-
PDF
- Split View
-
Views
-
Cite
Cite
Christine E Wamsley, John Hoopman, Jeffrey M Kenkel, Safety Guidelines Concerning the Use of Protective Eyewear and Gauze During Laser Procedures, Aesthetic Surgery Journal, Volume 41, Issue 10, October 2021, Pages 1179–1185, https://doi.org/10.1093/asj/sjaa233
Close - Share Icon Share
Abstract
The advancement of laser technology has seen its use gain popularity across a wide range of specialties to treat diseases, as well as address aesthetic concerns. In order to protect both the patient and the healthcare personnel providing treatment, instruction and knowledge of laser safety remain of utmost importance. In this paper, we discuss the classification of laser systems, review ocular injuries that may be caused by inappropriate laser exposure, and provide background on laser protective eyewear. In addition, we highlight the current recommendations for proper eyewear during laser use outlined in the American National Standards Institute standard Z136.3, Safe Use of Lasers in Health Care. Finally, although it is common in some healthcare facilities to place gauze under external eye shields or use gauze alone over eyes during laser procedures, this practice poses an extreme risk to both patients and healthcare personnel. Therefore, we discuss why the use of gauze under eyewear for any laser procedures is not recommended, and instead, offer suggestions to consider when acquiring safe and comfortable patient eyewear.
Ongoing advancements in laser technology have led to its application in treating a variety of diseases as well as addressing aesthetic concerns. Due to the increasing popularity of lasers, instruction and knowledge of laser safety are of the utmost importance. The American National Standards Institute (ANSI) is a private organization that develops a wide range of standards, including guidelines for the safe use of lasers in both industry and medicine.1 In particular, 2 documents published by the organization outline these standards. The American National Standard for Safe Use of Lasers (ANSI Z136.1) discusses the general topic of laser safety, whereas the American National Standard for Safe Use of Lasers in Health Care (ANSI Z136.3) focuses on the proper operation of lasers serving as medical devices.2,3 These guidelines are revised approximately every 5 years to reflect current laser practices and technologies and are effective immediately upon publication. The most recent version of ANSI Z136.1 was released in 2014 and Z136.3 in 2018. Although compliance with these guidelines is only voluntary, they are generally regarded as the best current practice and considered standard of care for manufacturers, consumers, and the general public in the United States.4 The Occupational Safety and Health Administration (OSHA) does not have its own set of comprehensive guidelines regarding eye protection and laser safety. Instead, it defers to the standards outlined by ANSI and the Center for Devices and Radiological Health branch of the Food and Drug Administration.4
Laser safety is based on the potential hazard that can result from operating the system. The maximum permissible exposure (MPE) is the “level of laser radiation to which a person, under normal circumstances, may be exposed without hazardous effects,” such as eye injury or skin damage.3 In general, the longer the wavelength emitted, the higher the MPE, and the longer the exposure time, the lower the MPE.5 The nominal hazard zone (NHZ) is the “space within which the level of direct, reflected, or scattered radiation during normal operation exceeds the applicable MPE.” 2,3 In other words, this is the area in which the energy emitted by the laser is greater than the MPE.1,6 Both ANSI Z136.1 and ANSI Z136.3 give recommendations for the MPE and NHZ for most lasers in commercial and clinical use.3,6
Laser systems in the United States are classified according to ANSI Z136.1 and are divided into 4 classes, with further subcategorizations. Class 1 lasers do not emit enough radiation to exceed the MPE and inflict eye or skin damage.7 They are extremely low powered, and measures to prevent laser exposure are therefore generally unnecessary.1,6 Examples include laser printers and barcode scanners.7,8 Class 1C applies to lasers operating in contact with their intended target, and these lasers are therefore required to have safeguards to prevent the leakage of laser radiation greater than the accessible emission limits of Class 1.3 Class 1M laser systems cannot produce hazardous exposure conditions unless viewed through an optical instrument, such as a microscope or telescope.3 Class 2 lasers emit energy in the visible light spectrum (400-700 nm), but do not emit radiant energy greater than 1 mW.7 The blink reflex, which occurs within 0.25 s, generally protects against potential hazards caused by these lasers.2,7 Although momentary viewing is generally not harmful, the MPE may be exceeded by staring into the beam for a prolonged period of time.8 An example of a device in this class would be a helium-neon laser pointer.6 Class 2M laser systems also emit energy in the visible light spectrum and the blink reflex protects against eye hazards, but these lasers can potentially be hazardous if viewed with certain optical aids.3 Class 3 is subdivided into two categories: 3R and 3B. The direct beam or specular (mirror-like) reflection of 3R lasers can be potentially hazardous. These lasers are relatively low risk, but can inflict severe eye damage if viewed through optical instruments, such as binoculars or microscopes.7 3B lasers are of medium power, ranging from 5 to 500 mW, and can also be dangerous if viewed directly or via specular reflection.6 Class 4 lasers have power outputs greater than 500 mW and represent a potential fire hazard.3,8 Their direct, specular, and even diffusely reflected beams are capable of causing serious adverse events, including instantaneous eye damage and severe skin injury, as well as dangerous hazards, such as the ignition of flammable materials.6 Nearly all surgical lasers fall into this class.8Table 1 provides a brief summary of the 4 laser classes.
