-
PDF
- Split View
-
Views
-
Cite
Cite
In Chang Cho, Beom-Jun Kim, Hi-Jin You, Woo Hyun Tark, Surgical Correction of Upper Eyelid Ectropion Presenting Dry Eye Symptoms, Aesthetic Surgery Journal, Volume 41, Issue 1, January 2021, Pages NP1–NP9, https://doi.org/10.1093/asj/sjaa143
Close - Share Icon Share
Abstract
Upper eyelid ectropion occurs as a post-blepharoplasty complication or involution change, and it causes dry eye symptoms that cannot be resolved with conservative management.
The aim of this study is to describe the authors’ surgical technique of anatomical correction of upper eyelid ectropion, including tarsal scoring incision.
The technique involves the following 4 steps: (1) adhesiolysis at the preaponeurotic layer; (2) undermining and redraping of the pretarsal flap in a pretarsal plane; (3) optional, partial thickness tarsal scoring incision over the central two-thirds; and (4) downward repositioning of the pretarsal flap and lower fixation to the tarsus. Outcomes were assessed based on the position of eyelid margin and the improvement of the dry eye symptoms.
A retrospective review of 54 cases of patients who underwent ectropion correction, including tarsal scoring incision, was performed. The eyelid margin was well positioned in 51 patients (94.4%). Of the 32 patients involved in the study assessed with the 7-point Patient Global Impression of Improvement, 29 (90.6%) reported the resolution of dry eye symptoms. Furthermore, in the 22 patients assessed with the Ocular Surface Disease Index, the mean score significantly decreased from 43.2 ± 24.1 before surgery to 29.8 ± 23.3 (P = 0.006) after surgery.
The combination of partial-thickness tarsal plate scoring and lower flap redraping surgical techniques resolved the upper eyelid ectropion, reducing the dry eye symptoms.
Ectropion is an outward turning (eversion) of the eyelid margin. It primarily involves the lower lid, but an upper lid eversion can also occur. Unlike lower eyelid ectropion, which is widely recognized and well described, upper eyelid ectropion is much less studied in terms of etiology and treatment.1 Patients with ectropion often experience symptoms of chronic conjunctivitis and dry eye due to tarsal conjunctiva exposure and inadequate lubrication. There are 4 main types of ectropion: involutional, cicatrical, paralytic, and mechanical. Involutional ectropion is caused by an increased laxity of the eyelid during aging. Cicatrical ectropion is caused by shortening of the anterior lamella, which is comprised of the skin and orbicularis muscle. Paralytic ectropion is caused by a decreased orbicularis muscle tone supporting the eyelid following nerve damage. Mechanical ectropion can develop when a tumor displaces the eyelid margin.2
Upper eyelid ectropion is similar to the lower eyelid counterpart,3,4 although upper lid ectropion is far less common, usually occurring as the result of senile changes or following a blepharoplasty.5,6 Lipham et al suggested a mechanism for senile ectropion development. This outward curvature or folding of the upper eyelid tarsus is due to the atrophy of Riolan’s muscle. The muscle is located near the orifices of the Meibomian glands, where it keeps the orifices patent and maintains the eyelid and globe in close vicinity.7 Ischemic atrophy of this muscle over time leads to the involutional ectropion of the eyelid, which in turn can cause dry eye symptoms.8-11 In addition to the involutional cause of upper eyelid ectropion, some patients present a postsurgical cause. Most cases of upper blepharoplasty in Asian patients are for an upper eyelid crease. To make this double fold, the pretarsal composite flap should be pulled upward. However, excessive pulling may result in a varying degree of ectropion or lid margin eversion. Kim et al12 described the eversion of the eyelid margin and eyelashes as marginal ectropion. Although the eversion of the eyelid margin is not as prominent as in cases of classical cicatricial ectropion and the eyelid itself is positioned normally, marginal ectropion results in upturned eyelashes and gray line exposure. Therefore, it may cause not only a “sausage-like” appearance but also dry eye symptoms in some cases.
