-
PDF
- Split View
-
Views
-
Cite
Cite
Jacqueline M Torres, Oleg Sofrygin, Kara E Rudolph, Mary N Haan, Rebeca Wong, M Maria Glymour, US Migration Status of Adult Children and Cognitive Decline Among Older Parents Who Remain in Mexico, American Journal of Epidemiology, Volume 189, Issue 8, August 2020, Pages 761–769, https://doi.org/10.1093/aje/kwz277
Close - Share Icon Share
Abstract
Low- and middle-income countries (LMICs) are experiencing rapid aging, a growing dementia burden, and relatively high rates of out-migration among working-age adults. Family member migration status may be a unique societal determinant of cognitive aging in LMIC settings. We aimed to evaluate the association between adult child US migration status and change in cognitive performance scores using data from the Mexican Health and Aging Study, a population-based, national-level cohort study of Mexico adults aged ≥50 years at baseline (2001), with 2-, 12-, and 14-year follow-up waves (2003, 2012, and 2015). Cognitive performance assessments were completed by 5,972 and 4,939 respondents at 11 years and 14 years of follow-up, respectively. For women, having an adult child in the United States was associated with steeper decline in verbal memory scores (e.g., for 9-year change in immediate verbal recall z score, marginal risk difference (RD) = –0.09 (95% confidence interval (CI): −0.16, −0.03); for delayed verbal recall z score, RD = –0.10 (95% CI: −0.17, −0.03)) and overall cognitive performance (for overall cognitive performance z score, RD = –0.04, 95% CI: −0.07, −0.00). There were mostly null associations for men. To our knowledge, this is the first study to have evaluated the association between family member migration status and cognitive decline; future work should be extended to other LMICs facing population aging.
Abbreviations
- CI
confidence interval
- LMICs
low- and middle-income countries
- MHAS
Mexican Health and Aging Study
- RD
risk difference
- SD
standard deviation
It is expected that by 2050, 131.5 million persons will be living with dementia, 68% of whom will reside in low- and middle-income countries (LMICs) (1). Dementia burden is increasing more rapidly in LMICs than in wealthier nations (2). Population-level contributors to cognitive aging in LMICs should be a research priority.
Family member out-migration may be one population-level determinant of cognitive outcomes for older adults in LMICs. Emigrants from LMICs constitute a large proportion of migrants worldwide and are primarily working-age adults (3). For older adults who remain in LMICs, family member out-migration may constrict opportunities for social engagement and increase social isolation. In some studies (4), but not all (5, 6), social engagement with family and community members has been linked to lower risk of dementia (7–9), better cognitive function (10–12), and a lower rate of cognitive decline (13). Conversely, social isolation and related feelings of loneliness have been linked to faster rates of cognitive decline (13, 14).
Family member out-migration may also influence cognitive outcomes through health-related pathways, including by increasing risk of elevated levels of depressive symptoms (15–18). However, some studies have found null or even protective associations between having an adult child migrant and depressive symptoms (18, 19), self-rated health (20), and physical functioning (20, 21)—which could, in turn, have positive impacts on cognitive aging. While authors of 2 prior studies (22, 23) reported null associations between the migration status of adult children and level of cognitive performance, no prior studies, to our knowledge, have evaluated associations with change in cognitive performance over time.
Estimating the associations between family member migration status and cognitive change presents substantial methodological challenges, because persons with migrant family members probably differ from those who do not with regard to myriad contextual and family-level factors (24–26). Decisions about migration are generally partially informed by family-level economic needs arising from a lack of employment prospects in the sending community and/or economic shocks related to population-level (e.g., natural disasters) or family-level (e.g., needs for expensive medical treatment) crises (26, 27). These economic needs are often balanced against the family’s caregiving needs, including care of elderly parents, as well as the availability of siblings to provide care (24, 28). Economic and caregiving considerations intersect with community and personal migration histories, including older parents’ past experience with US migration, to inform migration decisions (25, 29, 30). Prior family and community migration history may lower the barriers to migration by offering information about the migration process and social connections in destination communities (25, 29, 30).
All of these factors—economic needs, prior health and caregiving, and past migration experiences—may also contribute to late-life cognitive performance and decline, confounding the relationship between adult child migration status and older parents’ cognitive outcomes. Previous studies have evaluated marginal associations between adult child migration status and older parents’ health outcomes using propensity score matching (20, 22, 24). While this approach may balance observed time-invariant covariates across persons with and without an adult child migrant, it relies on correctly specifying the model used to estimate the propensity to have an adult child migrant.
In the present study, we leveraged data from a population-based prospective study of mid- and late-life Mexican adults aged ≥50 years who were followed over a 14-year period to evaluate the association between having an adult child migrant and cognitive decline. Mexico is a middle-income country experiencing rapid aging (31), a growing dementia burden (32), and historically high rates of out-migration, primarily to the United States (33, 34). Departing from prior studies, we used a doubly robust estimation approach that reduces reliance on the correct specification of a single model (35–37), correctly accounts for time-varying confounders given time-varying exposures, and addresses respondent attrition in the cohort.
