-
PDF
- Split View
-
Views
-
Cite
Cite
Anita Wong, Claudia Cooper, Catherine J Evans, Mark James Rawle, Kate Walters, Simon Paul Conroy, Nathan Davies, Supporting older people through Hospital at Home care: a systematic review of patient, carer and healthcare professionals’ perspectives, Age and Ageing, Volume 54, Issue 2, February 2025, afaf033, https://doi.org/10.1093/ageing/afaf033
Close - Share Icon Share
Abstract
Hospital at Home provides hospital-level type care at home, both remote and face-to-face by a multidisciplinary team of healthcare professionals. In practice, various different models are employed, but we do not know what older people, their family carers (carers) and healthcare professionals think of what works best for them. This review aimed to describe the various Hospital at Home models and synthesise literature exploring patient, carer and staff perspectives of Hospital at Home care for older people.
A systematic review of UK studies. Medline, Embase and CINAHL and grey literature were searched from 1991 to 2024, using predetermined inclusion and exclusion criteria; data were extracted from included papers. Tabulation, thematic grouping and concept mapping of themes were used to narratively synthesise the literature.
Twenty studies met eligibility. Hospital at Home models included admission avoidance and early discharge. Studies were largely positive regarding Hospital at Home, with benefits including home familiarity, enabling person-centred care and shared decision-making and provision of family carer support. Challenges included staff accessibility, patient and carer anxieties regarding the safety of virtual wards, coordination across sectors and older people using technology.
Provision of holistic, accessible and continuous care for older people in Hospital at Home services facilitated patient and carer empowerment, dignity and autonomy. There are gaps in our understanding and evidence surrounding paid care workers and informal carers’ perspectives in UK settings, especially within rigorous Hospital at Home literature.
Key Points
Care provision in a familiar home environment with shared decision-making was valued by all stakeholders.
Older people, family carers and healthcare professionals’ experiences should be integrated in future research and evaluation.
Older people and their family carers reported mainly positive experiences with hospital at home.
Hospital at home were perceived by older people and family carers as a positive driver for patient independence and recovery.
Research potential for developing evidence-based support for family carers in hospital at home to alleviate carer burden.
Introduction
Better public health, medical advances and improved living conditions have led to longer lifespans [1]. In recent years, reports illustrate notable increases in potentially avoidable older adult hospitalisation and emergency admission, prolonged recovery time and inpatient stays, leading to worsening health outcomes such as delirium [2–4]. Older adults with frailty describe negative experiences in emergency care, with their needs not being met, potentially contributing to their reluctance to attend hospital in the first place [5]. This is perhaps in part due to the variable provision of gold-standard evidence-based care (comprehensive geriatric assessment) in acute hospital settings [6, 7].
The COVID-19 pandemic accelerated nationwide incorporation of teleconsultations—key to NHS England’s national Virtual Ward (VW) expansion programme which launched in 2022 [8–11]. NHS England defines VWs as technology-enabled, safe alternatives to hospital care, led by an appropriate clinical lead and a multidisciplinary team (MDT) [12, 13]. NHS’ shift of terminology from ‘Hospital at Home’ (HaH) to ‘Virtual Ward’ aimed to highlight the integration of digital technology [12, 13]. However, the Hospital at Home Society, British Geriatrics Society (BGS) and Royal College of Physicians have recently advocated for reverting back to using HaH terminology to better reflect the hospital-level care provided at home, align with global standards and reduce confusion amongst patients [14]. Although much of the recent literature refers to VWs, this paper follows BGS’s terminology recommendation for clarity and refers to all models as Hospital at Home (HaH).
The main HaH models include ‘Step-up’ hospital admission avoidance and ‘Step-down’ early hospital discharge, with subsequent home treatment and monitoring [15–17]. Studies show that these models offer safety and clinical effectiveness comparable to hospitalisation, alleviating staff and healthcare system pressures [15–18]. However, existing reviews focus on quantitative outcomes like mortality and readmissions, often neglecting components that optimise outcomes from the perspectives of patients, family carers (hereafter carers) and healthcare professionals [15, 17, 18]. A research agenda established after the First World HaH Congress in 2019 identified HaH experiences as a key priority for understanding barriers and facilitators to home care [19].
The aim of this review was to systematically examine the literature of HaH care for older people in the UK, focussing on older people, carers and healthcare professionals’ experiences and perceptions of what optimises outcomes.
Objectives include
Summarise HaH experiences and perspectives of older people, carers and healthcare professionals.
Understand service and patient-level barriers and facilitators for optimising care outcomes.
Compare different HaH models and care delivery to support older people at home.
Devise recommendations for clinical practice and policy to optimise HaH care for older people.
Methods
This systematic review was conducted in accordance with the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) 2020 statement [20] (see Appendix 1). This was also used to shape the search strategy and eligibility criteria using the Population, Intervention, Comparator, Study Type approach [20]. Searches were conducted up to January 2024 (PROSPERO protocol ID: CRD42024535878).
Eligibility criteria
This review focused on the UK due to its unique publicly funded healthcare and social care system, which integrates HaHs into this framework. This approach allows for a targeted understanding of factors influencing care that are directly relevant to national policy and practice, enabling incorporation of UK-specific grey literature.
Search strategy
This was an iterative process with search terms devised in collaboration with an information specialist and Patient Public Involvement (PPI) members to ensure an extensive search (see Table 1). An initial scoping search of literature was conducted on MEDLINE using the concepts of ‘virtual ward’ OR ‘hospital at home’ AND ‘older adult’ to develop keywords and Medical Subject Headings (MeSH) terms. A comprehensive search on MEDLINE, CINAHL and EMBASE was undertaken in January 2024 using the terms identified from the scoping search (search strategy results seen in Appendix 2). Grey literature was searched in March 2024 from Overton (NHS and government documents), customised Google search engines (first 10 pages) and think tanks (The Kings Fund and Nuffield Trust).
| . | Inclusion . | Exclusion . |
|---|---|---|
| Population |
|
|
| Intervention |
|
|
| Comparator | N/A | N/A |
| Outcome |
| |
| Study type |
|
|
| . | Inclusion . | Exclusion . |
|---|---|---|
| Population |
|
|
| Intervention |
|
|
| Comparator | N/A | N/A |
| Outcome |
| |
| Study type |
|
|
N/A, not available.
| . | Inclusion . | Exclusion . |
|---|---|---|
| Population |
|
|
| Intervention |
|
|
| Comparator | N/A | N/A |
| Outcome |
| |
| Study type |
|
|
| . | Inclusion . | Exclusion . |
|---|---|---|
| Population |
|
|
| Intervention |
|
|
| Comparator | N/A | N/A |
| Outcome |
| |
| Study type |
|
|
N/A, not available.
Screening and selection process
Titles and abstracts were screened against the inclusion and exclusion criteria using the Rayyan Systematic Review Software by one reviewer (A.W.). A random 10% of these were double screened by a second reviewer (C.S.A.). Any disputes were resolved via discussion and consensus or, if necessary, involvement of a third reviewer (N.D.). This process was repeated in the full-text screening. Subsequent forward and backward citation tracking of included full texts were conducted.
Data extraction
A data extraction tool was developed in Microsoft Excel, informed by the Cochrane data extraction template—seen in Appendix 3 [21]. This was completed by one reviewer (A.W.) and a random 20% checked by a second reviewer (N.D.).
