-
PDF
- Split View
-
Views
-
Cite
Cite
Ryan C Maves, Stephanie A Richard, David A Lindholm, Nusrat Epsi, Derek T Larson, Christian Conlon, Kyle Everson, Steffen Lis, Paul W Blair, Sharon Chi, Anuradha Ganesan, Simon Pollett, Timothy H Burgess, Brian K Agan, Rhonda E Colombo, Christopher J Colombo, EPICC COVID-19 Cohort Study Group , Predictive Value of an Age-Based Modification of the National Early Warning System in Hospitalized Patients With COVID-19, Open Forum Infectious Diseases, Volume 8, Issue 12, December 2021, ofab421, https://doi.org/10.1093/ofid/ofab421
Close - Share Icon Share
Abstract
Early recognition of high-risk patients with coronavirus disease 2019 (COVID-19) may improve outcomes. Although many predictive scoring systems exist, their complexity may limit utility in COVID-19. We assessed the prognostic performance of the National Early Warning Score (NEWS) and an age-based modification (NEWS+age) among hospitalized COVID-19 patients enrolled in a prospective, multicenter US Military Health System (MHS) observational cohort study.
Hospitalized adults with confirmed COVID-19 not requiring invasive mechanical ventilation at admission and with a baseline NEWS were included. We analyzed each scoring system’s ability to predict key clinical outcomes, including progression to invasive ventilation or death, stratified by baseline severity (low [0–3], medium [4–6], and high [≥7]).
Among 184 included participants, those with low baseline NEWS had significantly shorter hospitalizations (P < .01) and lower maximum illness severity (P < .001). Most (80.2%) of low NEWS vs 15.8% of high NEWS participants required no or at most low-flow oxygen supplementation. Low NEWS (≤3) had a negative predictive value of 97.2% for progression to invasive ventilation or death; a high NEWS (≥7) had high specificity (93.1%) but low positive predictive value (42.1%) for such progression. NEWS+age performed similarly to NEWS at predicting invasive ventilation or death (NEWS+age: area under the receiver operating characteristics curve [AUROC], 0.69; 95% CI, 0.65–0.73; NEWS: AUROC, 0.70; 95% CI, 0.66–0.75).
NEWS and NEWS+age showed similar test characteristics in an MHS COVID-19 cohort. Notably, low baseline scores had an excellent negative predictive value. Given their easy applicability, these scoring systems may be useful in resource-limited settings to identify COVID-19 patients who are unlikely to progress to critical illness.
The coronavirus disease 2019 (COVID-19) pandemic has profoundly impacted health systems worldwide. COVID-19 patients with severe disease often progress to requiring mechanical ventilation and other resource-intense forms of supportive care. Early recognition of patients at low or high risk for critical illness may facilitate the dedication of appropriate resources and improve patient outcomes.
Scoring systems to help clinicians recognize early signs of clinical deterioration or predict risk of mortality exist for a variety of disease states. Several of these, such as the quick Sequential Organ Failure Assessment (qSOFA), CURB-65, and various iterations of the National Early Warning Score (NEWS) have been employed during the COVID-19 pandemic [1–3]; however, questions remain regarding their validity in this disease. There has also been rapid development of numerous novel prognostic scores designed specifically for use in COVID-19 [3–9]. Many of these showed promising results in their initial study populations, but concerns persist about their general applicability due to the risk of bias, limited external validation, and potentially overly optimistic performance estimates in the studies performed to date [10]. Additionally, the complexity of many of the novel scores, which often require extensive laboratory testing and imaging capabilities, hinder their use in resource-limited environments and busy clinical settings.
The use of established prognostic scores for COVID-19 patients may allow for broader adoption, given their existing familiarity and the wide availability of their input variables. NEWS was developed in the United Kingdom to standardize and improve detection of clinical worsening in adult patients and consists of 7 commonly identified physiologic parameters. Patients with an aggregate NEWS score of ≥7 are classified as high clinical risk, and those with a score of 5 or 6 are considered medium risk [11]. NEWS has performed better than qSOFA when predicting in-hospital mortality or intensive care unit (ICU) admission for hospitalized adult patients with and without infection [12]. NEWS has also demonstrated prognostic value for acutely dyspneic patients presenting to the emergency department [13]. NEWS2 is a modification of NEWS that incorporates an additional oxygen saturation scale for patients at risk of hypercapnic respiratory failure and accounts for new-onset confusion [14]. The Royal College of Physicians adopted NEWS2 as the standard for use in the National Health Service (NHS) in England; however, there is ongoing debate whether NEWS2 offers benefit over NEWS [15].
Most studies assessing NEWS and NEWS2 in COVID-19 have been retrospective or single-center; thus, there remains a question regarding how they perform in other populations. One small study suggested that NEWS2 underestimates mortality risk in COVID-19 patients by up to 24% compared with non-COVID-19 patients admitted with equivalent scores during the same period [16]. Variations on NEWS have been suggested to improve the prognostic value in COVID-19. In preparing for the pandemic response in Sichuan Province, China, Liao et al. proposed a modified NEWS incorporating an additional parameter of age ≥65 years as a risk factor to assist with early recognition of patients with severe infection [17]. This proposal was based on epidemiologic data showing a higher severity of illness with advanced age, although no evidence was provided regarding the effectiveness of this approach. Volff et al. reported that this age-based modification of NEWS did not enhance its ability to predict clinical deterioration compared with NEWS alone in a retrospective analysis of 363 patients with COVID-19 [18]. However, Carr et al. reported that the addition of age, C-reactive protein, neutrophil count, estimated glomerular filtration rate, and albumin to NEWS2 resulted in a better risk stratification model for COVID-19 [19].
We assessed the ability of NEWS vs an age-based modification of NEWS (NEWS+age) to predict progression to invasive mechanical ventilation or death among patients hospitalized with COVID-19 who were enrolled in a prospective, multicenter observational cohort study conducted within the United States Military Health System.