METHODS
Data
Data came from 4 waves of the Mexican Health and Aging Study (MHAS) a national cohort study of Mexican adults (38). The MHAS selected households with adults aged ≥50 years who had previously been included in a nationally representative survey, the 2000 Mexican Employment Survey. Within each household, a target respondent and spouse/cohabitating partner (regardless of age) were interviewed; proxy informants answered for older adults who could not respond on their own. Response rates were 91.8% in 2001, 93.3% in 2003, 88.1% in 2012, and 88.3% in 2015.
The MHAS surveyed 15,186 respondents at baseline. Respondents who had proxy informants, had no living children at baseline, or were spouse respondents aged <50 years were excluded from the primary analytical sample. Respondents aged ≥50 years at baseline with at least 1 living child who completed direct interviews all provided information for the analyses, although final estimates were limited to respondents with at least 1 living child who completed direct interviews at the 2-year follow-up and the 9- or 12-year follow-up, respectively (see Web Figure 1, available at https://dbpia.nl.go.kr/aje).
Exposure
Adult child US migration status was constructed from a household roster that solicited the location of each of the respondents’ nonresident children in each survey wave. We focused on adult child migration status at baseline and the 2-year follow-up (2001 and 2003), given that these waves preceded the outcomes of 9- and 12-year cognitive decline. Specifically, we evaluated outcomes under contrasting exposures of 1) having an adult child in the United States in both the 2001 and 2003 waves and 2) having no adult children in the United States in either study wave. There was relatively little change in adult child migration status between these 2 waves: Of those respondents who had an adult child in the United States at the 2-year follow-up, about 80% had also had an adult child in the United States at baseline (992 (81%) of 1,225 women and 753 (79%) of 953 men).
Outcomes
Cognitive performance was measured with the screening component of the Cross-Cultural Cognitive Examination (39), which was designed for the diagnosis of dementia in the community by nonmedical personnel and to be independent of the effects of literacy. In all waves of the MHAS, respondents completed immediate and delayed verbal recall of an 8-word list, visual scanning, and complex figure copy and recall tasks. In 2003, a task measuring orientation was added. In 2012 and 2015, numeracy and animal naming tasks were also included (see Web Table 1 for further details on cognitive tasks and Web Table 2 for correlation coefficients across cognitive tasks).
Our primary analyses focused on change in the immediate and delayed verbal recall tasks (transformed as z scores), given that these tasks remained consistent across study waves and correspond to verbal recall tasks used in other population-based studies (e.g., the US Health and Retirement Study). We additionally evaluated a global cognitive performance score that was the average of the z scores of all available cognitive tasks in a given wave. We generated z scores utilizing the mean values and standard deviations for the first wave in which each respective cognitive performance measure was administered.
An initial evaluation of descriptive results suggested an unanticipated improvement in overall cognitive performance scores between the 2003 and 2012 follow-up waves, driven by improvements in performance on complex figure copy and complex figure recall tasks. We therefore also estimated associations with an alternative cognitive performance score that excluded these tasks.
We created measures of both 9- and 12-year change in immediate and delayed verbal recall and overall cognitive performance scores by subtracting scores at the 2003 visit (2 years after baseline) from scores at the 2012 and 2015 visits, respectively. Our a priori assessment was that outcomes reflecting change in cognitive performance from the baseline (2001) assessment would have presented substantial challenges in terms of 1) teasing apart the potentially reciprocal associations between adult child migration status and cognitive performance and 2) correctly specifying time-varying confounders. We nevertheless report the results of post-hoc analyses that evaluated change from baseline cognitive assessments (see further details below).
Covariates
All models stratified the results by sex, given prior evidence of sex differences in the association between adult child migration status and health outcomes (18, 21). Time-invariant covariates included baseline age, indicators of early-life socioeconomic status and health, lifetime occupational status, and a binary indicator for whether any of the respondents’ siblings had ever migrated to the United States. Prior personal US migration was included for men (few women in the cohort were US migrants). Time-varying covariates included measures of physical functioning, depressive symptoms, number of self-reported chronic diseases, past-year health-care utilization, health insurance coverage, monthly income, number of household assets, employment status, marital status, total numbers of living children and grandchildren, presence of adult children in the household, and the availability of social and instrumental support within the community. Further details on select covariates are given in Web Table 3.
Analytical strategy
We used longitudinal targeted maximum likelihood estimation, a doubly robust semiparametric approach (35, 36), to estimate the associations of having an adult child migrant at baseline and at the 2-year follow-up with subsequent change in cognitive performance scores. Directed acyclic graphs guiding the analyses are presented in Web Figures 2 and 3. We first generated estimates of average change in cognitive performance scores under counterfactual exposure regimes of 1) having an adult child in the United States at baseline and the 2-year follow-up and 2) not having an adult child in the United States at either of these time points, conditional only on inclusion in the follow-up survey. We subsequently generated estimates under the same counterfactual exposure regimes, conditional on inclusion in the follow-up survey, time-invariant covariates, and lagged (i.e., baseline and 2-year follow-up) time-varying covariates.
The targeted maximum likelihood estimation algorithm incorporated 1) inverse probability of treatment weights generated from separate models of exposure (i.e., having an adult child in the United States) at each wave, conditional on time-invariant covariates, lagged time-varying covariates (i.e., measured at the prior wave), and inclusion in the survey wave, and 2) inverse probability of attrition weights to account for respondent attrition, generated from models of inclusion in the survey conditional on time-invariant covariates and lagged (i.e., measured at the prior wave) time-varying covariates, including lagged measures of having an adult child in the United States.