Dry eye is caused by decreased tear production and/or increased tear film evaporation. The tear film is composed of lipids, proteins, and mucins located on the hydrophobic surface of the epithelium. The outer shell of the tear film, the lipid layer, is composed of a combination of polar and nonpolar lipids secreted from the Meibomian glands. These glands are embedded in the tarsal plates with the ductal openings usually at the lid margin just anterior to the mucocutaneous junction.4 One of the most common causes of dry eye symptoms is decreased production of the lipid layer from the Meibomian gland, resulting in the rapid evaporation of the tear film.13
The upper eyelid ectropion frequently causes dry eye symptoms among patients. The dry eye symptoms are due to the eversion of the lid margin away from the ocular surface, thus resulting in lipid deficiency. Histological examination of an eyelid with ectropion showed subacute inflammation and epithelialization around the tarsal conjunctiva, which could induce Meibomian gland dysfunction.8,14 Hyperkeratinization of the ductal opening is generally considered the main mechanism that causes Meibomian gland dysfunction.15 Typical symptoms include dryness, burning sensation, and a sandy or gritty sensation aggravated during activities that reduce blinking, such as watching television, driving, and computer use.16
Periodic massage and activation of the Meibomian gland together with the administration of heat to the eyelids are the suggested treatment modalities for managing dry eye caused by Meibomian gland dysfunction.17,18 However, even regular and repeated care will not resolve the symptoms in patients who have an anatomical abnormality of the eyelids that causes the dysfunction of the glands.19
In this article, we describe the strategies for the anatomical correction of upper eyelid ectropion and the technique of tarsal scoring incision with which we have obtained consistently satisfactory results and few complications.
METHODS
A retrospective review of the cases of consecutive patients who underwent upper eyelid ectropion correction was performed from December 2007 to April 2018. The study protocol was approved by the institutional review board of Korea University Ansan Hospital (IRB No. 2019AS0190). Data including patient demographics, cause of ectropion, presenting symptoms, other ocular abnormalities, and length of follow-up were collected. Ectropion with severe symblepharon or severe ocular surface disease were excluded.
Surgical Technique
All surgical procedures were performed with intravenous sedation and local infiltrative anesthesia. The surgical steps employed to correct upper eyelid ectropion were as follows.
Step 1: Adhesiolysis
After marking the previous blepharoplasty scar or the desired upper eyelid crease line, local anesthesia was administered by infiltration of 2% lidocaine with 1:100,000 epinephrine. The incision was made with a no. 15 blade, and a small strip of skin was excised. The underlying scar tissue was then incised with scissors, and the adhesion between the levator aponeurosis and the overlying soft tissue was released at the preaponeurotic layer (Figure 1A,B).
Intraoperative view of post-blepharoplasty ectropion correction in this 74-year-old woman. (A, B) Adhesiolysis at the preaponeurotic layer. (C, D) Undermining and redraping of the pretarsal flap in a pretarsal plane. (E, F) Optional, partial thickness tarsal scoring incision over the central two-thirds. (G, H) Downward repositioning of the pretarsal flap and lower fixation to the tarsus.
Step 2: Undermining and Redraping the Pretarsal Flap
After adhesiolysis, the inferior skin and pretarsal orbicularis muscle flap were dissected in a pretarsal plane. Once adequately undermined, the composite musculocutaneous pretarsal flap was redraped at the desired lid margin position, which was lower than the preoperative lid margin position (Figure 1C,D).
Step 3: Tarsal Scoring
If the ectropion was not resolved after steps 1 and 2, the pretarsal flap was dissected in the pretarsal plane toward the inferior edge of the tarsal plate until the eyelashes were exposed. Then, scoring of the tarsal plate was performed with a number 15 blade. The incision was made 2 mm above and in parallel with the inferior edge of the tarsal plate, extending over the central two-thirds. The scoring depth was about two-thirds of the thickness of the tarsus, with the incision tilted approximately 45° caudally to the inferior border of the palpebral conjunctiva. Care was taken to not truncate the eyelash follicles. The lid margin was allowed to naturally lie in contact with the ocular surface (Figure 1E,F; Video).