METHODS
Participants were enrolled in Epidemiology, Immunology, and Clinical Characteristics of Emerging Infectious Diseases with Pandemic Potential (EPICC), a prospective observational cohort study at 8 military treatment facilities (Brooke Army Medical Center, Fort Belvoir Community Hospital, Madigan Army Medical Center, Naval Medical Center Portsmouth, Naval Medical Center San Diego, Tripler Army Medical Center, William Beaumont Army Medical Center, and Walter Reed National Military Medical Center) from March 23, 2020, through March 10, 2021. Individuals were enrolled if they had confirmed SARS-CoV-2 infection, a COVID-like illness, or were at high risk of developing SARS-CoV-2 infection as a result of exposure. Upon enrollment, research staff collected information including demographics, illness symptoms, and comorbidities from the participant themselves and/or through an electronic health record (EHR) review. Participants in EPICC consent to a 1-year follow-up period, during which they complete periodic surveys, and research staff collect information about hospitalizations from the EHR and review health care encounters from the Military Health System Data Repository.
Adult participants (≥18 years old) were included in this analysis if (1) they were hospitalized for COVID-19; (2) all information needed to calculate a baseline NEWS (respiratory rate, oxygen saturation, supplemental oxygen use, systolic blood pressure, heart rate, and the alert, verbal, pain, unresponsive [AVPU] scale) was available from the time of admission; and (3) treatment data were available for the period of hospitalization, including type of supplemental oxygen therapy (if any). NEWS was categorized as low (0–3), medium (4–6), and high (≥7). This modification of the original NEWS stratification scale (0–4, 5–6, ≥7) is based on a prior study showing that presentation with a score of ≤3 has been associated with emergency department (ED) discharge, whereas higher scores have been associated with hospital admission [13]. We excluded those participants who required invasive mechanical ventilation on the day of admission as our primary outcome of interest was the association of NEWS with maximal illness severity, primarily defined by type of oxygen treatment received.
Oxygen treatment was categorized as follows: low-flow oxygen (≤15 L/min, delivered via nasal cannula or simple mask), high-flow oxygen (>15 L/min and including both high-flow nasal cannula oxygen and noninvasive ventilation), and invasive mechanical ventilation. Illness recovery was defined as participants reporting in their symptom diary (inFLUenza Patient Reported Outcome [FLU-PRO] assessment [20]) that they were back to usual health or activities or reporting in follow-up surveys that their symptoms had resolved.
We calculated NEWS based on NHS guidelines [11] and added 3 points to NEWS if the participant was ≥65 years of age (at time of hospital admission) to create NEWS+age [17]. We compared hospitalization duration and time to recovery among the different NEWS categories using the Kruskal-Wallis rank-sum test, and we compared maximum severity of illness among the different NEWS categories using the Pearson chi-square test. We calculated the sensitivity, specificity, and area under the receiver operating characteristic curve (AUROC) using NEWS cutoffs of 4 and 7 to identify severe outcomes of invasive ventilation and death. Kaplan-Meier survival curves were used to compare time to hospital discharge among those who were discharged within 30 days in the different NEWS categories. To determine the impact of changes in care over the course of the pandemic, we separately analyzed data from the periods of March 2020–August 2020 and September 2020–March 2021. All analyses were performed in RStudio, version 4.0.2 (R Foundation for Statistical Computing) [21, 22].
Patient Consent
All patients, or their designated legal surrogates in the event of incapacitation, provided written informed consent. The design of this study was approved by the Uniformed Services University (USU) Office of Research under protocol IDCRP-085 and by the Institutional Review Boards of the participating sites, in accordance with the Declaration of Helsinki and all applicable US Federal and state laws and regulations.
RESULTS
Of the 330 EPICC participants who required hospitalization as of March 10, 2021, the information necessary to calculate a baseline NEWS was available for 195. Of these, 185 also had complete treatment data at the time of this analysis. One additional participant was excluded due to requiring mechanical ventilation at the time of baseline NEWS ascertainment. This resulted in a total cohort size of 184 for this analysis.
Most participants in this hospitalized cohort were male (65%), ≥45 years old (82%), and had ≥1 prespecified comorbidity (84%) (Table 1). The most common comorbidities were hypertension (53%) and obesity (44%). The majority of participants in the cohort identified as non-White race. There were not any statistically significant differences in cohort demographic and comorbidity characteristics between the low, medium, and high NEWS groups.
