-
PDF
- Split View
-
Views
-
Cite
Cite
Michael W Otto, Rebecca E Lubin, David Rosenfield, Daniel J Taylor, Jeffrey L Birk, Colin A Espie, Ari Shechter, Donald Edmondson, Justin M Shepherd, Michael J Zvolensky, The association between race- and ethnicity-related stressors and sleep: the role of rumination and anxiety sensitivity, Sleep, Volume 45, Issue 10, October 2022, zsac117, https://doi.org/10.1093/sleep/zsac117
Close - Share Icon Share
Abstract
This study was designed to investigate the association between psychosocial factors and self-reported sleep duration and two indices of sleep quality in a racially and ethnically diverse sample of adults. We investigated the relations between both rumination and anxiety sensitivity with these self-reported sleep outcomes. We also examined rumination and anxiety sensitivity as moderators of three race- and ethnicity-related stressors: discrimination, acculturative stress, and socioeconomic status.
In a cross-sectional design, we assessed 1326 adults (ages 18–48 years) selected for self-reported racial and ethnic minority status. Regression analyses were used to examine the associations between demographic, social/environmental stressors, depression severity, rumination, and anxiety sensitivity and three sleep outcomes: sleep duration, sleep quality subscale, and global sleep quality.
Our findings supported the hypothesized role of rumination as an amplification factor for the influence of race- and ethnicity-related stressors on sleep duration and quality. Rumination was associated with all three sleep outcomes (sleep duration, sleep quality subscale, and global sleep quality) and was a moderator of the associations between discrimination and all 3 sleep outcomes. Anxiety sensitivity was not consistently associated with these sleep outcomes. Depression symptoms did not account for these findings.
If confirmed in longitudinal study, our findings introduce a potentially important treatment target—rumination—for addressing sleep disparities in prevention or intervention models. Rumination appears to amplify the negative sleep consequences of race- and ethnicity-related stressors and is a modifiable treatment target.
Strategies are urgently needed to address racial and ethnic sleep disparities. We investigated whether two hypothesized amplification factors—rumination and anxiety sensitivity—were linked to sleep disruption in racially and ethnically diverse adults. We specifically examined whether rumination and anxiety sensitivity moderated the influence of racism-related stressors on sleep. Our hypotheses were supported for rumination: (1) rumination was directly associated with shorter sleep length and poor sleep quality, and (2) rumination amplified the negative association between discrimination and sleep outcomes. Our findings are limited by the study’s cross-sectional nature, but if confirmed in longitudinal study, would encourage attention to rumination in prevention and intervention models as a possible strategy for addressing sleep disparities.
Introduction
Poor sleep (e.g., shorter duration or quality) is a key contributor to negative health outcomes, including physical health conditions (such as cardiovascular diseases, diabetes, and respiratory disorders) and mental health conditions (such as depression and dementia) [1–4]. Adults who demonstrate shorter sleep duration or quality are also more likely to manifest the negative health characteristics—obesity, sedentary lifestyle, and smoking—that play a disproportionate role in morbidity and mortality over time [5].
Short sleep duration (i.e., less than 7 hours of sleep per night) is widely prevalent (i.e., 35.2%) in the United States [5]. Less is known about the prevalence of poor sleep quality, owing mostly to inconsistent definitions and lack of large-scale studies. There appear to be racial and ethnic disparities in both duration and quality, with greater rates of short sleep and poorer sleep quality documented in Black/African American, Native-American, Asian, and Hispanic populations [6–13]. The magnitude of these racial disparities can be striking; for example, the CARDIA study found almost 1 hour less sleep on average for Black relative to White adults [14].
Studies evaluating health disparities have examined the role of racism and other race- and ethnicity-related stressors [15–17]. There is strong evidence for negative associations between racial/interpersonal discrimination events and both sleep duration and quality [18–26], and racial discrimination has been found to be a more important predictor of shorter sleep duration than other concurrent stressors or nonracial discrimination [11]. Indeed, in some studies discrimination events fully accounted for racial differences in sleep [11], although the majority of research suggests that sleep disparities may be only partially explained by discrimination (for a review, see Slopen et al. [22]). Other race- and ethnicity-related stressors also predict poorer sleep duration or quality: greater acculturation-related stress [25, 27] and lower SES [28, 29], due to the complex relationship between SES and race and ethnicity, and the influence of SES on cumulative vulnerabilities to negative health behaviors and outcomes [30].