| Author, year . | Study type . | Methods . | Population characteristics: (total) . | Population breakdown . | Mean patient age (years) . | Key findings . |
|---|---|---|---|---|---|---|
| Chen, 2024 [22] | Literature review + qualitative | Small group/individual interview | Staff: 16 | 5 nurses, 8 doctors. 1 PA, 1 PT, 1 OT | Services were mostly older people >65 | Holistic healing effects of home environment, better therapeutic staff–patient–carer relationships, more continuity of care |
| Dismore, 2018 [23] | Qualitative embedded in RCT | Semi-structured interview and Carer Burden Scale | Patient: 31 Carer: 15 Staff: 30 | Patient: (15 HaH, 16 hospital), 13 decliners Carer: (10 HaH, 5 hospital) Staff: 11 specialist nurses, 15 doctors, 4 managers | 68 Decliners: 73 | HaH preferred—more independence, maintenance of daily routine, better sleep. Safety concerns of patient being alone at night |
| Dowell, 2018 [24] | Qualitative | Telephone questionnaire | Patient, carer: 105 Staff: GPs | N/A | 84% 65 to 85+ | High satisfaction. HaH allows for holistic care |
| Gunnell, 2000 [25] | RCT | Postal Questionnaire—carer strain index, patient satisfaction | Carer: 133 | 93 HaH, 40 hospital | 65 | HaH had no significant impact on carer burden, HaH carers had significantly higher carer satisfaction compared to hospital carers |
| Health Innovation Network, 2021 [26] | Grey literature—mixed methods | Current Health Patient Experience Survey and Interview | Patient Questionnaire: 37 Patient Interview: 3 | N/A | 60% of patients >60, 25% of patients >80 | Therapeutic care relationship enabled shared decision-making, increased patient/carer confidence. Staff recognise digital exclusion |
| Jester, 2002 [27] | Mixed methods—longitudinal follow-up study | Modified hospital patient satisfaction index survey and carer semi-structured interviews | Patient: 109 Carer: 21 | Patient: 64 HaH, 45 hospital | 74 | Patient satisfaction significantly higher in HaH vs hospital. All but one carer would choose HaH care again |
| Karacaoglu, 2021 [28] | Qualitative | Satisfaction questionnaire and semi-structured interview | Staff: 13 | 3 Advanced practitioners, 5 healthcare support workers, 2 pharmacists, 3 management | 86.2 | Upskilling care practitioners seen as facilitator. Positive feedback from patients regarding increased confidence, and value of home support |
| Kirkcaldy, 2017 [29] | Qualitative | Focus group interview | Staff: 14 | 5 pharmacists, 9 from wider MDT (PT, OT, district nurses) | N/A due to staff perspectives | Increased patient confidence at home, value of HaH holistic care. Challenge accessing patient GP record by pharmacist |
| Knowelden, 1991 [30] | Qualitative | Questionnaire—degree of satisfaction and interview of carers | Patient questionnaire: 105 Patient interview: 66 | Questionnaire: 50 HaH, 55 hospital Interview: 33 HaH, 6 with carer, 33 hospital | HaH: 67 Hospital: 64 | Patients content with HaH care. Carers found some degree of burden with HaH but was similar with burden from usual hospital care |
| Kotb, 2023 [31] | Qualitative—proof-of-concept study | Questionnaire—NHS Friends and Family test and narrative feedback | Patient: 45 | N/A | 66 | Feelings of empowerment, active care participation, hospital stay avoidance and ease of access to healthcare staff. Difficulty with technology, lack of communication and lack of ‘visible’ healthcare staff |
| Makela, 2020 [32] | Qualitative—within RCT | Semi-structured interview | Patient: 34 Carer: 29 | Patient: 15 HaH, 19 hospital Carer: 12 HaH, 17 hospital | HaH: 83 Hospital: 84 | Carers facilitate HaH continuity of care. Upskilling healthcare professionals facilitate care. Barriers: lack of shared decision-making, and HaH safety concerns |
| Ojoo, 2002 [33] | RCT | Structured interview of satisfaction questionnaire | Patient: 54 Carer: 34 | Patient: 27 HaH, 27 hospital | HaH: 69.7 Hospital: 70.1 | Patients and carers prefer HaH |
| Saleh, 2024 [34] | Qualitative—service evaluation | Questionnaire—NHS Friends and Family Test | Patient: 43 | N/A | 65 | Remote monitoring equipment increased patient perceptions of safety. Increased empowerment via digital education. Barriers: technical difficulty, digital exclusion |
| Schiff, 2022 [35] | Qualitative | Retrospective telephone questionnaire | Patient: 3 Carer: 13 | N/A | 85 | Increase NHS capacity for beds, value of staying at home with family support |
| Schofield, 2005 [36] | Mixed methods | Postal survey + interview | Patient, carer: 104 | All used HaH service Total interviews: 30 (18 patient, 10 patient and carer, 2 carer) | 68 | Wholly positive experiences with HaH compared to negative hospital experiences |
| Shepperd, 1998 [37] | RCT | Satisfaction questionnaire Carer strain index to measure carer burden | Patient: 347 Carer: 155 | Patient: 149 HaH, 198 hospital Carer: 80 HaH, 75 hospital | Mean age ranged depending on pathway HaH: 68–77 Hospital: 70–76 | All patients except those with COPD preferred HaH care. No significant differences in carer burden between HaH and hospital |
| Shepperd, 2021 [38] | Multi-site RCT | Picker Institute patient-reported experience questionnaire | Patient: 1032 | 687 HaH, 345 hospital | 83.3 | Responses regarding wait time, how to contact staff and decision-making involvement favoured HaH |
| Thornton, 2023 [39] | Grey literature | Survey from census | Public: 7100 Staff: 1251 | N/A | >16 years, included 65+ group | Public and NHS staff support HaHs, further need to clarify HaH terminology |
| Vindrola-Padros, 2021 [40] | Qualitative | Semi-structured interview | Staff: 22 | 8 pilot site leads, 7 monitoring leads, 7 staff with knowledge of data collection | N/A due to staff perspectives | Personalised care. Barriers: digital exclusion, lack of culturally appropriate resources, poor integration of service data with existing administration systems |
| Wilson, 2002 [41] | RCT | Questionnaire + semi-structured interview | Patient questionnaire: 83 Patient interview: 42 Carer: 25 | Questionnaire: 48 HaH, 35 hospital Patient interview: 24 HaH, 18 hospital Carer interview: 18 HaH, 7 hospital | Paper reported median age HaH: 82 Hospital: 81 | HaH more personalised, better communication vs hospital. Value of home. Carers had safety concerns. No carer burden increase |
| Author, year . | Study type . | Methods . | Population characteristics: (total) . | Population breakdown . | Mean patient age (years) . | Key findings . |
|---|---|---|---|---|---|---|
| Chen, 2024 [22] | Literature review + qualitative | Small group/individual interview | Staff: 16 | 5 nurses, 8 doctors. 1 PA, 1 PT, 1 OT | Services were mostly older people >65 | Holistic healing effects of home environment, better therapeutic staff–patient–carer relationships, more continuity of care |
| Dismore, 2018 [23] | Qualitative embedded in RCT | Semi-structured interview and Carer Burden Scale | Patient: 31 Carer: 15 Staff: 30 | Patient: (15 HaH, 16 hospital), 13 decliners Carer: (10 HaH, 5 hospital) Staff: 11 specialist nurses, 15 doctors, 4 managers | 68 Decliners: 73 | HaH preferred—more independence, maintenance of daily routine, better sleep. Safety concerns of patient being alone at night |
| Dowell, 2018 [24] | Qualitative | Telephone questionnaire | Patient, carer: 105 Staff: GPs | N/A | 84% 65 to 85+ | High satisfaction. HaH allows for holistic care |
| Gunnell, 2000 [25] | RCT | Postal Questionnaire—carer strain index, patient satisfaction | Carer: 133 | 93 HaH, 40 hospital | 65 | HaH had no significant impact on carer burden, HaH carers had significantly higher carer satisfaction compared to hospital carers |
| Health Innovation Network, 2021 [26] | Grey literature—mixed methods | Current Health Patient Experience Survey and Interview | Patient Questionnaire: 37 Patient Interview: 3 | N/A | 60% of patients >60, 25% of patients >80 | Therapeutic care relationship enabled shared decision-making, increased patient/carer confidence. Staff recognise digital exclusion |
| Jester, 2002 [27] | Mixed methods—longitudinal follow-up study | Modified hospital patient satisfaction index survey and carer semi-structured interviews | Patient: 109 Carer: 21 | Patient: 64 HaH, 45 hospital | 74 | Patient satisfaction significantly higher in HaH vs hospital. All but one carer would choose HaH care again |
| Karacaoglu, 2021 [28] | Qualitative | Satisfaction questionnaire and semi-structured interview | Staff: 13 | 3 Advanced practitioners, 5 healthcare support workers, 2 pharmacists, 3 management | 86.2 | Upskilling care practitioners seen as facilitator. Positive feedback from patients regarding increased confidence, and value of home support |
| Kirkcaldy, 2017 [29] | Qualitative | Focus group interview | Staff: 14 | 5 pharmacists, 9 from wider MDT (PT, OT, district nurses) | N/A due to staff perspectives | Increased patient confidence at home, value of HaH holistic care. Challenge accessing patient GP record by pharmacist |
| Knowelden, 1991 [30] | Qualitative | Questionnaire—degree of satisfaction and interview of carers | Patient questionnaire: 105 Patient interview: 66 | Questionnaire: 50 HaH, 55 hospital Interview: 33 HaH, 6 with carer, 33 hospital | HaH: 67 Hospital: 64 | Patients content with HaH care. Carers found some degree of burden with HaH but was similar with burden from usual hospital care |
| Kotb, 2023 [31] | Qualitative—proof-of-concept study | Questionnaire—NHS Friends and Family test and narrative feedback | Patient: 45 | N/A | 66 | Feelings of empowerment, active care participation, hospital stay avoidance and ease of access to healthcare staff. Difficulty with technology, lack of communication and lack of ‘visible’ healthcare staff |
| Makela, 2020 [32] | Qualitative—within RCT | Semi-structured interview | Patient: 34 Carer: 29 | Patient: 15 HaH, 19 hospital Carer: 12 HaH, 17 hospital | HaH: 83 Hospital: 84 | Carers facilitate HaH continuity of care. Upskilling healthcare professionals facilitate care. Barriers: lack of shared decision-making, and HaH safety concerns |
| Ojoo, 2002 [33] | RCT | Structured interview of satisfaction questionnaire | Patient: 54 Carer: 34 | Patient: 27 HaH, 27 hospital | HaH: 69.7 Hospital: 70.1 | Patients and carers prefer HaH |
| Saleh, 2024 [34] | Qualitative—service evaluation | Questionnaire—NHS Friends and Family Test | Patient: 43 | N/A | 65 | Remote monitoring equipment increased patient perceptions of safety. Increased empowerment via digital education. Barriers: technical difficulty, digital exclusion |
| Schiff, 2022 [35] | Qualitative | Retrospective telephone questionnaire | Patient: 3 Carer: 13 | N/A | 85 | Increase NHS capacity for beds, value of staying at home with family support |
| Schofield, 2005 [36] | Mixed methods | Postal survey + interview | Patient, carer: 104 | All used HaH service Total interviews: 30 (18 patient, 10 patient and carer, 2 carer) | 68 | Wholly positive experiences with HaH compared to negative hospital experiences |
| Shepperd, 1998 [37] | RCT | Satisfaction questionnaire Carer strain index to measure carer burden | Patient: 347 Carer: 155 | Patient: 149 HaH, 198 hospital Carer: 80 HaH, 75 hospital | Mean age ranged depending on pathway HaH: 68–77 Hospital: 70–76 | All patients except those with COPD preferred HaH care. No significant differences in carer burden between HaH and hospital |
| Shepperd, 2021 [38] | Multi-site RCT | Picker Institute patient-reported experience questionnaire | Patient: 1032 | 687 HaH, 345 hospital | 83.3 | Responses regarding wait time, how to contact staff and decision-making involvement favoured HaH |
| Thornton, 2023 [39] | Grey literature | Survey from census | Public: 7100 Staff: 1251 | N/A | >16 years, included 65+ group | Public and NHS staff support HaHs, further need to clarify HaH terminology |
| Vindrola-Padros, 2021 [40] | Qualitative | Semi-structured interview | Staff: 22 | 8 pilot site leads, 7 monitoring leads, 7 staff with knowledge of data collection | N/A due to staff perspectives | Personalised care. Barriers: digital exclusion, lack of culturally appropriate resources, poor integration of service data with existing administration systems |
| Wilson, 2002 [41] | RCT | Questionnaire + semi-structured interview | Patient questionnaire: 83 Patient interview: 42 Carer: 25 | Questionnaire: 48 HaH, 35 hospital Patient interview: 24 HaH, 18 hospital Carer interview: 18 HaH, 7 hospital | Paper reported median age HaH: 82 Hospital: 81 | HaH more personalised, better communication vs hospital. Value of home. Carers had safety concerns. No carer burden increase |
N/A, not available; OT, occupational therapist; PA, physician’s associate; PT, physiotherapist; RCT, randomised controlled trial.
