-
PDF
- Split View
-
Views
-
Cite
Cite
Alyssa Ammazzalorso, Jennifer Han, Ebbing Lautenbach, Pranita Tamma, Pranita Tamma, Kerri Thom, Kevin Alby, Emily Blumberg, Warren Bilker, Jacqueline Omorogbe, Pam C Tolomeo, Alissa Werzen, Judith A Anesi, Judith A Anesi, 949. Risk Factors for Subsequent Multidrug-Resistant Gram-Negative Bloodstream Infection Following an Initial Gram-Negative Bloodstream Infection among Solid Organ Transplant Recipients, Open Forum Infectious Diseases, Volume 8, Issue Supplement_1, November 2021, Pages S567–S568, https://doi.org/10.1093/ofid/ofab466.1144
Close - Share Icon Share
Abstract
Multidrug-resistant (MDR) Gram-negative (GN) bloodstream infections (BSI) are a major cause of morbidity and mortality among solid organ transplant recipients (SOTR). We determined risk factors associated with subsequent MDR-GN BSI following an initial Enterobacterales (EB) BSI among SOTRs.
A retrospective cohort study was performed. All SOTR with an EB BSI at the Hospital of the University of Pennsylvania and University of Maryland Medical Center between 1 Jan 2007 and 30 June 2018 and The Johns Hopkins Hospital between 1 Jan 2005 and 31 Dec 2015 were included. The primary outcome was any MDR-GN BSI within 60 days of the EB BSI, including MDR-EB (defined by ceftriaxone MIC ≥8μg/mL), and MDR-Pseudomonas and Acinetobacter (defined by resistance to three or more antibiotic classes). Unadjusted analyses were performed to identify possible risk factors, using a Fisher’s exact or χ 2 test for categorical and Student’s t-test for continuous variables.
Of 988 SOTR with an EB BSI, 138 (14%) had a MDR-GN BSI within 60 days. In unadjusted analyses, possible risk factors for a subsequent MDR-GN BSI (Table 1) included: (1) an index BSI due to extended-spectrum beta-lactamase (ESBL)-producing EB (compared to a susceptible index EB BSI); (2) a carbapenem-resistant EB (CRE) index BSI (compared to a susceptible index EB BSI); (3) exposure to piperacillin-tazobactam or carbapenems in the 6 months prior to the index EB BSI; (4) prior liver transplantation; and (5) need for reoperation within four weeks of the original transplantation. There was no significant association between recurrent MDR-GN BSI and immunosuppression at time of infection, induction immunosuppression history, acute rejection history, or primary graft dysfunction.
Table 1. Risk factors for subsequent MDR-GN BSI following EB BSI among SOTR.
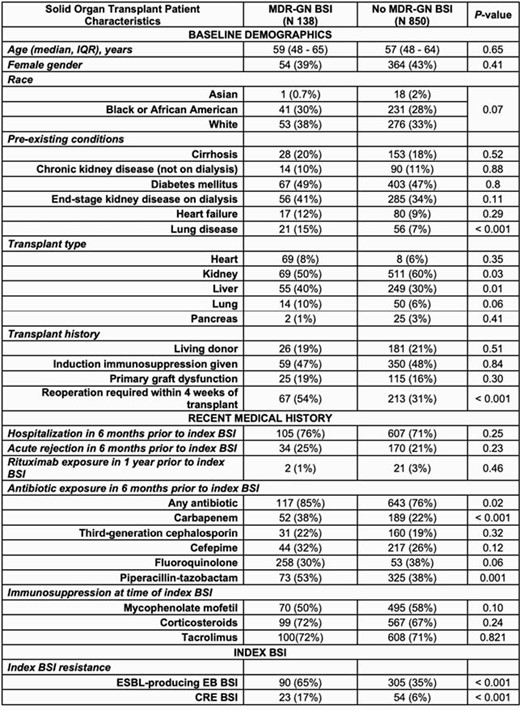
Data are presented as numbers (percentages) except where noted. Abbreviations: BSI, bloodstream infection; CRE, carbapenem-resistant Enterobacterales; EB, Enterobacterales; ESBL, extended-spectrum beta-lactamase; GN, Gram-negative; IQR, interquartile range; MDR, multidrug-resistant
This study shows that liver transplantation, reoperation following transplantation, an index ESBL-EB or CRE BSI, and recent exposure to broad-spectrum beta-lactam antibiotics are associated with an increased odds of subsequent MDR-GN BSI in SOTR, and underscores the need for future studies aimed at preventing emergence of MDR-GN infections in this vulnerable population.
Jennifer Han, MD, MSCE, GlaxoSmithKline (Employee, Shareholder) Ebbing Lautenbach, MD, MPH, MSCE, Merck (Other Financial or Material Support, Member of Data and Safety Monitoring Board (DSMB)) Pranita Tamma, MD, MHS, Nothing to disclose Emily Blumberg, MD, Amplyx (Other Financial or Material Support, Member of Data and Safety Monitoring Board (DSMB))Hologic (Research Grant or Support)Merck (Grant/Research Support, Other Financial or Material Support, Member of Scientific Advisory Committee)Takeda (Research Grant or Support, Other Financial or Material Support, Member of Scientific Advisory Committee) Judith A. Anesi, MD, MSCE, Nothing to disclose
- antibiotics
- ceftriaxone
- beta-lactam antibiotics
- carbapenem
- clinical trials data monitoring committees
- acinetobacter
- advisory committees
- disclosure
- liver transplantation
- maryland
- pseudomonas
- rejection (psychology)
- repeat surgery
- therapeutic immunosuppression
- natural immunosuppression
- infections
- morbidity
- mortality
- transplantation
- transplanted organ
- piperacillin/tazobactam
- extended-spectrum beta lactamases
- bloodstream infections
- interval data
- employee
- primary graft dysfunction
- carbapenem resistance
- primary outcome measure





Comments