Step 4: Fixation of the Pretarsal Flap to the Tarsal Plate
Buried interrupted 7-0 polydioxanone sutures between the inferior pretarsal flap and the tarsal plate were placed. The pretarsal flap was fixed lower than its original position. The downward repositioning of the inferior pretarsal flap can result in multiple fold formation due to an insufficient amount of soft tissue of the superior flap. In that case, an additional procedure was performed to prevent multiple fold formation as follows. The orbital septum and preaponeurotic fat was advanced down to the tarsal plate, forming an interpositional gliding layer between the orbicularis oculi muscle and the orbital septum.20 A skin incision was repaired with a continuous running suture utilizing 7-0 nylon (Figure 1G,H).
Evaluation
Outcomes were assessed on the basis of the extent of the eyelid margin inversion, the direction of the lashes, cosmesis, and postoperative complications.
Dry eye symptoms were assessed with either the 7-point Patient Global Impression of Improvement (PGI-I) scale or the Ocular Surface Disease Index (OSDI; Allergan Inc, Irvine, CA; Appendix A). From 2007 to 2016, patients were asked to rate the postoperative improvement of dry eye symptoms utilizing the PGI-I scale (1: very much better, 2: much better, 3: a little better, 4: no change, 5: a little worse, 6: much worse, 7: very much worse). The surgeon asked this question to the patient directly at the follow-up visits. From 2017 to April 2018, a questionnaire was conducted for dry eye symptom assessment. The survey paper was distributed by a nurse when the patients visited the clinic, and they answered the questions under their real name. The questionnaire is composed of 12 questions to evaluate the frequency of symptoms over the preceding week. The OSDI score is calculated with the following formula: OSDI = ([sum of scores for all questions answered × 100] / [total number of questions answered × 4]). The score ranges from 0 to 100. On the basis of the score, the patient’s symptoms can be categorized as normal (0-12), mild dry eye (13-22), moderate dry eye (23-32), or severe dry eye (33-100). The OSDI scores at the time of diagnosis (baseline) and follow-up visits were collected and analyzed. The OSDI score at the last follow-up was utilized for comparison with the baseline.
Statistical Analysis
Statistical analysis was performed utilizing the IBM SPSS Version 24 software (IBM Corp., Armonk, NY). Statistical significance was defined as P < 0.05.
RESULTS
A total of 54 patients (53 female and 1 male) were treated utilizing the technique described above. The mean age of the patients was 47.0 ± 13.1 years (range, 23-78 years). The ectropion causes included a prior upper blepharoplasty (48 patients) and senile changes (6 patients). Fifty-three patients (98.1%) complained of dry eye symptoms. Forty-eight patients who had undergone upper blepharoplasty presented with various degrees of high folds with pretarsal fullness. Severe asymmetric folds were observed in 3 patients. None of the patients had a history of lower blepharoplasty or ocular comorbidities such as lagophthalmos. The tarsal scoring (step 3 in the procedure) was performed in 28 patients (52%). The mean follow-up was 6 months, and the follow-up period ranged from 2 months to 6 years.
Of the 54 patients, 51 (94.4%) showed successful postoperative results as defined by lashes normally directed downward and a well-positioned eyelid margin without gray line exposure (Figures 2 and 3). The cosmetic results in all patients were good, and none of the patients were unsatisfied with the final appearance. Subtle inversion of the eyelid margin (marginal entropion) without trichiasis was observed in 3 of the 54 patients (5.6%). None of the patients experienced significant complications such as ptosis or blepharitis.
