-
PDF
- Split View
-
Views
-
Cite
Cite
Oliver L Hatheway, Arnold Mitnitski, Kenneth Rockwood, Frailty affects the initial treatment response and time to recovery of mobility in acutely ill older adults admitted to hospital, Age and Ageing, Volume 46, Issue 6, November 2017, Pages 920–925, https://doi.org/10.1093/ageing/afw257
Close - Share Icon Share
Abstract
to investigate how frailty and mobility impairment affect recovery of balance and mobility in acutely ill older patients.
secondary analysis of cohort study.
general and geriatric medicine inpatient units, QEII Health Sciences Centre, Dalhousie University, Canada.
four hundred and nine older adults (mean age = 81 ± 7 standard deviation, 64% women).
we constructed a frailty index based on a comprehensive geriatric assessment (FI-CGA), at baseline (2 weeks before admission; mean 0.31 ± 0.10), and on admission (mean 0.40 ± 0.10), and recorded Hierarchical Assessment of Balance and Mobility (HABAM) scores daily. Recovery was measured as the difference in HABAM scores between discharge and admission.
the odds of no or incomplete recovery increased by 1.06 (95% confidence interval: 1.01–1.11) for each 0.1 increment in the baseline FI-CGA. Recovery odds were similarly dependent on age, but independent of baseline HABAM scores. Recovery time was related to Day 1 HABAM scores, initial treatment response and change in the FI-CGA from baseline to admission (r = 0.35, P < 0.001). Recovery time was independent of age. Patients whose mobility improved within 48 h (n = 113; 28%) showed greater improvement and quicker recovery.
frailer patients are at a greater risk of incomplete or lengthier recovery from impaired mobility and balance. Tracking mobility and balance might help providers, patients and families understand the course of acute illness in older adults.
Introduction
Managing acute illness in older adults offers special challenges. Many, especially those who are frail, experience delirium, falls and functional decline [1]. Even though frail older adults are common users of health services, such disease presentations still challenge current models of care that often are based on single system problems in people well enough to go home after a few days of treatment [2–4]. Two practical challenges of such nonspecific disease presentations are that, in their attenuation of traditional signs of illness, they make recovery both more prolonged (and often incomplete [5]), and more difficult to discern.
Recognising this challenge, several instruments have become available to track changes in function and mobility in older adults [6]. This is sensible, given that function and mobility integrate a wide range of information about health and about a range of illnesses that affect respiration, metabolism and motor function, as well as subclinical age-related deficits. In addition, impaired recovery is an important part of frailty [7].
Frailty can be represented through a deficit accumulation model [8]. Deficits accumulate when damage can neither be removed nor repaired. Recovery after damage takes time, during which the organism is susceptible to further deficit accumulation, one basis of its reduced resilience. In consequence, recovery time can be directly related to the degree of frailty [7].
The study of mobility offers an excellent target for understanding the relationship between frailty and recovery time. Mobility performance is quantifiable and its impairment is definitional in phenotypic frailty [9]. Furthermore, the risk of mobility impairments increases as deficits accumulate [10] and is associated with chronic disability and death [11]. In general, impaired mobility in people who are frail can be interpreted as a sign of general system failure. This is the rationale for approaching mobility impairment (falls, taking to bed, etc.) as one of the so-called ‘geriatric giants’ [12]. That too is why tracking mobility and balance systematically can aid prognosis. A previous study showed that greater frailty was associated with worse baseline mobility and balance, defined by the history of such performance 2 weeks prior to admission. For prognosis, however, dynamical changes were most important. In older adult inpatients with a positive initial treatment response (those whose mobility and balance was the same as on admission or had improved within 48 h) the risk of death at 30 days was 4%, compared to 74% inpatients with declining mobility and balance. Declining mobility in the 1st 48 h represented a relative risk of death of 17.1 (95% confidence interval: 4.9–60.3) [13].
Despite the importance of the initial treatment response in the overall recovery course, there is little quantitative evaluation of the dynamics of acute illness recovery in frail older adults. For this reason, we examined whether the recovery of mobility and balance could be related to the degree of underlying frailty, and to the initial treatment response by reanalysing data from the Hubbard et al. [13]. Our objectives were to (i) relate the odds of recovery and recovery time to both (a) the degree of frailty and (b) initial treatment response, and (ii) to relate the odds of recovery and recovery time to the degree of damage that had been sustained acutely.
