-
PDF
- Split View
-
Views
-
Cite
Cite
Christine E Wamsley, John Hoopman, Jeffrey M Kenkel, The Role of the Laser Safety Officer and Laser Safety Programs in Clinical Practice, Aesthetic Surgery Journal, Volume 41, Issue 11, November 2021, Pages NP1550–NP1554, https://doi.org/10.1093/asj/sjaa239
Close - Share Icon Share
Abstract
Recent advancements in laser technology have led to its expanded utilization in smaller clinical settings and medical spas, particularly for facial rejuvenation and the treatment of other aesthetic concerns. Despite the increasing popularity of this technology, discussion of laser safety programs has remained limited, mostly to operating rooms at larger clinical institutions. Although smaller facilities do not operate at the same capacity as a large hospital or medical center, the requirements for utilizing a laser are no less stringent. Employers must comply with local and federal regulations, the Occupational Safety and Health Administration (OSHA) General Duty Clause, American National Standards Institute (ANSI) standards, and professional recommended practices applicable to their business. Although the laser safety officer (LSO) is often a full-time position within larger facilities, smaller clinical settings and medical spas may be limited in staff number. It is important, therefore, that clinical practices establish laser policies and procedures with consideration of their individual needs and capabilities. In this paper, we will define a laser safety program, highlight basic requirements needed to establish this program, and outline the specific responsibilities of the LSO. To ensure that safe laser practices are being conducted at the healthcare facility, it is imperative that small business owners are aware of these regulations and standards in place for the operation of laser systems.
According to the 2018 Plastic Surgery Statistics Report released by The Aesthetic Society, 37,849 full-field ablative laser skin-resurfacing procedures; 38,550 micro-ablative fractional resurfacing procedures; 135,619 intense pulsed light photorejuvenation procedures; and 118,592 laser or pulsed light hair removal procedures were performed in the previous year alone.1 Due to the increasing popularity of lasers not only within plastic surgery but across most specialties, safety education and injury prevention are important now more than ever.
The ANSI is a private organization that develops guidelines for the safe utilization of lasers in both industry and medicine.2 ANSI Z136.3, Safe Use of Lasers in Health Care, focuses on the proper operation of lasers serving as medical devices.3,4 Compliance with these recommendations is voluntary. However, they are regarded as standard of care for manufacturers, consumers, and practitioners in the United States.5 Although OSHA defers to the laser safety standards outlined by ANSI, all businesses are subject to the General Duty Clause. This act requires employers to protect employees to the best of their ability by furnishing a workplace free from recognized hazards that may cause serious injury or death. Employers must, therefore, comply with occupational safety and health standards applicable to their business.6
In reviewing the current literature, very little information has been published on laser safety programs and, specifically, the responsibilities of a LSO. The discussion of laser safety programs has remained limited to the operating room, not the clinical setting or medical spa, where minimally invasive laser procedures are commonly performed and at times with minimal physician oversight. Additionally, there are no publications outlining the role of a LSO within this clinical setting. It is imperative that practices utilizing lasers and light-based devices establish a knowledgeable and competent LSO.
ANSI Z136.3 acknowledges that laser systems may be utilized in a variety of non-hospital environments, included private practices, dental offices, salons, and medical spas. These smaller settings simply do not operate at the same capacity as large hospitals or academic institutions. This paper will provide the broad scope of a laser safety program, as outlined in ANSI Z136.3. However, these guidelines must be adjusted to fit the capabilities of each clinic. For example, within a larger facility, the LSO is often a full-time position. Within smaller clinics and private practices, the business owner or physician often assumes the administrative responsibilities of the LSO or must ensure that a qualified person is assigned to that role. Existing perioperative personnel may need to be cross-trained, because smaller clinics and medical spas often operate with a small staff and simply cannot hire the additional personnel mentioned in this paper and the ANSI standard. Regardless, the assigned LSO must be knowledgeable of local and federal regulations, OSHA General Duty Clause, ANSI standards, and professional recommended practices. They must oversee maintenance and policies required for safe laser operation and perform the duties outlined in the following sections of this paper. Additionally, this paper is not intended to serve as a standard of care guidelines, and individual state regulations will also contribute in dictating the approach clinics and medical spas must take in developing laser safety protocols and policies. Please refer to the Appendix for contact information for each state’s regulatory agency, which is current as of July 10, 2020.7 Rockwell Laser Industries regularly updates this reference. For the most recent list of state laser safety contacts, please refer to their resource online (https://www.rli.com/resources/statecontacts.aspx).