Racism has been relatively immutable to societal change efforts over time (e.g., Bonilla-Silva and Forman [31], and Joseph and colleagues [32]). The reasons for this ongoing failure are complex, but they may stem, in part, from the fact that few interventions have effectively targeted the structural basis of race- and ethnicity-related stressors in combination with attention to specific forms of these stressors (e.g., see the work of Gee and Ford [33]). As stated by Gee and Ford [33, p.116)], individual acts of discrimination, though often ubiquitous, harmful, and palpably felt, are merely the “tip of the iceberg” such that “[p]olicies and interventions that change the iceberg’s tip may do little to change its base, resulting in structural inequalities that remain intact….”. Accordingly, so that preventive interventions need not await much-needed successful societal change required to dismantle long-standing historical structures that create, maintain, and exacerbate race- and ethnicity-related stressors, it is important to consider additional means of improving health disparities. One approach is to understand which modifiable, person-level variables may be harnessed to influence the link between the continuing harm of race- and ethnicity-related stressors and worse sleep duration and quality.
The purpose of this paper is to examine the direct and moderating influence of two modifiable psychological factors that have preliminary support for their role in poor sleep: brooding rumination and anxiety sensitivity (AS). Both variables have been conceptualized as having amplifying roles on distress and negative health-behavioral responses to stress [34, 35]. Furthermore, each of these variables has been implicated in racial and ethnic disparities in sleep or in the pathway between race- and ethnicity-related stressors and sleep duration or quality, as detailed below.
Rumination has been defined as a pattern of response to distress in which an individual perseverates on negative aspects of their life or symptoms and the negative causes and consequences thereof, while failing to initiate active problem solving [36, 37]. Rumination appears to act as an amplification factor, enhancing negative affective responses to stressors [34], including discrimination [38]. Rumination has been found to be directly associated with lower sleep quality in individuals with insomnia [39]. This effect is similarly present for sleep disturbances found in individuals with depressive symptoms, even after controlling for baseline depression [40]. Further, this effect has been demonstrated prospectively, with a study of undergraduates finding that baseline rumination predicted reduction in sleep quality after three weeks [41]. In addition to these direct effects, rumination has been found to moderate (amplify) the influence of racial discrimination on sleep quality such that discrimination experiences decrease sleep quality more in individuals with high rumination than in individuals with low rumination [42].
There is similar evidence for the role of anxiety sensitivity (AS) in amplifying the negative effects of stress. AS refers to a fear of anxiety-related sensations due to the belief that they have catastrophic consequences [43]. The role of AS in relation to negative health behaviors can be characterized as enhancing the aversiveness of negative affective or somatic experiences and increasing the perceived need to escape or avoid these experiences, including the avoidance of healthy behaviors or over-engagement in unhealthy escape-oriented behaviors such as substance use [35]. AS significantly predicts sleep duration and/or sleep quality across both nonclinical and clinical samples, including patients with panic disorder and breast cancer [44–46]. Additional research suggests that AS can amplify the negative effects of pre-sleep anticipatory anxiety on latency of sleep onset [47]. Findings from clinical trials also lend support for a causal role of AS on sleep, where interventions specifically targeting AS improve sleep duration and quality through reductions in AS [48, 49]. Importantly, in a nationally representative sample of 1,289 adults with a history of cardiovascular disease, AS statistically accounted for racial differences in sleep duration, mediating almost 30% of the observed race effect on sleep duration [50].
Part of the value of examining the role of rumination and AS in sleep disturbances is that it may help identify prevention targets. Rumination and AS are both modifiable with short-term (targeted) interventions [51–53]. Hence, while societal efforts continue to target change in observable manifestations of racism, such as discrimination, acculturative stress, and lower SES, there may be an opportunity to address sleep duration and quality by focusing intervention efforts on factors that may amplify (or, conversely, ameliorate) the deleterious effects of these stressors. Accordingly, the current study is designed to investigate relations between both rumination and AS and sleep outcomes in a racially and ethnically diverse sample of adults, with a focus on both the direct and interactive effects of these factors with race- and ethnicity-related stressors.
We hypothesized that rumination and AS would each be related to shorter sleep duration and lower sleep quality in a racially and ethnically diverse sample. Further, we hypothesized that rumination and AS would act as amplifying factors, moderating the relation between three race- and ethnicity-related stressors—perceived racial/ethnic discrimination, acculturative stress, and indices of socioeconomic status—and both sleep duration and quality. Consistent with previous studies (e.g., Pillai et al. [38]), we hypothesized that the association between rumination and sleep duration and quality would not be fully explained by consideration of depression severity.
Methods
Participants and Procedures
Participants were drawn from a larger study of mental and physical health among racial- and ethnic-minority college students who were recruited from a large, southwestern university. Proficiency in English (to ensure comprehension of study questions) was required. Participants were recruited via flyers and online posts, inviting participation with racial/ethnic identification other than White non-Hispanic/Latinx. After providing electronic consent through Qualtrics, participants completed questionnaires examining demographic information, sleep, mental health symptoms, and related factors (e.g., depressed mood, rumination, AS), and race- and ethnicity-related stressors. Participants received extra credit for their psychology courses as compensation.