| Class . | Power output . |
|---|---|
| I, 1M, and 1Ca | Exempt from radiation hazard controls |
| II and IIM | Low powered |
| IIIR and IIIB | Medium powered |
| IV (all medical lasers) | High powered, >500 mW |
| Class . | Power output . |
|---|---|
| I, 1M, and 1Ca | Exempt from radiation hazard controls |
| II and IIM | Low powered |
| IIIR and IIIB | Medium powered |
| IV (all medical lasers) | High powered, >500 mW |
aClass IC is designated for home-use laser devices.
| Class . | Power output . |
|---|---|
| I, 1M, and 1Ca | Exempt from radiation hazard controls |
| II and IIM | Low powered |
| IIIR and IIIB | Medium powered |
| IV (all medical lasers) | High powered, >500 mW |
| Class . | Power output . |
|---|---|
| I, 1M, and 1Ca | Exempt from radiation hazard controls |
| II and IIM | Low powered |
| IIIR and IIIB | Medium powered |
| IV (all medical lasers) | High powered, >500 mW |
aClass IC is designated for home-use laser devices.
OCULAR HAZARDS
The eye contains many structures that can each act as a chromophore for laser light.6,9 The exact part of the eye at risk of damage depends upon the wavelength emitted by the laser.9 The “retinal hazard zone” spans from 400 to 1400 nm and includes visible light (400-780 nm) as well as the near-infrared region (780-1400 m).8,9 When the eye focuses, radiant energy is amplified roughly 100,000 times.6,7Figure 1 illustrates a parallel laser beam entering the cross section of a human eye. Focal magnification of the beam can result in significant optical injury. As this energy is absorbed in the form of heat, the thermal damage irreparably destroys retinal tissue, leading to loss of color vision, night blindness, and potentially complete loss of vision.6,7 It should be noted that the retina does not contain pain receptors and cannot perceive wavelengths greater than 780 nm, the high end of the visible light spectrum.6 Therefore, exposure to near-infrared light may go unnoticed until severe damage is done.6,10 One notable device that emits energy in this range is the 1064-nm neodymium:yttrium-aluminum-garnet (Nd:YAG) laser, which uses a synthetic crystal as a medium and is most commonly associated with accidental retinal injuries.11 Q-switched lasers, which emit short (~30 ns), high-powered pulses, are also potentially dangerous to the retina, as they can cause photoacoustic damage along with thermal damage.6 Photoacoustic damage is due to shock waves transmitted through the retina, which can lead to disruption or damage of the structure.
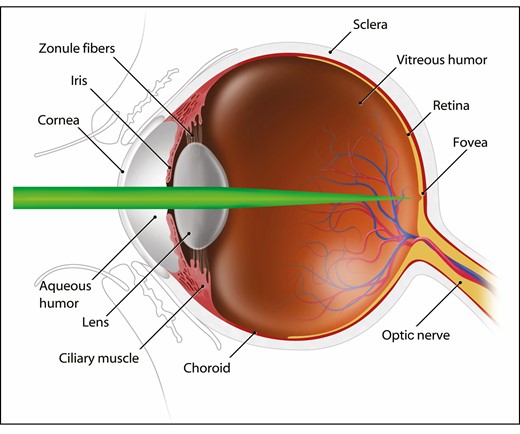
A cross-sectional image of a laser beam entering the eye. As the eye attempts to focus the image, radiant energy is amplified approximately 100 times. The type of optical injury is dependent upon the wavelength of laser radiation.
