-
PDF
- Split View
-
Views
-
Cite
Cite
Lisa McGarrigle, Yang Yang, Reena Lasrado, Matthew Gittins, Chris Todd, A systematic review and meta-analysis of the measurement properties of concerns-about-falling instruments in older people and people at increased risk of falls, Age and Ageing, Volume 52, Issue 5, May 2023, afad055, https://doi.org/10.1093/ageing/afad055
Close - Share Icon Share
Abstract
The 16-item Falls Efficacy Scale International (FES-I) is widely used to assess concerns-about-falling. Variants include 7-item Short FES-I, 30-item Iconographical Falls Efficacy Scale (Icon FES) and 10-item short Icon FES. No comprehensive systematic review and meta-analysis has been conducted to synthesise evidence regarding the measurement properties of these tools.
To conduct a systematic review and meta-analysis of the measurement properties of four FES-I variants.
MEDLINE, Embase, CINAHL Plus, PsycINFO and Web of Science were searched systematically and articles were assessed for eligibility independently. The methodological quality of eligible studies was assessed using COnsensus-based Standards for the selection of health Measurement INstruments (COSMIN) Risk of Bias checklist. The quality of measurement properties was assessed using COSMIN criteria for good measurement properties. Where possible, meta-analysis was conducted; otherwise, narrative synthesis was performed. Overall certainty of evidence was rated using a modified Grading of Recommendations, Assessment, Development and Evaluation system approach.
The review included 58 studies investigating measurement properties of the four instruments. There was high-quality evidence to support internal consistency, reliability and construct validity of all instruments. Moderate- to high-certainty evidence suggests one-factor structure of FES-I with two underlying dimensions, one-factor structure of Short FES-I and two-factor structure of Icon FES. There was high-certainty evidence to support the responsiveness of FES-I, with further research needed for the other instruments.
There is evidence for excellent measurement properties of all four instruments. We recommend the use of these tools with healthy older people and people at a greater risk of falls due to conditions that might affect mobility and balance.
Key Points
A comprehensive systematic review of the measurement properties of Falls Efficacy Scale International variants is lacking.
This review includes 58 studies on reliability, validity, responsiveness, feasibility and/or interpretability of four tools.
There is evidence for excellent measurement properties of all four instruments.
We recommend use with healthy older people and people at risk of falls (conditions that might affect mobility/balance).
These findings contributed to the World Guidelines for Falls Prevention in Older Adults.
Background
The 16-item Falls Efficacy Scale International (FES-I) and 7-item Short FES-I are widely used and accepted tools in the assessment of fear of (or more correctly) concerns-about-falling [1–4]. The tool was designed to address the need for a concerns-about-falling measure that accounted for both physical and social factors and was appropriate for cross-cultural use [3]. FES-I was initially developed following a review of concerns-about-falling instruments conducted by the Prevention of Falls Network Europe group [4]. The development built on and improved the original Falls Efficacy Scale (FES) [5], particularly in relation to more demanding and social activities and cross-cultural differences. The term ‘Falls Efficacy’ has been retained in the FES-I in order to acknowledge its origins; however, the purpose of the scale is to assess ‘concern’ about falling, a term closely related to fear, but less emotionally loaded [3]. Iconographical Falls Efficacy Scale (Icon FES) long version (30-item) and short version (10-item) were developed to assess concerns-about-falling in cognitively impaired individuals [6]. Many studies have investigated the measurement properties [7] of the various versions of FES-I [8, 9], but, to date, no comprehensive systematic review has been conducted to synthesise evidence regarding the measurement properties of these tools.
The objective of this study was to conduct a systematic review and meta-analysis of the measurement properties (structural validity, internal consistency, test-retest and inter-rater reliability, measurement error, construct validity, responsiveness) and interpretability and feasibility of FES-I instruments.
Methods
The study protocol was registered with PROSPERO (registration number: CRD42019161462). We followed the COnsensus-based Standards for the selection of health Measurement INstruments (COSMIN) methodology for systematic reviews of patient-reported outcome measures (PROMs) [10].
Search strategy and selection criteria
There are often multiple studies on different measurement properties described in one published, peer-reviewed article, thus we only use the term articles in relation to our literature search. Thereafter, we use the term studies to reflect individual studies reported in the articles. We followed COSMIN recommendations to develop our search terms (Supplementary Appendix A), searched MEDLINE (Ovid), CINAHL Plus (EBSCO), PsycINFO (Ovid), Embase (Ovid) and Web of Science, and included articles published from 2005 (the first FES-I publication) to October 2020, limited to title, abstract and index terms. In December 2020, a Google Scholar search was performed and all articles that cited the original FES-I development paper [3] were checked for eligibility. Original full-text articles were considered for inclusion if the main objective was to assess at least one measurement property OR interpretability/feasibility in any population, setting or language.
Article selection
Two independent reviewers (L.M. and R.L.) examined titles and abstracts for eligibility. Disagreements were resolved through discussion with a third reviewer (C.T.). Full texts of potentially relevant articles were obtained and independently assessed against the inclusion criteria by two independent reviewers (L.M. and Y.Y.), and, again, disagreement was resolved through discussion with a third reviewer (C.T.).
Data extraction
Data were extracted from included articles using standardised COSMIN forms that included authors, publication year, sample size, subject characteristics (e.g. age, gender [11]1, disease condition), type of study, intervention (if applicable), language and country. All available measurement property data were extracted independently by two reviewers (L.M. and Y.Y.) for 22 of 58 (38%) included papers. For the remaining papers, one reviewer (Y.Y.) extracted data, which was checked by a second reviewer (L.M.). Data included structural validity (factor analysis results on dimensionality), internal consistency (Cronbach’s alpha), reliability (intraclass/Pearson/Spearman correlations), measurement error (standard error of measurement; smallest detectable change), construct validity (convergent validity—correlation of FES-I instruments with comparator measures; and known-groups validity—comparison of FES-I instrument scores between two subgroups using relative effect sizes or area under the receiver operating curve) and responsiveness to change (relative effect sizes). Where convergent validity was assessed by correlating FES-I variants (including the original FES measure), data were not included due to a high risk of bias from overlap of items across measures. Criterion validity was not evaluated due to the lack of an established gold standard measure for concerns-about-falling with which to compare the FES-I instruments. Content validity was not evaluated as it is already well established in the literature (Supplementary Appendix B for a short overview). Interpretability included distribution of scores, percentage of missing items and total scores, and floor and ceiling effects. Feasibility included completion time, ease of administration, patient comprehensibility and clinician comprehensibility.
Assessment of risk of bias
Two reviewers (L.M. and Y.Y.) independently assessed methodological quality of each study using the COSMIN Risk of Bias (RoB) Checklist [12] (rated ‘very good’, ‘adequate’, ‘doubtful’ or ‘inadequate’). Disagreements were resolved through discussion with a third reviewer (C.T.).
Evaluation of measurement properties
The rating of each measurement property result was evaluated using the COSMIN updated criteria for good measurement properties [10] and rated sufficient (+), insufficient (−) or indeterminate (?). Additional criteria were developed for the assessment of structural validity (Supplementary Appendix C). Specific hypotheses were developed for construct validity and responsiveness (Supplementary Appendix D). All results per measurement property for each instrument were then qualitatively summarised and, where possible, quantitatively pooled, and this summarised and/or pooled result was again evaluated against the criteria for good measurement properties to get an overall rating.