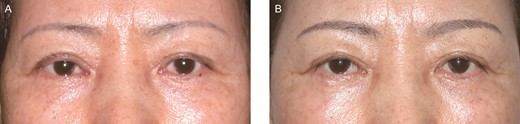
(A) Preoperative view of a dry eye case with involutional ectropion in this 66-year-old female patient. (B) Postoperative view at 1 year after tarsal scoring incision. The ectropion was successfully corrected, and dry eye symptoms were also resolved.
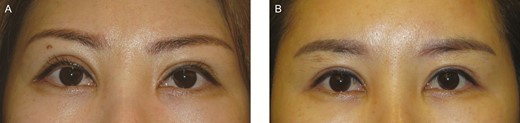
(A) Preoperative view of this 39-year-old woman who complained of asymmetric high fold with dry eye symptoms after previous upper blepharoplasty. The high fold is usually combined with a deep fold because of excessive upward pulling of the pretarsal composite flap. This deep fold may result in ectropion and eyelash eversion. The gray line is observed below the eyeline tattoo line. (B) Postoperative view 1 year after the tarsal scoring procedure. The everted eyelid margin had turned inward, and the gray line had returned to its normal position such that the tattoo line is placed on the lowest eyelid margin. Accordingly, the everted and upturned eyelashes were directed downward. Downward-directed upper eyelid lashes are normal in many Asian patients but are often considered abnormal in Caucasian patients.
We assessed 32 patients with the PGI-I scale and 22 patients with the OSDI scores for dry eye symptoms (Table 1). According to the PGI-I scale, 2 patients reported their symptoms to be very much better (6.3%); 20 patients, much better (62.5%); 7 patients, a little better (21.9%); 2 patients, no change (6.3%); and 1 patient, a little worse (3.1%; Figure 4). We considered the first 3 results in the scale (very much better, much better, and a little better) as acceptable results, comprising 90.6% of the assessed patients.
| . | PGI-I scale group (%) . | OSDI group (%) . |
|---|---|---|
| No. of patients | 32 | 22 |
| Age, y | ||
| Mean ± SD | 43.7 ± 14.0 | 51.5 ± 10.6 |
| Range | 23–76 | 33–78 |
| Sex | ||
| Female | 32 (100) | 21 (95) |
| Male | 0 (0) | 1 (5) |
| Cause of ectropion | ||
| Blepharoplasty | 29 (91) | 19 (86) |
| Aging | 3 (9) | 3 (14) |
| Tarsal scoring | ||
| Not performed | 10 (31) | 16 (73) |
| Performed | 22 (69) | 6 (27) |
| . | PGI-I scale group (%) . | OSDI group (%) . |
|---|---|---|
| No. of patients | 32 | 22 |
| Age, y | ||
| Mean ± SD | 43.7 ± 14.0 | 51.5 ± 10.6 |
| Range | 23–76 | 33–78 |
| Sex | ||
| Female | 32 (100) | 21 (95) |
| Male | 0 (0) | 1 (5) |
| Cause of ectropion | ||
| Blepharoplasty | 29 (91) | 19 (86) |
| Aging | 3 (9) | 3 (14) |
| Tarsal scoring | ||
| Not performed | 10 (31) | 16 (73) |
| Performed | 22 (69) | 6 (27) |
OSDI, Ocular Surface Disease Index; PGI-I, Patient Global Impression of Improvement; SD, standard deviation.