What Is a Laser Safety Program?
ANSI Z136.3 states that “the health care facility (HCF) shall establish and maintain an adequate safety program for the control of laser hazards.” 3 A laser safety program is required for the usage and ownership of all types of lasers, including those that are rented or leased.8 The program should delegate responsibility for the supervision, evaluation, and control of all laser systems within the facility. The program sets forth administrative controls and safety guidelines for all activities involving laser utilization.9 This includes authorization procedures, education, and training for all healthcare personnel working within the laser treatment area. The program also manages reports of any accidents and implements policies to prevent recurrence of any incidents. Additionally, the laser safety program performs routine audits to ensure the proper protective measures are in place. Ultimately, the laser safety program outlines policies and procedures to protect both clinical personnel and patients and monitors that healthcare personnel at the healthcare facility are complying with these standards.3
An important component of a laser safety program is the laser safety committee. This multi-disciplinary group should consist of the LSO and other individuals involved in the operation of the laser systems, including, but not limited to physicians, laser specialists, biomedical engineers, staff education managers, administrators and office staff, anesthesia, surgical technologists, risk management, and representatives from quality assurance.3,9 Smaller practices and medical spas may not interact with all of the aforementioned personnel. Therefore, the exact composition and size of a laser committee must be individualized for each clinic. At the smallest level, this committee can and will consist of the LSO and managing physician or practice owner.
The committee serves to answer questions and concerns related to laser use, assess the technology and potential hazards, monitor compliance with operational policies and procedures, review safety violations or incidents, and provide educational requirements and credentialing for personnel. The goal of this committee is to provide the best evidence-based guidance to assist personnel in performing safe laser procedures.
What Are the Responsibilities of a Laser Safety Officer?
ANSI Z136.3 defines the LSO as the employee in each facility responsible for the laser safety program. This person has the training necessary to oversee the laser safety program and is also responsible for monitoring laser hazards.3 Although there is no national certification requirement, the LSO serves in a supervisory and administrative role for all laser systems being utilized in the facility.8,10 Job expectations include recommending personal protective equipment (PPE), obtaining and posting proper warning signs and window shields, implementing standard operating procedures, training staff, maintaining laser systems and accessories within the practice, reporting incidents or injuries, and recommending and providing documentation according to OSHA and ANSI standards.10 Additionally, the designated LSO for a facility may serve as LSO for any cases in which they are operating a laser. Having an LSO does not protect a facility from punishment if adverse events arise due to noncompliance with OSHA and state regulations. The LSO is simply an overseer who monitors all policies and procedures, thus minimizing the risk of any adverse event. The following is a summary of the LSO’s specific responsibilities outlined in ANSI Z136.3.3
1. Hazard Classification
The LSO shall ensure that all laser systems in the facility have been labeled by the manufacturer with the proper hazard classification.
The 4 laser classes, as defined by ANSI, are listed in Table 1.
2. Hazards Evaluation
The LSO shall evaluate the potential hazards of the laser utilized in the treatment control area.
He or she may utilize hazard and safety guidelines provided by the laser manufacturer. In some cases, however, the LSO may perform a hazard evaluation and determine the hazard themselves.
3. Hazard Response
The LSO shall immediately inform users of imminent dangers that can occur when operating the laser system.
4. Control Measures
The LSO shall ensure control measures, as outlined by the manufacturer, are in effect for operating Class IIIb and IV laser systems.
When primary controls are not feasible, the LSO can recommend or substitute measures, provided these changes are documented.
The LSO shall periodically evaluate the efficacy of these controls.
5. Procedure Approvals
The LSO should approve laser systems and equipment before utilization and after any system is evaluated for hazards. Most states require lasers to be registered before operation. It is the responsibility of the LSO to determine the state board requirements and file the necessary paperwork before the laser system may be employed. Please refer to the Appendix, which includes websites with state-specific information as to whether a laser must be registered before operation as well as contact information for state governing bodies.7
Once registered, the LSO shall establish standard operating procedures for laser utilization. These include policies and procedures related to maintenance, calibration, and servicing of both the laser system and accessory attachments.