Given age-related differences in sleep duration and quality, with evidence for an inflection point around age [50, 54] we selected only individuals below age 50 for this study. Further, only individuals who completed all sleep assessments were included in analyses (N = 1326). The sample was largely female (81.1%) with a mean age of 21.2 years (SD = 3.91 years; range 18–48). Racial and ethnic status was as follows: 36.0% Asian/Pacific Islander, 35.4% Hispanic/Latinx, 16.8% Black/African American, 3.3% Multiracial, 2.8% Native-American/American Indian, and 4.7% Non-Hispanic White (which included a large sample, 52 of 62, of individuals identifying as White and Middle Eastern). Participants were enrolled between September 2019 through May 2021.
Measures
Participants provided gender, age, race, and ethnicity on a demographics self-report form. Sleep was assessed with the Pittsburgh Sleep Quality Index (PSQI [55]), which is a 19-item self-report questionnaire. The current study focused on the sleep parameters particularly well-represented in the sleep disparities research: sleep duration (primary outcome), and the subjective sleep quality subcomponent and the global score of the PSQI (secondary outcomes). Sleep duration was assessed with the PSQI question, “During the past month, how many hours of actual sleep did you get at night? (This may be different than the number of hours you spent in bed.)” Outliers were rescaled across subjects using a Winsorization procedure: values above or below 3 standard deviations from the mean of the full distribution of sleep duration values (i.e., across all eligible individuals with PSQI data) were rescaled to the last valid value within that range. Subjective sleep quality was assessed with the PSQI question, “During the past month, how would you rate your sleep quality overall?” with the original Likert-type ratings (i.e., 0 = “very good,” 1 = “fairly good,” 2 = “fairly bad,” and 3 = “very bad”) used. The global PSQI score was calculated using all 19 self-report items, with higher values indicating worse sleep quality.
Rumination was assessed with the 5-item Brooding subscale of the Ruminative Responses Scale (RRS [56, 57]). Brooding ruminative style has been particularly implicated as a predictor of negative mental health outcomes like depression compared to a reflective ruminative style (e.g., Nolen-Hoeksema et al. [36]; Treynor et al. [57]) higher scores indicate a greater tendency to ruminate.
AS was assessed with the Short Scale Anxiety Sensitivity Index (SSASI [58]), a 5-item instrument (e.g., “When my thoughts seem to speed up, I worry that I might be going crazy”), with items rated on a 5-point Likert scale ranging from 0 (“very little”) to 4 (“very much”). The SSASI has demonstrated good internal consistency (α = 0.79) and excellent convergent and discriminant validity [57].
Depression was assessed with the Inventory of Depression and Anxiety Symptoms (IDAS [59]), with removal of two items assessing sleep difficulties (“I slept very poorly” and “I had trouble falling asleep”), in order to prevent conceptual overlap with the sleep assessment. Severity of depression was evaluated as a covariate to clarify the unique contribution of rumination and AS.
Stressors related to race and ethnicity were evaluated in three domains: discrimination, acculturative stress, and socioeconomic status. Discrimination was evaluated with the Perceived Ethnic Discrimination Questionnaire (PEDQ [60]), a 22-item instrument that assesses discrimination based on one’s ethnicity across multiple forms of discrimination, including experiences such as verbal rejection and threat/aggression. Participants were asked to rate the frequency of these discriminatory experiences over the past 3 months on a 7-point Likert scale ranging from 1 (“never”) to 7 (“very often”). Acculturative stress was assessed with the Social, Attitudinal, Familial, and Environmental Scale (SAFE [61]), a 24-item measure of acculturative stress, composed of four subscales that examine experiences of social, attitudinal, familial, and environmental acculturative stress. Some SAFE items reflect overt experiences of racism (e.g., “I feel uncomfortable when others make jokes about or put down people of my ethnic background”). Other items assess interpersonal isolation or familial conflict. Individuals are asked to rate each experience or situation according to how stressful it is for them; item responses range from 1 (“not stressful”) to 5 (“extremely stressful”).
The conceptual variable of SES was operationalized as both income and subjective social status. Income was assessed by self-report using a scale from 1 (“$0 to $10 000”) to 8 (“>$100,000”). Subjective social status was assessed with the MacArthur Scale of Subjective Social Status [62, 63], a widely used single-item instrument in which individuals assess their perceived rank relative to others in their (self-defined) community based on their income, education, and job. Our composite SES variable was created by first z-scoring both measures of SES and then averaging the z-scores to get a composite z-score for our estimate of SES.