| . | Overall Cohort . | Baseline NEWS Category . | . | . | . |
|---|---|---|---|---|---|
| . | Total (n = 184) . | Low (0–3) (n = 106) . | Medium (4–6) (n = 59) . | High (≥7) (n = 19) . | P Value . |
| Age group, No. (%) | .08 | ||||
| 18–44 y | 33 (17.9) | 26 (24.5) | 6 (10.2) | 1 (5.3) | |
| 45–64 y | 91 (49.5) | 46 (43.4) | 33 (55.9) | 12 (63.2) | |
| 65+ y | 60 (32.6) | 34 (32.1) | 20 (33.9) | 6 (31.6) | |
| Age (continuous) | .15 | ||||
| Mean (SD), y | 57.1 (14.8) | 55.4 (15.9) | 59.1 (14.0) | 60.9 (8.9) | |
| Range, y | 20.8–96.1 | 22.1–96.1 | 20.8–89.0 | 43.2–78.6 | |
| Sex: male, No. (%) | 120 (65.2) | 70 (66.0) | 40 (67.8) | 10 (52.6) | .47 |
| Race, No. (%) | .42 | ||||
| Black | 46 (25.0) | 26 (24.5) | 15 (25.4) | 5 (26.3) | |
| Hispanic | 50 (27.2) | 34 (32.1) | 11 (18.6) | 5 (26.3) | |
| Other | 25 (13.6) | 14 (13.2) | 7 (11.9) | 4 (21.1) | |
| White, non-Hispanic | 63 (34.2) | 32 (30.2) | 26 (44.1) | 5 (26.3) | |
| Any comorbidities, No. (%) | 154 (83.7) | 84 (79.2) | 53 (89.8) | 17 (89.5) | .16 |
| Multiple comorbidities, No. (%) | 83 (45.1) | 46 (43.4) | 27 (45.8) | 10 (52.6) | .75 |
| Hypertension, No. (%) | 97 (52.7) | 52 (49.1) | 34 (57.6) | 11 (57.9) | .51 |
| Chronic cardiac condition, No. (%) | 40 (21.7) | 25 (23.6) | 12 (20.3) | 3 (15.8) | .71 |
| Chronic pulmonary disease, No. (%) | 21 (11.4) | 13 (12.3) | 6 (10.2) | 2 (10.5) | .91 |
| Asthma, No. (%) | 19 (10.3) | 13 (12.3) | 4 (6.8) | 2 (10.5) | .54 |
| Chronic neurological disorder, No. (%) | 13 (7.1) | 11 (10.4) | 1 (1.7) | 1 (5.3) | .11 |
| Obesity, No. (%) | 81 (44.0) | 41 (38.7) | 30 (50.8) | 10 (52.6) | .23 |
| Diabetes, No. (%) | 65 (35.3) | 35 (33.0) | 23 (39.0) | 7 (36.8) | .74 |
| . | Overall Cohort . | Baseline NEWS Category . | . | . | . |
|---|---|---|---|---|---|
| . | Total (n = 184) . | Low (0–3) (n = 106) . | Medium (4–6) (n = 59) . | High (≥7) (n = 19) . | P Value . |
| Age group, No. (%) | .08 | ||||
| 18–44 y | 33 (17.9) | 26 (24.5) | 6 (10.2) | 1 (5.3) | |
| 45–64 y | 91 (49.5) | 46 (43.4) | 33 (55.9) | 12 (63.2) | |
| 65+ y | 60 (32.6) | 34 (32.1) | 20 (33.9) | 6 (31.6) | |
| Age (continuous) | .15 | ||||
| Mean (SD), y | 57.1 (14.8) | 55.4 (15.9) | 59.1 (14.0) | 60.9 (8.9) | |
| Range, y | 20.8–96.1 | 22.1–96.1 | 20.8–89.0 | 43.2–78.6 | |
| Sex: male, No. (%) | 120 (65.2) | 70 (66.0) | 40 (67.8) | 10 (52.6) | .47 |
| Race, No. (%) | .42 | ||||
| Black | 46 (25.0) | 26 (24.5) | 15 (25.4) | 5 (26.3) | |
| Hispanic | 50 (27.2) | 34 (32.1) | 11 (18.6) | 5 (26.3) | |
| Other | 25 (13.6) | 14 (13.2) | 7 (11.9) | 4 (21.1) | |
| White, non-Hispanic | 63 (34.2) | 32 (30.2) | 26 (44.1) | 5 (26.3) | |
| Any comorbidities, No. (%) | 154 (83.7) | 84 (79.2) | 53 (89.8) | 17 (89.5) | .16 |
| Multiple comorbidities, No. (%) | 83 (45.1) | 46 (43.4) | 27 (45.8) | 10 (52.6) | .75 |
| Hypertension, No. (%) | 97 (52.7) | 52 (49.1) | 34 (57.6) | 11 (57.9) | .51 |
| Chronic cardiac condition, No. (%) | 40 (21.7) | 25 (23.6) | 12 (20.3) | 3 (15.8) | .71 |
| Chronic pulmonary disease, No. (%) | 21 (11.4) | 13 (12.3) | 6 (10.2) | 2 (10.5) | .91 |
| Asthma, No. (%) | 19 (10.3) | 13 (12.3) | 4 (6.8) | 2 (10.5) | .54 |
| Chronic neurological disorder, No. (%) | 13 (7.1) | 11 (10.4) | 1 (1.7) | 1 (5.3) | .11 |
| Obesity, No. (%) | 81 (44.0) | 41 (38.7) | 30 (50.8) | 10 (52.6) | .23 |
| Diabetes, No. (%) | 65 (35.3) | 35 (33.0) | 23 (39.0) | 7 (36.8) | .74 |
Abbreviation: NEWS, National Early Warning Score.
| . | Overall Cohort . | Baseline NEWS Category . | . | . | . |
|---|---|---|---|---|---|
| . | Total (n = 184) . | Low (0–3) (n = 106) . | Medium (4–6) (n = 59) . | High (≥7) (n = 19) . | P Value . |
| Age group, No. (%) | .08 | ||||
| 18–44 y | 33 (17.9) | 26 (24.5) | 6 (10.2) | 1 (5.3) | |
| 45–64 y | 91 (49.5) | 46 (43.4) | 33 (55.9) | 12 (63.2) | |
| 65+ y | 60 (32.6) | 34 (32.1) | 20 (33.9) | 6 (31.6) | |
| Age (continuous) | .15 | ||||
| Mean (SD), y | 57.1 (14.8) | 55.4 (15.9) | 59.1 (14.0) | 60.9 (8.9) | |
| Range, y | 20.8–96.1 | 22.1–96.1 | 20.8–89.0 | 43.2–78.6 | |
| Sex: male, No. (%) | 120 (65.2) | 70 (66.0) | 40 (67.8) | 10 (52.6) | .47 |
| Race, No. (%) | .42 | ||||
| Black | 46 (25.0) | 26 (24.5) | 15 (25.4) | 5 (26.3) | |
| Hispanic | 50 (27.2) | 34 (32.1) | 11 (18.6) | 5 (26.3) | |
| Other | 25 (13.6) | 14 (13.2) | 7 (11.9) | 4 (21.1) | |
| White, non-Hispanic | 63 (34.2) | 32 (30.2) | 26 (44.1) | 5 (26.3) | |
| Any comorbidities, No. (%) | 154 (83.7) | 84 (79.2) | 53 (89.8) | 17 (89.5) | .16 |
| Multiple comorbidities, No. (%) | 83 (45.1) | 46 (43.4) | 27 (45.8) | 10 (52.6) | .75 |
| Hypertension, No. (%) | 97 (52.7) | 52 (49.1) | 34 (57.6) | 11 (57.9) | .51 |
| Chronic cardiac condition, No. (%) | 40 (21.7) | 25 (23.6) | 12 (20.3) | 3 (15.8) | .71 |
| Chronic pulmonary disease, No. (%) | 21 (11.4) | 13 (12.3) | 6 (10.2) | 2 (10.5) | .91 |
| Asthma, No. (%) | 19 (10.3) | 13 (12.3) | 4 (6.8) | 2 (10.5) | .54 |
| Chronic neurological disorder, No. (%) | 13 (7.1) | 11 (10.4) | 1 (1.7) | 1 (5.3) | .11 |
