-
Views
-
Cite
Cite
Laura M Kinlin, Sarah Carsley, Charles Keown-Stoneman, Natasha Saunders, Karen Tu, Lonnie Zwaigenbaum, Catherine S Birken, 58 Overweight and obesity in children with autism spectrum disorder: Findings from primary care electronic medical records, Paediatrics & Child Health, Volume 25, Issue Supplement_2, August 2020, Page e24, https://doi.org/10.1093/pch/pxaa068.057
Close - Share Icon Share
Abstract
Paediatric overweight and obesity are important public health problems worldwide. Children with autism spectrum disorder (ASD) may be at increased risk compared to their typically-developing peers; however, prevalence estimates in ASD have varied widely and existing studies have largely been limited by use of an external comparison group.
To compare prevalence of overweight and obesity in children and youth (<19 years of age) with and without ASD, using electronic medical record data from paediatric primary care visits.
This was a cross-sectional analysis of EMRPC (Electronic Medical Records Primary Care) data, representing 385 family physicians in 43 clinics in Ontario, Canada. Age- and sex-standardized body mass index (BMI) z-scores were calculated using abstracted heights and weights from the most recent visit between January 2011 and December 2015. Weight status was determined using World Health Organization growth reference standards. ASD was defined using a previously-validated algorithm in EMRPC, based on an ASD-related term in the ‘Cumulative Patient Profile.’ Chi-square test statistics and multinomial logistic regression were used to compare weight status of those with and without ASD.
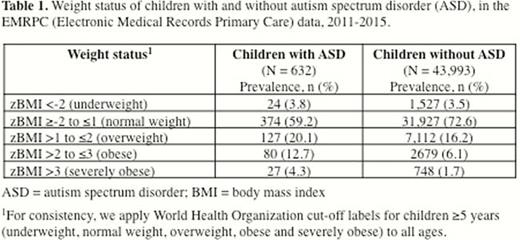
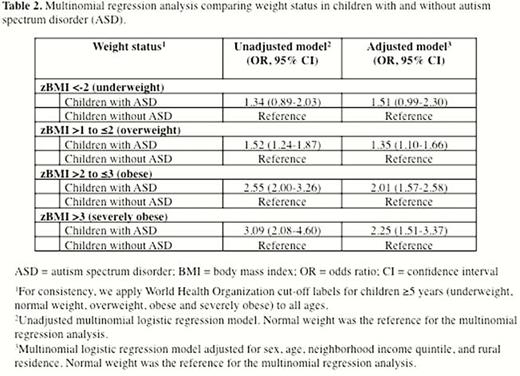
In total, 44,625 children and youth were included, 632 [1.42%] with ASD. Distribution of weight status was significantly different between those with and without ASD (p<0.001) [Table 1]. Compared to their typically-developing peers, children with ASD had significantly higher odds of overweight (unadjusted odds ratio [OR] 1.52; 95% confidence interval [CI] 1.24-1.87), obesity (unadjusted OR 2.55 (2.00-3.26) and severe obesity (unadjusted OR 3.09; 95% CI 2.08-4.60); these associations persisted after adjusting for sex, age, neighborhood income quintile and rural residence (Table 2).
Data from a large primary care database suggest that children with ASD are at substantially increased risk of overweight, obesity and severe obesity. Findings support the need for anticipatory guidance, prevention and management strategies specific to this clinical population. Future work will aim to better understand at what age differences in weight status emerge, and what nutritional, behavioural, or medical factors differentially affect weight status in the ASD population.