| . | PGI-I scale group (%) . | OSDI group (%) . |
|---|---|---|
| No. of patients | 32 | 22 |
| Age, y | ||
| Mean ± SD | 43.7 ± 14.0 | 51.5 ± 10.6 |
| Range | 23–76 | 33–78 |
| Sex | ||
| Female | 32 (100) | 21 (95) |
| Male | 0 (0) | 1 (5) |
| Cause of ectropion | ||
| Blepharoplasty | 29 (91) | 19 (86) |
| Aging | 3 (9) | 3 (14) |
| Tarsal scoring | ||
| Not performed | 10 (31) | 16 (73) |
| Performed | 22 (69) | 6 (27) |
| . | PGI-I scale group (%) . | OSDI group (%) . |
|---|---|---|
| No. of patients | 32 | 22 |
| Age, y | ||
| Mean ± SD | 43.7 ± 14.0 | 51.5 ± 10.6 |
| Range | 23–76 | 33–78 |
| Sex | ||
| Female | 32 (100) | 21 (95) |
| Male | 0 (0) | 1 (5) |
| Cause of ectropion | ||
| Blepharoplasty | 29 (91) | 19 (86) |
| Aging | 3 (9) | 3 (14) |
| Tarsal scoring | ||
| Not performed | 10 (31) | 16 (73) |
| Performed | 22 (69) | 6 (27) |
OSDI, Ocular Surface Disease Index; PGI-I, Patient Global Impression of Improvement; SD, standard deviation.

Patient Global Impression of Improvement scale distribution. Acceptable results (very much better, much better, and a little better) were achieved in 29 (90.6%) of the assessed patients.
In the OSDI group, the mean OSDI score changed significantly from 43.2 ± 24.1 at baseline to 29.8 ± 23.3 at the final visit (P = 0.006 by Wilcoxon signed rank test; Figure 5). The mean difference in OSDI score, calculated as the score at final follow-up minus the baseline score, was 13.4 ± 23.7. The mean difference was significantly higher in the patients who underwent tarsal scoring than in those who underwent just redraping (15.5 ± 18.5 vs. 12.7 ± 25.9; P < 0.05 by Mann Whitney U test).
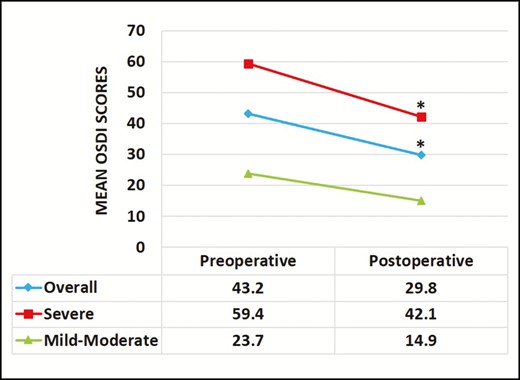
Changes in mean Ocular Surface Disease Index (ODSI) score. The mean Ocular Surface Disease Index score significantly decreased from 43.2 ± 24.1 before the surgery to 29.8 ± 23.3 after the surgery. A significant decrease in mean postoperative Ocular Surface Disease Index score was observed in the patients with severe dry eyes (n = 13; preoperative Ocular Surface Disease Index ≥ 33) and not in the mild to moderate category (n = 7; preoperative Ocular Surface Disease Index 13-33; *P < 0.05 by Wilcoxon signed rank test).
The mean preoperative score in the 13 patients with severe dry eye (OSDI ≥ 33) was 59.4 ± 16.6, which improved significantly after surgery to 42.1 ± 21.4 (P = 0.034). In the 7 patients with mild to moderate dry eye (OSDI = 13-33), the mean score decreased from 23.7 ± 3.6 to 14.9 ± 11.8, but the change was not significant (P = 0.089; Figure 5). We observed changes in the number of patients for each category preoperatively and postoperatively. Although 13 patients were included in the severe category before the surgery, the number of patients decreased to 10 after the surgery. Conversely, the patients in the normal category increased from 2 to 6 after the surgery. Although the overall postoperative severity was lower, as shown in Figure 6, the difference was not significant (P > 0.05 by linear-by-linear association chi-square test).