| Obesity, No. (%) | 81 (44.0) | 41 (38.7) | 30 (50.8) | 10 (52.6) | .23 |
| Diabetes, No. (%) | 65 (35.3) | 35 (33.0) | 23 (39.0) | 7 (36.8) | .74 |
| . | Overall Cohort . | Baseline NEWS Category . | . | . | . |
|---|---|---|---|---|---|
| . | Total (n = 184) . | Low (0–3) (n = 106) . | Medium (4–6) (n = 59) . | High (≥7) (n = 19) . | P Value . |
| Age group, No. (%) | .08 | ||||
| 18–44 y | 33 (17.9) | 26 (24.5) | 6 (10.2) | 1 (5.3) | |
| 45–64 y | 91 (49.5) | 46 (43.4) | 33 (55.9) | 12 (63.2) | |
| 65+ y | 60 (32.6) | 34 (32.1) | 20 (33.9) | 6 (31.6) | |
| Age (continuous) | .15 | ||||
| Mean (SD), y | 57.1 (14.8) | 55.4 (15.9) | 59.1 (14.0) | 60.9 (8.9) | |
| Range, y | 20.8–96.1 | 22.1–96.1 | 20.8–89.0 | 43.2–78.6 | |
| Sex: male, No. (%) | 120 (65.2) | 70 (66.0) | 40 (67.8) | 10 (52.6) | .47 |
| Race, No. (%) | .42 | ||||
| Black | 46 (25.0) | 26 (24.5) | 15 (25.4) | 5 (26.3) | |
| Hispanic | 50 (27.2) | 34 (32.1) | 11 (18.6) | 5 (26.3) | |
| Other | 25 (13.6) | 14 (13.2) | 7 (11.9) | 4 (21.1) | |
| White, non-Hispanic | 63 (34.2) | 32 (30.2) | 26 (44.1) | 5 (26.3) | |
| Any comorbidities, No. (%) | 154 (83.7) | 84 (79.2) | 53 (89.8) | 17 (89.5) | .16 |
| Multiple comorbidities, No. (%) | 83 (45.1) | 46 (43.4) | 27 (45.8) | 10 (52.6) | .75 |
| Hypertension, No. (%) | 97 (52.7) | 52 (49.1) | 34 (57.6) | 11 (57.9) | .51 |
| Chronic cardiac condition, No. (%) | 40 (21.7) | 25 (23.6) | 12 (20.3) | 3 (15.8) | .71 |
| Chronic pulmonary disease, No. (%) | 21 (11.4) | 13 (12.3) | 6 (10.2) | 2 (10.5) | .91 |
| Asthma, No. (%) | 19 (10.3) | 13 (12.3) | 4 (6.8) | 2 (10.5) | .54 |
| Chronic neurological disorder, No. (%) | 13 (7.1) | 11 (10.4) | 1 (1.7) | 1 (5.3) | .11 |
| Obesity, No. (%) | 81 (44.0) | 41 (38.7) | 30 (50.8) | 10 (52.6) | .23 |
| Diabetes, No. (%) | 65 (35.3) | 35 (33.0) | 23 (39.0) | 7 (36.8) | .74 |
Abbreviation: NEWS, National Early Warning Score.
Table 2 shows the outcomes of interest stratified by initial NEWS, including length of hospitalization, time to recovery both from symptom onset and hospital admission, and the maximum severity of illness. There was a statistically significant association between initial NEWS and length of hospitalization, with low NEWS having the shortest stay (median [interquartile range {IQR}], 3 [2–6] days) and high NEWS having the longest (median [IQR], 10 [5.5–13.5] days). Among the 104 participants with recovery data at the time of this analysis, there was no significant difference in either of the time to recovery measures according to NEWS category.
| . | Overall Cohort . | Baseline NEWS Category . | . | . | . |
|---|---|---|---|---|---|
| Outcomes . | Total (n = 184) . | Low (0–3) (n = 106) . | Medium (4–6) (n = 59) . | High (≥7) (n = 19) . | P Value . |
| Length of hospitalization | <.01a | ||||
| Median (Q1, Q3), d | 4.0 (2.0, 8.0) | 3.0 (2.0, 6.0) | 5.0 (3.0, 11.5) | 10.0 (5.5, 13.5) | |
| Min–max, d | 0.0–77.0 | 0.0–77.0 | 1.0–47.0 | 2.0–23.0 | |
| No. | 184 | 106 | 59 | 19 | |
| Onset to recovery | .90a | ||||
| Median (Q1, Q3) | 19.0 (10.75, 30.0) | 19.0 (10.5, 30.0) | 18.0 (13.5, 30.0) | 17.5 (10.5, 20.8) | |
| Min–max | 3.0–210.0 | 3.0–90.0 | 3.0–210.0 | 6.0–60.0 | |
| No. | 104 | 71 | 27 | 6 | |
| Admission to recovery | .83a | ||||
| Median (Q1, Q3) | 11.50 (6.0, 21.0) | 12.0 (5.5, 21.5) | 11.0 (7.5, 18.5) | 11.0 (3.0, 17.5) | |
| Min–max | 0.0–200.0 | 0.0–79.0 | 0.0–200.0 | 0.0–41.0 | |
| No. | 104 | 71 | 27 | 6 | |
| Maximum severity, No. (%) | <.001b | ||||
| No supplemental O2 | 32 (17.4) | 28 (26.4) | 4 (6.8) | 0 (0.0) | |
| Low-flow O2 | 85 (46.2) | 57 (53.8) | 25 (42.4) | 3 (15.8) | |
| High-flow O2 | 41 (22.3) | 17 (16.0) | 16 (27.1) | 8 (42.1) | |
| Invasive ventilation | 13 (7.1) | 2 (1.9) | 6 (10.2) | 5 (26.3) | |
| Death | 13 (7.1) | 2 (1.9) | 8 (13.6) | 3 (15.8) |
| . | Overall Cohort . | Baseline NEWS Category . | . | . | . |
|---|---|---|---|---|---|
| Outcomes . | Total (n = 184) . | Low (0–3) (n = 106) . | Medium (4–6) (n = 59) . | High (≥7) (n = 19) . | P Value . |
| Length of hospitalization | <.01a | ||||
| Median (Q1, Q3), d | 4.0 (2.0, 8.0) | 3.0 (2.0, 6.0) | 5.0 (3.0, 11.5) | 10.0 (5.5, 13.5) | |
| Min–max, d | 0.0–77.0 | 0.0–77.0 | 1.0–47.0 | 2.0–23.0 | |
| No. | 184 | 106 | 59 | 19 | |
| Onset to recovery | .90a | ||||
| Median (Q1, Q3) | 19.0 (10.75, 30.0) | 19.0 (10.5, 30.0) | 18.0 (13.5, 30.0) | 17.5 (10.5, 20.8) | |
| Min–max | 3.0–210.0 | 3.0–90.0 | 3.0–210.0 | 6.0–60.0 | |
| No. | 104 | 71 | 27 | 6 | |
| Admission to recovery | .83a | ||||
| Median (Q1, Q3) | 11.50 (6.0, 21.0) | 12.0 (5.5, 21.5) | 11.0 (7.5, 18.5) | 11.0 (3.0, 17.5) | |
| Min–max | 0.0–200.0 | 0.0–79.0 | 0.0–200.0 | 0.0–41.0 | |
| No. | 104 | 71 | 27 | 6 | |
| Maximum severity, No. (%) | <.001b | ||||
| No supplemental O2 | 32 (17.4) | 28 (26.4) | 4 (6.8) | 0 (0.0) | |
| Low-flow O2 | 85 (46.2) | 57 (53.8) | 25 (42.4) | 3 (15.8) | |
| High-flow O2 | 41 (22.3) | 17 (16.0) | 16 (27.1) | 8 (42.1) | |
| Invasive ventilation | 13 (7.1) | 2 (1.9) | 6 (10.2) | 5 (26.3) | |
| Death | 13 (7.1) | 2 (1.9) | 8 (13.6) | 3 (15.8) |
Abbreviation: NEWS, National Early Warn ing Score.
