-
PDF
- Split View
-
Views
-
Cite
Cite
J Samanta, G S R S N K Naidu, R Sood, R Nada, A Sharma, S Jain, Calcinosis cutis with amyopathic dermatomyositis, QJM: An International Journal of Medicine, Volume 115, Issue 9, September 2022, Pages 613–614, https://doi.org/10.1093/qjmed/hcac148
Close - Share Icon Share
A 26-year-old female presented with swelling over fingers and elbows with occasional chalky white discharge from them for the last 8 years. There was no history of the Raynaud phenomenon, skin tightening and proximal muscle weakness. She also denied a history of photosensitivity but on examination, there were erythematous macular rashes in sun-exposed areas over the anterior chest, neck and face. There were nodular chalky white soft tissue swellings over the right thumb, index finger and both elbows. Systemic examination was normal. Investigations revealed normal liver enzymes, creatinine kinase, serum calcium, phosphorous, vitamin D and parathormone levels. Plain radiography of hands and elbows revealed calcifications in the subcutaneous tissues consistent with calcinosis cutis (Figure 1A–C). She had anti-nuclear antibody and anti-melanoma-differentiation-associated gene 5 (MDA-5) positivity. Skin biopsy showed perivascular and peri-adnexal lymphomononuclear infiltrate and healed panniculitis consistent with connective tissue disorder (Figure 1D–F). Diagnosis of MDA-5-associated dermatomyositis (DM) with calcinosis cutis was made and was started on hydroxychloroquine and diltiazem.
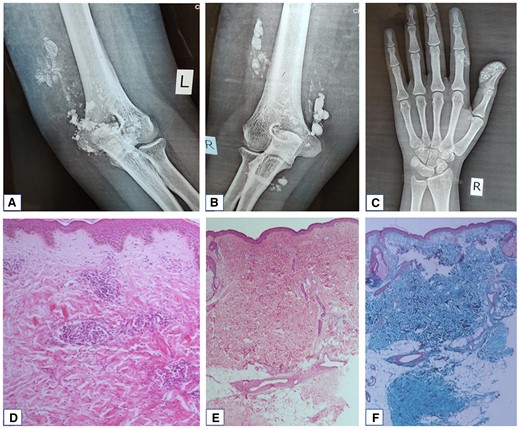
Plain radiographs showing soft tissue calcification around left elbow (A), right elbow (B) and right first and second fingers (C) consistent with calcinosis cutis. Histopathology of skin showing focally atrophic dermis with mild perivascular lymphocytic infiltrates in superficial and deep dermis (D, 100×, hematoxylin and eosin), areas of sclerosis representing healed panniculitis (E, 400×, hematoxylin and eosin), better highlighted on Masson’s trichrome stain (F).
Calcinosis cutis is more frequent in juvenile DM than adult DM patients.1 Reports of calcinosis in MDA-5-associated DM are very limited. Valenzuela et al. reported calcinosis in 5 out of 16 (31.3%) patients with MDA-5 positivity, and Hou et al. reported a case with extensive calcinosis in a patient with MDA-5-associated DM.2,3 Calcinosis cutis can rarely be the presenting manifestation of MDA-5-associated DM, and myositis-specific antibody testing may help in establishing a diagnosis in such patients.
Funding: None declared.
Conflict of interest: None declared.
Consent: A written informed consent was obtained from the patient.



