-
Views
-
Cite
Cite
Lala Allahverdiyeva, G E Agaragimova, Veronica Mugarab Samedi, 96 Sublingual allergen-specific immunotherapy in pediatric patients: biomarkers and molecular allergy diagnostics as predictors of therapeutic success, Paediatrics & Child Health, Volume 25, Issue Supplement_2, August 2020, Page e40, https://doi.org/10.1093/pch/pxaa068.095
Close - Share Icon Share
Abstract
Efficacy of allergen-specific immunotherapy (ASIT) in patients with asthma could be significantly enhanced when physicians have an opportunity to identify those who are most likely to respond, determine when to stop treatment, and predict relapse. Thus, molecular allergy diagnostic is an effective tool that could help to individualize the diagnosis and treatment of asthma by accurate detection of the causative and cross-reactive allergens in pediatric patients. Cytokines are known as reliable diagnostic and prognostic biomarkers for asthma and can be used to evaluate the therapeutic effect.
To evaluate the roles of molecular allergy diagnostic and biomarkers (L-10, IFNγ и TGFβ) as predictors of ASIT efficacy in pediatric patients with asthma.
Eighty children aged 5 to 18 years with mild and moderate atopic bronchial asthma were included in the study. Sixty-eight out of 80 (85%) were found to have sensitization to house dust mites Dermatophagoides Pteronyssinus and/or Dermatophagoides Farinae. All these patients underwent molecular diagnostics using ImmunoCAP (Phadia 100) to determine the major (r Der p1, r Der p 2) and minor allergens (r Der p10) of the house dust mites. Twenty-eight patients with mild and moderate asthma were found to have a high sensitivity to these allergens and received SLIT with a mixture of house dust mites (Dermatophagoides Pteronyssinus and/or Dermatophagoides Farinae). To compare the efficacy of SLIT, we evaluated the severity of asthma clinical symptoms on a point scale from 0 to 3, and biomarker levels (IL-10, IFNγ и TGFβ) before and 6 months after SLIT. Twelve healthy children were included in the study as a reference group.
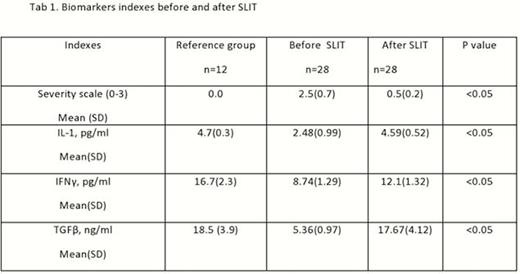
At the beginning of the study, the average daily score in the SLIT group of 2.5 ± 0.7, and after 6 months of treatment, it decreased to 0.5 ± 0.2. The levels of biomarkers were markedly decreased prior to the treatment, especially TGFβ levels, and normalized at the end of treatment (Tab.1).
These findings support the efficacy of molecular diagnosis to determine the efficacy of allergen-specific immunotherapy in patients with asthma.