aP value from Kruskal-Wallis rank-sum test.
bP value from Pearson’s chi-square test.
| . | Overall Cohort . | Baseline NEWS Category . | . | . | . |
|---|---|---|---|---|---|
| Outcomes . | Total (n = 184) . | Low (0–3) (n = 106) . | Medium (4–6) (n = 59) . | High (≥7) (n = 19) . | P Value . |
| Length of hospitalization | <.01a | ||||
| Median (Q1, Q3), d | 4.0 (2.0, 8.0) | 3.0 (2.0, 6.0) | 5.0 (3.0, 11.5) | 10.0 (5.5, 13.5) | |
| Min–max, d | 0.0–77.0 | 0.0–77.0 | 1.0–47.0 | 2.0–23.0 | |
| No. | 184 | 106 | 59 | 19 | |
| Onset to recovery | .90a | ||||
| Median (Q1, Q3) | 19.0 (10.75, 30.0) | 19.0 (10.5, 30.0) | 18.0 (13.5, 30.0) | 17.5 (10.5, 20.8) | |
| Min–max | 3.0–210.0 | 3.0–90.0 | 3.0–210.0 | 6.0–60.0 | |
| No. | 104 | 71 | 27 | 6 | |
| Admission to recovery | .83a | ||||
| Median (Q1, Q3) | 11.50 (6.0, 21.0) | 12.0 (5.5, 21.5) | 11.0 (7.5, 18.5) | 11.0 (3.0, 17.5) | |
| Min–max | 0.0–200.0 | 0.0–79.0 | 0.0–200.0 | 0.0–41.0 | |
| No. | 104 | 71 | 27 | 6 | |
| Maximum severity, No. (%) | <.001b | ||||
| No supplemental O2 | 32 (17.4) | 28 (26.4) | 4 (6.8) | 0 (0.0) | |
| Low-flow O2 | 85 (46.2) | 57 (53.8) | 25 (42.4) | 3 (15.8) | |
| High-flow O2 | 41 (22.3) | 17 (16.0) | 16 (27.1) | 8 (42.1) | |
| Invasive ventilation | 13 (7.1) | 2 (1.9) | 6 (10.2) | 5 (26.3) | |
| Death | 13 (7.1) | 2 (1.9) | 8 (13.6) | 3 (15.8) |
| . | Overall Cohort . | Baseline NEWS Category . | . | . | . |
|---|---|---|---|---|---|
| Outcomes . | Total (n = 184) . | Low (0–3) (n = 106) . | Medium (4–6) (n = 59) . | High (≥7) (n = 19) . | P Value . |
| Length of hospitalization | <.01a | ||||
| Median (Q1, Q3), d | 4.0 (2.0, 8.0) | 3.0 (2.0, 6.0) | 5.0 (3.0, 11.5) | 10.0 (5.5, 13.5) | |
| Min–max, d | 0.0–77.0 | 0.0–77.0 | 1.0–47.0 | 2.0–23.0 | |
| No. | 184 | 106 | 59 | 19 | |
| Onset to recovery | .90a | ||||
| Median (Q1, Q3) | 19.0 (10.75, 30.0) | 19.0 (10.5, 30.0) | 18.0 (13.5, 30.0) | 17.5 (10.5, 20.8) | |
| Min–max | 3.0–210.0 | 3.0–90.0 | 3.0–210.0 | 6.0–60.0 | |
| No. | 104 | 71 | 27 | 6 | |
| Admission to recovery | .83a | ||||
| Median (Q1, Q3) | 11.50 (6.0, 21.0) | 12.0 (5.5, 21.5) | 11.0 (7.5, 18.5) | 11.0 (3.0, 17.5) | |
| Min–max | 0.0–200.0 | 0.0–79.0 | 0.0–200.0 | 0.0–41.0 | |
| No. | 104 | 71 | 27 | 6 | |
| Maximum severity, No. (%) | <.001b | ||||
| No supplemental O2 | 32 (17.4) | 28 (26.4) | 4 (6.8) | 0 (0.0) | |
| Low-flow O2 | 85 (46.2) | 57 (53.8) | 25 (42.4) | 3 (15.8) | |
| High-flow O2 | 41 (22.3) | 17 (16.0) | 16 (27.1) | 8 (42.1) | |
| Invasive ventilation | 13 (7.1) | 2 (1.9) | 6 (10.2) | 5 (26.3) | |
| Death | 13 (7.1) | 2 (1.9) | 8 (13.6) | 3 (15.8) |
Abbreviation: NEWS, National Early Warn ing Score.
aP value from Kruskal-Wallis rank-sum test.
bP value from Pearson’s chi-square test.
