-
PDF
- Split View
-
Views
-
Cite
Cite
Y -X Zhang, T -Y Zhang, J -P Zhou, Z -R Liu, Concurrent reversible splenial lesion syndrome and extrapontine osmotic demyelination syndrome associated with hypernatremia, QJM: An International Journal of Medicine, Volume 117, Issue 8, August 2024, Pages 595–596, https://doi.org/10.1093/qjmed/hcae061
Close - Share Icon Share
Osmotic demyelinating syndrome (ODS), encompassing central pontine and extrapontine involvement, represents a rare acute metabolic disorder.1 Reversible splenial lesion syndrome (RESLES) is a clinico-radiological entity identified by a reversible, localized lesion typically situated in the central part of the splenium of the corpus callosum (SCC).2 This report presents a unique case of concurrent ODS and RESLES in an older patient with hypernatremia, an association rarely documented previously.
A 75-year-old man was admitted for cardiac valve replacement surgery. On the seventh postoperative day, the patient exhibited an acute alteration of mental status. Neurological examination demonstrated that the patient was confused and showed an avoidance response to painful stimuli without specific localizing or lateralizing signs. Laboratory evaluation uncovered severe hypernatremia, with a sodium level of 192.8 mmol/l (normal range: 135.0–145.0 mmol/l), along with elevated plasma osmolality of 393 mOsm/kg (normal range: 292–310 mOsm/kg), without any signs of infection. Brain magnetic resonance imaging (MRI) revealed prominent restricted diffusion along with slight T2 hyperintensities in the central portion of SCC and symmetrical involvement of the bilateral posterior limb of the internal capsule, cerebral peduncles and middle cerebellar peduncles (Figure 1, A–F). The patient’s symptoms improved with a gradual decrease in serum sodium levels through administering hypotonic solutions. Consciousness was restored within 5 days. Follow-up MRI after 2 weeks showed a nearly complete resolution of previously observed signal abnormalities (Figure 1, G–L), confirming a diagnosis of RESLES with concurrent extrapontine ODS.
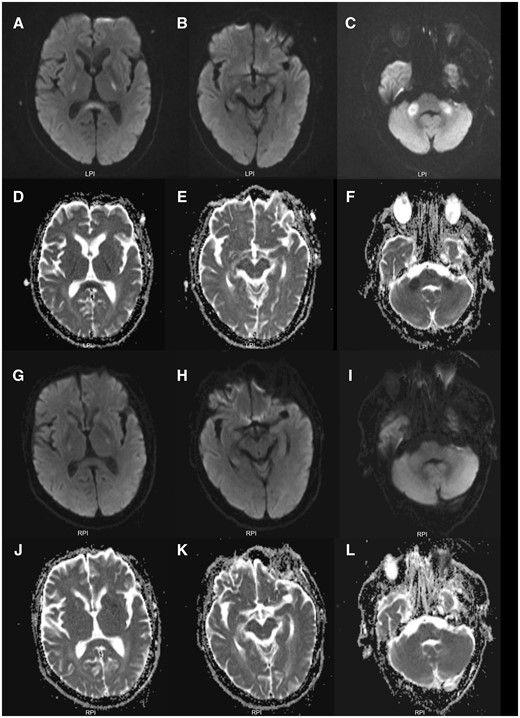
Initial brain MRI scans and repeated brain MRI scans. Initial brain MRI showed prominent hyperintensities on diffusion-weighted imaging (A–C) with decreased apparent diffusion coefficient values (D–F) and mild T2 hyperintensities (not shown) in the splenium of corpus callosum, and bilateral posterior limb of internal capsule, cerebral peduncles and middle cerebellar peduncles, indicating cytotoxic edema. A follow-up brain MRI after 2 weeks demonstrated near-complete resolution of abnormalities on diffusion-weighted imaging (G–I) and apparent diffusion coefficient mapping (J–L).
Extrapontine ODS is characterized by bilateral symmetrical lesions frequently affecting the cerebellum, lateral geniculate body, basal ganglia, thalamus and the external and extreme capsule.3 In this case, the involvement was predominantly in the tracts (internal capsule, cerebral peduncle, middle cerebellar peduncle), a pattern seldom reported. Typically, lesions exhibit increased signal intensity on diffusion-weighted imaging with decreased apparent diffusion coefficient values, particularly in the initial course, indicative of cytotoxic edema associated with acute demyelination,3,4 as observed in our patient.
Furthermore, this case presented with a transient lesion in the SCC, aligning with the characteristics of RESLES; however, it is scarce in ODS. The diagnosis of RESLES primarily relies on its prominent radiographical characteristics (distribution, morphology and the reversible nature of the lesion).2 The presence of cytotoxic edema is considered a key pathological mechanism in RESLES, evidenced by diffusion restriction on neuroimaging.2
Notably, the concurrence of ODS and RESLES in patients with hypernatremia has barely been presented. For this patient, the acute hypernatremia could be attributed to diuretic therapy and inadequate fluid replacement, exacerbated by concerns over cardiac dysfunction, and cytotoxic edema was hypothesized to be involved in the formation of these lesions. The comprehensive resolution of clinical symptoms and extensive brain lesions following the management of hypernatremia represents an extraordinary occurrence, emphasizing the important role of prompt and appropriate treatment.
Our findings expand the clinico-radiological spectrum of these two disorders, suggesting that cytotoxic cerebral edema is a common early imaging hallmark. Early recognition and immediate intervention are critical for achieving a favorable prognosis.
Author contributions
Yin-Xi Zhang (Conceptualization [equal], Data curation [equal], Formal analysis [equal], Investigation [equal], Writing—original draft [equal], Writing—review and editing [equal]), Tian-Yi Zhang (Conceptualization [equal], Data curation [equal], Formal analysis [equal], Investigation [equal], Writing—original draft [equal], Writing—review and editing [equal]), Ji-Ping Zhou (Data curation [equal], Formal analysis [equal], Investigation [equal], Writing—review and editing [equal]) and Zhi-Rong Liu (Conceptualization [equal], Data curation [equal], Formal analysis [equal], Investigation [equal], Supervision [equal], Validation [equal], Writing—review and editing [equal]).
Funding
None.
Conflict of interest
None declared.
Data availability
Anonymized data not published within this article will be made available upon reasonable request from any qualified investigator within 5 years after publication.
References
Author notes
Y.-X. Zhang and T.-Y. Zhang contributed equally to this work.



