-
PDF
- Split View
-
Views
-
Cite
Cite
Shahar Shmuel, Charles E Leonard, Katsiaryna Bykov, Kristian B Filion, Marissa J Seamans, Jennifer L Lund, Breaking Research Silos and Stimulating “Innovation at the Edges” in Epidemiology, American Journal of Epidemiology, Volume 192, Issue 3, March 2023, Pages 323–327, https://doi.org/10.1093/aje/kwac192
Close - Share Icon Share
Abstract
Epidemiological training often requires specialization in a subdiscipline (e.g., pharmacoepidemiology, genetic epidemiology, social epidemiology, or infectious disease epidemiology). While specialization is necessary and beneficial, it comes at the cost of decreased awareness of scientific developments in other subdisciplines of epidemiology. In this commentary, we argue for the importance of promoting an exchange of ideas across seemingly disparate epidemiologic subdisciplines. Such an exchange can lead to invaluable opportunities to learn from and merge knowledge across subdisciplines. It can promote “innovation at the edges,” a process of borrowing and transforming methods from one subdiscipline in order to develop something new and advance another subdiscipline. Further, we outline specific actionable steps at the researcher, institution, and professional society level that can promote such innovation.
While epidemiology has its own core methodology, epidemiologic training frequently requires specialization in a specific subdiscipline (e.g., pharmacoepidemiology, genetic epidemiology, social epidemiology, or infectious disease epidemiology). Specialization allows for in-depth methodological and substantive knowledge of a given research area and development of a research network of colleagues with shared interests. However, it comes at the cost of decreased awareness of scientific developments in other subdisciplines of the field. Most researchers (trainees and faculty members alike) do not regularly engage in seminars, conferences, and discourse outside their chosen subdiscipline. Given the substantial time constraints of existing professional and personal responsibilities, it is challenging to allocate time to such activities that are often perceived to have limited applicability. Furthermore, at the institutional level, there may be a lack of incentive to do so. Promotion and other accolades often are contingent on being a leader and expert within a subdiscipline, and less (and sometimes, substantially less) credit is given for collaborative work done outside of the direct scope of one’s research program, where one may play a supporting rather than a leadership role. This isolation of subdisciplines is further reinforced at the professional society level, where scientific conferences and journals tend to be specialized or to promote subdiscipline focus.
These multilevel barriers contribute to siloed and increasingly isolated epidemiologic subdisciplines, with key developments remaining in a specialized knowledge domain, as opposed to spreading across subdisciplines. This leads to inefficiency and missed opportunities to learn from each other’s progress by applying methodological advances from another subdiscipline to address a pressing issue in one’s own research. The healthy-worker survivor bias, which originated within the subdiscipline of occupational epidemiology (1), is a key example of the importance of cross-pollination of epidemiologic subdisciplines. Awareness of this bias helped inform the origin of and coining of the term healthy-user bias and the development of the new-user study design in pharmacoepidemiology (2), a design which has played a pivotal role in shaping this subdiscipline. Yet it took time for the awareness of this bias and methods to address it to spread across subdisciplines, leading to flawed observational studies, the results of which were later refuted by randomized trial results (3).
As pharmacoepidemiologists, we are accustomed to interdisciplinary collaborations with clinicians, biostatisticians, pharmacologists, patient advocates, and health policy experts. We rely on these collaborations because our subdiscipline is primarily a methods-based subdiscipline rather than a disease-based subdiscipline (e.g., cancer epidemiology) and therefore we need to recognize the limits of our knowledge and to call on external expertise. However, to be truly innovative, we need to not only recognize the limits of our knowledge but be open to novel ideas coming from unexpected sources. The idea that innovation tends to occur at the interfaces of disciplines (4), or edges of knowledge, has been previously described in other contexts (5, 6). This idea speaks to the value of breaking down barriers and bringing together seemingly disparate fields in order to explore the potential for finding connections that allow existing concepts to be combined to form something new (5).