Due to individual missing values on the questionnaires, mean imputation was used for 7 individuals for the perceived ethnic discrimination variable, 9 individuals for the acculturative stress variable, 4 individuals for the brooding rumination variable, and 9 individuals for the IDAS depression variable. The strategy for missing values affecting the computation of the global PSQI score is described in the analytic plan.
Analytic Plan
We conducted 3 hierarchical multiple linear regression analyses with (A) sleep duration, (B) sleep quality, and (C) PSQI Global Score treated as the respective dependent variables in the three separate hierarchical regression models. Each of the three hierarchical regressions had three steps: Step 1 was a main-effects-only model in which the demographic variables and race- and ethnicity-related stressors were treated as predictors; Step 2 in the hierarchical regression added rumination and AS along with their interactions with the race- and ethnicity-related stressor variables to the model; and Step 3 (the full model) added depression severity as a covariate. Semi-partial r squared (sr2: the proportion of variance accounted for by a variable over and above all the other variables in the regression) is reported as an effect size for each independent variable. All continuous variables were z-scored so that main effects (for discrimination, acculturation stress, SES, rumination, and AS) that were involved in interactions would reflect the average effect of the variable on the outcome. Because the hierarchical regression was repeated 3 times (once for each sleep outcome), Type 1 error may be inflated. Thus, we used the Benjamini-Hochberg method to correct for the false discovery rate. As a result, the p-values that are reported below were those that survived correction for the false discovery rate. p-Values that were < .05 but did not survive correction for the false discovery rate are not reported. Because the PSQI Global Score was not calculable for 155 (11.5%) participants (due to data with impossible scores, i.e., sleep efficiency greater than 100%, negative values, or other illogical incongruities), we conducted an exploratory analysis in which the data that was not calculable was imputed using multiple imputation (MI).
Results
Preliminary Analyses: Characteristics of Core Variables
Table 1 provides distribution characteristics for each of the predictor variables examined. Mean self-reported sleep duration was 7.07 (SD = 1.51, range: 3.0–11.0). 37.3% of the sample reported less than 7 hours of sleep per night. On the PSQI, the mean self-reported sleep quality rating for the sample was 1.20 (SD = 0.68), with 29.1% of the sample reporting ratings of fairly or very bad. The average global PSQI score was 6.16 (SD = 3.42).
| Predictor . | M (SD) or count(%) . |
|---|---|
| Age | 21.21 (3.91) |
| Gender (female) | 1076 (81.1%) |
| Race | |
| Asian | 477 (36.0%) |
| Hispanic/Latinx | 469 (35.4%) |
| Black/African American | 223 (16.8%) |
| White (Non-Hispanic) | 62 (4.7%) |
| Multi | 44 (3.3.%) |
| Native-American/Alaskan | 37 (2.8%) |
| Other | 14 (1.1%) |
| Income (<$10 000) | 937 (70.7%) |
| Subjective social status | 5.69 (2.69) |
| Perceived ethnic discrimination | 45.80 (25.17) |
| Acculturative stress | 54.14 (17.99) |
| Depressive symptoms | 43.11 (13.92) |
| Rumination | 11.28 (4.05) |
| Anxiety sensitivity | 4.65 (4.62) |
| Predictor . | M (SD) or count(%) . |
|---|---|
| Age | 21.21 (3.91) |
| Gender (female) | 1076 (81.1%) |
| Race | |
| Asian | 477 (36.0%) |
| Hispanic/Latinx | 469 (35.4%) |
| Black/African American | 223 (16.8%) |
| White (Non-Hispanic) | 62 (4.7%) |
| Multi | 44 (3.3.%) |
| Native-American/Alaskan | 37 (2.8%) |
| Other | 14 (1.1%) |
| Income (<$10 000) | 937 (70.7%) |
| Subjective social status | 5.69 (2.69) |
| Perceived ethnic discrimination | 45.80 (25.17) |
| Acculturative stress | 54.14 (17.99) |
| Depressive symptoms | 43.11 (13.92) |
| Rumination | 11.28 (4.05) |