Data synthesis and analysis
Where possible, data relating to internal consistency, reliability and construct validity were quantitatively pooled. We pooled results where three or more studies reported the required parameter estimates including standard errors for meta-analysis. The individual study measurement properties were pooled using restricted maximum-likelihood random-effects meta-analysis to produce pooled effect sizes, or correlations, or Cohen’s d effect sizes (and 95% confidence intervals). Where meta-analysis was not appropriate, if we had three or more studies but did not have suitable standard errors, we have reported weighted means. The pooled result was then compared against the COSMIN criteria for good measurement properties to determine whether, overall, the measurement properties of each FES-I instrument were sufficient (+), insufficient (−) or indeterminate (?). Where it was not possible to pool results statistically, results were descriptively summarised. These were again compared against the COSMIN criteria for good measurement properties. Where results were found to be inconsistent (±) (i.e. fewer than 75% of results supporting a particular conclusion), we sought to find explanations based on subgroups, or based the conclusions on the majority of consistent results, and downgraded for inconsistency during Grading of Recommendations, Assessment, Development and Evaluation system (GRADE) assessment. Where no explanations could be found or where there was no clear majority supporting a particular conclusion, we did not interpret the result or perform GRADE assessment.
Subgroup analysis
Where number of studies available allowed (>3), we repeated the meta-analysis for subgroups to evaluate properties based on the methodological quality of the study (RoB assessment) and the study population. We were interested in whether properties varied between populations that were generally healthy and those with conditions that might affect mobility and balance, thus at a higher risk of falling. As such, we compared results between two broad groupings: generally healthy older people and people with conditions that might affect mobility and balance (e.g. stroke, Parkinson’s disease, multiple sclerosis, vestibular disorders, dystonia, vertigo).
Where it was not possible to pool results, we explored subgroup differences where results appeared inconsistent. First, we excluded studies of low methodological quality (doubtful or inadequate RoB ratings). If inconsistency remained, if possible, we further investigated results by other characteristics (e.g. population). We explored results on interpretability and feasibility in relation to population (generally healthy older people vs. people with conditions that might affect mobility and balance) and mode of administration (interview vs. self-report).
Grading of Recommendations, Assessment, Development and Evaluation
The certainty of the evidence was graded by two independent reviewers (Y.Y., L.M.) using modified GRADE approach outlined by COSMIN (high, moderate, low, very low). The following three factors were assessed: (i) risk of bias (i.e. the methodological quality of the studies), (ii) inconsistency (i.e. unexplained inconsistency of results across studies) and (iii) imprecision (i.e. total sample size of the available studies).
Results
Study characteristics
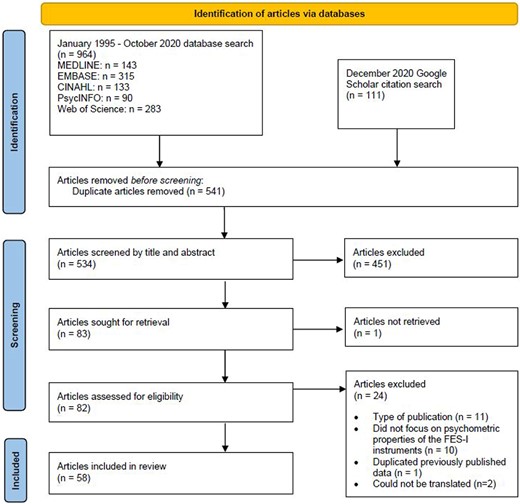
The search identified 534 articles, 58 of which were included in the review (Figure 1). Key study characteristics are summarised in Table 1, with full characteristics included in Supplementary Appendix E. Characteristics of the included FES-I instruments are summarised in Supplementary Appendix F. The majority of articles (n = 52) were in English. Six non-English-language articles were translated using Google Translate. An overview of the measurement properties reported in each article is provided in Supplementary Appendix G.
Measurement properties
Below and in Table 2, we present an overview of the measurement properties of the four instruments. Full results are provided in Supplementary Appendices H (Results Table) and I (Summary of Findings). Note that it was not possible to evaluate measurement error (an indicator of reliability) following COSMIN guidelines [67] as minimal important change (MIC) was not presented in the literature. Although we did not evaluate this property, we summarise any available information reported on it in Supplementary Appendices H and I.
| PROM . | Author . | Age (mean years) . | Disease/condition . | Setting . |
|---|---|---|---|---|
| FES-I | Alghadir 2015 [13] | 32.5 | Vestibular disorders | Outpatient dizziness centre |
| Azad 2014 [14] | 60.1 | Stroke | Outpatient neurological clinics | |
| Baharlouei 2013 [15] | 69.2 | – | Rehabilitation centres and nursing homes | |
| Billis 2011 [16] | 72.9 | – | Community | |
| Boyce 2017 [17] | 52 | Dystonia | Community | |
| Camargos 2010 [18] | 73.4 | – | Community | |
| Choobsaz 2020 [19] | 35.1 | MS | Community | |
| Figueiredo 2017 [20] | 74.3 | – | Community | |
| Figueiredo 2018 [21] | 81.9 | – | Day care service users | |
| Friscia 2014 [22] | 56 | Vertigo, dizziness, unsteadiness | Neurotology clinic | |
| Greenberg 2016 [23] | 77 | Multiple chronic conditions | Community | |
| Halaweh 2016 [24] | 67.3 | – | Community | |
| Halvarsson 2013 [25] | 76.5 | Osteoporosis, balance problems, CaF | Community | |
| Halvarsson 2018 [26] | 76 | Osteoporosis, balance problems, CaF | Community | |
| Hauer 2010 [27] | 81.7 | Cognitive impairment | Geriatric rehabilitation | |
| Hill 2014 [28] | 74.7 | – | Community | |
| Jonasson 2014 [29] | 73 | Parkinson’s disease | Outpatient clinic | |
| Kempen 2007a [30] | 76.8 | – | Community | |
| Kempen 2007b [31] | 76.6 | – | Community | |
| Kisvetrová 2019 [32] | 80 | People with dementia | Geriatric and neurological outpatient clinics | |
| Kovács 2018 [33] | 70.4 | – | Community | |
| Lipardo 2020 [34] | 69.4 | – | Community | |
| Lomas-Vega 2012 [35] | 57.5 | Post-menopausal | Community | |