6. Protective Equipment
The LSO shall ensure PPE is available, in good working order, and properly utilized by everyone in the laser treatment area.
Eyewear should be regularly examined for pitting, cracking, discoloration, light leaks, and scratches.
Any PPE noted to have imperfections should be discarded and replaced.11
7. Signs and Labels
The LSO shall ensure warning signs are available, properly worded, and conspicuously displayed on all entrances to the laser treatment area. Figure 1 illustrates a sample of a warning sign for a Temporary Controlled Area.
It is important to note that according to OSHA regulations, signs can only be posted when the laser is on. When a laser is not in use, the sign must be removed from view or flipped around so the wording is not visible.
8. Facilities and Equipment
The LSO shall approve the laser installation and equipment prior to utilization.
Any modifications to existing equipment shall be reviewed by the LSO and must comply with FDA standards. A hazard evaluation of this modified equipment shall be prepared and filed by the LSO.
The LSO shall ensure routine maintenance and service is performed by qualified personnel and that these events are properly documented.
9. Training
The LSO shall ensure safety education and training is provided to all people associated with the laser. The LSO shall be responsible for documenting certification of trained employees.
Education content should be in accordance with OSHA and ANSI standards, facility policies and procedures, federal, state, and local regulations
Laser users must be trained specifically for each wavelength and modality that they operate. Their skills should be revalidated by the LSO every year.
The LSO shall educate staff on reporting adverse events or product malfunction. Additionally, this person shall recommend policies and procedures to ensure the risk of future events is minimized.
| Class . | Power output . |
|---|---|
| Class I, 1M, and 1Ca | Exempt from radiation hazard controls |
| Class II and IIM | Low powered |
| Class IIIR and IIIB | Medium powered |
| Class IV (all medical lasers) | High powered, >500 mW |
| Class . | Power output . |
|---|---|
| Class I, 1M, and 1Ca | Exempt from radiation hazard controls |
| Class II and IIM | Low powered |
| Class IIIR and IIIB | Medium powered |
| Class IV (all medical lasers) | High powered, >500 mW |
ANSI, American National Standards Institute. aClass IC is designated for home use laser devices.
| Class . | Power output . |
|---|---|
| Class I, 1M, and 1Ca | Exempt from radiation hazard controls |
| Class II and IIM | Low powered |
| Class IIIR and IIIB | Medium powered |
| Class IV (all medical lasers) | High powered, >500 mW |
| Class . | Power output . |
|---|---|
| Class I, 1M, and 1Ca | Exempt from radiation hazard controls |
| Class II and IIM | Low powered |
| Class IIIR and IIIB | Medium powered |
| Class IV (all medical lasers) | High powered, >500 mW |
ANSI, American National Standards Institute. aClass IC is designated for home use laser devices.
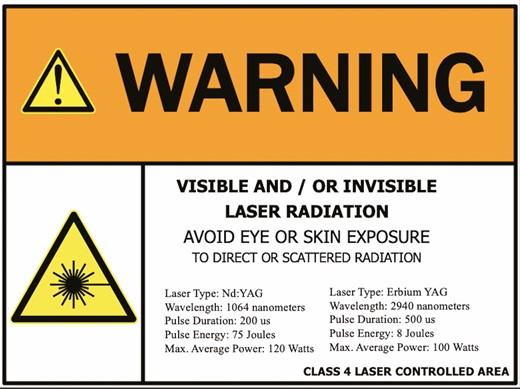
Sample warning sign for laser treatment area. Pertinent information on the notice sign includes a signal word (Warning), special precautionary instructions (Avoid Eye or Skin Exposure to Direct or Scattered Radiation), the type of laser (Nd:YAG and Erbium YAG), emitted wavelength (1064nm and 2940nm), pulse duration (200 us and 500 us), maximum output (120 Watts and 100 Watts), and hazard classification (Class 4).