| Anxiety sensitivity | 4.65 (4.62) |
| Predictor . | M (SD) or count(%) . |
|---|---|
| Age | 21.21 (3.91) |
| Gender (female) | 1076 (81.1%) |
| Race | |
| Asian | 477 (36.0%) |
| Hispanic/Latinx | 469 (35.4%) |
| Black/African American | 223 (16.8%) |
| White (Non-Hispanic) | 62 (4.7%) |
| Multi | 44 (3.3.%) |
| Native-American/Alaskan | 37 (2.8%) |
| Other | 14 (1.1%) |
| Income (<$10 000) | 937 (70.7%) |
| Subjective social status | 5.69 (2.69) |
| Perceived ethnic discrimination | 45.80 (25.17) |
| Acculturative stress | 54.14 (17.99) |
| Depressive symptoms | 43.11 (13.92) |
| Rumination | 11.28 (4.05) |
| Anxiety sensitivity | 4.65 (4.62) |
| Predictor . | M (SD) or count(%) . |
|---|---|
| Age | 21.21 (3.91) |
| Gender (female) | 1076 (81.1%) |
| Race | |
| Asian | 477 (36.0%) |
| Hispanic/Latinx | 469 (35.4%) |
| Black/African American | 223 (16.8%) |
| White (Non-Hispanic) | 62 (4.7%) |
| Multi | 44 (3.3.%) |
| Native-American/Alaskan | 37 (2.8%) |
| Other | 14 (1.1%) |
| Income (<$10 000) | 937 (70.7%) |
| Subjective social status | 5.69 (2.69) |
| Perceived ethnic discrimination | 45.80 (25.17) |
| Acculturative stress | 54.14 (17.99) |
| Depressive symptoms | 43.11 (13.92) |
| Rumination | 11.28 (4.05) |
| Anxiety sensitivity | 4.65 (4.62) |
Sleep Duration
In step 1 of the hierarchical regression with sleep duration as the outcome, older age significantly predicted shorter sleep duration (b = ‐.126, 95% CI = [‐.197, ‐.056], t(1311) = 3.509, p < .001, sr2 = .01). Of the main effects of the race- and ethnicity-related stressors, only acculturative stress reached significance, such that greater acculturative stress predicted shorter sleep duration (b = ‐.080, 95% CI = [‐.141, ‐.019], t(1311) = 2.59, p =.010, sr2 = .01).
In step 2 of the hierarchical regression for sleep duration, rumination, but not AS, significantly improved prediction. On average, greater rumination was related to shorter sleep duration as a main effect (b = ‐.164, 95% CI = [‐.229, ‐.100], t(1303) = ‐4.970, p < .001, sr2 = .02). Rumination also was a significant moderator of the effect of perceived discrimination on sleep duration (see Figure 1a; interaction b = ‐.088, 95% CI = [‐.159, ‐.017], t(1303) = ‐2.429, p = .015, sr2 = .004). For individuals with high rumination scores (1 SD above the mean), higher perceived discrimination was significantly related to shorter sleep time (b = ‐.102, 95% CI = [‐.193, ‐.011], t(1303) = ‐2.192, p = .029, sr2 = .003), but for those with low rumination scores (1 SD below the mean) perceived discrimination was not related to sleep time (b = .074, 95% CI = [‐.024,.172], t(1303) = ‐1.488, p = .137, sr2 = .002). In the context of the variables that were added to the regression in this second step (rumination, AS, and their interactions with race- and ethnicity-related stress), acculturative stress was no longer related to sleep duration, either as a main effect or in interactions with rumination or AS. With these variables in the model, race/ethnicity was related to sleep duration. In particular, Non-Hispanic White participants reported the longest sleep duration, and Black/African American, Hispanic/Latinx, Asian, and multiracial participants all reported shorter sleep duration than the White sample (b = ‐.574, 95% CI = [‐.994, ‐.154], t(1303) = ‐2.679, p = .007, sr2 = .005; b = ‐.471, 95% CI = [‐.864, ‐.078], t(1303) = ‐2.349, p = .019, sr2 = .004; b = ‐.419, 95% CI = [‐.813, ‐.025], t(1303) = ‐2.087, p = .037, sr2 = .003; b = ‐.640, 95% CI = [‐1.213, ‐.067], t(1303) = ‐2.192, p = .029, sr2 = .004, respectively), where the b is the difference in sleep duration between each group and the average of the White participants. Greater age remained related to shorter sleep duration, b = ‐.130, 95% CI = [‐.200, ‐.060], t(1303) = ‐3.652, p < .001, sr2 = .01).
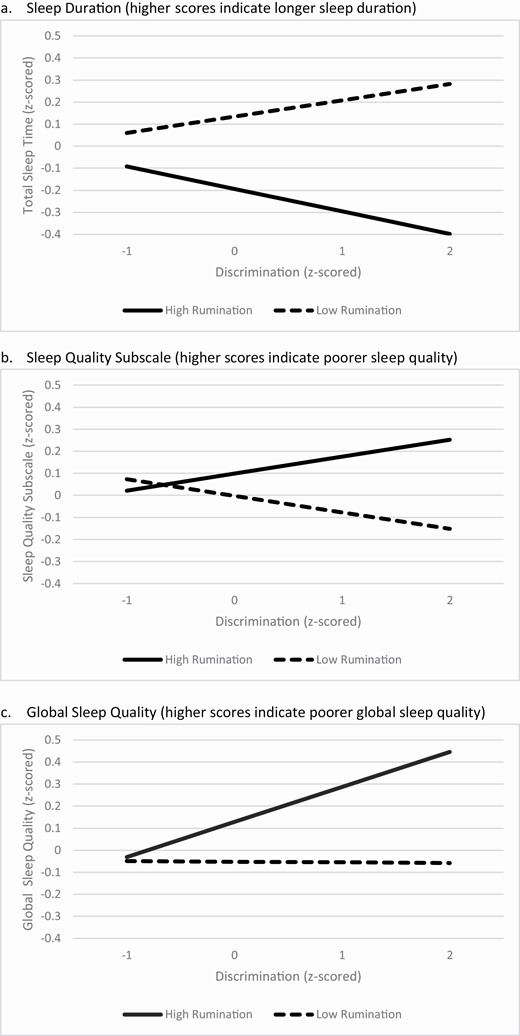
Rumination Moderates the Effect of Discrimination on (A) sleep duration, (B) sleep quality subscale, and (C) global sleep quality.