Methods
This was a secondary analysis of a cohort study reported in 2011 [13] of 409 elderly patients (mean age = 81.8 ± 7.9 standard deviation, 64% women) admitted to a general or geriatric medicine ward in a tertiary care teaching hospital.
Measures
Balance and mobility
The Hierarchical Assessment of Balance and Mobility (HABAM) was developed as a daily measure of balance and mobility in elderly patients in an acute-care setting [14]. It assesses three domains: balance, mobility and transfers, and has been shown to be valid, reliable and responsive to change [15]. Scores were recorded on a daily basis by attending physicians, house staff and on the rehabilitation services, ward physiotherapists. Here, the HABAM scoring scale was transformed such that the possible score from each of the three assessed domains ranged from zero to one, making the range of possible HABAM scores scale from zero to three. Then, as in dynamical physical system analysis, the scores were rescaled such that a lower HABAM score corresponded to better mobility (see Supplementary data, available at Age and Ageing online for further details).
Frailty index
On admission, patients were assessed using a standardised Comprehensive Geriatric Assessment (CGA), which considers a wide range of aspects of health including cognitive and emotional status, motivation, mobility, communication, medical problems, number of medications etc. The CGA can be used to quantify frailty as a frailty index (FI) whereby information is taken from the CGA and coded either as binary (e.g. delirium present = 1, absent = 0), or graded variables (e.g. 1 point = dependent for bathing, 0.5 = needs assistance and 0 = independent) [16]. Any FI based on a comprehensive geriatric assessment (FI-CGA) is calculated by adding up the total number of points a patient has then dividing by the number of possible deficits considered. Thus the FI-CGA in theory ranges from zero to one, with higher scores corresponding to higher degrees of frailty [17]. The CGA form contains sections to evaluate both a patient's current state as well as their baseline 2 weeks prior, allowing for an FI-CGA to be calculated at two time points (FI-CGACURR and FI-CGABASE, respectively). Typically, even in acutely ill patients, <1% of FI-CGA scores exceed 0.7 [6, 18]. Change in the FI-CGA score from baseline was taken as marking the degree of acute impairment.
Mobility impairment
The HABAM score on admission quantified the degree of impairment in balance and mobility. Mildly impaired mobility was signified by a HABAM score (range 0–3) ≤1.25, whereas severe impairment was present with HABAM scores ≥1.75. Moderately impaired HABAM scores fell between 1.25 and 1.75. These values correspond to significant clinical grades of mobility and balance: a person with mild mobility impairment (HABAM score ≤1.25) can move independently, whereas severe impairment levels (score ≥1.75) correspond to the thresholds of and not being able to transfer from bed without assistance.
Recovery
Recovery was operationalized in two ways. First, it was dichotomised, so that an individual patient was defined as having recovered if all of the following were met:
Balance and mobility improved while in hospital (quantified as an improved HABAM score), or for those in the top centile, remained unchanged, and;
The patient did not require a higher level of care upon discharge and
They did not die within 30 days of admission.
In those patients who met the recovery criteria, recovery time was measured in days since admission. Here, to avoid trivial changes, in the subset of patients who met the recovery criteria, recovery was defined as having occurred on the 1st day a patient's combined HABAM score reached 85% of their discharge HABAM score.
Analysis
The relationship between the degree of mobility impairment on admission and age, sex and the degree of frailty (baseline and current) was determined. In each case, ANOVA was used in relation to continuous variables, and χ2 for ordinal variables. To relate the occurrence of recovery to the degree of frailty (Objective 1), a logistic regression model was used. Similarly, to relate recovery time to the degree of damage that had been sustained (Objective 2), recovery time was analysed using a linear regression model. Recovery time was regressed on change in the FI from baseline, HABAM score on Day 1, treatment response and age. Recovery was further analysed by stratifying patients into three groups: those whose HABAM scores improved in the 1st 48 h, those whose scores remained the same and those whose scores worsened. The proportion of people who recovered in each cohort was then determined daily and plotted.
Ethics
The original project was approved by the Research Ethics Committee of the Capital District Health Authority. All information was collected as part of routine care. Consent was sought for initial enrolment was sought for access to these routinely collected data. Secondary analysis was approved by the Centre for Clinical Research at Capital Health, REB file #: CDHA-RS/2015-033.