| Marques-Vieira 2018 [36] | 71.1 | – | Community | |
| Martha Anggarani 2020 [37] | 76.3 | – | Nursing homes | |
| Mehdizadeh 2019 [38] | 60.3 | Parkinson’s disease | Movement disorder clinic | |
| Monjezi 2019 [39] | 36 | MS | Community | |
| Moore 2011 [40] | 74.4 | – | Community | |
| Morgan 2013 [41] | 54 | Balance and vestibular dysfunction | Community | |
| Nordell 2009 [42] | 65.5 | Fall-related fracture | Community | |
| Park 2010 [43] | 72.8 | – | Public health centre | |
| Guo 2015 [44] | 72.4 | – | – | |
| Scremim 2020 [45] | 68.3 | COPD | Pulmonary function service | |
| Smee 2015 [46] | 68.1 | – | Community | |
| Thiamwong 2012 [47] | 70.4 | Community | ||
| Ulus 2012 [48] | 69.7 | Ambulation difficulties | Community | |
| Visschedijk 2015 [49] | 83.1 | Hip fracture | Outpatients in skilled nursing facility | |
| Yardley 2005 [3] | 74.7 | Older people with and without fall risk | Community | |
| Short FES-I | del-Rio-Valeiras 2016 [50] | 77.2 | Age-induced balance disorders | Hospital neurology department |
| Deng 2015 [51] | 59.8 | Cerebral infarction | Inpatient neurology departments | |
| Kamide 2018 [52] | 71.4 | – | Community | |
| Kempen 2008 [1] | 76.6 | – | Community | |
| Kim 2017 [53] | 72.6 | Fallers and non-fallers | Community | |
| Mazumder 2015 [54] | 39.6 | MS | Community | |
| Mehta 2015 [55] | 62.6 | Distal radius fracture | Outpatient rehabilitation clinics | |
| Tan 2018 [56] | 73.1 | – | Community | |
| FES-I and Short FES-I | Araya 2017 [57] | 71 | – | Community |
| Delbaere 2010 [2] | 77.4 | – | Community | |
| Hauer 2011 [58] | 82.3 | Cognitive impairment | Geriatric rehabilitation inpatients | |
| Jonasson 2017 [59] | 73 | Parkinson’s disease | Outpatient clinics | |
| Kwan 2013 [60] | 74.9 | – | Community | |
| Ruggiero 2009 [61] | 79.4 | – | Community | |
| van Vliet 2013 [62] | 50.6 | MS | Community | |
| Short Icon FES and Short FES-I | Chan 2018 [63] | 76.8 | – | Community |
| Icon FES and Short Icon FES | Delbaere 2011 [6] | 80.2 | – | Community |
| Delbaere 2013 [64] | 82.1 | Cognitive impairment | Community | |
| Franco 2018 [65] | 71.4 | – | Community | |
| Moreira 2020 [66] | 69.6 | – | Community |
| PROM . | Author . | Age (mean years) . | Disease/condition . | Setting . |
|---|---|---|---|---|
| FES-I | Alghadir 2015 [13] | 32.5 | Vestibular disorders | Outpatient dizziness centre |
| Azad 2014 [14] | 60.1 | Stroke | Outpatient neurological clinics | |
| Baharlouei 2013 [15] | 69.2 | – | Rehabilitation centres and nursing homes | |
| Billis 2011 [16] | 72.9 | – | Community | |
| Boyce 2017 [17] | 52 | Dystonia | Community | |
| Camargos 2010 [18] | 73.4 | – | Community | |
| Choobsaz 2020 [19] | 35.1 | MS | Community | |
| Figueiredo 2017 [20] | 74.3 | – | Community | |
| Figueiredo 2018 [21] | 81.9 | – | Day care service users | |
| Friscia 2014 [22] | 56 | Vertigo, dizziness, unsteadiness | Neurotology clinic | |
| Greenberg 2016 [23] | 77 | Multiple chronic conditions | Community | |
| Halaweh 2016 [24] | 67.3 | – | Community | |
| Halvarsson 2013 [25] | 76.5 | Osteoporosis, balance problems, CaF | Community | |
| Halvarsson 2018 [26] | 76 | Osteoporosis, balance problems, CaF | Community | |
| Hauer 2010 [27] | 81.7 | Cognitive impairment | Geriatric rehabilitation | |
| Hill 2014 [28] | 74.7 | – | Community | |
| Jonasson 2014 [29] | 73 | Parkinson’s disease | Outpatient clinic | |
| Kempen 2007a [30] | 76.8 | – | Community | |
| Kempen 2007b [31] | 76.6 | – | Community | |
| Kisvetrová 2019 [32] | 80 | People with dementia | Geriatric and neurological outpatient clinics | |
| Kovács 2018 [33] | 70.4 | – | Community | |
| Lipardo 2020 [34] | 69.4 | – | Community | |
| Lomas-Vega 2012 [35] | 57.5 | Post-menopausal | Community | |
| Marques-Vieira 2018 [36] | 71.1 | – | Community | |
| Martha Anggarani 2020 [37] | 76.3 | – | Nursing homes | |
| Mehdizadeh 2019 [38] | 60.3 | Parkinson’s disease | Movement disorder clinic | |
| Monjezi 2019 [39] | 36 | MS | Community | |
| Moore 2011 [40] | 74.4 | – | Community | |
| Morgan 2013 [41] | 54 | Balance and vestibular dysfunction | Community | |
| Nordell 2009 [42] | 65.5 | Fall-related fracture | Community | |
| Park 2010 [43] | 72.8 | – | Public health centre | |
| Guo 2015 [44] | 72.4 | – | – | |
| Scremim 2020 [45] | 68.3 | COPD | Pulmonary function service | |
| Smee 2015 [46] | 68.1 | – | Community | |
| Thiamwong 2012 [47] | 70.4 | Community | ||
| Ulus 2012 [48] | 69.7 | Ambulation difficulties | Community | |
| Visschedijk 2015 [49] | 83.1 | Hip fracture | Outpatients in skilled nursing facility | |
| Yardley 2005 [3] | 74.7 | Older people with and without fall risk | Community | |
| Short FES-I | del-Rio-Valeiras 2016 [50] | 77.2 | Age-induced balance disorders | Hospital neurology department |
| Deng 2015 [51] | 59.8 | Cerebral infarction | Inpatient neurology departments | |
| Kamide 2018 [52] | 71.4 | – | Community | |
| Kempen 2008 [1] | 76.6 | – | Community | |
| Kim 2017 [53] | 72.6 | Fallers and non-fallers | Community | |
| Mazumder 2015 [54] | 39.6 | MS | Community | |
| Mehta 2015 [55] | 62.6 | Distal radius fracture | Outpatient rehabilitation clinics | |
| Tan 2018 [56] | 73.1 | – | Community | |
| FES-I and Short FES-I | Araya 2017 [57] | 71 | – | Community |
| Delbaere 2010 [2] | 77.4 | – | Community | |
| Hauer 2011 [58] | 82.3 | Cognitive impairment | Geriatric rehabilitation inpatients | |
| Jonasson 2017 [59] | 73 | Parkinson’s disease | Outpatient clinics | |
| Kwan 2013 [60] | 74.9 | – | Community | |
| Ruggiero 2009 [61] | 79.4 | – | Community | |
| van Vliet 2013 [62] | 50.6 | MS | Community | |
| Short Icon FES and Short FES-I | Chan 2018 [63] | 76.8 | – | Community |
| Icon FES and Short Icon FES | Delbaere 2011 [6] | 80.2 | – | Community |
| Delbaere 2013 [64] | 82.1 | Cognitive impairment | Community | |
| Franco 2018 [65] | 71.4 | – | Community | |
| Moreira 2020 [66] | 69.6 | – | Community |
COPD, chronic obstructive pulmonary disease; CaF, concerns-about-falling; MS, multiple sclerosis.
