-
PDF
- Split View
-
Views
-
Cite
Cite
Adeel A Butt, Peng Yan, Samia Aslam, Vincent Lo Re III, Obaid Shaikh, 2896. Reduction in Liver-related Mortality Among HCV Infected Persons Is Driven by Attainment of SVR Independent of the Regimen Used: Results from the ERCHIVES Cohort, Open Forum Infectious Diseases, Volume 6, Issue Supplement_2, October 2019, Page S82, https://doi.org/10.1093/ofid/ofz359.174
Close - Share Icon Share
Abstract
Beneficial effect of hepatitis C virus (HCV) treatment with directly acting antiviral agents (DAAs) upon overall mortality is well-established. However, the effect of treatment upon liver-related mortality is not well documented.
We used ERCHIVES database to identify all chronic HCV-infected persons between January 1, 2002 and December 31, 2016. We excluded those with HIV or HBV coinfection or hepatocellular carcinoma. HCV treatment status was defined as prescription of pegylated interferon (PEG)/ribavirin (RBV) for >24 weeks, PEG/RBV plus boceprevir or telaprevir, or a newer DAA regimen for >8 weeks. Propensity score-matched untreated controls were identified for each treated person. We linked HCV+ cases to the National Death Index (NDI) data updated to the end of 2016. Cause of death was retrieved from the underlying cause listed on the death certificate by using ICD‐10 codes. The listed primary cause was assigned as the cause of death. Each cause of death was categorized as “Liver related” or “Not liver related” by two physician members of the study team. Liver-related causes included viral hepatitis-related causes, complications of liver disease, and hepatocellular carcinoma, but excluded any cause where alcohol or any other known liver disease other than viral hepatitis was specified. Discordant results were adjudicated by a third physician member.
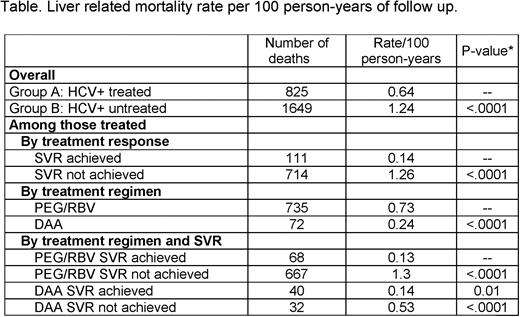
Among 34,412 treated and 21,287 untreated controls, there were 13,098 deaths, of which 2,474 (18.9%) were liver related. Overall liver-related mortality rate per 100 person-years of follow-up was 0.64 in the treated and 1.24 in the untreated group (P). Among the treated group, the liver-related mortality rate per 100 person-years was 0.14 for those who achieved SVR and 1.26 among those who did not achieve SVR. When stratified by treatment regimen, those treated with PG/RBV had a mortality rate of 0.73 vs. 0.24 for those treated with a DAA regimen. However, further stratification by attainment of SVR revealed that the difference between regimens was almost entirely driven by the difference in SVR rates (see table).
HCV-infected persons who receive treatment have a substantial reduction in liver-related mortality. This reduction is largely driven by attainment of SVR and is independent of the regimen use when stratified by SVR attainment.
All Authors: No reported Disclosures.
Session: 310. Hepatitis C: Progress on Elimination and Treatment
Saturday, October 5, 2019: 3:27 PM
- ethanol
- hiv
- liver diseases
- hepatitis
- antiviral agents
- carcinoma, hepatocellular
- cause of death
- death certificates
- disclosure
- follow-up
- ribavirin
- hepatitis b virus
- hepatitis b virus measurement
- liver
- mortality
- viral hepatitis
- hepatitis c virus
- coinfection
- stratification
- peginterferon
- telaprevir
- boceprevir





Comments