Models for generating inverse probability of attrition weights were fitted separately for attrition due to death, loss to follow-up, and having one’s questionnaire answered by a proxy informant or no longer having an adult child.
All models were fitted data-adaptively by means of the gradient boosting machine algorithm, with 10-fold cross-validation (40, 41), using the stremr (42) and sl3 (43) packages for R (R Foundation for Statistical Computing, Vienna, Austria). Multiple imputation was used to address missing data with the Amelia package for R (44). Ten multiply imputed data sets were created for the baseline wave, and mean values from multiply imputed baseline models were incorporated into the multiple imputation of time-varying measures at successive follow-up waves. Estimates were combined using Rubin’s rules (45).
Sensitivity analyses
Further details on sensitivity analyses are provided in the Web Appendix. Briefly, we first evaluated potential bias induced by excluding respondents with proxy informants from our main analyses (46). We refitted our models including respondents whose surveys were answered by proxy informants, assigning these respondents cognitive performance scores based on proxy-reported cognitive information. We varied these assigned scores under a range of scenarios and evaluated deviations in the estimated associations from those reported in our primary analyses (Web Tables 4 and 5).
Second, we reestimated associations between baseline adult child migration status and cognitive decline from baseline through the 14-year follow-up using linear mixed models. Correct specification of time-varying exposures and time-varying confounders is not straightforward in the mixed-model context. Moreover, the targeted maximum likelihood estimation approach has additional advantages of being doubly robust, being semiparametric, and allowing for data-adaptive model-fitting, which is why we preferred it for our primary analyses (36). However, prior studies have demonstrated that associations with cognitive change scores measured over 2 time points may not replicate when decline is captured over 3 or more time points, as with the estimates from the linear mixed model (47).
Baseline Characteristics of Respondents With At Least 1 Living Child, Mexican Health and Aging Study, 2001–2015
| Characteristic . | Women (n = 6,374) . | Men (n = 5,432) . | ||||
|---|---|---|---|---|---|---|
| No. . | % . | Mean (SD) . | No. . | % . | Mean (SD) . | |
| Cognitive outcomes | ||||||
| Immediate verbal recalla | 4.76 (1.23) | 4.59 (1.27) | ||||
| Delayed verbal recalla | 5.17 (1.86) | 4.87 (1.84) | ||||
| Overall cognitive performanceb | 35.80 (16.94) | 38.32 (17.04) | ||||
| Exposures | ||||||
| ≥1 child living in United States in 2001 | 1,532 | 24.0 | 1,237 | 22.8 | ||
| ≥1 child living in United States in 2001 and 2003c | 992 | 18.1 | 753 | 17.2 | ||
| Demographic characteristics | ||||||
| Age, years | 61.73 (9.22) | 62.17 (9.42) | ||||
| Urban residence | 4,323 | 67.8 | 3,546 | 65.3 | ||
| Residence in high US out-migration state | 1,779 | 27.9 | 1,488 | 27.4 | ||
| US migrant | 209 | 3.3 | 896 | 16.5 | ||
| Married | 3,795 | 59.5 | 4,658 | 85.8 | ||
| Life-course socioeconomic status | ||||||
| Paternal education, years | 1.77 (0.91) | 1.73 (0.90) | ||||
| Respondent education, years | 3.99 (3.92) | 5.05 (4.83) | ||||
| No sanitation facilities during childhood | 4,175 | 65.5 | 3,753 | 69.1 | ||
| Total monthly household income, pesos | 4,510 (53,384) | 6,083 (65,977) | ||||
| Total household net worth, pesos | 362,000 (697,264) | 429,593 (889,858) | ||||
| Currently employed outside the home | 1,493 | 23.4 | 3,787 | 69.7 | ||
| No. of material items in householdd | 4.36 (1.69) | 4.35 (1.70) | ||||
| Self-rated economic statuse | 1.06 (0.66) | 1.07 (0.68) | ||||