| PROM . | Author . | Age (mean years) . | Disease/condition . | Setting . |
|---|---|---|---|---|
| FES-I | Alghadir 2015 [13] | 32.5 | Vestibular disorders | Outpatient dizziness centre |
| Azad 2014 [14] | 60.1 | Stroke | Outpatient neurological clinics | |
| Baharlouei 2013 [15] | 69.2 | – | Rehabilitation centres and nursing homes | |
| Billis 2011 [16] | 72.9 | – | Community | |
| Boyce 2017 [17] | 52 | Dystonia | Community | |
| Camargos 2010 [18] | 73.4 | – | Community | |
| Choobsaz 2020 [19] | 35.1 | MS | Community | |
| Figueiredo 2017 [20] | 74.3 | – | Community | |
| Figueiredo 2018 [21] | 81.9 | – | Day care service users | |
| Friscia 2014 [22] | 56 | Vertigo, dizziness, unsteadiness | Neurotology clinic | |
| Greenberg 2016 [23] | 77 | Multiple chronic conditions | Community | |
| Halaweh 2016 [24] | 67.3 | – | Community | |
| Halvarsson 2013 [25] | 76.5 | Osteoporosis, balance problems, CaF | Community | |
| Halvarsson 2018 [26] | 76 | Osteoporosis, balance problems, CaF | Community | |
| Hauer 2010 [27] | 81.7 | Cognitive impairment | Geriatric rehabilitation | |
| Hill 2014 [28] | 74.7 | – | Community | |
| Jonasson 2014 [29] | 73 | Parkinson’s disease | Outpatient clinic | |
| Kempen 2007a [30] | 76.8 | – | Community | |
| Kempen 2007b [31] | 76.6 | – | Community | |
| Kisvetrová 2019 [32] | 80 | People with dementia | Geriatric and neurological outpatient clinics | |
| Kovács 2018 [33] | 70.4 | – | Community | |
| Lipardo 2020 [34] | 69.4 | – | Community | |
| Lomas-Vega 2012 [35] | 57.5 | Post-menopausal | Community | |
| Marques-Vieira 2018 [36] | 71.1 | – | Community | |
| Martha Anggarani 2020 [37] | 76.3 | – | Nursing homes | |
| Mehdizadeh 2019 [38] | 60.3 | Parkinson’s disease | Movement disorder clinic | |
| Monjezi 2019 [39] | 36 | MS | Community | |
| Moore 2011 [40] | 74.4 | – | Community | |
| Morgan 2013 [41] | 54 | Balance and vestibular dysfunction | Community | |
| Nordell 2009 [42] | 65.5 | Fall-related fracture | Community | |
| Park 2010 [43] | 72.8 | – | Public health centre | |
| Guo 2015 [44] | 72.4 | – | – | |
| Scremim 2020 [45] | 68.3 | COPD | Pulmonary function service | |
| Smee 2015 [46] | 68.1 | – | Community | |
| Thiamwong 2012 [47] | 70.4 | Community | ||
| Ulus 2012 [48] | 69.7 | Ambulation difficulties | Community | |
| Visschedijk 2015 [49] | 83.1 | Hip fracture | Outpatients in skilled nursing facility | |
| Yardley 2005 [3] | 74.7 | Older people with and without fall risk | Community | |
| Short FES-I | del-Rio-Valeiras 2016 [50] | 77.2 | Age-induced balance disorders | Hospital neurology department |
| Deng 2015 [51] | 59.8 | Cerebral infarction | Inpatient neurology departments | |
| Kamide 2018 [52] | 71.4 | – | Community | |
| Kempen 2008 [1] | 76.6 | – | Community | |
| Kim 2017 [53] | 72.6 | Fallers and non-fallers | Community | |
| Mazumder 2015 [54] | 39.6 | MS | Community | |
| Mehta 2015 [55] | 62.6 | Distal radius fracture | Outpatient rehabilitation clinics | |
| Tan 2018 [56] | 73.1 | – | Community | |
| FES-I and Short FES-I | Araya 2017 [57] | 71 | – | Community |
| Delbaere 2010 [2] | 77.4 | – | Community | |
| Hauer 2011 [58] | 82.3 | Cognitive impairment | Geriatric rehabilitation inpatients | |
| Jonasson 2017 [59] | 73 | Parkinson’s disease | Outpatient clinics | |
| Kwan 2013 [60] | 74.9 | – | Community | |
| Ruggiero 2009 [61] | 79.4 | – | Community | |
| van Vliet 2013 [62] | 50.6 | MS | Community | |
| Short Icon FES and Short FES-I | Chan 2018 [63] | 76.8 | – | Community |
| Icon FES and Short Icon FES | Delbaere 2011 [6] | 80.2 | – | Community |
| Delbaere 2013 [64] | 82.1 | Cognitive impairment | Community | |
| Franco 2018 [65] | 71.4 | – | Community | |
| Moreira 2020 [66] | 69.6 | – | Community |
| PROM . | Author . | Age (mean years) . | Disease/condition . | Setting . |
|---|---|---|---|---|
| FES-I | Alghadir 2015 [13] | 32.5 | Vestibular disorders | Outpatient dizziness centre |
| Azad 2014 [14] | 60.1 | Stroke | Outpatient neurological clinics | |
| Baharlouei 2013 [15] | 69.2 | – | Rehabilitation centres and nursing homes | |
| Billis 2011 [16] | 72.9 | – | Community | |
| Boyce 2017 [17] | 52 | Dystonia | Community | |
| Camargos 2010 [18] | 73.4 | – | Community | |
| Choobsaz 2020 [19] | 35.1 | MS | Community | |
| Figueiredo 2017 [20] | 74.3 | – | Community | |
| Figueiredo 2018 [21] | 81.9 | – | Day care service users | |
| Friscia 2014 [22] | 56 | Vertigo, dizziness, unsteadiness | Neurotology clinic | |
| Greenberg 2016 [23] | 77 | Multiple chronic conditions | Community | |
| Halaweh 2016 [24] | 67.3 | – | Community | |
| Halvarsson 2013 [25] | 76.5 | Osteoporosis, balance problems, CaF | Community | |
| Halvarsson 2018 [26] | 76 | Osteoporosis, balance problems, CaF | Community | |
| Hauer 2010 [27] | 81.7 | Cognitive impairment | Geriatric rehabilitation | |
| Hill 2014 [28] | 74.7 | – | Community | |
| Jonasson 2014 [29] | 73 | Parkinson’s disease | Outpatient clinic | |
| Kempen 2007a [30] | 76.8 | – | Community | |
| Kempen 2007b [31] | 76.6 | – | Community | |
| Kisvetrová 2019 [32] | 80 | People with dementia | Geriatric and neurological outpatient clinics | |
| Kovács 2018 [33] | 70.4 | – | Community | |
| Lipardo 2020 [34] | 69.4 | – | Community | |
| Lomas-Vega 2012 [35] | 57.5 | Post-menopausal | Community | |
| Marques-Vieira 2018 [36] | 71.1 | – | Community | |
| Martha Anggarani 2020 [37] | 76.3 | – | Nursing homes | |
| Mehdizadeh 2019 [38] | 60.3 | Parkinson’s disease | Movement disorder clinic | |
| Monjezi 2019 [39] | 36 | MS | Community | |
| Moore 2011 [40] | 74.4 | – | Community | |
| Morgan 2013 [41] | 54 | Balance and vestibular dysfunction | Community | |
| Nordell 2009 [42] | 65.5 | Fall-related fracture | Community | |
| Park 2010 [43] | 72.8 | – | Public health centre | |
| Guo 2015 [44] | 72.4 | – | – | |
| Scremim 2020 [45] | 68.3 | COPD | Pulmonary function service | |
| Smee 2015 [46] | 68.1 | – | Community | |
| Thiamwong 2012 [47] | 70.4 | Community | ||
| Ulus 2012 [48] | 69.7 | Ambulation difficulties | Community | |
| Visschedijk 2015 [49] | 83.1 | Hip fracture | Outpatients in skilled nursing facility | |
| Yardley 2005 [3] | 74.7 | Older people with and without fall risk | Community | |
| Short FES-I | del-Rio-Valeiras 2016 [50] | 77.2 | Age-induced balance disorders | Hospital neurology department |
| Deng 2015 [51] | 59.8 | Cerebral infarction | Inpatient neurology departments | |
| Kamide 2018 [52] | 71.4 | – | Community | |
| Kempen 2008 [1] | 76.6 | – | Community | |
| Kim 2017 [53] | 72.6 | Fallers and non-fallers | Community | |
| Mazumder 2015 [54] | 39.6 | MS | Community | |
| Mehta 2015 [55] | 62.6 | Distal radius fracture | Outpatient rehabilitation clinics | |
| Tan 2018 [56] | 73.1 | – | Community | |
| FES-I and Short FES-I | Araya 2017 [57] | 71 | – | Community |
| Delbaere 2010 [2] | 77.4 | – | Community | |
| Hauer 2011 [58] | 82.3 | Cognitive impairment | Geriatric rehabilitation inpatients | |
| Jonasson 2017 [59] | 73 | Parkinson’s disease | Outpatient clinics | |
| Kwan 2013 [60] | 74.9 | – | Community | |
| Ruggiero 2009 [61] | 79.4 | – | Community | |
| van Vliet 2013 [62] | 50.6 | MS | Community | |
| Short Icon FES and Short FES-I | Chan 2018 [63] | 76.8 | – | Community |
| Icon FES and Short Icon FES | Delbaere 2011 [6] | 80.2 | – | Community |
| Delbaere 2013 [64] | 82.1 | Cognitive impairment | Community | |
| Franco 2018 [65] | 71.4 | – | Community | |
| Moreira 2020 [66] | 69.6 | – | Community |
COPD, chronic obstructive pulmonary disease; CaF, concerns-about-falling; MS, multiple sclerosis.
