-
PDF
- Split View
-
Views
-
Cite
Cite
J Guo, T Xiang, Y Wang, G Yuan, A rare mutation in THRB gene of resistance to thyroid hormone: a case report of a Chinese pedigree, QJM: An International Journal of Medicine, Volume 117, Issue 7, July 2024, Pages 538–540, https://doi.org/10.1093/qjmed/hcae057
Close - Share Icon Share
Clinical manifestations of resistance to thyroid hormone syndrome exhibit a wide range of variations. Here, we present a Chinese pedigree harboring a thyroid hormone receptor beta gene mutation (c.1358C>T) with clinical evidence of thyrotoxicosis.
Case presentation
The proband, a 34-year-old male patient, was initially admitted to another hospital with goiter and symptoms of thyrotoxicosis such as palpitations, irritability, insatiable appetite and heat intolerance since the age of 10. Hormonal assessment revealed elevated triiodothyronine (T3) and thyroxine (T4) levels, contrasting with non-suppressed thyroid-stimulating hormone (TSH). Administered antithyroid therapy for 5 months, the patient’s thyroid hormone (TH) levels slightly dropped while his TSH levels rose dramatically above the upper normal limit. The proposita was then treated with propranolol to control his heart beats and tremor. To differentiate from TSH-secreting adenomas (TSHoma), the high-dose dexamethasone test was performed and it showed a TSH inhibition rate of approximately 65.78%. Afterwards, a 42% TSH inhibition rate was identified during T3 suppression test. Moreover, thyroid ultrasonography revealed a diffuse enlargement. Pituitary enhanced MRI showed decreased enhancement on the right side with an unclear margin. Somatostatin receptor imaging, however, showed no significant findings. Perimetry showed a right temporal scotoma and a left nasal scotoma. No tumor tissues were found during the endonasal exploratory surgery.
The patient was then transferred to our hospital and we conducted Sanger sequencing on the patient and his 18 other family members (Figure 1).
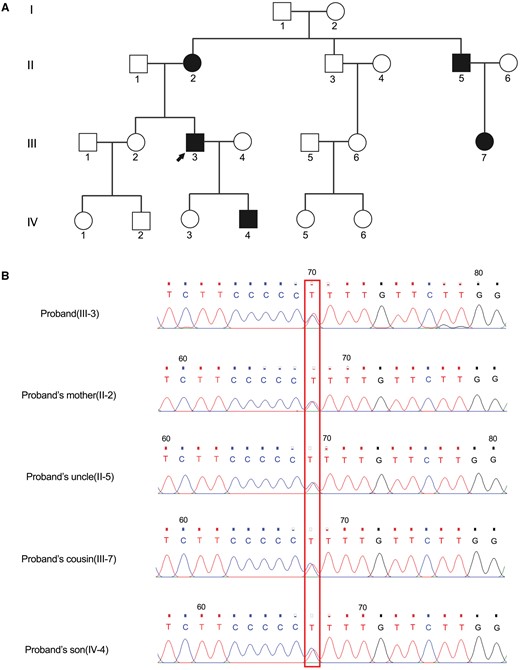
(A) The pedigree of thyroid hormone resistance syndrome. The proband was indicated by the black arrow. (B) Sanger sequencing validated the compound heterozygous variants of c.1358C>T in the proband (III-3), his mother (II-2), his uncle (II-5), his cousin (III-7) and his son (IV-4). The variant sites were marked by the red pane.
Discussion
RTH is an endocrine inherited disorder characterized by reduced responsiveness of the target organ or peripheral tissues to thyroid hormone. Since its first report in 1967,1 a total of 236 different point mutations involving 805 families have been identified,2 which are predominantly located on exons 7–10 of the THRB gene. Clinical phenotype varies mainly depending on the site of hormonal resistance. In our report, the patient’s marked symptoms of thyroid excess indicate that it was the pituitary gland rather than peripheral tissues that were insensitive to TSH stimulation. This suggests a possible diagnosis of pituitary resistance to thyroid hormone (PRTH). While the majority of generalized resistance to thyroid hormone (GRTH) cases are expected to be eumetabolic with high TH levels. Signs of hypothyroidism are often observed in patients with peripheral tissue resistance to thyroid hormone (PTRTH). Other conditions associated with high TH levels and normal TSH include hereditary thyroid hormone-binding globulin hyperplasia, familial dysalbuminemic hyperthyroxinemia (FDH) and TSHoma. However, most of the former two patients are asymptomatic.3 TSHoma usually can be noticed by neurological disturbances or pituitary MRI and is not responsiveness to T3 or dexamethasone administration. Although in recent years, specific cut-off points for the interpretation of dynamic tests have been provided,4 concrete test methods and diagnosis standards still remain inconsistent. Through genetic sequencing analysis, we identified a heterozygous missense mutation c.1358C>T and demonstrated an autosomal dominant mode of inheritance. Mutant THRs not only show low responsiveness to T3 but also interfere with the function of the wild-type receptor by competing binding sites. This is its first report in China since 2009.5 No radical treatment is available at present. The aim of the therapy is to diminish symptoms rather than correct hormone levels. Back to our report, the patient should be treated symptomatically. Beta-blockers can help improve tachycardia due to his relatively mild manifestations. Antithyroid drugs are not recommended as their efficacy in reducing TH is limited. On the contrary, they potentially enhance TSH secretion and may induce hyperplasia of pituitary cells.6 TH substitutive therapy is limited to individuals suffering from hypometabolic signs as delayed growth or learning disabilities. And those without clinical abnormalities typically do not need treatment.
Author contributions
Jia Guo (Formal analysis [equal], Investigation [equal], Writing—original draft [equal]), Tongjun Xiang (Data curation [equal], Investigation [equal]), Yingju Wang (Data curation [equal], Investigation [equal]), and Geheng Yuan (Data curation [equal], Funding acquisition [equal], Methodology [equal], Project administration [equal], Resources [equal], Writing—review & editing [equal])
Conflict of interest
None declared.