Results
On admission most patients had moderately or severely impaired HABAM scores (Table 1). People who were frailer at baseline were less likely to recover their balance and mobility. For each 0.1 increment in the FI-CGABASE, the odds of no or incomplete recovery increased by 1.06 (95% confidence interval: 1.01–1.11). Recovery odds were similarly dependent on age (OR = 1.010, 95% CI: 1.008–1.012), but independent of HABAM scores on Day 1 (P = 0.22).
Characteristics of the cohort in relation to mobility impairment severity on admission
| HABAM balance and mobility scores: . | ≤1.25 (mild impairment) N = 76 (19%) . | 1.25–1.75 (moderate impairment) N = 154 (38%) . | >1.75 (severe impairment) N = 179 (42%) . | P-value . |
|---|---|---|---|---|
| Age (SDa) | 79.2 (6.5) | 81.4 (7.7) | 83.1 (8.2) | <0.001 |
| Sex (% women) | 51.3 | 57.8 | 67.6 | 0.03 |
| Mean FI-CGA Baseb (SD) | 0.28 (0.10) | 0.30 (0.10) | 0.32 (0.11) | 0.007 |
| Mean FI-CGACurrb (SD) | 0.36 (0.10) | 0.39 (0.097) | 0.42 (0.092) | <0.001 |
| Proportion recovered in each group (%) | 73.6 | 66.9 | 66.5 | 0.49 |
| Mean recovery time (SD) | 3.7 (3.5) | 8.3 (6.4) | 1.8 (9.3) | <0.001 |
| HABAM balance and mobility scores: . | ≤1.25 (mild impairment) N = 76 (19%) . | 1.25–1.75 (moderate impairment) N = 154 (38%) . | >1.75 (severe impairment) N = 179 (42%) . | P-value . |
|---|---|---|---|---|
| Age (SDa) | 79.2 (6.5) | 81.4 (7.7) | 83.1 (8.2) | <0.001 |
| Sex (% women) | 51.3 | 57.8 | 67.6 | 0.03 |
| Mean FI-CGA Baseb (SD) | 0.28 (0.10) | 0.30 (0.10) | 0.32 (0.11) | 0.007 |
| Mean FI-CGACurrb (SD) | 0.36 (0.10) | 0.39 (0.097) | 0.42 (0.092) | <0.001 |
| Proportion recovered in each group (%) | 73.6 | 66.9 | 66.5 | 0.49 |
| Mean recovery time (SD) | 3.7 (3.5) | 8.3 (6.4) | 1.8 (9.3) | <0.001 |
aSD, standard deviation.
bFI-CGABase/Curr = FI at two-week baseline and current levels respectively.
Characteristics of the cohort in relation to mobility impairment severity on admission
| HABAM balance and mobility scores: . | ≤1.25 (mild impairment) N = 76 (19%) . | 1.25–1.75 (moderate impairment) N = 154 (38%) . | >1.75 (severe impairment) N = 179 (42%) . | P-value . |
|---|---|---|---|---|
| Age (SDa) | 79.2 (6.5) | 81.4 (7.7) | 83.1 (8.2) | <0.001 |
| Sex (% women) | 51.3 | 57.8 | 67.6 | 0.03 |
| Mean FI-CGA Baseb (SD) | 0.28 (0.10) | 0.30 (0.10) | 0.32 (0.11) | 0.007 |
| Mean FI-CGACurrb (SD) | 0.36 (0.10) | 0.39 (0.097) | 0.42 (0.092) | <0.001 |
| Proportion recovered in each group (%) | 73.6 | 66.9 | 66.5 | 0.49 |
| Mean recovery time (SD) | 3.7 (3.5) | 8.3 (6.4) | 1.8 (9.3) | <0.001 |
| HABAM balance and mobility scores: . | ≤1.25 (mild impairment) N = 76 (19%) . | 1.25–1.75 (moderate impairment) N = 154 (38%) . | >1.75 (severe impairment) N = 179 (42%) . | P-value . |
|---|---|---|---|---|
| Age (SDa) | 79.2 (6.5) | 81.4 (7.7) | 83.1 (8.2) | <0.001 |
| Sex (% women) | 51.3 | 57.8 | 67.6 | 0.03 |
| Mean FI-CGA Baseb (SD) | 0.28 (0.10) | 0.30 (0.10) | 0.32 (0.11) | 0.007 |
| Mean FI-CGACurrb (SD) | 0.36 (0.10) | 0.39 (0.097) | 0.42 (0.092) | <0.001 |
| Proportion recovered in each group (%) | 73.6 | 66.9 | 66.5 | 0.49 |
| Mean recovery time (SD) | 3.7 (3.5) | 8.3 (6.4) | 1.8 (9.3) | <0.001 |
aSD, standard deviation.