The majority of participants did not require invasive ventilation (Table 2). The medium and high NEWS groups had significantly higher maximum illness severity, whereas participants with low NEWS had lower maximum severity (P < .001). Specifically, 80.2% of low NEWS participants vs 15.8% of high NEWS participants required either no supplemental oxygen or only low-flow oxygen. Critical illness (represented by need for invasive ventilation) or death occurred in 3.8%, 23.8%, and 42.1% of the low, medium, and high NEWS groups, respectively.
Figure 1 depicts the distribution of maximal illness severity stratified by baseline NEWS (Figure 1A) and NEWS+age (Figure 1B) in cohort participants hospitalized with COVID-19, suggesting a greater association between higher baseline scores and more severe outcomes with NEWS+age than with NEWS alone.
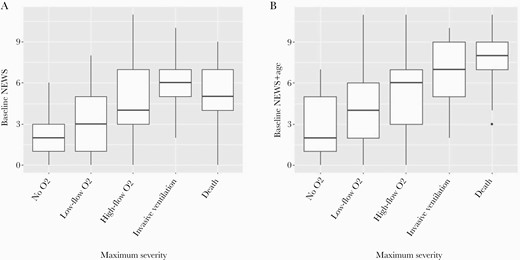
Distribution of baseline NEWS or NEWS+age by maximum severity. A, NEWS. B, NEWS+age. Abbreviation: NEWS, National Early Warning Score.
To better assess the clinical utility of both NEWS and NEWS+age, we analyzed test characteristics corresponding to medium (score of ≥4) (Figure 2A and B) and high (score of ≥7) (Figure 2C and D) thresholds. At a cutoff of ≥4, NEWS (Figure 2A) had moderate sensitivity (87.5%) for detecting increased risk for progression to invasive ventilation or death but limited specificity (64.3%) and poor positive predictive value (PPV; 26.9%). The negative predictive value (NPV) for progression to invasive ventilation or death among those who presented with a score <4 was excellent (97.2%), and it was even higher if the outcome was restricted to death (99.1%). NEWS+age showed similar values for sensitivity (87.5%) and NPV (96.2%) for progression to invasive ventilation or death at this cutoff (Figure 2B).
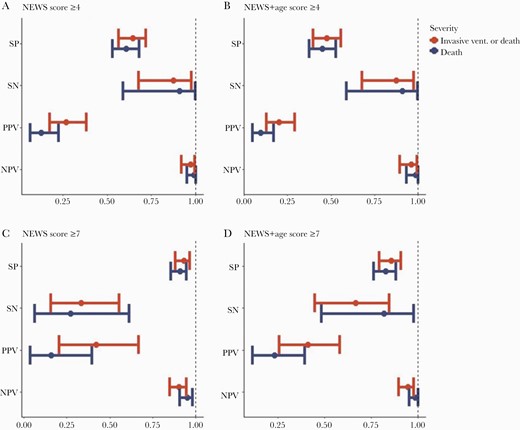
Specificity, sensitivity, positive predictive value, and negative predictive value of baseline NEWS and NEWS+age at designated thresholds. Abbreviation: NEWS, National Early Warning Score.
NEWS of ≥7 (Figure 2C) had high specificity (93.1%) for invasive ventilation or death, as did high NEWS+age (Figure 2D). In this cohort, the NPV for a score <7 was 90.3% with NEWS and 94.5% with NEWS+age. Interestingly, the addition of age to NEWS increased the sensitivity from 33% to 66.7% at a threshold of ≥7. However, the positive predictive value was relatively poor for both NEWS (42.1%) and NEWS+age (41.0%) due to the low prevalence of severe disease overall in the cohort.
When death was assessed alone, NEWS+age showed slightly better overall prognostic value (AUROC, 0.71; 95% CI, 0.66–0.76) than NEWS alone (AUROC, 0.66; 95% CI, 0.59–0.72); however, the difference was not statistically significant. When both invasive ventilation and death were included as outcomes, the performance characteristics of NEWS (AUROC, 0.70; 95% CI, 0.66–0.75) and NEWS+age (AUROC, 0.69; 95% CI, 0.65–0.73) were very similar. The models’ performance varied at different thresholds, with NEWS outperforming NEWS+age at a cut-point of ≥4 (P < .001), whereas NEWS+age was more prognostic than NEWS for a score ≥7 when either death alone or invasive ventilation and death together were considered (P < .02) (Supplementary Table 1). The receiver operating characteristics curves for NEWS and NEWS+age at the different cut-points are depicted in Supplementary Figure 1.
We further analyzed the ability of baseline NEWS and NEWS+age to predict time to hospital discharge (Figure 3). Among those who discharged within 30 days, there was a statistically significant association between risk category and time to hospital discharge for both NEWS (P = .0006) and NEWS+age (P < .001). A larger percentage of participants who had low scores at baseline were more likely to discharge within 30 days than those with baseline medium or high scores (Figure 3).
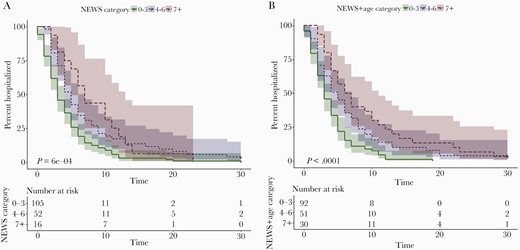
Kaplan-Meier plot of days to hospital discharge by (A) baseline NEWS and (B) NEWS+age. Abbreviation: NEWS, National Early Warning Score.
To account for the impact in changes in care during the course of the pandemic (eg, changes in the use of glucocorticoids or remdesivir), participants enrolled from March 2020–August 2020 (“early group”) were compared with those enrolled from September 2020–March 2021 (“late group”). While the overall risk of death was higher in the early group, the sensitivity, specificity, and positive and negative predictive values of NEWS were comparable to the overall results for both the early and late groups, albeit limited by wide confidence intervals (Supplementary Figures 2 and 3).