| Health and health-care utilization | ||||||
| Major illness or injury during childhood | 717 | 11.3 | 609 | 11.2 | ||
| Health insurance coverage | 4,101 | 64.3 | 3,316 | 61.1 | ||
| Past-year medical visit | 4,578 | 71.8 | 3,083 | 56.8 | ||
| Lower-body functional limitationsf | 3.07 (2.46) | 2.11 (2.32) | ||||
| Elevated level of depressive symptomsg | 3,004 | 47.1 | 2,060 | 37.9 | ||
| Chronic health conditionsh | 0.80 (0.81) | 0.58 (0.78) | ||||
| Family and community | ||||||
| Sibling living in United States | 1,470 | 23.1 | 1,392 | 25.6 | ||
| ≥1 child living in a different city in Mexico | 2,329 | 36.5 | 1,868 | 34.4 | ||
| ≥1 adult child living in the household | 4,512 | 70.8 | 3,953 | 72.8 | ||
| No. of living children | 5.57 (2.95) | 5.59 (2.98) | ||||
| No. of living grandchildren | 11.44 (10 .72) | 9.41 (10.23) | ||||
| Can count on neighbors/friends for help with daily activities | 4,092 | 64.2 | 3,482 | 64.1 | ||
| Characteristic . | Women (n = 6,374) . | Men (n = 5,432) . | ||||
|---|---|---|---|---|---|---|
| No. . | % . | Mean (SD) . | No. . | % . | Mean (SD) . | |
| Cognitive outcomes | ||||||
| Immediate verbal recalla | 4.76 (1.23) | 4.59 (1.27) | ||||
| Delayed verbal recalla | 5.17 (1.86) | 4.87 (1.84) | ||||
| Overall cognitive performanceb | 35.80 (16.94) | 38.32 (17.04) | ||||
| Exposures | ||||||
| ≥1 child living in United States in 2001 | 1,532 | 24.0 | 1,237 | 22.8 | ||
| ≥1 child living in United States in 2001 and 2003c | 992 | 18.1 | 753 | 17.2 | ||
| Demographic characteristics | ||||||
| Age, years | 61.73 (9.22) | 62.17 (9.42) | ||||
| Urban residence | 4,323 | 67.8 | 3,546 | 65.3 | ||
| Residence in high US out-migration state | 1,779 | 27.9 | 1,488 | 27.4 | ||
| US migrant | 209 | 3.3 | 896 | 16.5 | ||
| Married | 3,795 | 59.5 | 4,658 | 85.8 | ||
| Life-course socioeconomic status | ||||||
| Paternal education, years | 1.77 (0.91) | 1.73 (0.90) | ||||
| Respondent education, years | 3.99 (3.92) | 5.05 (4.83) | ||||
| No sanitation facilities during childhood | 4,175 | 65.5 | 3,753 | 69.1 | ||
| Total monthly household income, pesos | 4,510 (53,384) | 6,083 (65,977) | ||||
| Total household net worth, pesos | 362,000 (697,264) | 429,593 (889,858) | ||||
| Currently employed outside the home | 1,493 | 23.4 | 3,787 | 69.7 | ||
| No. of material items in householdd | 4.36 (1.69) | 4.35 (1.70) | ||||
| Self-rated economic statuse | 1.06 (0.66) | 1.07 (0.68) | ||||
| Health and health-care utilization | ||||||
| Major illness or injury during childhood | 717 | 11.3 | 609 | 11.2 | ||
| Health insurance coverage | 4,101 | 64.3 | 3,316 | 61.1 | ||
| Past-year medical visit | 4,578 | 71.8 | 3,083 | 56.8 | ||
| Lower-body functional limitationsf | 3.07 (2.46) | 2.11 (2.32) | ||||
| Elevated level of depressive symptomsg | 3,004 | 47.1 | 2,060 | 37.9 | ||
| Chronic health conditionsh | 0.80 (0.81) | 0.58 (0.78) | ||||
| Family and community | ||||||
| Sibling living in United States | 1,470 | 23.1 | 1,392 | 25.6 | ||
| ≥1 child living in a different city in Mexico | 2,329 | 36.5 | 1,868 | 34.4 | ||
| ≥1 adult child living in the household | 4,512 | 70.8 | 3,953 | 72.8 | ||
| No. of living children | 5.57 (2.95) | 5.59 (2.98) | ||||
| No. of living grandchildren | 11.44 (10 .72) | 9.41 (10.23) | ||||
| Can count on neighbors/friends for help with daily activities | 4,092 | 64.2 | 3,482 | 64.1 | ||
Abbreviation: SD, standard deviation.
a Possible range, 0–8 words.
b Possible range, 0–80.
c Calculated for persons remaining in the analytical sample in 2003 (5,490 women and 4,373 men).
d Possible range, 0–6 possible household items.
e Possible range, 0–4.
f Possible range, 0–8 lower-body functional limitations.
g Reporting ≥5 (vs. <5) past-week depressive symptoms.
h Possible range, 0–6 chronic conditions.