In step 3 of the hierarchical regression for sleep duration, higher depression severity was associated with shorter sleep duration (b = ‐.207, 95% CI = [‐.289, ‐.133], t(1302) = ‐5.488, p < .001, sr2 = .02). Critically, all the significant effects in model 2 were still significant after accounting for depression severity, including rumination, and its interactions with perceived discrimination.
Sleep Quality Subscale
It is important to note that higher scores on the sleep quality subscale indicate worse sleep quality. In step 1 of the hierarchical regression with the sleep quality subscale as the outcome, sex at birth emerged as significantly related to sleep quality (b = .154, 95% CI = [.016, .291], t(1311) = 2.189, p = .029, sr2 = .004), with women reporting worse sleep quality (i.e., higher scores) than males. No racial/ethnic group reported significantly different sleep quality. As with sleep duration, higher acculturative stress was significantly related to worse sleep quality (b = .140, 95% CI = [.079, .291], t(1311) = 4.534, p < .001, sr2 = .015).
In step 2 of the hierarchical regression for the sleep quality subscale, both higher rumination (b = .215, 95% CI = [.151, .279], t(1303) = 6.602, p < .001. sr2 = .03) and higher AS (b = .093, 95% CI = [.028, 157], t(1303) = 2.826, p = .005, sr2 = .005) were related to poorer sleep quality. However, neither of these variables significantly moderated the association of any of the race- and ethnicity-related stressor variables with sleep quality, all ps >.05.
In step 3 of the hierarchical regression, greater depression severity was associated with poorer sleep quality ratings (b = .428, 95% CI = [.358, .497], t(1302) = 12.01, p <.001, sr2 = .09). In this model (that accounted for variance explained by depression severity), rumination and AS were not related to sleep quality over and above the effects of depression severity. However, rumination moderated the effect of discrimination on sleep quality (see Figure 1b; b = .076, 95% CI = [.009, .142], t(1302) = 2.227, p = .026, sr2 = .004). For participants with high levels of rumination (1 SD above the mean), higher perceived discrimination was marginally related to worse sleep quality (b = .077, 95% CI = [‐.009, .162], t(1302) = 1.763, p = .078, sr2 = .002), However, for participants with low levels of rumination (1 SD below the mean), this relation was negative, although not significant (b = ‐.075, 95% CI = [‐.166, .017], t(1302) = 1.595, p = .111, sr2 = .002).
Global Sleep Quality
It is important to note that higher scores on the global sleep quality scale indicate worse sleep quality. In step 1 of the hierarchical regression with global sleep quality as the outcome, sex at birth was significantly related to sleep quality (b = .158, 95% CI = [.017, .300], t(1160) = 2.191, p = .029, sr2 = .004), with women reporting worse sleep (i.e., higher scores). No racial/ethnic group reported significantly different global sleep quality. As with sleep duration and sleep quality, higher acculturative stress was significantly related to worse sleep (b = .212, 95% CI = [.149, .274], t(1160) = 6.632, p < .001, sr2 = .034). In addition, higher discrimination was related to worse global sleep ratings (b = .098, 95% CI = [.034, .163], t(1150) = 2.996, p = .003, sr2 = .007).
In step 2 of the hierarchical regression for global sleep quality, both higher rumination (b = .275, 95% CI = [.212, .339], t(1152) = 8.541, p < .001, sr2 = .050) and higher AS (b = .179, 95% CI = [.113, 244], t(1152) = 5.346, p < .001, sr2 = .020) predicted poorer global sleep quality. Acculturative stress was no longer related to sleep when controlling for rumination and AS in step 2. Neither AS nor rumination significantly moderated any of the associations between the race- and ethnicity-related variables and global sleep quality, all ps > .074. Finally, in this model, Hispanic/Latinx, and multiracial individuals reported worse overall sleep than White individuals (b = .341, 95% CI = [.088, 593], t(1152) = 2.646, p = .008, sr2 = .005, and b = .437, 95% CI = [.071, 804], t(1152) = 2.342, p = .019, sr2 = .004, respectively).