In addition to appointing an LSO, clinical practices and medical spas should appoint and train a deputy LSO, who is as knowledgeable and proficient in laser operation policies and procedures as the designated LSO. The deputy LSO will serve as a back-up if, for example, the appointed LSO leaves the practice. If an LSO precipitously quits before the deputy LSO role is filled, an interim LSO may be appointed among the remaining staff to serve on a temporary basis until training or hiring of a new LSO in completed; this may include hiring a new staff member on a temporary basis to serve as LSO until the position is permanently filled. In the interim, this temporary LSO will oversee safety in the workplace according to standard operating procedures already established for the facility.
Another situation precipitating the need for an LSO occurs when renting laser units. Many smaller hospitals and clinical settings, who only require a laser for sporadic cases, may elect to rent a unit on a temporary basis. Nevertheless, an LSO should still be appointed while the unit is being housed and operated within the facility. The LSO has the authority to stop or suspend a case. Therefore, this person should be someone employed by the hospital or facility; the laser rental company cannot and does not assume responsibility for this role.
What Are the Components of a Laser Safety Audit?
Equipment safety audits shall be performed and documented under the supervision of the LSO. The frequency of these audits may be determined by the LSO, but should be no less than once per year. The audit should include an evaluation of all laser systems and equipment associated with their utilization, examination of the storage and treatment areas, assessment of staff knowledge on laser operation and safety, a review of documentation for each laser system, and observation of procedures to ensure all operators are in compliance with policies and procedures. Additionally, safety controls should be assessed, including PPE, barrier systems, inhalation protection, fire and electrical safety, and laser storage and entryways. A written report of this audit shall be completed by the LSO and any follow-up actions documented.
Conclusions
The LSO is at the core of the laser safety program. This individual is responsible for the education, supervision, and documentation of all laser operations within the healthcare facility. The LSO evaluates potential hazards and oversees the installation, operation, and maintenance of lasers within the facility. He or she recommends and enforces control measures to prevent injuries that may occur with laser use. Within larger facilities, LSOs cooperate with other members of the laser safety committee to provide operational policies and procedures and educates healthcare personnel on these standards. It is important that these policies and procedures be developed with consideration of the individual practice, standards of care, and federal and state regulations. Additionally, it is the responsibility of the LSO to review these policies and procedures, revise them as necessary, and monitor healthcare personnel for compliance to ensure that safe laser practices are being conducted at the healthcare facility.
It is important to note the limitations of this overview. Because there is no previous literature published on this topic, our discussion is limited to our personal experience developing a laser safety program at our clinical facility based on ANSI guidelines, the OSHA General Duty Clause, and local and federal regulations. Additionally, there is no universal approach for developing an appropriate laser safety program. Smaller clinical settings and medical spas may be limited in staff number and therefore must customize their laser safety program to fit their specific size and needs. The business owner automatically assumes the responsibilities of the LSO or must assign this role to another member of the team. This will most likely require cross-training of existing perioperative personnel. It is important to note that although these smaller facilities do not operate at the same capacity as a large hospital or academic institution, the requirements for operating a laser are no less stringent. The responsibilities of the LSO, as outlined in the ANSI standards and this paper, are just as important, regardless of the business’s size. Although there are no fines specifically for not having an appointed LSO, the purpose of this position is to ensure policies and procedures are properly followed. Not having an LSO to oversee laser operations potentially exposes a facility to more risk and, ultimately, noncompliance with OSHA, state, and federal regulations. These violations can lead to heavy fines and litigation. Similarly, having an LSO does not prevent punishment should an adverse event arise due to noncompliance with policies set forth by regulatory agencies. The LSO simply monitors all aspects of laser operations within a facility to minimize the risk of any adverse events. Clinical practices and medical spas should reach out to their specific state regulatory agency, listed in the Appendix, should they have any questions regarding the development and execution of laser policies and procedures.7 Rockwell Laser Industries regularly updates this reference. For the most recent list of state laser safety contacts, please refer to their resource online (https://www.rli.com/resources/statecontacts.aspx).
Disclosures
The authors report sponsor-supported funding from Venus Concept (Toronto, Canada) and Bellus Medical (Dallas, TX) for research studies outside of the submitted work.
Funding
The authors received no financial support for the research, authorship, and publication of this article.
References
American National Standards Institute.
American National Standards Institute.
United States Department of Labor.
Author notes
Dr Kenkel is Associate Editor of Aesthetic Surgery Journal (ASJ) and Editor-in-Chief of ASJ Open Forum