Diez Roux stressed that engaging multiple disciplines of population health is challenging but vital for epidemiologic research (7). As Gilman et al. described in another commentary in the Journal, social epidemiology is a subdiscipline that embodies this approach and is “…at the leading edge of expanding the standard methodological repertoire in epidemiology, in part through [social epidemiologists’] close collaborations with [their] colleagues in methods development and in part through borrowing techniques used in other disciplines” (8, p. 559). In the spirit of Basu et al.’s endorsement of a “…cross-discipline intellectual arbitrage between epidemiology and economics” (9, p. 542), we argue that a methodological arbitrage between seemingly disparate epidemiologic subdisciplines will support innovation and that there is an opportunity to borrow and transform methods from one subdiscipline to develop something new and advance another subdiscipline.
Our personal experience working at the intersection of pharmacoepidemiology and other subdisciplines led to several exciting innovations and inspired ideas for future applications. For example, working at the intersection of pharmacoepidemiology and social epidemiology, Seamans et al. (10) adapted the new-user study design to develop the new-household design, which they applied to study incident prescription opioid use among household members. The new-household study design has potential applications for other subdisciplines such as injury epidemiology and psychiatric epidemiology. Working at the intersection of pharmacoepidemiology and cardiovascular disease epidemiology, Filion et al. (11) applied the prevalent new-user design to compare the risk of serious cardiovascular events among users of two different diabetes medications (12). This approach can be adapted to study behavioral changes, such as the effect of smoking cessation on long-term cardiovascular outcomes. Working at the intersection of pharmacoepidemiology and environmental epidemiology, Nam et al. (13) reported an interaction between empiric potassium use and daily maximum temperature which may have implications for patients taking furosemide. Bykov et al. (14) have been adopting self-controlled designs, some of which have been until recently more commonly used in other fields, such as environmental epidemiology, to studying drug-drug interactions, work that also has potential applications in genetic epidemiology. While these examples represent our own personal experiences in applying our training, we believe unresolved issues in pharmacoepidemiology may be prime opportunities for future collaborations across other subdisciplines as well. For instance, increased collaboration with social epidemiologists can help us strive to achieve pharmacoequity (15).
To promote methodological arbitrage between seemingly unrelated epidemiologic subdisciplines, we started a dialogue by curating a symposium entitled “Recent Advances in Pharmacoepidemiologic Study Design: Opportunities for Collaboration and Dissemination” at the 2021 Society for Epidemiologic Research Annual Meeting. Here we outline several actionable steps to enhance innovation at the edges in epidemiology at the researcher, institution, and professional society levels (Figure 1).
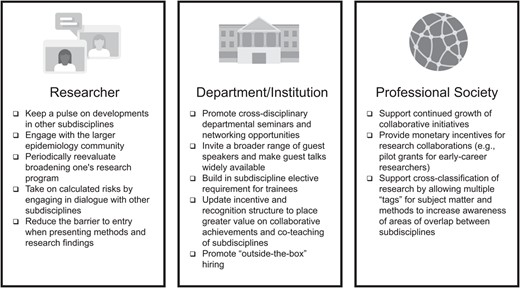
Actionable steps to enhance innovation at the edges in epidemiology at the researcher, institution, and professional society levels.
At the researcher level, we recommend that, as epidemiologists, we remain open to and curious about other epidemiologic subdisciplines and stay up to date on new developments in other areas, even when there is no immediate application for this knowledge to our own work. This can be achieved at the training stage by assigning readings from general epidemiology journals, recommending that trainees subscribe to a variety of general and subdiscipline-specific journals’ electronic tables of contents, and encouraging them to follow and engage with the larger epidemiology community through epidemiology-themed podcasts and #EpiTwitter, where some researchers promote and react to newly published work. Trainees should also be encouraged to attend seminars that are outside their subdiscipline, if available. As one progresses in their career trajectory, it is important to periodically reevaluate whether there are opportunities to broaden the focus of one’s research program. We further encourage epidemiologists at all career stages to take on calculated risks by engaging in dialogue outside their subdiscipline, embarking on new collaborations, testing out new ideas, and considering how their research may contribute to other subdisciplines. Additionally, when writing or presenting results, we encourage researchers to strive to reduce the barrier to entry by providing sufficient context, defining terms, and making the methods and findings accessible to researchers in other epidemiologic subdisciplines.