Wavelengths within the mid-infrared (1400-3000 nm) and far-infrared regions (3000-10,600 nm) are primarily absorbed by water, the main component of the cornea and lens. Through this absorption, these wavelengths cause protein denaturation on the corneal surface, leading to corneal burns and opacities.4,6 This injury can be seen with the use of carbon dioxide (CO2) lasers and erbium:YAG lasers.8,12 Unlike the retina, the superficial layers of the cornea are not subject to light amplification and are capable of regeneration, usually within a few days.10,13 Additionally, mid-infrared wavelengths may penetrate deeper and cause photochemical denaturation of lens proteins, resulting in cataract formation.8 Cataracts are also a potential hazard caused by near-ultraviolet wavelengths (315-400 nm), as they can also pass through the cornea and be absorbed by the lens.8Table 2, adapted from chapter 6.III of the OSHA Technical Manual, lists the optical injuries that can occur as a result of exposure to lasers at various wavelengths.4
| Wavelength of light . | Eye effects . |
|---|---|
| UV C (200–280 nm) | Photokeratitis |
| UV B (280–315 nm) | |
| UV A (315–400 nm) | Photochemical ultraviolet cataract |
| Visible light (400–780 nm) | Photochemical and thermal retinal injury |
| Near-infrared (780–1400 nm) | Cataract, retinal burns |
| Mid-infrared (1400–3000 nm) | Corneal burn, aqueous flare, infrared cataract |
| Far-infrared (3000–10,000 nm) | Corneal burn |
| Wavelength of light . | Eye effects . |
|---|---|
| UV C (200–280 nm) | Photokeratitis |
| UV B (280–315 nm) | |
| UV A (315–400 nm) | Photochemical ultraviolet cataract |
| Visible light (400–780 nm) | Photochemical and thermal retinal injury |
| Near-infrared (780–1400 nm) | Cataract, retinal burns |
| Mid-infrared (1400–3000 nm) | Corneal burn, aqueous flare, infrared cataract |
| Far-infrared (3000–10,000 nm) | Corneal burn |
| Wavelength of light . | Eye effects . |
|---|---|
| UV C (200–280 nm) | Photokeratitis |
| UV B (280–315 nm) | |
| UV A (315–400 nm) | Photochemical ultraviolet cataract |
| Visible light (400–780 nm) | Photochemical and thermal retinal injury |
| Near-infrared (780–1400 nm) | Cataract, retinal burns |
| Mid-infrared (1400–3000 nm) | Corneal burn, aqueous flare, infrared cataract |
| Far-infrared (3000–10,000 nm) | Corneal burn |
| Wavelength of light . | Eye effects . |
|---|---|
| UV C (200–280 nm) | Photokeratitis |
| UV B (280–315 nm) | |
| UV A (315–400 nm) | Photochemical ultraviolet cataract |
| Visible light (400–780 nm) | Photochemical and thermal retinal injury |
| Near-infrared (780–1400 nm) | Cataract, retinal burns |
| Mid-infrared (1400–3000 nm) | Corneal burn, aqueous flare, infrared cataract |
| Far-infrared (3000–10,000 nm) | Corneal burn |
There are 2 transition zones where damage may be inflicted to the retina as well as the cornea and lens simultaneously. These include the transition from UV to visible light (around 400 nm) and from near-infrared to mid-infrared light (around 1300 nm).6 Currently, lasers around 400 nm are not commonly used for aesthetic treatment. A literature search found no scientific papers discussing ocular safety near this wavelength. One example that falls within the transition zone is the 1320-nm Nd:YAG laser, a nonablative laser still commonly used for skin rejuvenation.14,15 Ocular exposure to this wavelengths has been found to simultaneously cause both corneal and retinal lesions, as well as cortical cataracts.14
PROTECTIVE EYEWEAR BACKGROUND
Laser protective eyewear (LPE) is required for providers and patients receiving laser treatment or for healthcare personnel operating Class 3B or 4 lasers.3 When patient and staff eyes are potentially within the NHZ, they must be shielded in order to reduce the potential ocular hazard to below the MPE. Under some conditions, the NHZ may occupy the entire room in which the laser procedure is being performed. In these circumstances, everyone present must wear the appropriate LPE. Protective eyewear may include wavelength-specific goggles, face shields, spectacles, or prescription eyewear with special filters or reflective coatings.1,3,7 An appointed laser safety officer (LSO), the laser operator, or ancillary personnel are responsible for selecting the proper eyewear before a procedure is performed. It should be noted that standard eyeglasses and contact lenses have no role as personal protective equipment.3