| Reliability . | |||
|---|---|---|---|
| . | Internal consistency . | Test-retest reliability . | Inter-rater reliability . |
| FES-I | |||
| Overall results | Very good to excellent internal consistency (Cronbach’s alpha range: 0.78–0.99) | Very good to excellent test-retest reliability (ICC range: 0.79–0.99) | Very good to excellent inter-rater reliability (ICC range: 0.72–0.98) |
| Pooled results | Pooled result (weighted mean and SDa of 39 study results) is excellent: Cronbach’s alpha = 0.93 (0.05) | Pooled result (meta-analysis of 16 study results) is excellent: pooled ICC = 0.94 (95% CI 0.91–0.96) | Pooled result (meta-analysis of 5 study results) is excellent: pooled ICC = 0.93 (95% CI 0.88–0.98) |
| Short FES-I | |||
| Overall results | Good to excellent internal consistency (Cronbach’s alpha range: 0.63–0.98) | Very good to excellent test-retest reliability (ICC range: 0.77–0.99) | Excellent inter-rater reliability (one study: ICC = 0.93) |
| Pooled results | Pooled result (weighted mean and SDa of 12 study results) is very good: Cronbach’s alpha = 0.84 (0.10) | Pooled result (meta-analysis of three study results) is excellent: pooled ICC = 0.90 (95% CI 0.87–0.94) | Not assessed: insufficient data for pooling |
| Icon FES | |||
| Overall results | Excellent internal consistency (Cronbach’s alpha range: 0.94–0.97) | Excellent test-retest reliability (ICC range: 0.90–0.96) | Not assessed: no studies |
| Pooled results | Pooled result (weighted mean and SDa of 4 study results) is excellent: Cronbach’s alpha = 0.96 (0.01) | Not assessed: insufficient data for pooling | Not assessed: no studies |
| Short Icon FES | |||
| Overall results | Very good to excellent internal consistency (Cronbach’s alpha range: 0.83–0.91)b | Excellent test-retest reliability (ICC range: 0.92–0.93) | Not assessed: no studies |
| Pooled results | Pooled result (weighted mean and SDa of 5 study results) is very good: Cronbach’s alpha = 0.87 (0.02)b | Not assessed: insufficient data for pooling | Not assessed: no studies |
| Validity and responsiveness | |||
| Structural validity | Hypothesis testing for construct validity | Responsiveness | |
| FES-I | |||
| Overall results | Majority of studies support a one- or two-factor structure | Majority of studies supported our hypotheses in relation to convergent and known-groups validity | Majority of studies supported our hypotheses in relation to responsiveness |
| Pooled results | Not possible to pool | Majority of pooled results supported hypotheses in relation to convergent validity with similar constructs. The majority of pooled results supported our hypotheses in relation to known-groups validity | Not assessed: insufficient data for pooling |
| Short FES-I | |||
| Overall results | Majority of studies support a one-factor structure | Small majority of studies supported our hypotheses in relation to convergent and known-groups validity | Results are inconsistent |
| Pooled results | Not possible to pool | Pooled results did not support convergent validity (note: only possible to pool correlations with one variable). Further research needed. Pooled results supported known-groups validity (note: only possible to pool correlation with one variable). Further research needed | Not assessed: insufficient data for pooling |
| Icon FES | |||
| Overall results | Some evidence to support a two-factor structure. More research needed | No studies investigated convergent validity. Majority of results supported known-groups validity | Not assessed: no studies |
| Pooled results | Not possible to pool | Pooled results supported known-groups validity. | Not assessed: no studies |
| Short Icon FES | |||
| Overall results | Two studies are suggestive of a one-factor structure. More research needed | Majority of studies supported our hypotheses in relation to convergent and known-groups validity | Not assessed: no studies |
| Pooled results | Not possible to pool | Majority of pooled results supported known-groups validity. Not enough data to pool results in relation to convergent validity | Not assessed: no studies |
| Reliability . | |||
|---|---|---|---|
| . | Internal consistency . | Test-retest reliability . | Inter-rater reliability . |
| FES-I | |||
| Overall results | Very good to excellent internal consistency (Cronbach’s alpha range: 0.78–0.99) | Very good to excellent test-retest reliability (ICC range: 0.79–0.99) | Very good to excellent inter-rater reliability (ICC range: 0.72–0.98) |
| Pooled results | Pooled result (weighted mean and SDa of 39 study results) is excellent: Cronbach’s alpha = 0.93 (0.05) | Pooled result (meta-analysis of 16 study results) is excellent: pooled ICC = 0.94 (95% CI 0.91–0.96) | Pooled result (meta-analysis of 5 study results) is excellent: pooled ICC = 0.93 (95% CI 0.88–0.98) |
| Short FES-I | |||
| Overall results | Good to excellent internal consistency (Cronbach’s alpha range: 0.63–0.98) | Very good to excellent test-retest reliability (ICC range: 0.77–0.99) | Excellent inter-rater reliability (one study: ICC = 0.93) |
| Pooled results | Pooled result (weighted mean and SDa of 12 study results) is very good: Cronbach’s alpha = 0.84 (0.10) | Pooled result (meta-analysis of three study results) is excellent: pooled ICC = 0.90 (95% CI 0.87–0.94) | Not assessed: insufficient data for pooling |
| Icon FES | |||
| Overall results | Excellent internal consistency (Cronbach’s alpha range: 0.94–0.97) | Excellent test-retest reliability (ICC range: 0.90–0.96) | Not assessed: no studies |
| Pooled results | Pooled result (weighted mean and SDa of 4 study results) is excellent: Cronbach’s alpha = 0.96 (0.01) | Not assessed: insufficient data for pooling | Not assessed: no studies |
| Short Icon FES | |||
| Overall results | Very good to excellent internal consistency (Cronbach’s alpha range: 0.83–0.91)b | Excellent test-retest reliability (ICC range: 0.92–0.93) | Not assessed: no studies |
| Pooled results | Pooled result (weighted mean and SDa of 5 study results) is very good: Cronbach’s alpha = 0.87 (0.02)b | Not assessed: insufficient data for pooling | Not assessed: no studies |
| Validity and responsiveness | |||
| Structural validity | Hypothesis testing for construct validity | Responsiveness | |
| FES-I | |||
| Overall results | Majority of studies support a one- or two-factor structure | Majority of studies supported our hypotheses in relation to convergent and known-groups validity | Majority of studies supported our hypotheses in relation to responsiveness |
| Pooled results | Not possible to pool | Majority of pooled results supported hypotheses in relation to convergent validity with similar constructs. The majority of pooled results supported our hypotheses in relation to known-groups validity | Not assessed: insufficient data for pooling |
| Short FES-I | |||
| Overall results | Majority of studies support a one-factor structure | Small majority of studies supported our hypotheses in relation to convergent and known-groups validity | Results are inconsistent |
| Pooled results | Not possible to pool | Pooled results did not support convergent validity (note: only possible to pool correlations with one variable). Further research needed. Pooled results supported known-groups validity (note: only possible to pool correlation with one variable). Further research needed | Not assessed: insufficient data for pooling |
| Icon FES | |||
| Overall results | Some evidence to support a two-factor structure. More research needed | No studies investigated convergent validity. Majority of results supported known-groups validity | Not assessed: no studies |
| Pooled results | Not possible to pool | Pooled results supported known-groups validity. | Not assessed: no studies |
| Short Icon FES | |||
| Overall results | Two studies are suggestive of a one-factor structure. More research needed | Majority of studies supported our hypotheses in relation to convergent and known-groups validity | Not assessed: no studies |
| Pooled results | Not possible to pool | Majority of pooled results supported known-groups validity. Not enough data to pool results in relation to convergent validity | Not assessed: no studies |
ICC, intraclass correlation; SD, standard deviation; CI, confidence interval; RoB, COSMIN Risk of Bias assessment.