DISCUSSION
Surging cases of COVID-19 have required health systems around the world to increase their capacity to provide care rapidly to large numbers of ill patients. In these times, saturation of critical resources, such as ICU beds and mechanical ventilators, contributed to increased mortality rates [23, 24]. In times of COVID-19 surges, NEWS-based risk stratification may assist with care by drawing attention to higher-risk patients requiring closer monitoring, while patients with lower NEWS scores could be safely observed at a less intensive frequency. Improving detection of patients at high (or low) risk of critical illness and death may facilitate interhospital transfer of patients from overwhelmed facilities to hospitals with preserved capacity, thereby enhancing overall system capability and improving patient outcomes [25, 26].
Prognostic scoring in COVID-19 remains challenging despite a growing number of published scoring systems [10]. The performance of these scores has been variable during the pandemic. The Sequential Organ Failure Assessment (SOFA) gained significant attention because of its incorporation into a number of triage algorithms for ventilator allocation by regional and national authorities [27]. However, more recent analyses have suggested that SOFA is inadequate for predicting long-term survival in COVID-19 [28, 29], similar to prior modeling studies of SOFA in pandemic influenza [30].
Unlike SOFA or similar scores, NEWS uses only clinical measurements such as level of consciousness and vital signs and does not require laboratory testing. Thus, it may be rapidly calculated at the time of initial emergency department triage or on the hospital ward. This enhances its applicability in resource-limited settings and times of strained laboratory capacity.
A number of retrospective and often small studies have evaluated the performance of NEWS and similar early warning scores in COVID-19 specifically. In 1 single-center study, NEWS was equivalent or superior to assessment using systemic inflammatory response syndrome (SIRS) and qSOFA in predicting mortality or ICU admission in hospitalized patients with confirmed COVID-19 [1]. Ihle-Hansen et al. similarly found that qSOFA had little utility in COVID-19, whereas higher median NEWS2 scores at presentation were associated with increased risks for ICU admission or death [31]. A NEWS2 score of ≥7 was associated with an increased risk of ICU admission in a series of 68 patients in Italy [32], as was a similar early warning score described in 36 patients treated in Switzerland [33]. Despite these associations, NEWS and NEWS2, with or without the incorporation of age, had generally consistent AUROC scores of <0.75 in these series, suggesting only moderate predictive performance in COVID-19.
The incorporation of age into NEWS was proposed early in the pandemic as a potential way to improve the model’s performance [17], a theory reinforced by observations that mortality in COVID-19 is greatly influenced by age [34]. In our cohort, the addition of age to NEWS had a relatively small impact on the score’s overall predictive power. However, incorporating age did notably improve the ability to predict progression to death (AUROC, 0.82 vs 0.59) and invasive ventilation or death (AUROC, 0.76 vs 0.63) at a cutoff of ≥7. Conversely, NEWS alone seemed to outperform NEWS+age (AUROC, 0.76 vs 0.67) when a lower cutoff (≥4) was employed. It may be that other unmeasured factors influenced by age, such as frailty or physiologic reserve, have a greater influence on COVID-19 mortality [35, 36]. Nonetheless, more complex models validated in large patient populations, such as the Coronavirus Clinical Characterization Consortium (4C) Mortality Score, using a wide array of demographic, historical, physiologic, and laboratory measurements, have not performed significantly better than simpler scores such as NEWS [37].
A concern about many prognostic systems is whether they add anything meaningful to the clinician’s assessment at the bedside; one does not need a score or a laboratory test to know that a hypotensive patient with tachypnea and hypoxemia is sick, for example. However, it is worth noting that a patient with relatively moderate tachypnea (26 breaths per minute), hypoxemia (oxygen saturation of 90%), tachycardia (95 beats per minute), and fever (temperature 38.4°C) would have a NEWS of 8. In our study, a baseline NEWS of ≥7 had high specificity for determining the risk of progression to critical illness or death. Knowing that such a patient who may “look good” in the emergency department is at substantial risk for deterioration is useful for ensuring appropriate disposition and care. This is consistent with prior Italian and Swiss studies evaluating the ability of NEWS2 and a similar early warning score to predict ICU admission in hospitalized patients with COVID-19, finding that a score ≥7 in either model had high reported prognostic accuracy [32, 33].
Positive and negative predictive values are additional clinically significant measures of a test’s performance. In this cohort with low overall mortality rates, the scores had poor positive predictive values at both low and high thresholds. However, the negative predictive value for progression to critical illness or death was excellent, particularly in patients with a baseline NEWS of <4. By identifying patients at low risk of deterioration, more stable patients may be safely admitted to a general ward or potentially even discharged to home. Notably, lower NEWS and NEWS+age categories were also associated with shorter hospitalizations.
The strengths of this study are its prospective nature, demographic diversity, multiple study sites, and the availability of detailed individual participant data. While larger than some prior retrospective studies, our analysis remains limited by a relatively small sample size, low mortality rates, and missing data. In particular, a disproportionately large percentage of missing symptom recovery data among the high (68%) and medium (54%) NEWS groups likely limited the ability to detect a difference in recovery outcomes by baseline NEWS category. Also, as the analysis focused on hospitalized patients, the results may not be generalizable to outpatients. For this analysis, we have not considered prior ED visits that did not result in hospitalization. Other risk factors for severe COVID-19, such as obesity and immunocompromising conditions, are captured in our study data but were not separately evaluated in our analysis here; it is unknown whether NEWS may perform differently in the setting of other such comorbidities. Anti-SARS-CoV-2 monoclonal antibody therapy was not administered to any participant during hospitalization, but we cannot exclude prior receipt of such agents and whether they would have modified the performance of these scoring systems.
In summary, our prospectively obtained data confirm existing evidence that NEWS and NEWS+age may aid in the clinical evaluation of patients with COVID-19, particularly identification of those at low risk of progression to critical illness or death. However, given their AUROCs in the range of 0.6–0.8, they are not sufficiently predictive to independently guide clinical decisions. To date, more complex models that incorporate comorbidities and laboratory markers of organ dysfunction in order to achieve stronger predictive performance have done so at the expense of longer turnaround times [38]. The simple addition of age to NEWS appeared to modestly improve the ability to predict risk of death in our cohort, although there were too few deaths overall to be able to detect a significant difference. Whether the addition of other easily assessed comorbidities and clinical characteristics, such as morbid obesity and frailty, to simple scoring systems such as NEWS or NEWS+age may further enhance their ability to predict severe outcomes is unknown. Further research is needed to develop prognostic models that accurately identify patients at risk for critical illness and death from COVID-19 without sacrificing timely applicability.