bFI-CGABase/Curr = FI at two-week baseline and current levels respectively.
Recovery time was related to the initial treatment response (Figure 1). Improvement in HABAM scores over the 1st 48 h (seen in 113 patients; 28%) was associated with greater improvement overall, and with shorter recovery times, compared to those who remained the same (268; 66%) or who worsened (19; 6%).
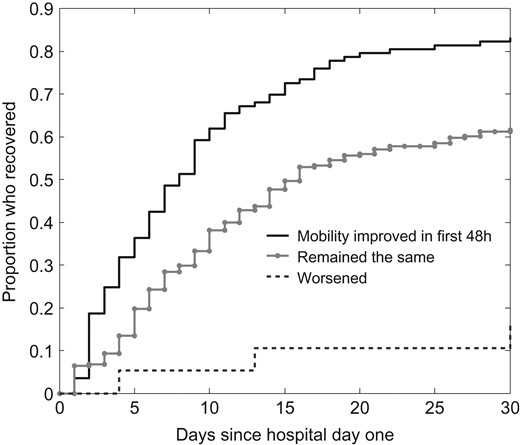
Time and extent of recovery in mobility and balance, relation to the initial (48 h) treatment response.
In those patients who recovered, recovery time (Objective 2) was found by multiple linear regression to be related to mobility impairment on admission, treatment response over the 1st 48 h of hospitalisation and change in frailty from baseline (r = 0.35, P < 0.001). Such a relationship took the form of an increasing exponential curve, with an increase in each coefficient corresponding to an exponential increase in recovery time. Recovery time was independent of age (P = 0.82). Of those who recovered, patients with mild mobility impairment recovered sooner (Figure 2a). By the 5th hospital day, about half of those with mild impairment, and one quarter of those with moderate impairment had recovered, compared with 1 in 10 of those with severe impairment (Figure 2b).
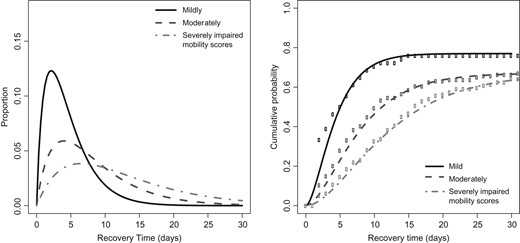
Proportion (a) and cumulative probability (b) distributions of recovery time for differing categories of mobility impairment on admission. Proportion corresponds to the fraction of people in each mobility impairment category who recovered on a given hospital day. These data are represented here by best-fit gamma distributions. The cumulative probability distribution includes all patients. Given that not all patients recovered, the curves asymptotically approach the proportion of people recovered in each category, not 1.0. Figure 2b contains both the best-fit curve and the raw data.
Discussion
In hospitalised, frail older adults, recovery of mobility was related to the degree of baseline frailty and to age. Patients who recovered tended to be less frail at baseline and to be younger. This relationship between the degree of baseline frailty and recovery was independent of the extent of mobility impairment at admission. In short, the less frail a person was at baseline, the more likely they were to recover from acute illness regardless of its current impact on balance and mobility. Recovery time was exponentially related to the change in frailty from baseline, Day 1 HABAM scores and initial treatment response. Declining balance and mobility over the 1st 2 days in hospital was predicted exponentially longer recovery time. Recovery time was independent of age.
Our results must be interpreted with caution. Patients were recruited from a single site. Given the variability between patients and outcomes, the sample size is modest. Furthermore, a patient's 2-week baseline frailty measure was done by self- or family reporting and not by observer assessment. Inasmuch as estimating baseline function is done regularly by geriatricians and many other clinicians, and otherwise largely is unavailable, this was unavoidable.
