce blepharoptosis without any intrinsic effect from the levator muscle. Converting a high fold to a low fold reduces the weight load on the levator aponeurosis. This in turn can resolve iatrogenic ptosis occurring from high double-eyelid folds that burden the eye-elevating mechanism in patients without preexisting ptosis.6
Because the dermis has been fixed with the levator aponeurosis at a lower position, less upper lid skin is involved in the supratarsal crease during eye opening, and the skin between the brow and the upper eyelid margin becomes thinner after revision surgery. As a byproduct of our technique, the brow lid distance is also increased, which makes the patient look younger.16
Our technique has limitations. First, for severe static fold patients, if there is no sufficient ROOF or orbicularis oculi muscle, it is very difficult to correct the PTD. Furthermore, several patients developed sunken upper eyelids postoperatively. For patients with sunken upper eyelids, free fat grafts or dermofat grafts should be performed. Second, several patients developed fold loss. This is because after PTD reconstruction, there was ROOF graft or orbicularis oculi muscle tissue between the skin and tarsal plate of the lower flap, which hindered double-eyelid formation. If the suture creating the supratarsal crease was loosened, there was risk of fold loss. Suture fixation was performed again for those patients.
CONCLUSION
To convert a static fold to a dynamic fold, we devised a technique that releases the adhesion and reconstructs the PTDs with an orbicularis oculi muscle or ROOF graft for the lower flap. A management algorithm dependent on the severity of a static fold was also developed.
Acknowledgments
Dr Huang and Dr Feng made an equal contribution to this work as co-first authors.
Disclosures
The authors declared no potential conflicts of interest with respect to the research, authorship, and publication of this article.
Funding
The authors received no financial support for the research, authorship, and publication of this article.
REFERENCES