In step 3 of this hierarchical regression, greater depression severity was associated with poorer global sleep quality ratings (b = .485, 95% CI = [.418, .552], t(1151) = 14.130, p < .001, sr2 = .117). In this model (that accounted for variance explained by depression severity), higher rumination continued to be related to worse overall sleep (b = .090, 95% CI = [.026, 154], t(1151) = 2.755, p = .006, sr2 = .004), but AS was no longer related to overall sleep over and above the effects of depression severity. Furthermore, higher perceived discrimination continued to be related to worse sleep quality overall (b = .078, 95% CI = [.021, .136], t(1151) = 2.686, p = .007, sr2 = .004), and rumination moderated the effect of discrimination on sleep quality (see Figure 1c; b = .081, 95% CI = [.016, .146], t(1151) = 2.460, p = .014, sr2 = .003). For individuals with rumination scores 1 SD above the mean, higher perceived discrimination was significantly related to poorer global sleep quality (b = .160, 95% CI = [.077, .242], t(1151) = 3.775, p < .001, sr2 = .01). However, for individuals with rumination scores 1 SD below the mean, the relation between perceived discrimination and global sleep quality was not present (b = ‐.003, 95% CI = [‐.092, .087], t(1151) = ‐.059, p = .953, sr2 = .000). Importantly, all the other significant effects in model 2 were still significant in model 3 after accounting for depression severity.
Because of missing PSQI Global scores for 155 participants, we conducted an exploratory analysis in which the data that was not calculable was imputed using multiple imputation (MI). Twenty data sets were imputed using all of the variables in the regression models for the imputation. The three hierarchical regression models (1 for each of the 3 sleep outcomes) were then run on the 20 imputed data sets, and pooled results for the regression coefficients from the MI data sets were compared to the results from the regression models using the non-imputed data. With one exception, every significant finding in each of the three models in the non-imputed data set was similarly significant in the MI data set. And every non-significant finding in the non-imputed data set was non-significant in the imputed data set. The one divergent finding was that multiracial individuals did not report significantly worse Global PSQI scores than White individuals (p = .054) in the MI data set, while they did report significantly worse scores in the non-imputed data set (p = .019, see above).
Discussion
Examination of factors related to sleep duration and sleep quality in a racially and ethnically diverse sample provided support for the role of one of the two hypothesized amplification factors. Specifically, rumination was significantly related to all three sleep outcomes (sleep duration, sleep quality subscale, and global sleep quality) both as a main effect (for sleep duration and global sleep quality) and as a moderator of the effects of discrimination for all three sleep outcomes. Importantly, each of these effects were independent of associations with depression severity. The influence of rumination, considered alone, and in interaction with discrimination, accounted for 3–5% of variance in sleep outcomes over and above the other 20 independent variables in the regression. Hence, for our sample, rumination appeared to be an important factor for affecting the relation between race- and ethnicity-related stressors and sleep outcomes. The role of rumination as a moderator may account for some of the variability in findings in the racial/ethnic disparity literature, where variations in the level of rumination in samples may account for whether an association between discrimination findings are or are not found (see Slopen et al.’s review of variable findings [22]). More importantly, one implication of the moderating effects of rumination is that treatment of rumination may help insulate individuals to some degree against adverse consequences of discrimination on sleep duration and sleep quality. Indeed, in our study, we found (across the three sleep outcomes examined) that the frequency of discriminatory experiences was not related to poorer sleep for participants who had low levels of rumination. The magnitude of this protection is difficult to estimate, given the degree of varying estimates of the strength of association between rumination and sleep observed across studies (3–5% of the variance in the current study, in the range of small to moderate effects in other studies) [39, 42, 64].
Although there is other research indicating that rumination prospectively predicts shorter sleep duration and poor sleep quality [64–66], we cannot rule out the possibility that aspects of the associations we observed are due to the reverse causality: shorter sleep duration and poor quality may increase rumination (e.g., Nota and Coles [67]). Also, discrimination and acculturative stress represent prototypic uncontrolled and chronic stressors which may themselves enhance rumination [34]. As such, there may be a cascade of events stemming from race- and ethnicity-related stressors that lead to subsequent elevated rumination tendencies and thus to disrupted sleep. As perhaps a reflection of this shared variance, it is noteworthy that in the current study acculturative stress was significantly associated with poor sleep only when levels of rumination and AS were not considered in the regression model; once these factors were in the model, associations between acculturative stress and sleep were no longer significant. Longitudinal confirmation of the cross-sectional associations identified here will be important to support the hypothesized role of rumination in amplifying race- and ethnicity-associated stress into disrupted sleep duration and quality.