Baseline Characteristics of Respondents With At Least 1 Living Child, Mexican Health and Aging Study, 2001–2015
| Characteristic . | Women (n = 6,374) . | Men (n = 5,432) . | ||||
|---|---|---|---|---|---|---|
| No. . | % . | Mean (SD) . | No. . | % . | Mean (SD) . | |
| Cognitive outcomes | ||||||
| Immediate verbal recalla | 4.76 (1.23) | 4.59 (1.27) | ||||
| Delayed verbal recalla | 5.17 (1.86) | 4.87 (1.84) | ||||
| Overall cognitive performanceb | 35.80 (16.94) | 38.32 (17.04) | ||||
| Exposures | ||||||
| ≥1 child living in United States in 2001 | 1,532 | 24.0 | 1,237 | 22.8 | ||
| ≥1 child living in United States in 2001 and 2003c | 992 | 18.1 | 753 | 17.2 | ||
| Demographic characteristics | ||||||
| Age, years | 61.73 (9.22) | 62.17 (9.42) | ||||
| Urban residence | 4,323 | 67.8 | 3,546 | 65.3 | ||
| Residence in high US out-migration state | 1,779 | 27.9 | 1,488 | 27.4 | ||
| US migrant | 209 | 3.3 | 896 | 16.5 | ||
| Married | 3,795 | 59.5 | 4,658 | 85.8 | ||
| Life-course socioeconomic status | ||||||
| Paternal education, years | 1.77 (0.91) | 1.73 (0.90) | ||||
| Respondent education, years | 3.99 (3.92) | 5.05 (4.83) | ||||
| No sanitation facilities during childhood | 4,175 | 65.5 | 3,753 | 69.1 | ||
| Total monthly household income, pesos | 4,510 (53,384) | 6,083 (65,977) | ||||
| Total household net worth, pesos | 362,000 (697,264) | 429,593 (889,858) | ||||
| Currently employed outside the home | 1,493 | 23.4 | 3,787 | 69.7 | ||
| No. of material items in householdd | 4.36 (1.69) | 4.35 (1.70) | ||||
| Self-rated economic statuse | 1.06 (0.66) | 1.07 (0.68) | ||||
| Health and health-care utilization | ||||||
| Major illness or injury during childhood | 717 | 11.3 | 609 | 11.2 | ||
| Health insurance coverage | 4,101 | 64.3 | 3,316 | 61.1 | ||
| Past-year medical visit | 4,578 | 71.8 | 3,083 | 56.8 | ||
| Lower-body functional limitationsf | 3.07 (2.46) | 2.11 (2.32) | ||||
| Elevated level of depressive symptomsg | 3,004 | 47.1 | 2,060 | 37.9 | ||
| Chronic health conditionsh | 0.80 (0.81) | 0.58 (0.78) | ||||
| Family and community | ||||||
| Sibling living in United States | 1,470 | 23.1 | 1,392 | 25.6 | ||
| ≥1 child living in a different city in Mexico | 2,329 | 36.5 | 1,868 | 34.4 | ||
| ≥1 adult child living in the household | 4,512 | 70.8 | 3,953 | 72.8 | ||
| No. of living children | 5.57 (2.95) | 5.59 (2.98) | ||||
| No. of living grandchildren | 11.44 (10 .72) | 9.41 (10.23) | ||||
| Can count on neighbors/friends for help with daily activities | 4,092 | 64.2 | 3,482 | 64.1 | ||
| Characteristic . | Women (n = 6,374) . | Men (n = 5,432) . | ||||
|---|---|---|---|---|---|---|
| No. . | % . | Mean (SD) . | No. . | % . | Mean (SD) . | |
| Cognitive outcomes | ||||||
| Immediate verbal recalla | 4.76 (1.23) | 4.59 (1.27) | ||||
| Delayed verbal recalla | 5.17 (1.86) | 4.87 (1.84) | ||||
| Overall cognitive performanceb | 35.80 (16.94) | 38.32 (17.04) | ||||
| Exposures | ||||||
| ≥1 child living in United States in 2001 | 1,532 | 24.0 | 1,237 | 22.8 | ||
| ≥1 child living in United States in 2001 and 2003c | 992 | 18.1 | 753 | 17.2 | ||
| Demographic characteristics | ||||||
| Age, years | 61.73 (9.22) | 62.17 (9.42) | ||||
| Urban residence | 4,323 | 67.8 | 3,546 | 65.3 | ||
| Residence in high US out-migration state | 1,779 | 27.9 | 1,488 | 27.4 | ||
| US migrant | 209 | 3.3 | 896 | 16.5 | ||
| Married | 3,795 | 59.5 | 4,658 | 85.8 | ||
| Life-course socioeconomic status | ||||||
| Paternal education, years | 1.77 (0.91) | 1.73 (0.90) | ||||
| Respondent education, years | 3.99 (3.92) | 5.05 (4.83) | ||||
| No sanitation facilities during childhood | 4,175 | 65.5 | 3,753 | 69.1 | ||
| Total monthly household income, pesos | 4,510 (53,384) | 6,083 (65,977) | ||||
| Total household net worth, pesos | 362,000 (697,264) | 429,593 (889,858) | ||||
| Currently employed outside the home | 1,493 | 23.4 | 3,787 | 69.7 | ||
| No. of material items in householdd | 4.36 (1.69) | 4.35 (1.70) | ||||
| Self-rated economic statuse | 1.06 (0.66) | 1.07 (0.68) | ||||
| Health and health-care utilization | ||||||
| Major illness or injury during childhood | 717 | 11.3 | 609 | 11.2 | ||
| Health insurance coverage | 4,101 | 64.3 | 3,316 | 61.1 | ||
| Past-year medical visit | 4,578 | 71.8 | 3,083 | 56.8 | ||
| Lower-body functional limitationsf | 3.07 (2.46) | 2.11 (2.32) | ||||
| Elevated level of depressive symptomsg | 3,004 | 47.1 | 2,060 | 37.9 | ||
| Chronic health conditionsh | 0.80 (0.81) | 0.58 (0.78) | ||||
| Family and community | ||||||
| Sibling living in United States | 1,470 | 23.1 | 1,392 | 25.6 | ||
| ≥1 child living in a different city in Mexico | 2,329 | 36.5 | 1,868 | 34.4 | ||
| ≥1 adult child living in the household | 4,512 | 70.8 | 3,953 | 72.8 | ||
| No. of living children | 5.57 (2.95) | 5.59 (2.98) | ||||
| No. of living grandchildren | 11.44 (10 .72) | 9.41 (10.23) | ||||
| Can count on neighbors/friends for help with daily activities | 4,092 | 64.2 | 3,482 | 64.1 | ||
Abbreviation: SD, standard deviation.
a Possible range, 0–8 words.
b Possible range, 0–80.
c Calculated for persons remaining in the analytical sample in 2003 (5,490 women and 4,373 men).
d Possible range, 0–6 possible household items.
e Possible range, 0–4.
f Possible range, 0–8 lower-body functional limitations.
g Reporting ≥5 (vs. <5) past-week depressive symptoms.
h Possible range, 0–6 chronic conditions.