| Author, year . | Study type . | Methods . | Population characteristics: (total) . | Population breakdown . | Mean patient age (years) . | Key findings . |
|---|---|---|---|---|---|---|
| Chen, 2024 [22] | Literature review + qualitative | Small group/individual interview | Staff: 16 | 5 nurses, 8 doctors. 1 PA, 1 PT, 1 OT | Services were mostly older people >65 | Holistic healing effects of home environment, better therapeutic staff–patient–carer relationships, more continuity of care |
| Dismore, 2018 [23] | Qualitative embedded in RCT | Semi-structured interview and Carer Burden Scale | Patient: 31 Carer: 15 Staff: 30 | Patient: (15 HaH, 16 hospital), 13 decliners Carer: (10 HaH, 5 hospital) Staff: 11 specialist nurses, 15 doctors, 4 managers | 68 Decliners: 73 | HaH preferred—more independence, maintenance of daily routine, better sleep. Safety concerns of patient being alone at night |
| Dowell, 2018 [24] | Qualitative | Telephone questionnaire | Patient, carer: 105 Staff: GPs | N/A | 84% 65 to 85+ | High satisfaction. HaH allows for holistic care |
| Gunnell, 2000 [25] | RCT | Postal Questionnaire—carer strain index, patient satisfaction | Carer: 133 | 93 HaH, 40 hospital | 65 | HaH had no significant impact on carer burden, HaH carers had significantly higher carer satisfaction compared to hospital carers |
| Health Innovation Network, 2021 [26] | Grey literature—mixed methods | Current Health Patient Experience Survey and Interview | Patient Questionnaire: 37 Patient Interview: 3 | N/A | 60% of patients >60, 25% of patients >80 | Therapeutic care relationship enabled shared decision-making, increased patient/carer confidence. Staff recognise digital exclusion |
| Jester, 2002 [27] | Mixed methods—longitudinal follow-up study | Modified hospital patient satisfaction index survey and carer semi-structured interviews | Patient: 109 Carer: 21 | Patient: 64 HaH, 45 hospital | 74 | Patient satisfaction significantly higher in HaH vs hospital. All but one carer would choose HaH care again |
| Karacaoglu, 2021 [28] | Qualitative | Satisfaction questionnaire and semi-structured interview | Staff: 13 | 3 Advanced practitioners, 5 healthcare support workers, 2 pharmacists, 3 management | 86.2 | Upskilling care practitioners seen as facilitator. Positive feedback from patients regarding increased confidence, and value of home support |
| Kirkcaldy, 2017 [29] | Qualitative | Focus group interview | Staff: 14 | 5 pharmacists, 9 from wider MDT (PT, OT, district nurses) | N/A due to staff perspectives | Increased patient confidence at home, value of HaH holistic care. Challenge accessing patient GP record by pharmacist |
| Knowelden, 1991 [30] | Qualitative | Questionnaire—degree of satisfaction and interview of carers | Patient questionnaire: 105 Patient interview: 66 | Questionnaire: 50 HaH, 55 hospital Interview: 33 HaH, 6 with carer, 33 hospital | HaH: 67 Hospital: 64 | Patients content with HaH care. Carers found some degree of burden with HaH but was similar with burden from usual hospital care |
| Kotb, 2023 [31] | Qualitative—proof-of-concept study | Questionnaire—NHS Friends and Family test and narrative feedback | Patient: 45 | N/A | 66 | Feelings of empowerment, active care participation, hospital stay avoidance and ease of access to healthcare staff. Difficulty with technology, lack of communication and lack of ‘visible’ healthcare staff |
| Makela, 2020 [32] | Qualitative—within RCT | Semi-structured interview | Patient: 34 Carer: 29 | Patient: 15 HaH, 19 hospital Carer: 12 HaH, 17 hospital | HaH: 83 Hospital: 84 | Carers facilitate HaH continuity of care. Upskilling healthcare professionals facilitate care. Barriers: lack of shared decision-making, and HaH safety concerns |
| Ojoo, 2002 [33] | RCT | Structured interview of satisfaction questionnaire | Patient: 54 Carer: 34 | Patient: 27 HaH, 27 hospital | HaH: 69.7 Hospital: 70.1 | Patients and carers prefer HaH |
| Saleh, 2024 [34] | Qualitative—service evaluation | Questionnaire—NHS Friends and Family Test | Patient: 43 | N/A | 65 | Remote monitoring equipment increased patient perceptions of safety. Increased empowerment via digital education. Barriers: technical difficulty, digital exclusion |
| Schiff, 2022 [35] | Qualitative | Retrospective telephone questionnaire | Patient: 3 Carer: 13 | N/A | 85 | Increase NHS capacity for beds, value of staying at home with family support |
| Schofield, 2005 [36] | Mixed methods | Postal survey + interview | Patient, carer: 104 | All used HaH service Total interviews: 30 (18 patient, 10 patient and carer, 2 carer) | 68 | Wholly positive experiences with HaH compared to negative hospital experiences |
| Shepperd, 1998 [37] | RCT | Satisfaction questionnaire Carer strain index to measure carer burden | Patient: 347 Carer: 155 | Patient: 149 HaH, 198 hospital Carer: 80 HaH, 75 hospital | Mean age ranged depending on pathway HaH: 68–77 Hospital: 70–76 | All patients except those with COPD preferred HaH care. No significant differences in carer burden between HaH and hospital |
| Shepperd, 2021 [38] | Multi-site RCT | Picker Institute patient-reported experience questionnaire | Patient: 1032 | 687 HaH, 345 hospital | 83.3 | Responses regarding wait time, how to contact staff and decision-making involvement favoured HaH |
| Thornton, 2023 [39] | Grey literature | Survey from census | Public: 7100 Staff: 1251 | N/A | >16 years, included 65+ group | Public and NHS staff support HaHs, further need to clarify HaH terminology |
| Vindrola-Padros, 2021 [40] | Qualitative | Semi-structured interview | Staff: 22 | 8 pilot site leads, 7 monitoring leads, 7 staff with knowledge of data collection | N/A due to staff perspectives | Personalised care. Barriers: digital exclusion, lack of culturally appropriate resources, poor integration of service data with existing administration systems |
| Wilson, 2002 [41] | RCT | Questionnaire + semi-structured interview | Patient questionnaire: 83 Patient interview: 42 Carer: 25 | Questionnaire: 48 HaH, 35 hospital Patient interview: 24 HaH, 18 hospital Carer interview: 18 HaH, 7 hospital | Paper reported median age HaH: 82 Hospital: 81 | HaH more personalised, better communication vs hospital. Value of home. Carers had safety concerns. No carer burden increase |
| Author, year . | Study type . | Methods . | Population characteristics: (total) . | Population breakdown . | Mean patient age (years) . | Key findings . |
|---|---|---|---|---|---|---|
| Chen, 2024 [22] | Literature review + qualitative | Small group/individual interview | Staff: 16 | 5 nurses, 8 doctors. 1 PA, 1 PT, 1 OT | Services were mostly older people >65 | Holistic healing effects of home environment, better therapeutic staff–patient–carer relationships, more continuity of care |
| Dismore, 2018 [23] | Qualitative embedded in RCT | Semi-structured interview and Carer Burden Scale | Patient: 31 Carer: 15 Staff: 30 | Patient: (15 HaH, 16 hospital), 13 decliners Carer: (10 HaH, 5 hospital) Staff: 11 specialist nurses, 15 doctors, 4 managers | 68 Decliners: 73 | HaH preferred—more independence, maintenance of daily routine, better sleep. Safety concerns of patient being alone at night |
| Dowell, 2018 [24] | Qualitative | Telephone questionnaire | Patient, carer: 105 Staff: GPs | N/A | 84% 65 to 85+ | High satisfaction. HaH allows for holistic care |
| Gunnell, 2000 [25] | RCT | Postal Questionnaire—carer strain index, patient satisfaction | Carer: 133 | 93 HaH, 40 hospital | 65 | HaH had no significant impact on carer burden, HaH carers had significantly higher carer satisfaction compared to hospital carers |
| Health Innovation Network, 2021 [26] | Grey literature—mixed methods | Current Health Patient Experience Survey and Interview | Patient Questionnaire: 37 Patient Interview: 3 | N/A | 60% of patients >60, 25% of patients >80 | Therapeutic care relationship enabled shared decision-making, increased patient/carer confidence. Staff recognise digital exclusion |
| Jester, 2002 [27] | Mixed methods—longitudinal follow-up study | Modified hospital patient satisfaction index survey and carer semi-structured interviews | Patient: 109 Carer: 21 | Patient: 64 HaH, 45 hospital | 74 | Patient satisfaction significantly higher in HaH vs hospital. All but one carer would choose HaH care again |