aMeta-analysis could not be conducted as standard errors were not available to be extracted; thus, we present weighted means and standard deviations.
bAlthough very good internal consistency was reported, these results cannot be used as evidence of internal consistency as the structural validity of the Short Icon FES, which is a prerequisite for the interpretation of Cronbach’s alpha, remains unclear. Further research is needed.
| Reliability . | |||
|---|---|---|---|
| . | Internal consistency . | Test-retest reliability . | Inter-rater reliability . |
| FES-I | |||
| Overall results | Very good to excellent internal consistency (Cronbach’s alpha range: 0.78–0.99) | Very good to excellent test-retest reliability (ICC range: 0.79–0.99) | Very good to excellent inter-rater reliability (ICC range: 0.72–0.98) |
| Pooled results | Pooled result (weighted mean and SDa of 39 study results) is excellent: Cronbach’s alpha = 0.93 (0.05) | Pooled result (meta-analysis of 16 study results) is excellent: pooled ICC = 0.94 (95% CI 0.91–0.96) | Pooled result (meta-analysis of 5 study results) is excellent: pooled ICC = 0.93 (95% CI 0.88–0.98) |
| Short FES-I | |||
| Overall results | Good to excellent internal consistency (Cronbach’s alpha range: 0.63–0.98) | Very good to excellent test-retest reliability (ICC range: 0.77–0.99) | Excellent inter-rater reliability (one study: ICC = 0.93) |
| Pooled results | Pooled result (weighted mean and SDa of 12 study results) is very good: Cronbach’s alpha = 0.84 (0.10) | Pooled result (meta-analysis of three study results) is excellent: pooled ICC = 0.90 (95% CI 0.87–0.94) | Not assessed: insufficient data for pooling |
| Icon FES | |||
| Overall results | Excellent internal consistency (Cronbach’s alpha range: 0.94–0.97) | Excellent test-retest reliability (ICC range: 0.90–0.96) | Not assessed: no studies |
| Pooled results | Pooled result (weighted mean and SDa of 4 study results) is excellent: Cronbach’s alpha = 0.96 (0.01) | Not assessed: insufficient data for pooling | Not assessed: no studies |
| Short Icon FES | |||
| Overall results | Very good to excellent internal consistency (Cronbach’s alpha range: 0.83–0.91)b | Excellent test-retest reliability (ICC range: 0.92–0.93) | Not assessed: no studies |
| Pooled results | Pooled result (weighted mean and SDa of 5 study results) is very good: Cronbach’s alpha = 0.87 (0.02)b | Not assessed: insufficient data for pooling | Not assessed: no studies |
| Validity and responsiveness | |||
| Structural validity | Hypothesis testing for construct validity | Responsiveness | |
| FES-I | |||
| Overall results | Majority of studies support a one- or two-factor structure | Majority of studies supported our hypotheses in relation to convergent and known-groups validity | Majority of studies supported our hypotheses in relation to responsiveness |
| Pooled results | Not possible to pool | Majority of pooled results supported hypotheses in relation to convergent validity with similar constructs. The majority of pooled results supported our hypotheses in relation to known-groups validity | Not assessed: insufficient data for pooling |
| Short FES-I | |||
| Overall results | Majority of studies support a one-factor structure | Small majority of studies supported our hypotheses in relation to convergent and known-groups validity | Results are inconsistent |
| Pooled results | Not possible to pool | Pooled results did not support convergent validity (note: only possible to pool correlations with one variable). Further research needed. Pooled results supported known-groups validity (note: only possible to pool correlation with one variable). Further research needed | Not assessed: insufficient data for pooling |
| Icon FES | |||
| Overall results | Some evidence to support a two-factor structure. More research needed | No studies investigated convergent validity. Majority of results supported known-groups validity | Not assessed: no studies |
| Pooled results | Not possible to pool | Pooled results supported known-groups validity. | Not assessed: no studies |
| Short Icon FES | |||
| Overall results | Two studies are suggestive of a one-factor structure. More research needed | Majority of studies supported our hypotheses in relation to convergent and known-groups validity | Not assessed: no studies |
| Pooled results | Not possible to pool | Majority of pooled results supported known-groups validity. Not enough data to pool results in relation to convergent validity | Not assessed: no studies |
| Reliability . | |||
|---|---|---|---|
| . | Internal consistency . | Test-retest reliability . | Inter-rater reliability . |
| FES-I | |||
| Overall results | Very good to excellent internal consistency (Cronbach’s alpha range: 0.78–0.99) | Very good to excellent test-retest reliability (ICC range: 0.79–0.99) | Very good to excellent inter-rater reliability (ICC range: 0.72–0.98) |
| Pooled results | Pooled result (weighted mean and SDa of 39 study results) is excellent: Cronbach’s alpha = 0.93 (0.05) | Pooled result (meta-analysis of 16 study results) is excellent: pooled ICC = 0.94 (95% CI 0.91–0.96) | Pooled result (meta-analysis of 5 study results) is excellent: pooled ICC = 0.93 (95% CI 0.88–0.98) |
| Short FES-I | |||
| Overall results | Good to excellent internal consistency (Cronbach’s alpha range: 0.63–0.98) | Very good to excellent test-retest reliability (ICC range: 0.77–0.99) | Excellent inter-rater reliability (one study: ICC = 0.93) |
| Pooled results | Pooled result (weighted mean and SDa of 12 study results) is very good: Cronbach’s alpha = 0.84 (0.10) | Pooled result (meta-analysis of three study results) is excellent: pooled ICC = 0.90 (95% CI 0.87–0.94) | Not assessed: insufficient data for pooling |
| Icon FES | |||
| Overall results | Excellent internal consistency (Cronbach’s alpha range: 0.94–0.97) | Excellent test-retest reliability (ICC range: 0.90–0.96) | Not assessed: no studies |
| Pooled results | Pooled result (weighted mean and SDa of 4 study results) is excellent: Cronbach’s alpha = 0.96 (0.01) | Not assessed: insufficient data for pooling | Not assessed: no studies |
| Short Icon FES | |||
| Overall results | Very good to excellent internal consistency (Cronbach’s alpha range: 0.83–0.91)b | Excellent test-retest reliability (ICC range: 0.92–0.93) | Not assessed: no studies |
| Pooled results | Pooled result (weighted mean and SDa of 5 study results) is very good: Cronbach’s alpha = 0.87 (0.02)b | Not assessed: insufficient data for pooling | Not assessed: no studies |
| Validity and responsiveness | |||
| Structural validity | Hypothesis testing for construct validity | Responsiveness | |
| FES-I | |||
| Overall results | Majority of studies support a one- or two-factor structure | Majority of studies supported our hypotheses in relation to convergent and known-groups validity | Majority of studies supported our hypotheses in relation to responsiveness |
| Pooled results | Not possible to pool | Majority of pooled results supported hypotheses in relation to convergent validity with similar constructs. The majority of pooled results supported our hypotheses in relation to known-groups validity | Not assessed: insufficient data for pooling |