At the institution or department level, departments would benefit from promoting cross-departmental seminars and offering networking opportunities to connect colleagues at multiple careers stages—undergraduate students, graduate students, postdoctoral fellows, early career faculty, mid-career faculty, and late career faculty. They should also leverage the increased connectivity capabilities developed during the coronavirus disease 2019 pandemic to: 1) invite a broader range of guest speakers across departments, institutions, and countries, and 2) advertise guest talks widely and, if possible, make them publicly available. Departments can also require that trainees take one or two electives in another subdiscipline during their graduate studies. Additionally, we recommend that departments and institutions update their incentive and recognition structures to place greater value on team and collaborative science achievements as well as co-teaching across subdisciplines. It is difficult to attribute the current incentive structures to the institution versus the individuals involved in decision-making. However, increasing diversity in leadership and professional society support are key to bringing about this change. Furthermore, institutions can promote “outside-the-box” hiring by encouraging postdoctoral and faculty candidates with training in other subdisciplines and skill sets to apply. These applicants have unique perspectives and can enrich the research conducted in the department by generating new ideas.
At the epidemiologic society or organization level, we encourage the continued growth of collaboration initiatives. For instance, the Society for Epidemiologic Research (SER) Collaborations Initiative program has already had several successful cross-organization events, including with the Interdisciplinary Association for Population Health Science, the American Society of Preventative Oncology, and the International Society for Pharmacoepidemiology. We also recommend providing monetary incentives for collaborations. Societies offering pilot grants for multidisciplinary teams will encourage early-career researchers to collaborate across institutions and engage with other subdisciplines at a stage in which they are building their research programs. This will both lead to stronger, more thoughtful immediate end products and may encourage early-career researchers to adopt a collaborative approach as they continue in their career path. Last, borrowing from how researchers engage with one another on social media platforms, we encourage greater cross-classification of research. Rather than siloing manuscripts in a journal or presentations at a conference to a single subdiscipline (e.g., environmental health), we suggest that they be allowed and encouraged to have multiple “tags” for both the subject matter (e.g., exposure, outcome, study population) and methods (e.g., study design, main analytical methods). This cross-classification approach may alert researchers to shared interests and approaches, enabling them to network and increase the potential for future collaboration.
We further recommend three paradigm-shifting suggestions to be scaled up over time. At the department level, the key to increasing collaboration is greater exposure to each of the subdisciplines during the training phase. Incorporating guest lectures (and eventually rotating the core teaching faculty) will allow the methods and examples discussed to reflect the diversity of epidemiologic subdisciplines. The core curriculum should highlight how methods from one subdiscipline can inform another and the importance of collaboration. This tag-team approach to the curriculum will promote faculty collaboration, which will hopefully be mirrored by trainees.
At the institution level, we propose developing funded creativity hubs in which urgent problems are addressed using a collaborative problem-solving approach, and multiple disciplines (e.g., epidemiology, biostatistics, health behavior, health policy) play a role. The coronavirus disease 2019 pandemic forced this type of cross-disciplinary collaboration, in which infectious disease epidemiologists, social epidemiologists, geographers, and health-services researchers collaborated to understand disease spread and the impact of potential interventions. This approach can start with studies to define the problem all the way through studies of interventions to guide public policy. The outputs of one study will be the appropriate inputs for the next. If successful, these hubs will become the problem-solving norm university-wide.
At the professional society level, we propose problem-solving sessions where students, postdoctoral fellows, and faculty tackle high-priority methodological issues affecting multiple subdisciplines (e.g., selection bias). Currently, the Society for Causal Inference, which includes some epidemiologists, organizes such events (16), but we encourage the Society for Epidemiologic Research to host these events also. If successful, they can become a pillar of the conference, with a day dedicated to problem-solving sessions. At the professional society level, we should also evaluate subdiscipline organization (e.g., disease-focused, exposure-focused) to decide how best to organize in the future.