Requiring that each patient's balance and mobility scores improve might overlook patients admitted with little impairment. Roughly 20 patients were admitted with very little to no balance or mobility impairment and thus had little room to recover by HABAM measurements. Given that these patients represent only 5% of the sample size, this had little impact on the final results. Furthermore, our result of recovery being dependent on baseline level of frailty and not mobility impairment has been independently verified where frailty showed a stronger association with death [19] and functional decline [20]. This is in keeping with the thought that frailty is a marker of decreased capacity for recovery [7, 21, 22].
As noted, mobility is an integrative measure, incorporating both physiologic and social faculties, with a demonstrably important bearing on quality of life in older adults [23]. Its clinical interpretation is straightforward: when people are well, they move about; if they are ill they move less and when they are about to die they hardly move at all. The relationships between incipient frailty and life-space mobility [24], and between executive function and mobility, also underscores it status as a higher order function [25]. Therefore, decreased mobility is a marker of widespread system damage. Viewed in this light, even movement in bed, transferring in and out of bed are important parts of the mobility continuum.
Frailty arises from multisystem impairment that decreases the ability to respond to stress. This has often been referred to as impaired physiologic reserve, a concept that has been studied on the cellular [26] and genetic levels [27, 28]. Even so, if impaired physiological reserve is such a direct consequence of frailty, is there any value added in considering these concepts as separable? We have proposed that queuing theory offers a way forward by distinguishing damage and repair [7]. Just as the length of a queue is a function of the number of people who arrive and the time it takes for them to be processed, so too does the value of the FI depend on the rate of damage the person sustains, and the time it takes to recovery from that damage. If additional damage arises before recovery from pervious insults has occurred, then deficits accumulate and FI scores increase. Though we do not have FI-CGA data at the time of discharge to test this hypothesis directly, our data do suggest both that recovery time and the degree of baseline frailty are related to each other, and that increases in frailty represented through a decrease in mobility (i.e. damage) also relate to prolonged recovery time. In this way, deficits accumulate (the degree of frailty increases) when damage arrives at a rate that does not allow for recovery to have occurred. In this way, these results support the queuing theory model wherein deficits accumulate when the damage rate exceeds the recovery time and the recovery time becomes prolonged as deficits accumulate. They also demonstrate a common property of complex systems: the rich get richer, or as here, recovery is most likely, and takes least time, in those least impaired at baseline [7].
The results from our work have clinical value. Many frail, elderly patients lack ‘traditional’ signs and symptoms of disease, making measures that perform well and have predictive value for all patients worth considering [19]. We have shown that assessing mobility clinically can, early in the hospital course, aid in predicting which frail patients admitted to hospital are most likely to recovery, and those who are most likely to die.
Recovery from an acute illness in older adults was best predicted by a patient's baseline level of function, and the extent of overall change in function: what matters is both repair capability (baseline frailty) the extent of a given insult (acute change in the degree of frailty). Given that recovery odds and recovery time differ in how they depend on the degree of mobility impairment and the degree of frailty, here measured using an FI-CGA underscores the need to close the gap between what we know about GCA and how we employ that knowledge [29]. How best to translate the specific clinical actions needed, and then evaluating their impact, is motivating further inquiries by our group.
Acute illness commonly manifests in frail older adults with nonspecific signs and symptoms such as impairment in balance, mobility and transfers.
Standardised assessments of mobility can be used to track the degree of recovery from acute illness in frail older adults.
Greater mobility impairment relative to baseline, and greater absolute impairment at presentation, each herald a worse prognosis in older adults admitted to hospital.
Prognosis also depends on the initial treatment response: a good prognosis is marked by early improvement in recovery of mobility and balance.
Supplementary data
Supplementary data mentioned in the text are available to subscribers in Age and Ageing online.
Acknowledgements
These analyses were supported by the Research Medicine Program of the Dalhousie University Faculty of Medicine (Studentship to O.L.H.) and by the Foundation Family Innovation Fund of the Nova Scotia Health Authority Foundation, which also supported the initial study. K.R. receives career support from the Dalhousie Medical Research Foundation as the Kathryn Allen Weldon Professor of Alzheimer Research.




Comments