-
PDF
- Split View
-
Views
-
Cite
Cite
Nikki Tran, Gregory Eschenauer, Gianni Scappaticci, David Frame, Marisa H Miceli, Twisha S Patel, 578. Infections in Patients Treated with Chimeric Antigen Receptor T-cells (CAR-T) therapy, Open Forum Infectious Diseases, Volume 7, Issue Supplement_1, October 2020, Page S354, https://doi.org/10.1093/ofid/ofaa439.772
Close - Share Icon Share
Abstract
Although chimeric antigen receptor T cells (CAR-T) is a promising novel therapy for the treatment of relapsed or refractory (R/R) B-cell malignancies, data on infectious complications associated with this therapy are limited. Therefore, further assessment of infections after CAR-T therapy is warranted.
We retrospectively reviewed and analyzed infectious complications for 6 months following CAR-T therapy infusion (CTI) in 39 adult and pediatric patients with R/R acute lymphoblastic leukemia (ALL) and Non-Hodgkin Lymphoma (NHL) at Michigan Medicine.
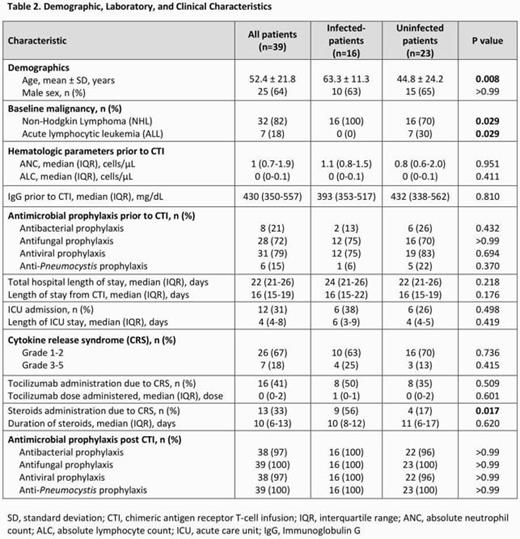
Overall, 20 infections were identified in 16 of 39 patients (41%) following CTI [detailed in Table 1]; 8 (40%) infections occurred in the early period (Day 0–30) and 12 (60%) infections occurred during late period (Day 31–180). The most common infections were viral (n=10, 50%; 80% of viral infections were respiratory viruses), followed by 8 bacterial infections (40%), and 2 fungal infections (10%). More bacterial infections were seen in the early period post-CTI (30% vs. 10%, p = 0.019), whereas viral infections were more common during the late period (40% vs. 10%, p = 0.68). Antimicrobial prophylaxis prior to CTI and following CTI were similar (Table 2). The majority of patients included in the study had NHL (n=32, 82%). Mean age of the cohort was 52 ± 22 years, and 64% were male. 85% of the population developed cytokine release syndrome (CRS) with 67% grade 1–2 and 18% grade 3–5. As shown in Table 2, most baseline characteristics were similar between patients with and without infections post CTI except infected patients were older (63.3 ± 11.3 vs. 44.8 ± 24.2, p = 0.01) and more received steroids for CRS (56% vs 17%, p = 0.02). All-cause mortality within 6 months following CTI was similar in infected and uninfected groups (38% vs 26%, p= 0.50).
Table 1
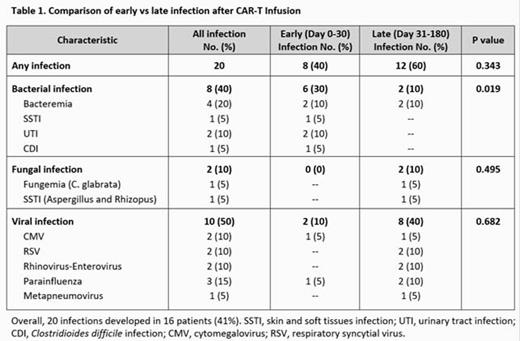
Table 2
Infectious complications are common following CAR-T therapy. We found the majority of infections to be caused by various bacteria or respiratory viruses in a cohort of patients with lymphoma as the most common underlying malignancy.
Marisa H. Miceli, MD, FIDSA, SCYNEXIS, Inc. (Advisor or Review Panel member)
- antibiotic prophylaxis
- acute lymphocytic leukemia
- b-lymphocytes
- bacterial infections
- cancer
- mycoses
- adult
- disclosure
- lymphoma
- lymphoma, non-hodgkin
- michigan
- pediatrics
- steroids
- t-lymphocytes
- virus diseases
- infections
- bacteria
- infection as complication of medical care
- mortality
- viruses
- infusion procedures
- chimeric antigen receptors
- cytokine release syndrome
- chimeric antigen receptor t-cell therapy





Comments