| Karacaoglu, 2021 [28] | Qualitative | Satisfaction questionnaire and semi-structured interview | Staff: 13 | 3 Advanced practitioners, 5 healthcare support workers, 2 pharmacists, 3 management | 86.2 | Upskilling care practitioners seen as facilitator. Positive feedback from patients regarding increased confidence, and value of home support |
| Kirkcaldy, 2017 [29] | Qualitative | Focus group interview | Staff: 14 | 5 pharmacists, 9 from wider MDT (PT, OT, district nurses) | N/A due to staff perspectives | Increased patient confidence at home, value of HaH holistic care. Challenge accessing patient GP record by pharmacist |
| Knowelden, 1991 [30] | Qualitative | Questionnaire—degree of satisfaction and interview of carers | Patient questionnaire: 105 Patient interview: 66 | Questionnaire: 50 HaH, 55 hospital Interview: 33 HaH, 6 with carer, 33 hospital | HaH: 67 Hospital: 64 | Patients content with HaH care. Carers found some degree of burden with HaH but was similar with burden from usual hospital care |
| Kotb, 2023 [31] | Qualitative—proof-of-concept study | Questionnaire—NHS Friends and Family test and narrative feedback | Patient: 45 | N/A | 66 | Feelings of empowerment, active care participation, hospital stay avoidance and ease of access to healthcare staff. Difficulty with technology, lack of communication and lack of ‘visible’ healthcare staff |
| Makela, 2020 [32] | Qualitative—within RCT | Semi-structured interview | Patient: 34 Carer: 29 | Patient: 15 HaH, 19 hospital Carer: 12 HaH, 17 hospital | HaH: 83 Hospital: 84 | Carers facilitate HaH continuity of care. Upskilling healthcare professionals facilitate care. Barriers: lack of shared decision-making, and HaH safety concerns |
| Ojoo, 2002 [33] | RCT | Structured interview of satisfaction questionnaire | Patient: 54 Carer: 34 | Patient: 27 HaH, 27 hospital | HaH: 69.7 Hospital: 70.1 | Patients and carers prefer HaH |
| Saleh, 2024 [34] | Qualitative—service evaluation | Questionnaire—NHS Friends and Family Test | Patient: 43 | N/A | 65 | Remote monitoring equipment increased patient perceptions of safety. Increased empowerment via digital education. Barriers: technical difficulty, digital exclusion |
| Schiff, 2022 [35] | Qualitative | Retrospective telephone questionnaire | Patient: 3 Carer: 13 | N/A | 85 | Increase NHS capacity for beds, value of staying at home with family support |
| Schofield, 2005 [36] | Mixed methods | Postal survey + interview | Patient, carer: 104 | All used HaH service Total interviews: 30 (18 patient, 10 patient and carer, 2 carer) | 68 | Wholly positive experiences with HaH compared to negative hospital experiences |
| Shepperd, 1998 [37] | RCT | Satisfaction questionnaire Carer strain index to measure carer burden | Patient: 347 Carer: 155 | Patient: 149 HaH, 198 hospital Carer: 80 HaH, 75 hospital | Mean age ranged depending on pathway HaH: 68–77 Hospital: 70–76 | All patients except those with COPD preferred HaH care. No significant differences in carer burden between HaH and hospital |
| Shepperd, 2021 [38] | Multi-site RCT | Picker Institute patient-reported experience questionnaire | Patient: 1032 | 687 HaH, 345 hospital | 83.3 | Responses regarding wait time, how to contact staff and decision-making involvement favoured HaH |
| Thornton, 2023 [39] | Grey literature | Survey from census | Public: 7100 Staff: 1251 | N/A | >16 years, included 65+ group | Public and NHS staff support HaHs, further need to clarify HaH terminology |
| Vindrola-Padros, 2021 [40] | Qualitative | Semi-structured interview | Staff: 22 | 8 pilot site leads, 7 monitoring leads, 7 staff with knowledge of data collection | N/A due to staff perspectives | Personalised care. Barriers: digital exclusion, lack of culturally appropriate resources, poor integration of service data with existing administration systems |
| Wilson, 2002 [41] | RCT | Questionnaire + semi-structured interview | Patient questionnaire: 83 Patient interview: 42 Carer: 25 | Questionnaire: 48 HaH, 35 hospital Patient interview: 24 HaH, 18 hospital Carer interview: 18 HaH, 7 hospital | Paper reported median age HaH: 82 Hospital: 81 | HaH more personalised, better communication vs hospital. Value of home. Carers had safety concerns. No carer burden increase |
N/A, not available; OT, occupational therapist; PA, physician’s associate; PT, physiotherapist; RCT, randomised controlled trial.
Quality appraisal
The Hawker critical appraisal tool was used to appraise each paper by one reviewer (A.W.) and a random 20% checked by a second reviewer (N.D.) [42]. They were scored from 1 to 4 on nine items to give a total score. These scores were categorised as low (total score 9–24), medium (total score 24–29) or high quality (total score 30–36) indicated by the colours red, orange and green in Appendix 4. The AACODS checklist (Authority, Accuracy, Coverage, Objectivity, Date and Significance) was used for grey literature appraisal [43].
Data synthesis
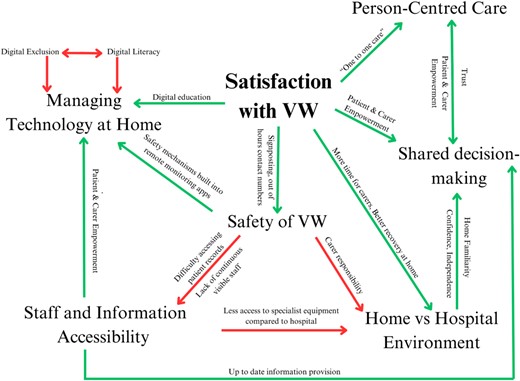
A stepwise narrative synthesis model was utilised, guided by Popay et al. [44, 45]. This included tabulation of studies in thematic analysis form and concept mapping. Each theme was plotted and lines drawn to represent relationships between them (positive and/or negative experiences identified by study participants). Barriers and facilitators to specific themes were included where relevant.
Patient and public involvement and stakeholder involvement
Two former family carers of older people guided the methods of this review. We hosted a meeting to gather feedback on the themes and potential key messages for recommendation.
Results
Study selection
After removing duplicates, 2463 records were identified and assessed for relevance at title and abstract level. Also, 205 were assessed at full text, leading to the inclusion of 18 studies [22–25, 27–38, 40, 41] (see Table 2 for details). Grey literature database searches yielded 674 records with two included in this review [26, 39]. Figure 1 includes reasons for exclusion at full-text eligibility stage [20].
![PRISMA flow of study selection [20].](https://oup.silverchair-cdn.com/oup/backfile/Content_public/Journal/ageing/54/2/10.1093_ageing_afaf033/1/m_afaf033f1.jpeg?Expires=1748306280&Signature=hYw6GseqzAvL8V3AMM1pXNsbxUawB~9o10TGMJFr5ms-Xmn74kdh8vHPJ7ThbTi1E9KWWUvFBOyOs-MTWtIl8yKYgQKMhWKgKHDBOGMml6qFmhspQ0QEyoLr2txxa5~v~8ZGZKZ0Y37yjhg9-wJ4cMBWAk59qsuUd1Z81S-rEdG~VKLXnVU78~XwGArGiKG9hmsfN5DRd9m7DeWG4RhXk-GbEnEtEV6sQyo5Ed98cM2viDWwY8jelZT6CrlDOxHnSkdDofU56BuCKPkTS1S~mRvbl-jR4BHqmK13Z0OpgcYXzGwqMM8IyszVKDGR1hGltrnpIvuXYubRn8Wp6KD5lA__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
Study characteristics
Of the included papers, 11 were qualitative [23, 24, 28–32, 34, 35, 39, 40], 5 were randomised controlled trials [25, 33, 37, 38, 41] and 4 were mixed methods [22, 26, 27, 36]. The most common perspectives within included studies were those of patients and family carers (n = 1349 total participants, with n = 256 carers within this) [27, 30, 32, 33, 35–37, 41]. A further four studies included patient, carer and healthcare professional perspectives [23, 24, 26, 39].
Quality appraisal
The included studies were of moderate-good quality, with only two studies rated as poor. All included studies had a clear description of methods, population characteristics, data collection and justification of sample sizes, with findings in line with stated aims. Studies were rated poorly due to brief acknowledgement, if at all, of authors’ bias and limited generalisability to the wider population—seen in Appendix 4.
Care models
Studies report ‘step up’ admission avoidance [24, 26, 29, 32, 38, 41], ‘step down’ early discharge [23, 25, 27, 28, 30, 33, 36, 37] or both models [22, 31, 34, 35, 39, 40]. Most HaH services operated 7 days a week—four studies had 24-h service models [23, 24, 37, 41]. All had signposting to HaH staff contact numbers or out-of-hours services [23, 24, 26, 29, 31, 34, 38, 40]. Levels of digital technology implementation varied, but all included remote care via telephone calls and face-to-face home visits by healthcare professionals. Remote monitoring applications had safety mechanisms notifying patients and healthcare teams when recorded data indicated potential deterioration, signposting contact information for assistance [26, 34, 40].