Supplementary Data
Supplementary materials are available at Open Forum Infectious Diseases online. Consisting of data provided by the authors to benefit the reader, the posted materials are not copyedited and are the sole responsibility of the authors, so questions or comments should be addressed to the corresponding author.
Acknowledgments
We appreciate the EPICC participants for their central role in this study. Many thanks to the IDCRP team at the clinical research sites—physician/clinical investigators, site managers, regulatory staff, clinical research coordinators, and laboratory personnel—for their support of this study and contributions to its success under very challenging circumstances. The authors would like to thank Camille Estupigan for her editorial assistance.
EPICC COVID-19 Cohort Study Group. We thank the members of the EPICC COVID-19 Cohort Study Group for their many contributions in conducting the study and ensuring effective protocol operations. The following members were all closely involved with the design, implementation, and oversight of the study.
Brooke Army Medical Center, Fort Sam Houston, TX: J. Cowden; D. Lindholm; A. Markelz; K. Mende; S. Merritt; T. Merritt; R. Walter; CPT T. Wellington.
Carl R. Darnall Army Medical Center, Fort Hood, TX: MAJ S. Bazan; S. Michel.
Fort Belvoir Community Hospital, Fort Belvoir, VA: L. Brandon; MAJ E. Ewers; LCDR K. Gallagher; LCDR D. Larson; MAJ M. Odom.
Madigan Army Medical Center, Joint Base Lewis McChord, WA: LTC C. Colombo; R. Colombo; CPT C. Conlon; CPT K. Everson; LTC P. Faestel; COL T. Ferguson; MAJ L. Gordon; LTC S. Grogan; CPT S. Lis; M. Martin; COL C. Mount; LTC D. Musfeldt; CPT D. Odineal; W. Robb-McGrath; MAJ R. Sainato; C. Schofield; COL C. Skinner; M. Stein; MAJ M. Switzer; MAJ M. Timlin; MAJ S. Wood.
Naval Medical Center Portsmouth, Portsmouth, VA: G. Atwood; R. Carpenter; LCDR C. Eickhoff; CAPT K. Kronmann; T. Lalani; LCDR T. Lee; T. Warkentien.
Naval Medical Center San Diego, San Diego, CA: CAPT J. Arnold; CDR C. Berjohn; LCDR S. Husain; N. Kirkland; LCDR A. Lane; CAPT R. Maves; J. Parrish; G. Utz.
Tripler Army Medical Center, Honolulu, HI: S. Chi; MAJ E. Filan; K. Fong; S. Hopkinson; T. Horseman; MAJ M. Jones; COL A. Kanis; LTC A. Kayatani; MAJ W. Londeree; LTC C. Madar; MAJ J. Masel; MAJ M. McMahon; K. Miyasato; G. Murphy; COL V. Nguay; K. O’Connor; P. Schmidt; MAJ E. Schoenman; S. Scrivner; C. Uyehara; LTC R. Villacortalyew.
Uniformed Services University of the Health Sciences, Bethesda, MD: B. Agan; C. Broder; D. Brody; CAPT T. Burgess; C. Byrne; COL K. Chung; C. Coles; C. Dalgard; J.S. Dumler; C. English; M. Haigney; COL P. Hickey; E. Laing; LTC J. Livezey; A. Malloy; R. McLeroy; E. Millar; COL T. Oliver; S. Pollett; COL M. Rajnik; S. Richard; J. Rozman; J. Rusiecki; M. Sanchez; A. Scher; CDR M. Simons; A. Snow; D. Tribble.
Walter Reed Army Institute of Research, Silver Spring, MD: I. Berry; J. Currier; J. Darden; H. Friberg; LTC C. Lanteri; S. Peel.
Walter Reed National Military Medical Center, Bethesda, MD: P. Bhatia; A. Ganesan; MAJ N. Huprikar; M. Oyeneyin.
William Beaumont Army Medical Center, El Paso, TX: CPT M. Banda; CPT B. Davis; MAJ T. Hunter; CPT O. Ikpekpe-Magege; CPT S. Kemp; R. Mody; R. Resendez
Womack Army Medical Center, Fort Bragg, TX: MAJ A. Farmer; LTC D. Hostler; C. Maldonado; J. Mehrer; MAJ R. Radcliffe; MAJ D. Shaha; M. Swain; J. Weiss.
Financial support. This work was supported by awards from the Defense Health Program and the CARES Act (HU00012020067) and the National Institute of Allergy and Infectious Disease (HU00011920111). The protocol was executed by the Infectious Disease Clinical Research Program (IDCRP), a Department of Defense (DoD) program executed by the Uniformed Services University of the Health Sciences (USUHS) through a cooperative agreement by the Henry M. Jackson Foundation for the Advancement of Military Medicine, Inc. (HJF). This project has been funded in part by the National Institute of Allergy and Infectious Diseases at the National Institutes of Health, under an interagency agreement (Y1-AI-5072).
Potential conflicts of interest. All authors: no reported conflicts of interest. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
Disclaimers. The contents of this publication are the sole responsibility of the authors and do not necessarily reflect the views, opinions, or policies of Uniformed Services University of the Health Sciences (USUHS); the Department of Defense (DoD); the Departments of the Army, Navy, or Air Force; Brooke Army Medical Center; Walter Reed National Military Medical Center; Naval Medical Center San Diego; Madigan Army Medical Center; Naval Medical Center Portsmouth; Tripler Army Medical Center; Walter Reed Army Institute of Research; United States Air Force School of Aerospace Medicine; Fort Belvoir Community Hospital; or the Henry M. Jackson Foundation for the Advancement of Military Medicine. Mention of trade names, commercial products, or organizations does not imply endorsement by the US Government. The investigators have adhered to the policies for protection of human subjects as prescribed in 45 CFR 46.
Drs. R. Maves, D. Lindholm, D. Larson, C. Conlon, K. Everson, S. Lis, T. Burgess, and C. Colombo are service members or employees of the US Government. This work was prepared as part of their official duties. Title 17 U.S.C. §105 provides that “Copyright protection under this title is not available for any work of the United States Government.” Title 17 U.S.C. §101 defines a US Government work as a work prepared by a military service member or employee of the US Government as part of that person’s official duties.
References
Author notes
Equal contribution





Comments