The appropriate protection will depend on several factors, including the procedure being performed, the target tissue site, the laser wavelength, the positioning of the patient, and the type of anesthesia being administered.2 No single piece of eyewear can protect against laser emissions of all wavelengths. Wavelength-specific eyewear can prevent potential ocular hazards caused by use of a laser that emits energy at that wavelength. Additionally, built-in side shields can prevent any injury caused by tangential beams or scattered radiation.2,6 A cautionary note: no LPE is designed to prevent exposure when looking directly at a laser beam.2
Eye protection must be clearly and permanently labeled with 2 numbers: the optical density (OD) and the wavelength the eyewear protects against. OD is defined by ANSI as “a value that defines the attenuation property of a filter and is equal to the logarithm to the base ten of the reciprocal transmittance at a particular wavelength (OD = log10[1/τ(λ)], where τ(λ) is transmittance at wavelength λ.”2 In other words, the OD defines the ability of a lens to attenuate transmitted light of a specific wavelength.6Table 3 illustrates the conversion of OD to percent transmittance. Many lasers emit more than one wavelength. Therefore, the proper eyewear for a laser system must have adequate OD to cover all wavelengths emitted by that particular laser system.2
| Optical density . | Attenuation rate . | Percent transmittance . |
|---|---|---|
| 0 | 0 | 100 |
| 1 | 1/101 | 10 |
| 2 | 1/102 | 1 |
| 3 | 1/103 | 0.1 |
| 4 | 1/104 | 0.01 |
| 5 | 1/105 | 0.001 |
| 6 | 1/106 | 0.0001 |
| 7 | 1/107 | 0.00001 |
| 8 | 1/108 | 0.000001 |
| 9 | 1/109 | 0.0000001 |
| 10 | 1/1010 | 0.00000001 |
| Optical density . | Attenuation rate . | Percent transmittance . |
|---|---|---|
| 0 | 0 | 100 |
| 1 | 1/101 | 10 |
| 2 | 1/102 | 1 |
| 3 | 1/103 | 0.1 |
| 4 | 1/104 | 0.01 |
| 5 | 1/105 | 0.001 |
| 6 | 1/106 | 0.0001 |
| 7 | 1/107 | 0.00001 |
| 8 | 1/108 | 0.000001 |
| 9 | 1/109 | 0.0000001 |
| 10 | 1/1010 | 0.00000001 |
| Optical density . | Attenuation rate . | Percent transmittance . |
|---|---|---|
| 0 | 0 | 100 |
| 1 | 1/101 | 10 |
| 2 | 1/102 | 1 |
| 3 | 1/103 | 0.1 |
| 4 | 1/104 | 0.01 |
| 5 | 1/105 | 0.001 |
| 6 | 1/106 | 0.0001 |
| 7 | 1/107 | 0.00001 |
| 8 | 1/108 | 0.000001 |
| 9 | 1/109 | 0.0000001 |
| 10 | 1/1010 | 0.00000001 |
| Optical density . | Attenuation rate . | Percent transmittance . |
|---|---|---|
| 0 | 0 | 100 |
| 1 | 1/101 | 10 |
| 2 | 1/102 | 1 |
| 3 | 1/103 | 0.1 |
| 4 | 1/104 | 0.01 |
| 5 | 1/105 | 0.001 |
| 6 | 1/106 | 0.0001 |
| 7 | 1/107 | 0.00001 |
| 8 | 1/108 | 0.000001 |
| 9 | 1/109 | 0.0000001 |
| 10 | 1/1010 | 0.00000001 |
The OD is the inverse log of how much light is blocked by the material. Each increase in OD will reduce the transmittance, and therefore exposure, at a specific wavelength by a factor of 10. The greater the OD of a material, the greater resistance it has to light passing through it. For example, materials with an OD of 10 permit the least amount of light transmission, as seen in Table 3. Although in theory the highest possible OD is desirable, there must be a balance between eye protection and visibility.16 Therefore, protective eyewear should transmit as much visible light as possible, while still maintaining sufficient protection.6 Although increasing the OD by 1 lowers the amount of light exposure by a factor of 10, it also lowers the MPE hazard risk by 50%. An OD of 5 is recommended for maximum safety, as it balances the optical gain of the eye.