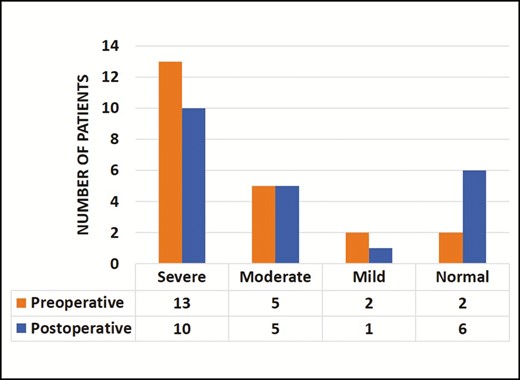
Change in the number of patients in each Ocular Surface Disease Index category. Although the overall postoperative severity based on the Ocular Surface Disease Index score tends to decrease, the difference was not significant (P > 0.05 by linear-by-linear association chi-square test).
DISCUSSION
We hypothesized that the cause of a part of the overall dry eye cases could be the upper eyelid ectropion. Anterior shifting of the mucocutaneous junction strongly correlates with eyelid ectropion; therefore, a long-standing exposure of the mucocutaneous junction induces the ductal hyperkeratinization, which is the major pathogenic mechanism of Meibomian gland dysfunction.
Several histopathological studies of eyelids with involutional ectropion demonstrated that subacute inflammation and epidermalization of the tarsal conjunctiva was a common event.8,14,21 Previous studies on Marx’s line, currently known as the mucocutaneous junction, suggested a relationship between the Meibomian gland dysfunction and location of the line. Yamaguchi et al showed that the location of Marx’s line was associated with the functionality of the Meibomian gland; that is, a line on the ocular side of the Meibomian gland orifices indicated normal function, whereas that on the cutaneous side indicated a dysfunction.22 Furthermore, Norn showed that with aging, Marx’s line became irregular and shifted anteriorly toward the cutaneous side of the Meibomian ductal openings.23
In addition to the involutional cause, upper eyelid ectropion frequently results from upper eyelid surgeries such as blepharoplasty for aging eyelids, blepharoptosis correction, and double fold formation in Asian patients.24 Excessive upward pulling of the pretarsal composite flap may result in anterior shifting of the mucocutaneous junction associated with the eversion of the eyelid margin. Dry eye symptoms following postsurgical ectropion is a common complication, but if it is not recognized and diagnosed it can negatively affect the functional surgical outcome, resulting in patients’ dissatisfaction.6,9,10,16,19,24
Unlike the lower eyelid ectropion, the treatment for upper eyelid ectropion is much less described in the literature.1 In the present study, we describe a novel 4-step surgical protocol for the treatment of upper eyelid ectropion. The first step, with the simple release of adhesions in the tarsal plate, levator aponeurosis, and skin, allows the everted eyelash to turn down and results in shallowness of the upper eyelid crease. In the second step, upward pulling tension is released. Most ectropion cases are solved in the first 2 steps. However, if it is not solved, an additional step is needed before the fixation of the pretarsal flap to the appropriate level as follows: anchoring the tarsus, dermis, and septum at the right level keeps the pretarsal flap taut and flat, preventing lash eversion (Figure 7).

If the ectropion was not resolved after adhesiolysis, undermining, and redraping, a tarsal scoring incision is needed before the lower fixation of the pretarsal flap to the appropriate level. Indications for tarsal scoring are as follows: (1) involutional ectropion; (2) postsurgical ectropion without skin stretching; and (3) few cases of severe congenital ectropion.
Thus, we introduced a novel step in which we performed a tarsal scoring procedure. It is a significant challenge to surgeons if patients do not respond to the first 2 steps described earlier. Therefore, a surgical procedure that can effectively address both upper eyelid ectropion and dry eye symptom is needed. The upper tarsal plate is a thick, elongated, semi-lunar plate of dense connective tissue abutting the eyelid margin. Manipulation of the upper tarsal plate allows the lid margin to curve inward. This is achieved through a single partial-thickness scoring incision of the tarsus over the central two-thirds, at the inferior edge near the hair follicles of the eyelash. The medial and lateral aspects of the tarsal plate did not usually require correction. After this procedure, dekeratinization of the eyelid margin occurs and might relieve the Meibomian gland obstruction. The loss of the upper eyelid crease and overcorrection with the resultant upper lid entropion are possible complications. To prevent the shallowing of the upper eyelid crease, a precise and firm refixation of the eyelid skin onto the tarsus at the new position should be performed. Although we had an initial concern that the scoring of the tarsus may transect the Meibomian gland ductal system, the satisfactory results suggested that this was a clinically safe procedure.