Included studies evaluated condition specific HaHs (most commonly COPD, atrial fibrillation and COVID-19) [23, 31, 33–35, 40, 46, 47]. Studies also looked at general HaHs led by consultant geriatricians or other healthcare professionals such as specialist nurses or advanced nurse practitioners [22, 24, 25, 27–30, 32, 37, 39, 48]. Conditions treated include frailty, dementia, delirium, stroke, post-surgery recovery from hip or knee replacements, urinary tract infections and falls (Table 3).
| Author, year . | Clinical responsibility . | Healthcare professionals’ team . | Conditions treated . | HaH model . | Technology enabled?a . |
|---|---|---|---|---|---|
| Chen, 2024 [22] | Consultant geriatrician/community specialist nurse | Nurse, ANP, SN, ACP, consultant geriatrician, GP, OT, PT, speech therapist, pharmacist, administration staff, PA | Unspecified—‘older patients with a range of conditions’ | Admission avoidance and early discharge Home visits and telephone calls by staff | No |
| Dismore, 2018 [23] | Respiratory consultant | Respiratory specialist nurse, respiratory consultant, GP | COPD | Early discharge, nurse led Home visits 1–2× daily by nurses | No |
| Dowell, 2018 [24] | Paramedics, nurses and physiotherapists | Nurse, GP, PT, specialist paramedic | Unwell adult pathway, COPD, UTI, palliative, IV, cellulitis, falls | Admission avoidance, 24 h Referral triage system | No |
| Gunnell, 2000 [25] | Not stated | Not stated | Fracture, elective orthopaedic surgery, stroke, dementia | Early discharge | No |
| Health Innovation Network, 2021 [26] | 2 consultant geriatricians, 1 respiratory consultant, rapid response GP | Nurse, consultant geriatrician, respiratory consultant, GP, project lead, rapid response matron | COVID-19 | Admission avoidance, 8 a.m.–8 p.m., 7 days a week Staff contacted patient via phone/video call, home visits. Out-of-hours service (111/999) Wearable integrated with tablet. Home hub connects wearable to cloud. Vital signs continuously collected and displayed on web dashboard for remote monitoring team | Yes |
| Jester, 2002 [27] | Orthopaedic surgeon | Nurse, orthopaedic consultant, PT | Hip/knee replacement surgery recovery | Early discharge, home visits from nurse/PT at least 1× a day. 7 days a week, 8 a.m.–8 p.m. Out of hours: senior on-call nurse | No |
| Karacaoglu, 2021 [28] | Clinical guidance from consultant geriatrician | ANP, consultant geriatrician, OT, PT, pharmacist, healthcare support worker | Geriatric syndrome | Early discharge providing rehabilitation support and home visits from nursing, PT, OT | No |
| Kirkcaldy, 2017 [29] | Not stated | Nurse, OT, PT, pharmacist, social care, community matron | Unspecified ‘older patients with a range of conditions’ | Admission avoidance—has medicines management team that delivers support to increase adherence | No |
| Knowelden, 1991 [30] | GP | Nurse, GP | Metastatic neoplasm, early discharge post-surgery, stroke | Early discharge, mainly district nurse led with home visits | No |
| Kotb, 2023 [31] | Consultant cardiologist | Nurse, ACP, cardiology consultant, registrar, pharmacist | Atrial fibrillation, atrial flutter and fast ventricular response | Admission avoidance, early discharge. 7-days-per-week service, 9 a.m.–5 p.m. Out of hours: on-call cardiology registrar/emergency services Provided with ECG devices, Bluetooth blood pressure monitor, pulse oximeter, smartphone app to record readings/symptom severity. If readings exceed threshold, patients and healthcare team notified. In-app messaging, telephone, video calls | Yes |
| Makela, 2020 [32] | Geriatrician | ANP, consultant geriatrician, GP, speciality training doctor, OT, PT, speech therapist, pharmacist, social care | Falls, delirium, COPD, back pain, cellulitis, chest infection, other | Admission avoidance—7 days a week, 9 a.m.—early evening. Emergency medical cover available 24 h a day. Primary care support | No |
| Ojoo, 2002 [33] | Respiratory outreach nurse | Respiratory specialist nurse | COPD | Early discharge—9 a.m.–5 p.m., monitor patients daily. Out-of-hours services—Medical Chest Unit direct line | No |
| Saleh, 2024 [34] | Cardiology consultant | Nurse, digital technology specialist nurse, ANP, cardiology consultant, registrar, allied healthcare professionals | Atrial fibrillation | Admission avoidance, early discharge. 8 a.m.–8 p.m. Out-of-hours signposting to 111/999 Weekly MDT meetings to discuss HaH patients FIBRICHECK remote monitoring app. Measurements and symptom severity recorded into app twice daily. Monitored by hub, where a dashboard of patients’ clinical data could be reviewed by clinicians twice daily | Yes |
| Schiff, 2022 [35] | Not stated | Not stated | COVID-19 | Admission avoidance, early discharge | No |
| Schofield, 2005 [36] | Respiratory consultant | Respiratory specialist nurse, respiratory consultant | COPD | Early discharge, 9 a.m.–5 p.m. Respiratory nurses do home visits and outreach treatment | No |
| Shepperd, 1998 [37] | GP | ANP, doctors, allied health professionals | Hip/knee replacement recovery, older medical patients, COPD | Admission avoidance, early discharge. Home visits, observations, administration of drugs such as IV, rehabilitation Patients provided mobile phones if needed | No |
| Shepperd, 2021 [38] | Geriatrician | Nurse, consultant geriatrician, speciality training doctor, OT, PT, speech therapist, pharmacist, social care | Dementia, falls, respiratory. gastrointestinal, musculoskeletal disorders, cardiovascular conditions, UTI | Admission avoidance—7 days a week, some sites offered 24-h care, but most were 9 a.m. to early evening. Emergency medical cover available 24 h a day. Primary care support | No |
| Thornton, 2023 [39] | Not stated | Nurse, doctors | Unspecified | Admission avoidance, early discharge Technology for monitoring considered in definition of HaH | Yes |
| Vindrola-Padros, 2021 [40] | GP/consultant depending on site | Nurse, ANP, respiratory specialist nurse, consultant, GP, registrar, senior and junior clinicians, PT, pilot site lead, OPAT nurse, practice manager, PA | COVID-19 | Admission avoidance, early discharge. Regular monitoring calls from primary or secondary care staff. Provided with pulse oximeter, digital app or paper diary to record observations. If patient observation exceeded ‘safe threshold’, patients and clinical team notified | Yes |
| Wilson, 2002 [41] | GP | Nurse, GP, OT, PT, generic health worker | Cardiovascular and respiratory conditions | Admission avoidance, 4–24-h care. Home visits by nurses | No |
| Author, year . | Clinical responsibility . | Healthcare professionals’ team . | Conditions treated . | HaH model . | Technology enabled?a . |
|---|---|---|---|---|---|
| Chen, 2024 [22] | Consultant geriatrician/community specialist nurse | Nurse, ANP, SN, ACP, consultant geriatrician, GP, OT, PT, speech therapist, pharmacist, administration staff, PA | Unspecified—‘older patients with a range of conditions’ | Admission avoidance and early discharge Home visits and telephone calls by staff | No |
| Dismore, 2018 [23] | Respiratory consultant | Respiratory specialist nurse, respiratory consultant, GP | COPD | Early discharge, nurse led Home visits 1–2× daily by nurses | No |
| Dowell, 2018 [24] | Paramedics, nurses and physiotherapists | Nurse, GP, PT, specialist paramedic | Unwell adult pathway, COPD, UTI, palliative, IV, cellulitis, falls | Admission avoidance, 24 h Referral triage system | No |
| Gunnell, 2000 [25] | Not stated | Not stated | Fracture, elective orthopaedic surgery, stroke, dementia | Early discharge | No |
| Health Innovation Network, 2021 [26] | 2 consultant geriatricians, 1 respiratory consultant, rapid response GP | Nurse, consultant geriatrician, respiratory consultant, GP, project lead, rapid response matron | COVID-19 | Admission avoidance, 8 a.m.–8 p.m., 7 days a week Staff contacted patient via phone/video call, home visits. Out-of-hours service (111/999) Wearable integrated with tablet. Home hub connects wearable to cloud. Vital signs continuously collected and displayed on web dashboard for remote monitoring team | Yes |
| Jester, 2002 [27] | Orthopaedic surgeon | Nurse, orthopaedic consultant, PT | Hip/knee replacement surgery recovery | Early discharge, home visits from nurse/PT at least 1× a day. 7 days a week, 8 a.m.–8 p.m. Out of hours: senior on-call nurse | No |
| Karacaoglu, 2021 [28] | Clinical guidance from consultant geriatrician | ANP, consultant geriatrician, OT, PT, pharmacist, healthcare support worker | Geriatric syndrome | Early discharge providing rehabilitation support and home visits from nursing, PT, OT | No |
| Kirkcaldy, 2017 [29] | Not stated | Nurse, OT, PT, pharmacist, social care, community matron | Unspecified ‘older patients with a range of conditions’ | Admission avoidance—has medicines management team that delivers support to increase adherence | No |
| Knowelden, 1991 [30] | GP | Nurse, GP | Metastatic neoplasm, early discharge post-surgery, stroke | Early discharge, mainly district nurse led with home visits | No |
| Kotb, 2023 [31] | Consultant cardiologist | Nurse, ACP, cardiology consultant, registrar, pharmacist | Atrial fibrillation, atrial flutter and fast ventricular response | Admission avoidance, early discharge. 7-days-per-week service, 9 a.m.–5 p.m. Out of hours: on-call cardiology registrar/emergency services Provided with ECG devices, Bluetooth blood pressure monitor, pulse oximeter, smartphone app to record readings/symptom severity. If readings exceed threshold, patients and healthcare team notified. In-app messaging, telephone, video calls | Yes |
| Makela, 2020 [32] | Geriatrician | ANP, consultant geriatrician, GP, speciality training doctor, OT, PT, speech therapist, pharmacist, social care | Falls, delirium, COPD, back pain, cellulitis, chest infection, other | Admission avoidance—7 days a week, 9 a.m.—early evening. Emergency medical cover available 24 h a day. Primary care support | No |