Cleaning and inspection of protective eyewear should be performed periodically. Care should be taken to avoid damaging the surface when handling or cleaning the eyewear. Recommendations for cleaning should be provided to the laser operator by the manufacturer.2 Any LPE noted to have imperfections should be discarded and replaced.2,8 The following should be inspected carefully when examining eyewear:
The attenuation material to ensure there is no pitting, cracking, or discoloration
The frame for mechanical integrity
The straps or fastening device to ensure they are not damaged or excessively worn
Any light leaks or scratches in the coating that may expose the eye to the laser beam2
PATIENT-SPECIFIC PROTECTIVE EYEWEAR
Conventional eyewear may be sufficient to protect a patient’s eyes during some laser treatments. However, facial procedures require snug-fitting external eye shields or internal corneal shields. Mini-goggles must be adjusted to ensure a light-proof seal.6 Additionally, there are commercially available disposable external eye shields specifically for laser, intense pulsed light (IPL), and light-emitting diode (LED) procedures. These patches adhere around the patient’s orbital rim in order to protect the eyes, eliminate light leakage, and avoid damaging the eyelashes. If there is any concern about inadequate protection, heat-proof stainless-steel corneal eye shields should be used. See Figure 2 for examples of these different types of eyewear.
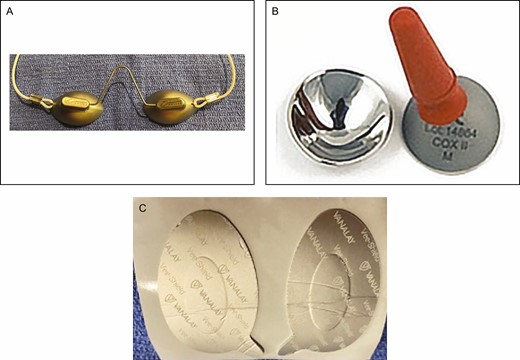
(A) External eye shields, (B) internal corneal eye shields, and (C) disposable eye shields.
Ries et al17 measured the thermal response curves of 6 commercially available eye protectors when exposed to 4 different lasers at 3 intensity settings. Plastic eye shields showed significant thermal damage when exposed to the lasers and actually ignited when exposed to the CO2 laser. Hence, such plastic eye shields are inappropriate and potentially dangerous if used on patients undergoing facial laser procedures. On the other hand, metallic shields remained intact and warmed only slightly (by between 0 and 5°C) due to their high reflectivity.
USE OF GAUZE WITH PROTECTIVE EYEWEAR
It has become increasingly common in some clinical practices to place gauze under the patient’s external eye shields or to use gauze alone as eye protection during laser procedures. These external eye shields are generally made of a stainless-steel material and are intended to protect the patient from a laser strike, diffuse reflections, or the bright flash some wavelengths can create. Common reasons for using gauze are discomfort caused by the eye shields, improperly fitting eye shields that may permit ocular exposure to the laser beam, or concern about damaging the patient’s eyelashes. Although the use of gauze may seem like a simple and practical solution to these issues, it is important to note that this material is extremely flammable. Its use during facial laser procedures creates a fire hazard and poses a significant risk to both the patient and the laser operator.
We conducted a study at our site to examine the inherent flammability of gauze when subjected to several lasers commonly used for aesthetic procedures. When dry gauze was exposed to a 2940-nm erbium:YAG laser at 20 J/cm2 to a depth of 80 μm, smoke was present on the first pass and a visible flame was present on the second pass. On the other hand, no smoke or flame appeared after 8 passes over wet gauze. Similarly, when dry gauze was exposed to a 10,600 nm CO2 laser at 11.3 J/cm2 at a rate of 50 Hz, smoke was present on the first pass, the gauze ignited on the second pass, and visible damage underneath the gauze was noted after the third pass. Moistened gauze, however, was much more resistant to ignition, and there was no perforation of the gauze after 3 passes (Video, available online at www.aestheticsurgeryjournal.com).
The results of our experiment mirror findings reported by Ahmed et al,18 who exposed both wet and dry surgical materials to a Sigmacon Acupulse Lumenis CO2 laser. After 180 seconds of continuous application, the laser failed to penetrate the wet gauze at all wattages, whereas dry gauze remained susceptible to penetration even at the lowest power. These results highlight the importance of keeping laser consumables wet throughout a laser treatment. However, Ahmed et al noted that gauze swabs may dry out during a lengthier operation. Due to the extreme risk of having dry gauze present within the treatment area, as highlighted in these 2 studies, it is our belief that clinicians should avoid the use of dampened gauze pads under protective eyewear altogether. Instead, the focus should be on acquiring properly fitting eyewear that provides adequate protection and comfort to the patient.