| Short FES-I | |||
| Overall results | Majority of studies support a one-factor structure | Small majority of studies supported our hypotheses in relation to convergent and known-groups validity | Results are inconsistent |
| Pooled results | Not possible to pool | Pooled results did not support convergent validity (note: only possible to pool correlations with one variable). Further research needed. Pooled results supported known-groups validity (note: only possible to pool correlation with one variable). Further research needed | Not assessed: insufficient data for pooling |
| Icon FES | |||
| Overall results | Some evidence to support a two-factor structure. More research needed | No studies investigated convergent validity. Majority of results supported known-groups validity | Not assessed: no studies |
| Pooled results | Not possible to pool | Pooled results supported known-groups validity. | Not assessed: no studies |
| Short Icon FES | |||
| Overall results | Two studies are suggestive of a one-factor structure. More research needed | Majority of studies supported our hypotheses in relation to convergent and known-groups validity | Not assessed: no studies |
| Pooled results | Not possible to pool | Majority of pooled results supported known-groups validity. Not enough data to pool results in relation to convergent validity | Not assessed: no studies |
ICC, intraclass correlation; SD, standard deviation; CI, confidence interval; RoB, COSMIN Risk of Bias assessment.
aMeta-analysis could not be conducted as standard errors were not available to be extracted; thus, we present weighted means and standard deviations.
bAlthough very good internal consistency was reported, these results cannot be used as evidence of internal consistency as the structural validity of the Short Icon FES, which is a prerequisite for the interpretation of Cronbach’s alpha, remains unclear. Further research is needed.
Falls Efficacy Scale-International
Overall, there is high certainty evidence (GRADE) supporting the reliability of the FES-I. FES-I demonstrates excellent internal consistency, test-retest reliability and inter-rater reliability. Internal consistency and test-retest reliability were compared across subgroups based on population and remained excellent. Test-retest reliability was compared across subgroups based on methodological quality and remained excellent. With regard to structural validity, there is moderate certainty evidence supporting one-, two- and three-factor structures. The majority of the evidence supports one- and two-factor structures, suggesting a hierarchical concern-about-falling construct composed of two underlying dimensions related to concerns about lower challenge activities inside the home and more challenging and social activities outside the home. With regard to construct validity, there is moderate to high certainty evidence supporting convergent and known-groups validity. Overall, there is high certainty evidence supporting its responsiveness.
Short FES-I
There is high certainty evidence (GRADE) to support the reliability of the Short FES-I, as it demonstrates very good internal consistency and excellent test-retest reliability. Internal consistency was compared in a subgroup analysis based on population and remained excellent. Evidence supporting inter-rater reliability is of very low certainty (one study [60], rated as doubtful methodological quality). Regarding structural validity, there is high certainty evidence supporting a one-factor structure. Evidence for construct validity was mixed. The certainty of the evidence to support convergent validity ranged from very low (Short FES-I correlation with ABC) to high certainty (Short FES-I correlations with self-report measures of functional ability in generally healthy populations only). There is moderate to high certainty evidence supporting known-groups validity of Short FES-I. The evidence for the responsiveness of the Short FES-I was inconsistent.
Icon FES
There is high certainty evidence (GRADE) supporting the reliability of the Icon FES, with excellent internal consistency and test-retest reliability results. Subgroup analyses were not performed due to insufficient data. Regarding structural validity, there was moderate certainty evidence supporting a two-factor structure. With regard to construct validity, there was moderate to high certainty evidence supporting known-groups validity, but there were no studies on convergent validity of Icon FES. There were no studies available on the responsiveness of the Icon FES.
Short Icon FES
There is high certainty evidence (GRADE) supporting excellent test-retest reliability of the Short Icon FES. With regard to validity, there was high certainty evidence for convergent validity in healthy populations. There were no studies in populations with conditions that might affect mobility and balance. There was high certainty evidence for known-groups validity. There were no studies available on the responsiveness of the Short Icon FES.
Regarding structural validity, there was insufficient evidence for the factor structure of the Short Icon FES. As evidence for structural validity is a prerequisite for the interpretation of internal consistency analyses (i.e. Cronbach’s alpha should only be computed when there is evidence for a single common factor or factors) [10, 68], we were unable to interpret results of studies on the internal consistency of the Short Icon FES.
Interpretability and feasibility
Interpretability
Very few studies reported on the distribution of the measures. Of those that reported results of skewness/kurtosis tests, findings were mixed (Supplementary Appendix J). In healthy older populations, distributions ranged from normally distributed [67] to highly skewed across the four measures. In populations with conditions that might affect mobility and balance reported distributions ranged from low to high levels of skewness. Information on missing data was only available in relation to the FES-I and Short FES-I and was not widely reported. Missing data occurred more often when the measures were administered via self-report rather than interview, and was observed in patients with cognitive impairment [27] and Parkinson’s disease [29, 59].
Floor and ceiling effects were considered present if 15% of participants achieved the lowest or highest score [69]. Both floor and ceiling effects were negligible for FES-I in generally healthy older populations; however, one study reported floor effects in patients with Parkinson’s disease [38]. In general, floor and ceiling effects were also negligible for the Short FES-I; however, one study reported a slight floor effect in a population of generally healthy older people [63], and another study reported a small floor effect in a population with Parkinson’s disease [59]. Again, floor and ceiling effects were negligible for the Icon FES and Short Icon FES, with only one study reporting a small floor effect for the Short Icon FES in a population of cognitively impaired older people [64].