We have performed the surgical correction of the upper eyelid ectropion since 2007. The results of the PGI-I group showed that the surgical technique did improve the dry eye symptoms, because 29 patients (90.6%) answered that their symptoms improved after surgery. Starting from 2017, we switched to the OSDI scoring to have more objective data as follows: the 12-item OSDI questionnaire contains 3 ocular symptom questions, 6 vision-related function questions, and 3 environmental trigger questions. Each question score ranges from 0 (“none of the time”) to 4 (“all of the time”). Although fewer patients subjected to the tarsal scoring step were included in the OSDI group than in the PSI-I group (69% vs 27%), we observed a significant decrease in the mean postoperative OSDI scores, especially in patients in the severe category. The overall severity based on this score also tends to decrease. In addition to the standard 12 questions of the OSDI, we asked 2 more questions about the utilization of eye drops: whether they utilized them and how often they utilized them each day. Most patients who answered that they utilized them answered that the frequency of postoperative use had decreased. These results demonstrate that the ectropion correction surgery is an effective method to resolve dry eye symptoms. Although the mean OSDI difference was significantly higher in the tarsal scoring subgroup than in the redraping only subgroup, the comparison is not appropriate because the tarsal scoring step is not an independent procedure but is a part of the overall surgical process.
Dry eye symptom is a common but often underdiagnosed problem following aesthetic blepharoplasties.6,9,10,16 Therefore, it is essential to evaluate preoperatively if the patient experienced dry eye symptoms so that an appropriate surgical technique should be performed to correct or prevent the aggravation of the dry eye.25,26 In addition to the postsurgical cause for upper eyelid ectropion, some patients present an involutional cause. We strongly recommend a careful patient examination to rule out ectropion and dry eye before performing ptosis correction, because involutional upper eyelid ectropion is often found in combination with involutional ptosis; both are caused by the rarefaction of the upper eyelid. A ptosis correction can worsen the degree of ectropion. As a result, subclinical dry eye could become clinically symptomatic, and dry eye symptoms may be aggravated after the surgery.
Despite the promising results of this technique, the retrospective nature of the study limited the assessment of dry eye. The benefit of the procedure is only considered by symptomatic improvement of dry eye without clinical examination. The length of follow-up was another limitation of this retrospective study. Even though some of our patients were followed for up >1 year, 2 months was relatively short to evaluate the surgical outcome. Variable duration of follow-up also limits the extent of comparison among patients. However, we found that the immediate postoperative position of the eyelid margin did not change much over time. The position of the eyelid margin remained unchanged from 1 month after surgery when acute swelling disappeared. It is thought that the scored tarsal plate is supported by the pretarsal flap, and the complex is well maintained during scar maturation. A large prospective study with a longer follow-up duration and further research investigating the anatomical and functional change of the tarsus and Meibomian gland after the scoring procedure are needed.
CONCLUSIONS
Upper eyelid ectropion associated with dry eye symptoms is a common but poorly recognized problem and is therefore an often undiagnosed condition in patients following aesthetic blepharoplasties or involutional change. The strategies for the correction of upper eyelid ectropion, including tarsal plate scoring and the lower redraping technique, provide simple but effective solutions for this problem, with low rates of complication and recurrence.
Disclosures
The authors declared no potential conflicts of interest with respect to the research, authorship, and publication of this article.
Funding
The authors received no financial support for the research, authorship, and publication of this article.
References
Author notes
Dr Cho is a plastic surgeon in private practice in Seoul, Republic of Korea.
Dr Tark is a plastic surgeon in private practice in Seoul, Republic of Korea.