| Ojoo, 2002 [33] | Respiratory outreach nurse | Respiratory specialist nurse | COPD | Early discharge—9 a.m.–5 p.m., monitor patients daily. Out-of-hours services—Medical Chest Unit direct line | No |
| Saleh, 2024 [34] | Cardiology consultant | Nurse, digital technology specialist nurse, ANP, cardiology consultant, registrar, allied healthcare professionals | Atrial fibrillation | Admission avoidance, early discharge. 8 a.m.–8 p.m. Out-of-hours signposting to 111/999 Weekly MDT meetings to discuss HaH patients FIBRICHECK remote monitoring app. Measurements and symptom severity recorded into app twice daily. Monitored by hub, where a dashboard of patients’ clinical data could be reviewed by clinicians twice daily | Yes |
| Schiff, 2022 [35] | Not stated | Not stated | COVID-19 | Admission avoidance, early discharge | No |
| Schofield, 2005 [36] | Respiratory consultant | Respiratory specialist nurse, respiratory consultant | COPD | Early discharge, 9 a.m.–5 p.m. Respiratory nurses do home visits and outreach treatment | No |
| Shepperd, 1998 [37] | GP | ANP, doctors, allied health professionals | Hip/knee replacement recovery, older medical patients, COPD | Admission avoidance, early discharge. Home visits, observations, administration of drugs such as IV, rehabilitation Patients provided mobile phones if needed | No |
| Shepperd, 2021 [38] | Geriatrician | Nurse, consultant geriatrician, speciality training doctor, OT, PT, speech therapist, pharmacist, social care | Dementia, falls, respiratory. gastrointestinal, musculoskeletal disorders, cardiovascular conditions, UTI | Admission avoidance—7 days a week, some sites offered 24-h care, but most were 9 a.m. to early evening. Emergency medical cover available 24 h a day. Primary care support | No |
| Thornton, 2023 [39] | Not stated | Nurse, doctors | Unspecified | Admission avoidance, early discharge Technology for monitoring considered in definition of HaH | Yes |
| Vindrola-Padros, 2021 [40] | GP/consultant depending on site | Nurse, ANP, respiratory specialist nurse, consultant, GP, registrar, senior and junior clinicians, PT, pilot site lead, OPAT nurse, practice manager, PA | COVID-19 | Admission avoidance, early discharge. Regular monitoring calls from primary or secondary care staff. Provided with pulse oximeter, digital app or paper diary to record observations. If patient observation exceeded ‘safe threshold’, patients and clinical team notified | Yes |
| Wilson, 2002 [41] | GP | Nurse, GP, OT, PT, generic health worker | Cardiovascular and respiratory conditions | Admission avoidance, 4–24-h care. Home visits by nurses | No |
Note: Gunnel et al. did not specify specific staffing in HaH model. ANP, advanced nurse practitioner; ACP, advanced clinical practitioner; OPAT, outpatient parenteral antimicrobial therapy; OT, occupational therapist; PA, physician’s associate; PT, physiotherapist; SN, nurse specialist; UTI, urinary tract infection.
aNHS definition of technology-enabled HaH consists of the following criteria [49]:
1. Patients measuring and inputting their health data into an application/done automatically via wearable or Bluetooth.
2. Data feeds into digital platform where the clinical team can review.
3. Clinical teams are alerted when patient moves outside of safe parameters, and can act accordingly.
| Author, year . | Clinical responsibility . | Healthcare professionals’ team . | Conditions treated . | HaH model . | Technology enabled?a . |
|---|---|---|---|---|---|
| Chen, 2024 [22] | Consultant geriatrician/community specialist nurse | Nurse, ANP, SN, ACP, consultant geriatrician, GP, OT, PT, speech therapist, pharmacist, administration staff, PA | Unspecified—‘older patients with a range of conditions’ | Admission avoidance and early discharge Home visits and telephone calls by staff | No |
| Dismore, 2018 [23] | Respiratory consultant | Respiratory specialist nurse, respiratory consultant, GP | COPD | Early discharge, nurse led Home visits 1–2× daily by nurses | No |
| Dowell, 2018 [24] | Paramedics, nurses and physiotherapists | Nurse, GP, PT, specialist paramedic | Unwell adult pathway, COPD, UTI, palliative, IV, cellulitis, falls | Admission avoidance, 24 h Referral triage system | No |
| Gunnell, 2000 [25] | Not stated | Not stated | Fracture, elective orthopaedic surgery, stroke, dementia | Early discharge | No |
| Health Innovation Network, 2021 [26] | 2 consultant geriatricians, 1 respiratory consultant, rapid response GP | Nurse, consultant geriatrician, respiratory consultant, GP, project lead, rapid response matron | COVID-19 | Admission avoidance, 8 a.m.–8 p.m., 7 days a week Staff contacted patient via phone/video call, home visits. Out-of-hours service (111/999) Wearable integrated with tablet. Home hub connects wearable to cloud. Vital signs continuously collected and displayed on web dashboard for remote monitoring team | Yes |
| Jester, 2002 [27] | Orthopaedic surgeon | Nurse, orthopaedic consultant, PT | Hip/knee replacement surgery recovery | Early discharge, home visits from nurse/PT at least 1× a day. 7 days a week, 8 a.m.–8 p.m. Out of hours: senior on-call nurse | No |
| Karacaoglu, 2021 [28] | Clinical guidance from consultant geriatrician | ANP, consultant geriatrician, OT, PT, pharmacist, healthcare support worker | Geriatric syndrome | Early discharge providing rehabilitation support and home visits from nursing, PT, OT | No |
| Kirkcaldy, 2017 [29] | Not stated | Nurse, OT, PT, pharmacist, social care, community matron | Unspecified ‘older patients with a range of conditions’ | Admission avoidance—has medicines management team that delivers support to increase adherence | No |
| Knowelden, 1991 [30] | GP | Nurse, GP | Metastatic neoplasm, early discharge post-surgery, stroke | Early discharge, mainly district nurse led with home visits | No |
| Kotb, 2023 [31] | Consultant cardiologist | Nurse, ACP, cardiology consultant, registrar, pharmacist | Atrial fibrillation, atrial flutter and fast ventricular response | Admission avoidance, early discharge. 7-days-per-week service, 9 a.m.–5 p.m. Out of hours: on-call cardiology registrar/emergency services Provided with ECG devices, Bluetooth blood pressure monitor, pulse oximeter, smartphone app to record readings/symptom severity. If readings exceed threshold, patients and healthcare team notified. In-app messaging, telephone, video calls | Yes |
| Makela, 2020 [32] | Geriatrician | ANP, consultant geriatrician, GP, speciality training doctor, OT, PT, speech therapist, pharmacist, social care | Falls, delirium, COPD, back pain, cellulitis, chest infection, other | Admission avoidance—7 days a week, 9 a.m.—early evening. Emergency medical cover available 24 h a day. Primary care support | No |
| Ojoo, 2002 [33] | Respiratory outreach nurse | Respiratory specialist nurse | COPD | Early discharge—9 a.m.–5 p.m., monitor patients daily. Out-of-hours services—Medical Chest Unit direct line | No |
| Saleh, 2024 [34] | Cardiology consultant | Nurse, digital technology specialist nurse, ANP, cardiology consultant, registrar, allied healthcare professionals | Atrial fibrillation | Admission avoidance, early discharge. 8 a.m.–8 p.m. Out-of-hours signposting to 111/999 Weekly MDT meetings to discuss HaH patients FIBRICHECK remote monitoring app. Measurements and symptom severity recorded into app twice daily. Monitored by hub, where a dashboard of patients’ clinical data could be reviewed by clinicians twice daily | Yes |
| Schiff, 2022 [35] | Not stated | Not stated | COVID-19 | Admission avoidance, early discharge | No |
| Schofield, 2005 [36] | Respiratory consultant | Respiratory specialist nurse, respiratory consultant | COPD | Early discharge, 9 a.m.–5 p.m. Respiratory nurses do home visits and outreach treatment | No |
| Shepperd, 1998 [37] | GP | ANP, doctors, allied health professionals | Hip/knee replacement recovery, older medical patients, COPD | Admission avoidance, early discharge. Home visits, observations, administration of drugs such as IV, rehabilitation Patients provided mobile phones if needed | No |
| Shepperd, 2021 [38] | Geriatrician | Nurse, consultant geriatrician, speciality training doctor, OT, PT, speech therapist, pharmacist, social care | Dementia, falls, respiratory. gastrointestinal, musculoskeletal disorders, cardiovascular conditions, UTI | Admission avoidance—7 days a week, some sites offered 24-h care, but most were 9 a.m. to early evening. Emergency medical cover available 24 h a day. Primary care support | No |
| Thornton, 2023 [39] | Not stated | Nurse, doctors | Unspecified | Admission avoidance, early discharge Technology for monitoring considered in definition of HaH | Yes |
| Vindrola-Padros, 2021 [40] | GP/consultant depending on site | Nurse, ANP, respiratory specialist nurse, consultant, GP, registrar, senior and junior clinicians, PT, pilot site lead, OPAT nurse, practice manager, PA | COVID-19 | Admission avoidance, early discharge. Regular monitoring calls from primary or secondary care staff. Provided with pulse oximeter, digital app or paper diary to record observations. If patient observation exceeded ‘safe threshold’, patients and clinical team notified | Yes |
| Wilson, 2002 [41] | GP | Nurse, GP, OT, PT, generic health worker | Cardiovascular and respiratory conditions | Admission avoidance, 4–24-h care. Home visits by nurses | No |
| Author, year . | Clinical responsibility . | Healthcare professionals’ team . | Conditions treated . | HaH model . | Technology enabled?a . |
|---|---|---|---|---|---|
| Chen, 2024 [22] | Consultant geriatrician/community specialist nurse | Nurse, ANP, SN, ACP, consultant geriatrician, GP, OT, PT, speech therapist, pharmacist, administration staff, PA | Unspecified—‘older patients with a range of conditions’ | Admission avoidance and early discharge Home visits and telephone calls by staff | No |