Marginal Risk Differences in Average Change in Cognitive Performance z Scores for Adults Aged ≥50 Years With At Least 1 Adult Migrant Child at Baseline and 2-Year Follow-up Versus No Migrant Children, by Sex, Mexican Health and Aging Study, 2001–2015
| Cognitive Outcome . | Womena . | Menb . | ||
|---|---|---|---|---|
| Marginal RD . | 95% CI . | Marginal RD . | 95% CI . | |
| 9-year change | ||||
| Immediate verbal recall | −0.09 | −0.156, −0.027 | 0.01 | −0.062, 0.072 |
| Delayed verbal recall | −0.10 | −0.165, −0.031 | −0.03 | −0.106, 0.046 |
| Global cognitive score | −0.04 | −0.068, −0.004 | −0.01 | −0.051, 0.034 |
| 12-year change | ||||
| Immediate verbal recall | −0.13 | −0.211, −0.055 | −0.04 | −0.102, 0.017 |
| Delayed verbal recall | −0.12 | −0.183, −0.047 | 0.02 | −0.049, 0.082 |
| Global cognitive score | −0.02 | −0.050, 0.011 | −0.01 | −0.036, 0.023 |
| Cognitive Outcome . | Womena . | Menb . | ||
|---|---|---|---|---|
| Marginal RD . | 95% CI . | Marginal RD . | 95% CI . | |
| 9-year change | ||||
| Immediate verbal recall | −0.09 | −0.156, −0.027 | 0.01 | −0.062, 0.072 |
| Delayed verbal recall | −0.10 | −0.165, −0.031 | −0.03 | −0.106, 0.046 |
| Global cognitive score | −0.04 | −0.068, −0.004 | −0.01 | −0.051, 0.034 |
| 12-year change | ||||
| Immediate verbal recall | −0.13 | −0.211, −0.055 | −0.04 | −0.102, 0.017 |
| Delayed verbal recall | −0.12 | −0.183, −0.047 | 0.02 | −0.049, 0.082 |
| Global cognitive score | −0.02 | −0.050, 0.011 | −0.01 | −0.036, 0.023 |
Abbreviations: CI, confidence interval; RD, risk difference.
an = 3,416 women included in estimates of 9-year change scores; n = 2,838 women included in estimates of 12-year change scores.
bn = 2,556 men included in estimates of 9-year change scores; n = 2,101 men included in estimates of 12-year change scores.
Marginal Risk Differences in Average Change in Cognitive Performance z Scores for Adults Aged ≥50 Years With At Least 1 Adult Migrant Child at Baseline and 2-Year Follow-up Versus No Migrant Children, by Sex, Mexican Health and Aging Study, 2001–2015
| Cognitive Outcome . | Womena . | Menb . | ||
|---|---|---|---|---|
| Marginal RD . | 95% CI . | Marginal RD . | 95% CI . | |
| 9-year change | ||||
| Immediate verbal recall | −0.09 | −0.156, −0.027 | 0.01 | −0.062, 0.072 |
| Delayed verbal recall | −0.10 | −0.165, −0.031 | −0.03 | −0.106, 0.046 |
| Global cognitive score | −0.04 | −0.068, −0.004 | −0.01 | −0.051, 0.034 |
| 12-year change | ||||
| Immediate verbal recall | −0.13 | −0.211, −0.055 | −0.04 | −0.102, 0.017 |
| Delayed verbal recall | −0.12 | −0.183, −0.047 | 0.02 | −0.049, 0.082 |
| Global cognitive score | −0.02 | −0.050, 0.011 | −0.01 | −0.036, 0.023 |
| Cognitive Outcome . | Womena . | Menb . | ||
|---|---|---|---|---|
| Marginal RD . | 95% CI . | Marginal RD . | 95% CI . | |
| 9-year change | ||||
| Immediate verbal recall | −0.09 | −0.156, −0.027 | 0.01 | −0.062, 0.072 |
| Delayed verbal recall | −0.10 | −0.165, −0.031 | −0.03 | −0.106, 0.046 |
| Global cognitive score | −0.04 | −0.068, −0.004 | −0.01 | −0.051, 0.034 |
| 12-year change | ||||
| Immediate verbal recall | −0.13 | −0.211, −0.055 | −0.04 | −0.102, 0.017 |
| Delayed verbal recall | −0.12 | −0.183, −0.047 | 0.02 | −0.049, 0.082 |
| Global cognitive score | −0.02 | −0.050, 0.011 | −0.01 | −0.036, 0.023 |
Abbreviations: CI, confidence interval; RD, risk difference.
an = 3,416 women included in estimates of 9-year change scores; n = 2,838 women included in estimates of 12-year change scores.
bn = 2,556 men included in estimates of 9-year change scores; n = 2,101 men included in estimates of 12-year change scores.