Learning the natural history of disease and the prevention and treatment landscape through subdiscipline training is key for asking meaningful questions and making appropriate study design decisions. However, we encourage epidemiologists, epidemiology departments, and professional epidemiologic organizations to work together to foster an exchange of ideas across epidemiologic subdisciplines. As we break silos within epidemiology, we should also collaborate with colleagues in other quantitative fields to break bigger silos across disciplines. This effort is especially crucial now, during the ongoing pandemic, when the propensity for siloing and isolation is particularly high, given that there are few opportunities for in-person interactions and networking. Therefore, we strongly recommend that as an epidemiologic community we prioritize taking the steps outlined above and have an ongoing conversation on how to increase connections so that we may continue to learn from one another, develop new ideas, and advance the fields of epidemiology and public health.
ACKNOWLEDGMENTS
Author affiliations: Department of Epidemiology, Gillings School of Global Public Health, University of North Carolina at Chapel Hill, Chapel Hill, North Carolina, United States (Shahar Shmuel, Jennifer L. Lund); Center for Real-World Effectiveness and Safety of Therapeutics, Perelman School of Medicine, University of Pennsylvania, Philadelphia, Pennsylvania, United States (Charles E. Leonard); Division of Pharmacoepidemiology and Pharmacoeconomics, Department of Medicine, Brigham and Women’s Hospital and Harvard Medical School, Boston, Massachusetts, United States (Katsiaryna Bykov); Department of Medicine, McGill University, Montreal, Quebec, Canada (Kristian B. Filion); Department of Epidemiology, Biostatistics, and Occupational Health, McGill University, Montreal, Quebec, Canada (Kristian B. Filion); and Department of Epidemiology, Fielding School of Public Health, University of California, Los Angeles, California, United States (Marissa J. Seamans).
This work was supported by the following funding sources. S.S.’s contribution was supported by the PhRMA Foundation Postdoctoral Fellowship in Health Outcomes. C.E.L.’s contribution was supported by funding from the National Institute on Aging (grant R01 AG060975). K.B.’s contribution was supported by funding from the National Institute on Aging (grant K01 AG068365) and Agency for Healthcare Research and Quality (grant R01 HS027623). K.B.F. is supported by a senior salary support award from the Fonds de recherche du Québec – santé (Quebec Foundation for Research – Health) and a William Dawson Scholar award from McGill University. J.L.L.’s contribution was supported by funding from the Patient-Centered Outcomes Research Institute (grant ME 2017C3-9337).
This commentary was inspired by a symposium entitled “Recent Advances in Pharmacoepidemiologic Study Design: Opportunities for Collaboration and Dissemination” that the authors presented at the Society for Epidemiologic Research Annual Meeting (online), June 22–25, 2021.
The views expressed in this article are those of the authors and do not necessarily represent the official position of their employers and funding agencies.
S.S. was a consultant for CERobs Consulting, LLC, on projects unrelated to the submitted work. She is currently a full-time employee at Pfizer Inc. The initial manuscript draft was completed prior to her employment at Pfizer Inc. C.E.L. is an Executive Committee Member of the University of Pennsylvania’s Center for Real-World Effectiveness and Safety of Therapeutics. The Center receives funds from Pfizer and Sanofi to support the education of trainees. C.E.L. recently received honoraria from the Canadian Institutes of Health Research, University of Massachusetts, University of Florida, the American College of Clinical Pharmacy Foundation, and the Consortium for Medical Marijuana Clinical Outcomes Research. C.E.L. receives support for conference travel from John Wiley & Sons Inc. C.E.L. is a Special Government Employee of the US Food and Drug Administration. C.E.L. consults for the Reagan-Udall Foundation for the FDA. C.E.L.’s spouse is employed by Merck; neither she nor C.E.L. hold stock in the company. K.B. is a consultant to Alosa Health on projects unrelated to the submitted work. J.L.L. receives salary support to UNC from AbbVie, Inc. and F. Hoffmann-La Roche AG. J.L.L.’s spouse was formerly employed by and owned stock in GlaxoSmithKline. The other authors report no conflicts.