In contrast to these significant effects for rumination, we found little evidence for a direct or interactive effect of AS on sleep outcomes. First, the suggestive relations between AS (as a main effect) and both measures of sleep quality were no longer significant when controlling for depression. And none of the moderating effects of AS survived correction for the false discovery rate. Thus, we found little support for the notion that our brief measure of AS was related to sleep over and above other psychological variables (in particular, rumination, and depression).
Our focus in the current study on factors influencing the impact of race- and ethnicity-associated stressors on sleep duration and quality is informed by research on sleep reactivity. Sleep reactivity refers to the degree to which individuals exhibit sleep-disruptive responses to stress [68, 69]. Rumination has been shown to be important to sleep reactivity more generally [70, 71], but may be particularly apt for understanding the impact of racism and other race- and ethnicity-related stressors on sleep. Such stressors (e.g., discrimination) are natural stimuli for rumination, in that they create a discrepancy with a person’s goals/desired states that cannot be readily resolved [34]. Likewise, rumination has been found to be elevated in groups that have been targeted for marginalization [72, 73], creating a particularly fertile ground for high sleep reactivity for those undergoing such social stressors.
This study is not without several limitations. We recruited a college student sample, for whom sleep duration and quality has important implications for academic success and health [74, 75]. Relationships between the variables studied may be different for those at a different stage of life or within select populations. For example, unlike the current study, AS was found to be a particularly important predictor for understanding racial differences in sleep duration in those with cardiovascular disease [50]. Also, we did not take into account parental SES or financial support relative to participants’ ratings of SES. Further, our study was not designed to evaluate whether racial and ethnic differences in sleep disparities were statistically explained by the variables examined; instead, our sample was composed of individuals responding to advertisements for those with a racial/ethnic identification other than White non-Hispanic/Latinx. Indeed, our sample of individuals self-reporting as White non-Hispanic was composed of a relatively high proportion of individuals reporting a Middle Eastern descent, a group known to face discrimination and challenges from current ethnoracial categorization systems [76]. In addition, our study relied on self-report assessments and focused on sleep duration and quality due to the prevalent reporting of these outcomes in the racial/ethnic disparity sleep literature. A direct measure of insomnia as well as objective measurement of sleep would have allowed for broader comparison to the clinical literature. Finally, our study utilized cross-sectional data; longitudinal study offers the ability to clarify the potential cascade of causality between exposure to racism, amplifying factors, and sleep disruption.
Although it is imperative that behavioral sciences broadly work to dismantle systemic racism, it is also important to identify mechanisms by which racism contributes to health disparities. Our findings here, if confirmed in longitudinal models, suggest a mechanistic target for addressing sleep disparities due to discrimination; reduction in ruminative tendencies that may amplify the deleterious effects of these stressors on sleep. This work is especially important given that these oppressive and often inescapable forms of racism and related stressors continue to hinder the lives—and health—of many people in the United States year after year [32, 77, 78]. Importantly, cognitive-behavior therapy for insomnia, a first line treatment for insomnia [79, 80], has not targeted rumination reliably [81]; hence, additional interventions may be needed for those high in rumination. There is evidence for the efficacy of rumination-focused interventions, as well as cognitive behavioral interventions for depression, in reducing rumination in both prevention [82] and intervention models [52, 82, 83]. Accordingly, these interventions may have a role in targeting ruminations in secondary or tertiary prevention models relevant to addressing sleep disparities.
Funding
Research reported in this publication was supported by the National Institute on Minority Health and Health Disparities (NIMHD) of the National Institutes of Health (NIH) to the University of Houston under Award Number U54MD015946. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Data Availability Statement
Data are available on request.
Financial Disclosure Statement
Although no competing interests are evident for the content of this manuscript, in the interest of full disclosure, the authors would like to acknowledge the following relationships: Dr. Otto receives compensation as a consultant for Big Health, receives book royalties from multiple publishers, and is supported by grants from NIH. Dr. Rosenfield reports stipends from various journals for duties related to their Editorial Boards, and fees from Rosenfield Analytics for data analysis and statistical consulting. In addition, he reports grants from the National Institutes of Health, the DOD, and the Cancer Prevention and Research Institute of Texas for research outside the submitted work. Dr. Zvolensky receives personal fees from Elsevier, Guilford Press, and is supported by grants from NIH, American Cancer Society, and Cancer Research Institute of Texas. Dr. Espie is supported by grants from NIHR-HTA (UK), receives royalties from publishers (Little, Brown; Oxford University Press), and holds shares in and receives salary from Big Health (developer of Sleepio).
Non-Financial Disclosure Statement
None.





Comments