| Dismore, 2018 [23] | Respiratory consultant | Respiratory specialist nurse, respiratory consultant, GP | COPD | Early discharge, nurse led Home visits 1–2× daily by nurses | No |
| Dowell, 2018 [24] | Paramedics, nurses and physiotherapists | Nurse, GP, PT, specialist paramedic | Unwell adult pathway, COPD, UTI, palliative, IV, cellulitis, falls | Admission avoidance, 24 h Referral triage system | No |
| Gunnell, 2000 [25] | Not stated | Not stated | Fracture, elective orthopaedic surgery, stroke, dementia | Early discharge | No |
| Health Innovation Network, 2021 [26] | 2 consultant geriatricians, 1 respiratory consultant, rapid response GP | Nurse, consultant geriatrician, respiratory consultant, GP, project lead, rapid response matron | COVID-19 | Admission avoidance, 8 a.m.–8 p.m., 7 days a week Staff contacted patient via phone/video call, home visits. Out-of-hours service (111/999) Wearable integrated with tablet. Home hub connects wearable to cloud. Vital signs continuously collected and displayed on web dashboard for remote monitoring team | Yes |
| Jester, 2002 [27] | Orthopaedic surgeon | Nurse, orthopaedic consultant, PT | Hip/knee replacement surgery recovery | Early discharge, home visits from nurse/PT at least 1× a day. 7 days a week, 8 a.m.–8 p.m. Out of hours: senior on-call nurse | No |
| Karacaoglu, 2021 [28] | Clinical guidance from consultant geriatrician | ANP, consultant geriatrician, OT, PT, pharmacist, healthcare support worker | Geriatric syndrome | Early discharge providing rehabilitation support and home visits from nursing, PT, OT | No |
| Kirkcaldy, 2017 [29] | Not stated | Nurse, OT, PT, pharmacist, social care, community matron | Unspecified ‘older patients with a range of conditions’ | Admission avoidance—has medicines management team that delivers support to increase adherence | No |
| Knowelden, 1991 [30] | GP | Nurse, GP | Metastatic neoplasm, early discharge post-surgery, stroke | Early discharge, mainly district nurse led with home visits | No |
| Kotb, 2023 [31] | Consultant cardiologist | Nurse, ACP, cardiology consultant, registrar, pharmacist | Atrial fibrillation, atrial flutter and fast ventricular response | Admission avoidance, early discharge. 7-days-per-week service, 9 a.m.–5 p.m. Out of hours: on-call cardiology registrar/emergency services Provided with ECG devices, Bluetooth blood pressure monitor, pulse oximeter, smartphone app to record readings/symptom severity. If readings exceed threshold, patients and healthcare team notified. In-app messaging, telephone, video calls | Yes |
| Makela, 2020 [32] | Geriatrician | ANP, consultant geriatrician, GP, speciality training doctor, OT, PT, speech therapist, pharmacist, social care | Falls, delirium, COPD, back pain, cellulitis, chest infection, other | Admission avoidance—7 days a week, 9 a.m.—early evening. Emergency medical cover available 24 h a day. Primary care support | No |
| Ojoo, 2002 [33] | Respiratory outreach nurse | Respiratory specialist nurse | COPD | Early discharge—9 a.m.–5 p.m., monitor patients daily. Out-of-hours services—Medical Chest Unit direct line | No |
| Saleh, 2024 [34] | Cardiology consultant | Nurse, digital technology specialist nurse, ANP, cardiology consultant, registrar, allied healthcare professionals | Atrial fibrillation | Admission avoidance, early discharge. 8 a.m.–8 p.m. Out-of-hours signposting to 111/999 Weekly MDT meetings to discuss HaH patients FIBRICHECK remote monitoring app. Measurements and symptom severity recorded into app twice daily. Monitored by hub, where a dashboard of patients’ clinical data could be reviewed by clinicians twice daily | Yes |
| Schiff, 2022 [35] | Not stated | Not stated | COVID-19 | Admission avoidance, early discharge | No |
| Schofield, 2005 [36] | Respiratory consultant | Respiratory specialist nurse, respiratory consultant | COPD | Early discharge, 9 a.m.–5 p.m. Respiratory nurses do home visits and outreach treatment | No |
| Shepperd, 1998 [37] | GP | ANP, doctors, allied health professionals | Hip/knee replacement recovery, older medical patients, COPD | Admission avoidance, early discharge. Home visits, observations, administration of drugs such as IV, rehabilitation Patients provided mobile phones if needed | No |
| Shepperd, 2021 [38] | Geriatrician | Nurse, consultant geriatrician, speciality training doctor, OT, PT, speech therapist, pharmacist, social care | Dementia, falls, respiratory. gastrointestinal, musculoskeletal disorders, cardiovascular conditions, UTI | Admission avoidance—7 days a week, some sites offered 24-h care, but most were 9 a.m. to early evening. Emergency medical cover available 24 h a day. Primary care support | No |
| Thornton, 2023 [39] | Not stated | Nurse, doctors | Unspecified | Admission avoidance, early discharge Technology for monitoring considered in definition of HaH | Yes |
| Vindrola-Padros, 2021 [40] | GP/consultant depending on site | Nurse, ANP, respiratory specialist nurse, consultant, GP, registrar, senior and junior clinicians, PT, pilot site lead, OPAT nurse, practice manager, PA | COVID-19 | Admission avoidance, early discharge. Regular monitoring calls from primary or secondary care staff. Provided with pulse oximeter, digital app or paper diary to record observations. If patient observation exceeded ‘safe threshold’, patients and clinical team notified | Yes |
| Wilson, 2002 [41] | GP | Nurse, GP, OT, PT, generic health worker | Cardiovascular and respiratory conditions | Admission avoidance, 4–24-h care. Home visits by nurses | No |
Note: Gunnel et al. did not specify specific staffing in HaH model. ANP, advanced nurse practitioner; ACP, advanced clinical practitioner; OPAT, outpatient parenteral antimicrobial therapy; OT, occupational therapist; PA, physician’s associate; PT, physiotherapist; SN, nurse specialist; UTI, urinary tract infection.
aNHS definition of technology-enabled HaH consists of the following criteria [49]:
1. Patients measuring and inputting their health data into an application/done automatically via wearable or Bluetooth.
2. Data feeds into digital platform where the clinical team can review.
3. Clinical teams are alerted when patient moves outside of safe parameters, and can act accordingly.
Perceptions of virtual wards
Six themes were generated from included studies and are represented in a concept map detailed in Figure 2.1
Familiarity of home versus a hospital environment
Studies highlighted home being the most comfortable environment for recovery due to better social support, sleep, nourishment and stress levels [22, 23, 27, 32, 35, 36, 41]: ‘You’re in your own surroundings which helps you get better quicker’ (HaH patient) [41]. Home familiarity in HaHs was found to positively influence patient confidence and independence, with HaH staff reporting their role in building this confidence during home assessment [22, 23, 25, 26, 32, 35, 37, 41]. It also helped mitigate distress for patients experiencing acute confusion and delirium due to unfamiliar hospital surroundings [22, 32]. Patients and carers across studies appreciated not being separated from their family [23, 24, 27, 35, 41]: ‘Having his family around him was the most important thing for him, and Hospital at Home allowed that to happen’ (Relative to COVID-19 HaH patient) [35].
Common negative hospital experiences described were in regard to poor cleanliness, nutrition and sleep disruption due to noise, nightly observations and lack of privacy [23, 33, 36, 41]. Carers faced challenges related to travel, restrictive visiting hours, absence of familial support and parking costs, making hospital stays less favourable [23, 27, 41]. However, it was not all negative for hospitals, as there was a balance to be struck between the value of the home environment versus the timely access to specialist care and equipment offered in hospital [35, 41].
Person-centred care
Person-centred care delivered by the HaH team was consistently recognised as a strength of care delivery by patients, carers and staff. HaH nurses were frequently commended for their clear explanations of treatment plans, active listening and rapport-building—often described to be ‘friendly’, ‘respectful’, ‘approachable’, ‘excellent’ and ‘caring’ [23–27, 30, 33, 34, 36, 38, 41]. Patients and carers especially appreciated the ‘one-to-one’ care relationship with nurses [23, 26, 41]: ‘I think you got more attention… it seems as if you are the only one…’ (HaH patient) [41]. Studies described similar or reduced carer burden, and higher carer satisfaction scores with HaHs compared to hospital [22, 25–27, 35, 37, 41]. Several frail family carers reported appreciation for the attention they received from HaHs: ‘…the home care nurses, they couldn’t have done more for him… and they looked after me.’ (HaH family carer) [41].
Enabling shared decision-making
Staff were identified to provide well-informed and up-to-date information on patient progress, particularly on discharge plans, additional equipment needs, home adaptations and service referrals [24, 25, 30, 31, 33, 36, 38, 39]. They enabled shared decision-making by eliciting patient and carer ideas and concerns regarding HaH care delivery [24, 25, 30, 31, 33, 36, 38, 39]: ‘It gives us a chance to be more involved in treatment and understanding the problem…’ (Patient onboard an atrial fibrillation HaH) [31]. Within papers that scored participants’ experiences, HaH patients and carers reported higher levels of satisfaction with discussions with healthcare staff and involvement in care decisions compared to usual hospital care groups [25, 38]. This was often contrasted with previous patient and carers’ lack of involvement in decision-making in hospital settings, where perceptions of NHS staff ‘rushing to empty beds’ meant care was transactional and less personalised compared to HaHs [32].