Feasibility
There was relatively little reporting of feasibility in included papers and none related to clinician perspective. Those papers reporting patient comprehensibility all indicate FES-I variants were appropriate for and comprehended by patients (Supplementary Appendix K). Completion time was not widely reported, but from papers reporting on this, FES-I and Icon FES take about 4–5 minutes (maximum 10 minutes), whilst Short FES-I and Short Icon FES take about 2 minutes. Administration time did not appear to vary widely with administration method nor population.
Discussion
There is evidence for excellent measurement properties of all four FES-I instruments, although certainty of evidence varies depending on properties being investigated. There is high certainty evidence to support internal consistency of FES-I, Short FES-I and Icon FES, both in healthy older populations and people with conditions that might affect mobility and balance. Although a number of studies using Short Icon FES report excellent Cronbach’s alpha values, further research on the structural validity of the measure is required to verify its internal consistency, as evidence for structural validity is a prerequisite for the interpretation of internal consistency analyses (i.e. Cronbach’s alpha should only be computed when there is evidence for a single common factor or factors) [10, 68]. There is high certainty evidence supporting excellent test-retest reliability for all four FES-I instruments. There is high certainty evidence for excellent inter-rater reliability of FES-I, but for the other FES-I versions, evidence is of poor quality or absent.
There is consistent high certainty evidence supporting a one-factor structure for Short FES-I as a single ‘concerns-about-falling’ construct. For FES-I, the picture is more complex, with half of studies (14/28) reporting a one-factor structure, although there is also evidence for a two-factor structure. Several articles report both one- and two-factor structures [3, 18, 36, 47, 60, 62], suggesting that FES-I assesses a hierarchical ‘concerns-about-falling’ factor with two underlying dimensions related to concerns about lower challenge activities inside the home and more challenging and social activities outside the home. Such an interpretation aligns well with the original rationale for developing FES-I [3]. There is moderate certainty evidence from one study supporting a two-factor structure of Icon FES, but results for Short Icon FES are inconsistent and further research is required.
Results on construct validity were often poorly reported (e.g. effect sizes not provided in relation to known-groups validity, in which case we were unable to test our hypotheses). Most of the evidence supports the construct validity of FES-I and meta-analysis shows that FES-I has good convergent validity with similar measures of concerns-about-falling. FES-I correlates as expected (according to our hypotheses) with measures of functional ability and well-being in both healthy older populations and people with conditions that increase falls risk. Because of lack of studies, there was very low certainty evidence for convergent validity of Short FES-I when comparing with similar constructs. However, there was high certainty evidence to support its convergent validity in relation to measures of functional ability and well-being in generally healthy older people. Due to low certainty evidence, we are not confident about the convergent validity of Short FES-I in populations with conditions that might affect mobility and balance and further research is needed. There is also high certainty evidence for convergent validity of Short Icon FES in relation to measures of functional ability and well-being in generally healthy older people (no studies in populations with conditions that might affect mobility and balance). There were no studies investigating the convergent validity of Icon FES. There was moderate to high certainty evidence to support the known-groups validity of all four measures. There is high certainty evidence supporting responsiveness of FES-I, but findings were inconsistent for Short FES-I. Further investigation of responsiveness is needed for all four FES-I instruments.
Overall, there is strong evidence to recommend FES-I for use with older people who are either generally healthy or have a condition that puts them at an increased risk of balance or mobility issues, as well as the general population that may have a condition that increases their risk of balance or mobility problems. FES-I is interpretable and feasible for both healthy adults and patients. Although there were fewer studies on Short FES-I, it is clearly a promising alternative with overall excellent measurement properties to assess concerns-about-falling in a couple of minutes in both healthy older people and people with conditions that might affect mobility and balance. More research is recommended in relation to the two Icon FES variants, but again initial results look promising.
Further research
Although the measurement properties of FES-I appear reasonably well established, further studies are needed in relation to the measurement properties of FES-I variants. In particular, additional research is needed on inter-rater reliability of Short FES-I, Icon FES and Short Icon FES, structural validity of Short Icon FES, convergent validity of Short FES-I and Icon FES (particularly in populations with conditions that might affect mobility and balance), and responsiveness of all four measures. Although there is evidence supporting responsiveness of FES-I, there was no evidence to support its responsiveness in relation to an intervention conducted as part of a randomised controlled trial (RCT). This was a limitation of the review as, following COSMIN guidelines, we only selected studies for inclusion if their explicit aim was to investigate one or more measurement properties of FES-I instruments. This led to the exclusion of RCTs that used FES-I instruments as outcome measures, rather than specifically to assess measurement properties. This could be the focus of a future review as these studies could potentially provide rich data on the responsiveness of FES-I instruments in relation to interventions targeting falls risk.
Further research is also required in relation to setting. Most studies were conducted in community or outpatient settings and very few studies (n = 6) were conducted in inpatient settings. Future research should aim to recruit from inpatient settings so that the measurement properties of FES-I instruments can be adequately compared with those from outpatient and community-based studies.
Finally, we were unable to evaluate measurement error due to lack of information on MIC of FES-I instruments, as we found no studies to establish the MIC of any of the FES-I instruments. This information would be useful as it informs both the interpretability of the measures as well as providing a standard against which measurement error can be evaluated.
Strengths and limitations
This study followed COSMIN methodology and a rigorous approach was taken to the evaluation of the quality and certainty of the evidence. Methodological quality was evaluated using the COSMIN RoB Checklist, and the quality of each individual result was evaluated by applying COSMIN’s criteria for good measurement properties; evidence was summarised and its certainty graded using modified GRADE. The study was limited in that we did not investigate measurement properties based on individual diseases or conditions as there were not enough data for meta-analysis. We did, however, conduct subgroup analysis by comparing measurement properties in generally healthy older people versus people with conditions that might affect mobility and balance, where possible. We were also unable to secure high-quality translations for two studies in Farsi (Persian) and thus had to exclude them.
Conclusion
In summary, we recommend the use of all four FES-I instruments with both generally healthy older people and people with conditions that might affect mobility and balance. The FES-I has the largest volume of evidence supporting its measurement properties, followed by Short FES-I, which is a robust alternative to FES-I for those seeking to reduce administration time. Further research is needed on specific properties outlined above, particularly responsiveness and measurement error, as well as measurement properties across different settings. This review helped inform the World Guidelines for Falls Prevention in Older Adults [70], where FES-I and Short FES-I have been recommended for assessment of concerns-about-falling.
Declaration of Sources of Funding
This work is supported by Professor Chris Todd’s NIHR Senior Investigator Award (Reference NIHR200299). Dr Lisa McGarrigle, Ms Yang Yang and Dr Reena Lasrado were employed on this award at The University of Manchester under sub-contract from Manchester University NHS Foundation Trust. The views expressed are those of the author(s) and not necessarily those of the NIHR or the Department of Health and Social Care. The University of Manchester acted as sponsor for this study.
Declaration of Conflicts of Interest
C.T. was the principal investigator on the EC grant used in the development of the FES-I and Short FES-I. He was the senior author on the original FES-I development papers and on a number of papers subsequently using FES-I/Short FES-I. The University of Manchester hosts the FES-I website (www.fes-i.org) administered under C.T.’s control. FES-I/Short FES-I are published and distributed free of charge. Commercial trial use of FES-I is permitted and companies encouraged to make a donation to The University of Manchester Development and Alumni Funding Scheme.
Footnotes
We refer to gender instead of sex throughout this review as we are dependent on reports from other studies where sex/gender categorisations were defined based on self-report; thus, we recognise the socially constructed nature of gender herein.
References
Moreira ACS de S,




Comments