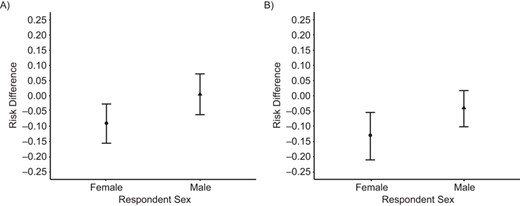
Marginal risk differences in 9-year (A) and 12-year (B) change in immediate verbal recall z scores for Mexican adults aged ≥50 years with an adult child in the United States as compared with their counterparts with no adult children in the United States, Mexican Health and Aging Study, 2001–2015.
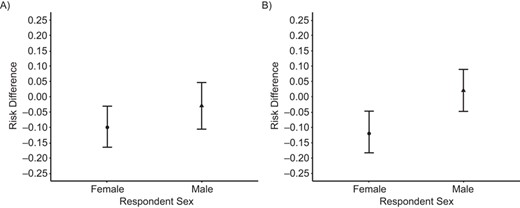
Marginal risk differences in 9-year (A) and 12-year (B) change in delayed verbal recall scores for older Mexican adults aged ≥50 years with an adult child in the United States as compared with their counterparts with no adult children in the United States, Mexican Health and Aging Study, 2001–2015.
RESULTS
Descriptive findings
A total of 11,806 respondents (6,374 women, 5,432 men) aged ≥50 years at baseline with at least 1 living child contributed information to models used to account for respondent attrition from the sample. A total of 5,972 respondents (3,416 women, 2,556 men) were included in the analytical sample for estimates of 9-year change (i.e., between 2- and 12-year follow-up) in cognitive scores; 4,939 respondents (2,838 women, 2,101 men) were included in the analytical sample for estimates of 12-year change (i.e., between 2- and 14-year follow-up) in cognitive scores.
On average, respondents were approximately 62 years of age at baseline (2001). About 24% of women and 23% of men had an adult child in the United States at baseline; of those remaining in the analytical sample by 2003, 18% of women and 17% of men had an adult child in the United States at both baseline and the 2-year follow-up (Table 1). Women had average baseline immediate verbal memory scores of 4.8 words remembered and delayed verbal memory scores of 5.2 words remembered; men had scores of 4.6 and 4.9 words remembered on immediate and delayed verbal recall scores, respectively.
The mean 9-year change in immediate verbal recall z score was −0.02 for both men and women (standard deviation (SD), 1.09 for women and 1.14 for men). The average 9-year change in delayed verbal recall z score was −0.24 (SD, 1.18) for women and −0.35 (SD, 1.45) for men (Web Table 6).
Associations between having an adult child migrant and change in cognitive scores
For women, unadjusted estimates conditional only on inclusion in the survey (Web Table 7) were consistent (albeit of larger magnitude) with adjusted estimates that were also conditional on covariates; we therefore focus on the adjusted estimates. Women who had an adult child in the United States at both baseline and the 2-year follow-up averaged steeper 9-year declines in immediate (for z score, marginal risk difference (RD) = –0.09, 95% confidence interval (CI): −0.16, −0.03) and delayed (RD = –0.10, 95% CI: −0.17, −0.03) verbal recall scores than those who had no adult children in the United States during the same period (Table 2, Figure 1). Similar associations were observed between having an adult child in the United States and 12-year decline in immediate (RD = –0.13, 95% CI: −0.21, −0.06) and delayed (RD = –0.12, 95% CI: −0.18, −0.05) verbal recall among women (Table 2, Figure 2). Estimates presented as the change in the absolute number of words remembered are shown in Web Table 8.
For women, having an adult child in the United States was not associated with steeper average 9-year decline in overall cognitive performance z score (RD = –0.04, 95% CI: −0.068, −0.004); this association was no longer apparent for the outcome of 12-year decline in overall cognitive performance score. Associations were of larger magnitude when using an alternative measure that excluded complex figure copy and recall task scores (e.g., for 9-year change, RD = –0.07, 95% CI: −0.11, −0.02) (Web Table 9).
Among men, having an adult child in the United States was associated with steeper change in delayed verbal recall (but not immediate verbal recall or overall cognitive performance) scores in estimates that were conditional only on inclusion in the analytical sample (for 9-year change, RD = –0.14 (95% CI: −0.24, −0.05); for 12-year change, RD = –0.15 (95% CI: −0.24, −0.07)) (Web Table 7). However, in estimates conditional on the full set of covariates, there were fully null associations between having an adult child in the United States and 9- or 12-year change in verbal recall scores and overall cognitive performance scores (Table 2, Figures 1 and 2).
There were generally similar associations between having an adult child in the United States and change in cognitive performance scores in sensitivity analyses that included proxy informants (Web Table 10).
Generally consistent with the primary analysis, estimates using linear mixed models indicated that, compared with women with no adult child in the United States at baseline, women with an adult child in the United States were estimated to have a steeper decline in immediate (β = –0.08, 95% CI: −0.13, −0.03) and delayed (β = −0.10, 95% CI: −0.16, −0.04) verbal recall z scores but not in the rate of change in overall cognitive performance scores in fully adjusted models. For men, having an adult child in the United States at baseline was associated with steeper decline in delayed verbal recall z scores (in fully adjusted models, β = –0.13, 95% CI: −0.20, −0.05) but not with immediate verbal recall or overall cognitive performance scores (Web Tables 11–13).