Challenges with staff and information accessibility
Family carers reported instances where HaH staff should have visited more frequently, with a lack of continuous ‘visible’ staff impacting their perceptions of HaH effectiveness [27, 31]. Makela et al. identified the role of carers acting as a ‘bridge to continuity of healthcare’ and facilitating HaH care [32]. Dissatisfaction with HaH care delivery arose when patients and carers reported difficulty contacting staff and obtaining patient records and goals set by the HaH team [27, 31–33]. The absence of written communication summaries reduced clarity for patients and carers post-discharge from HaHs, describing these as a form of communication between professionals rather than for patients [31, 32, 40].
Karacaoglu et al. and Vindrola-Padros et al. raised the challenges in delivering a 7-day service due to clinical lead unavailability, challenges with recruiting senior clinicians or having sufficient cover for HaHs to operate [28, 40]. Allied healthcare professionals and pharmacists cited difficulty in accessing GP patient health records [29]. Integrating HaH patient data with primary care record systems like EMIS and expansion of referral pathways to more acute departments were recognised facilitators for continuity of care in future practice [26, 28, 32].
Safety of HaH
Patient and family carers recognised safety as a priority in hospitals and raised concerns that HaHs required increased carer involvement and responsibility in monitoring patients, highlighting patient vulnerability at night when HaH staff were not present [22, 23, 27, 32, 41]: ‘it’s like sleeping with one eye open…’ (Family carer) [32].
However, some patients, especially those living alone, valued the provision of accessible telephone numbers, nurses’ encouragement to call with concerns and scheduled evening phone calls from healthcare professionals [22, 23, 41]:‘They all seemed to me to be very well trained and put me at ease’ (Patient in COPD HaH) [23].
Managing technology at home
Older people and their carers faced difficulty with HaH technology, including concerns about personal data privacy and patient anxiety or aversion to technology [26, 31, 34, 39, 40]. Staff concerns focused on digital exclusion as a barrier to HaH implementation, highlighting the need for a minimum level of patient digital literacy and access to devices for monitoring applications [26, 39, 40]. Saleh et al. and Vindrola-Padros et al. noted a lack of culturally appropriate resources in different languages, contributing to digital exclusion for non-English speakers [34, 40].
Despite this, many older people and their carers responded positively to digital technology [26, 31]. A key facilitator for HaH care delivery was the promotion of digital health education and clear explanations from healthcare professionals to build patient confidence in using technology [26, 31, 34, 39, 40]. Flexibility in equipment to enhance digital inclusion was demonstrated by using physical pulse oximeters for patients without compatible smartphones [34].
Discussion
Our findings indicate that person-centred care, rapport-building, home familiarity and shared decision-making are key components of HaHs from the perspectives of patients and family carers. Concerns included staff availability, digital literacy and carers’ anxiety about managing care, especially at night, without the reassurance of in-person HaH staff support. A summary of positive and negative themes with recommendations are provided in box 1.
Summary of positive and negative themes with recommendations.
Positive themes
Improved wellbeing and independence at home
Person-centred, ‘one-to-one’ care
Strong patient–staff relationship
HaH nurses identifying frail family carers
Staff keeping patients and carers well informed on progress, treatment and discharge plans, enabling shared decision-making
Clear explanations from staff to empower patients with technology use
Negative themes with recommendations
Lack of staff during the night
Recommendation: Scheduled evening phone calls with HaH staff, centralised overnight support service
HaHs required increased carer responsibility in monitoring patients
Recommendation: Use wearable devices that automatically send patient data to healthcare teams, provide comprehensive training programmes for carers on how to recognise warning signs, establish carer support services
Carers found difficulty contacting staff and obtaining patient records
Recommendation: Clear signposting of staff contact numbers, implementing cloud-based systems for real-time updates and syncing of patient records across teams
Difficulty accessing GP patient health records between teams
Recommendation: Integrate HaH patient data with other health record systems, expansion of referral pathways to more acute departments
Digital exclusion of older adult patients
Recommendation: Digital health education with patients and carers to build confidence, providing alternative equipment for those without compatible smartphones
Care environments
The therapeutic value of receiving care in a familiar home environment was a key driver for patient confidence, independence and recovery, especially for older people with dementia [22, 23, 27, 32, 35, 36, 41]. Despite views that hospital provided more specialised care and equipment compared to HaHs, there was a strong feeling from patients and carers regarding ‘disruptive hospital’ environments, reinforcing overarching preferences and satisfaction with home-based HaH care [23, 35, 36, 41].
Home supports the preservation of self-identity in older people, rather than reducing them to the role of a patient [50, 51]. Recognition of the benefits of a ‘small homelike environment’ for older people with dementia aligns with patient and carer preferences cited in this review [52–55]. Harreman et al. conceptualises ‘ageing in place’ as the process of a house becoming more than a physical space, deeply connected to personal identity [56]. This supports HaH care models, as it allows older people to preserve their autonomy, whilst maintaining the relationships that are central to their sense of self [50, 51, 57, 58].
Availability of family carer support
This review reveals a significant lack of carer representation in rigorous HaH studies, highlighting a research gap in the support and involvement of family carers. Although carer views were included and highly valuable for analysis in this review, the total number of carers participating was significantly lower than that of patients. This is an important omission, as the experiences of carers may be very different to care recipients. This difference in research participation may be due to carer-specific barriers such as a lack of time, managing their own health problems and the challenges of balancing active research involvement with their caring responsibilities [59].
Use of technology with older people
The UK Office of National Statistics consistently show older people as the largest proportion of adult internet non-users [60]. This age-related digital divide contributes to older adult hesitancy of HaH implementation and is further exacerbated by age-related barriers such as cognitive decline and physical impairments making technology use difficult [61–64]. Although the atrial fibrillation and COVID-19 HaHs in this review tailored care strategies to promote digital inclusion, there was no discussion of how to accommodate individuals with cognitive impairment using these technologies [26, 31, 34, 40].
Public perceptions of equating HaH care delivery with solely ‘virtual consultations’ may discourage older people who typically prefer face-to-face care [39]. However, since COVID-19, the increase in teleconsultation adoption amongst older people highlights a significant shift in digital engagement and potential for sustained digital integration within this demographic [65].
Implications and recommendations to practice, policy and research
Our findings highlight the importance of patient, carers and healthcare professional’s perceptions in optimising HaH care delivery. Future research should include more diverse perspectives from these stakeholder groups to align HaH models with user and provider needs.
Clear summaries of HaH care pathways can aid with clarifying HaH terminology for older people to enhance acceptance and understanding. Meanwhile, standardising communication protocols amongst healthcare providers can enable better information sharing. Policy initiatives should prioritise culturally appropriate digital care to increase digital education and equitable access to HaHs, such as simplified interfaces or supportive web platforms [66, 67].
Public Health England’s rapid review identified unpaid caring as a social determinant of health and a need for higher quality estimates of carer burden [68]. This mirrors gaps in HaH carer support services, indicating the need for greater carer inclusion in research to develop evidence-based systems that ease carer burden [69, 70]. There may be value in implementing systems to provide and signpost family carers to services that address their physical and emotional needs during their time caring for individuals onboard HaHs. Whilst not within the scope of this review, UK HaH systems can draw useful insights and apply study findings from global models in the Netherlands, USA, Singapore and Australia that focus on family carer strain experiences, thus enriching UK research on these outcomes [71–76].
Strengths and limitations
This review uses a broad systematic search strategy. A key strength is the inclusion of carer representation via PPI, amplifying often underrepresented carer voices and enhancing the relevance of findings and recommendations [77]. Only studies published in the UK and in English were included, so findings may not be applicable to other settings; however, the key messages may be considered in similar systems and settings to those in the UK. Quality appraisal revealed limited ethnic diversity in participant demographics, limiting representation of their experiences. Inconsistencies of how HaHs are defined and labelled across studies may have overlooked relevant results that do not include the terms ‘Virtual Ward’ or ‘Hospital at Home’, but the iterative development and broad variety of terms in the search potentially mitigates this risk. As this paper focusses on different conditions across the HaH models, the experiences on each might not be universally applicable. However, the core themes presented such as familiarity in the home environment, carer burden and provision of person-centred care should overlap between care models.
Conclusion
From patient, carer and healthcare professional perspectives, the value of care provision at home for older people embodies autonomy, dignity and faster recovery. However, empowerment is key to facilitate older people’s digital engagement. HaHs allow for a holistic approach in addressing older people’s care needs, with potential support for carers too. Carers play a significant role in providing a link between HaH care and older people. Yet, it is unknown how to best implement carer support; therefore, future studies should focus on devising sustainable carer support systems within HaHs and gather their perspectives to further optimise patient, carer wellbeing and satisfaction with HaH services.
Acknowledgements
We would like to thank our PPIE members for the support and contributions.
Declaration of Conflicts of Interest
None declared.
Declaration of Sources of Funding
This review was completed as part of an iBSc project.
Footnotes
All themes stem from general satisfaction with HaHs. The green arrows represent positive perspectives and experiences, highlighting facilitators and the link between themes. For example: the familiarity of home environment facilitates shared decision-making as older people and family carers are more confident and comfortable at home. The red arrows highlight concerns and barriers in relation to and between themes. For example: experiences of increased carer responsibility led to their anxiety at night when the HaH staff were not present are barriers to HaH safety. The double-headed arrow represents the mutual influence between person-centred care and shared decision-making within HaHs.




Comments