In addition to the issue of maintaining moisture throughout treatment, ANSI notes that wet eye pads are not appropriate for all wavelengths. In ANSI Z136.3, it is stated that for a CO2 laser treatment, the LSO may determine that wet eye pads or gauze are sufficient protection. However, wet eye pads may not confer eye protection for all wavelengths, in particular argon, potassium titanyl phosphate, and Nd:YAG,2 as the wavelength will transmit directly through water. Therefore, in order to minimize any potential risks, we do not recommend the use of gauze under protective eyewear.
AUTHOR RECOMMENDATIONS
In order to improve patient safety and comfort, the following guidelines may be implemented.
Use of Approved Eyewear
ANSI guidelines state that appropriate LPE must be worn by everyone in the NHZ while the laser is in operation. Appropriate LPE consists of glasses, goggles, or eye shields with sufficient OD to prevent ocular injury when a Class 3B or 4 laser is in use.
The user and LSO are responsible for selecting and examining eyewear for comfort, proper fit, and presence of labels describing both wavelength and OD. Any eyewear not bearing a permanent label stating the OD and wavelength against which it protects is not intended for laser use.
To eliminate any patient cross-contamination, it is imperative that eyewear is properly disinfected according to the manufacturer’s instructions.
Damaged LPE should be discarded and replaced.
Use of Properly Fitting External Eye Shields
In order to reduce costs, manufacturers often provide solid one-piece external eye shields with their device, which may not fit every patient properly.
There are eye shields currently available on the market with straps or arms that can be adjusted to fit each individual patient’s face.
Selecting an External Eye Shield That Is Comfortable and Easy to Use
There are external eye shields currently available that offer features such as a maneuverable nose bridge or brow bar, adjustable eye cups that can change pupillary distance, and silicone rims for added comfort.
Use of Disposable Eye Protection
Disposable shields tightly adhere to the patient’s orbital area to ensure that laser beams or bright light are sufficiently blocked out. These shields can be applied during laser, IPL, or LED procedures. They can be worn alone or in conjunction with external eye shields, and eliminate the risk of any fire hazard.
CONCLUSIONS
Lasers serve as an almost ideal point source of light. The most common cause of laser-induced eye injury is thermal damage.4 As laser energy is absorbed in the form of heat, tissue proteins are denatured. Different wavelengths inflict different types of damage to the various parts of the eye, and adverse events can vary in nature from burns and cataracts to permanent blindness. Therefore, it is crucial for laser operators to be familiar with the specific wavelength of laser they are using to treat patients. When a new type of laser is acquired, it is important that laser operators be retrained regarding the safe use of this newly acquired instrument. Clinical experience may not necessarily transfer from one type of laser to the next.4
This paper specifically highlights the current recommendations for proper eyewear during laser use. Currently, the literature regarding this topic is lacking, particularly relating to ocular safety when operating lasers within the plastic surgery setting. Our discussion is, therefore, limited to our site’s experiences and recommendations, based on standard-of-care guidelines, such as those produced by ANSI, and OSHA regulations. Although compliance with these standards is voluntary, they are based on a national consensus and generally considered best clinical practice. Organizations such as OSHA defer to the recommendations outlined by ANSI.
It is common practice in some healthcare facilities to place gauze under external eye shields or use gauze alone over eyes during laser procedures. This inherently flammable material poses an extreme fire hazard and danger to the patient, the laser operator, and anyone else present within the NHZ. Studies have shown that dampening the gauze may mitigate this risk.18-20 ANSI Z136.3 states that dry materials should be placed on the patient’s face or eyes only when absolutely necessary.2 However, as moistened eye pads are not appropriate for all wavelengths and it not always possible to maintain adequate moisture during lengthier procedures, we do not recommend the use of gauze under eyewear for any laser procedures.18 Rather, focus should be placed on acquiring the proper eyewear that provides adequate comfort and protection without the need for gauze.
Acknowledgement
The authors would like to thank Kate Mackley for her assistance in designing the figures and video included with this paper.
Disclosures
The authors report sponsor-supported funding from Venus Concept (Westin, FL) and Bellus Medical (Dallas, TX) for research studies outside of the submitted work.
Funding
The authors received no financial support for the research, authorship, and publication of this article.
REFERENCES
Author notes
Dr Kenkel is associate editor of Aesthetic Surgery Journal (ASJ) and editor-in-chief of ASJ Open Forum.