DISCUSSION
The growing burden of dementia in LMICs has lent increased urgency to the need to identify population drivers of cognitive outcomes in these settings. We evaluated the US migration status of adult children as one potential population-level contributor to cognitive aging in a cohort of older Mexican adults followed over a 14-year period. To our knowledge, this is the first study to have evaluated the relationship between adult child migration status and cognitive decline. Departing from most prior studies of adult child migration status and health, we evaluated longitudinal associations with a doubly robust estimation approach that accounted for respondent attrition.
For women in the cohort, we found that having an adult child in the United States was associated with steeper decline in immediate and delayed verbal recall scores and, to a lesser extent, overall cognitive performance scores. In contrast, we found fully null associations for men in our primary analyses. Analyses using an alternative linear mixed-model approach suggested that baseline adult child US migration status was also associated with steeper decline in delayed verbal memory scores for men. This divergence may have been the result of bias due to sample attrition. However, the direction of the association is consistent with the estimate of 9-year change we observed in primary analyses—and results were similar in analyses that used targeted maximum likelihood estimation but were conditional only on inclusion in the survey and not on covariates.
More consistent associations between having an adult child in the United States and steeper decline in cognitive performance scores for women could be explained by the potential influence of adult child out-migration on other psychosocial stressors, such as reduced social engagement, increased loneliness, and elevated levels of depressive symptoms, which have been linked to cognitive decline in prior research (10, 13, 14).
There are a number of other potential explanations for differences by sex. At baseline, men in the cohort were more likely to be married, to have an adult child living in the household, and to be working. More robust family networks may have helped protect men against the potentially adverse impacts of adult child out-migration on social engagement or psychological well-being. Continued work outside the home may have meant that men were more likely to be socially and/or cognitively engaged through their work lives, such that shifts in family dynamics may have been less impactful for cognitive outcomes in men than in women.
Limitations and strengths
These results should be interpreted in light of a number of limitations. First, the causal interpretation of the estimates hinges on a set of additional assumptions that may be unreasonable in this context. For example, unmeasured confounders, including local-level economic, environmental, or safety conditions (29, 48), as well as unmeasured dimensions of education (e.g., quality, literacy) (49, 50), could be driving both adult child out-migration and cognitive decline among older adults who remain in their home countries.
Second, scholars have recently drawn attention to the potential for effects of family member migration to be underestimated in population-based data sources, partly because of the fact that respondents may be unsure of family members’ whereabouts, including their migration status (51).
Third, findings from Mexico may not be generalizable to other LMICs—a large group of countries with substantial variability in patterns of aging and migration. Studies of adult child migration status and mental health among older parents in LMICs have uncovered mixed results across settings, including protective associations between adult child internal migration and older adults’ depressive symptoms in rural Thailand (19), adverse associations between internal migration and older adults’ mental health in rural China (52), and both adverse and null associations between adult child US migration and depressive symptoms among older adults in Mexico (16, 18). Differences could be driven by distinct methodological approaches but also by variability in associations between adult child migration status and mental health outcomes across settings, by type of migration, and by other factors (e.g., rural vs. urban residence). Future work on adult child migration and cognitive outcomes should explore the possibility of heterogeneous associations across and within settings using harmonized data and methods.
Conclusion
Despite the growing burden of dementia in LMICs, context-specific population drivers of cognitive aging are poorly understood. For older adults in LMICs, family member out-migration may be a unique societal determinant of cognitive outcomes. The present study is the first study, to our knowledge, to have evaluated associations between having an adult child living in the United States and cognitive decline. We used population-based data from Mexico and a doubly robust estimation strategy that accounted for the fact that family member migration decisions may be driven by sociodemographic factors and older adults’ prior health, both of which may have influenced subsequent cognitive decline. We found that for women, having an adult child migrant was associated with steeper decline in verbal memory scores, with largely null associations for men. In future research, investigators should evaluate potential mediators and modifiers of observed associations and extend these analyses to other LMIC settings facing rapid population aging.
ACKNOWLEDGMENTS
Author affiliations: Department of Epidemiology and Biostatistics, School of Medicine, University of California, San Francisco, San Francisco, California (Jacqueline M. Torres, Mary N. Haan, M. Maria Glymour); Division of Research, Kaiser Permanente, Oakland, California (Oleg Sofrygin); Department of Emergency Medicine, School of Medicine, University of California, Davis, Sacramento, California (Kara E. Rudolph); and Sealy Center on Aging, University of Texas Medical Branch, Galveston, Texas (Rebeca Wong).
The Mexican Health and Aging Study is funded by the National Institute on Aging, US National Institutes of Health (NIH; Bethesda, Maryland) (grant R01AG018016), and the Mexico National Institute of Statistics and Geography (Aguascalientes City, Aguascalientes, Mexico). J.M.T. was supported by the National Institute on Aging, NIH (grant K01AG056602). K.E.R. was supported by the National Institute on Drug Abuse, NIH (grant K99DA042127). O.S. was supported by the National Institute of Allergy and Infectious Diseases, NIH (grant R01AI074345-07). M.M.G. was supported by the National Institute on Aging, NIH (grant RF1AG05548601).
Conflict of interest: none declared.