-
PDF
- Split View
-
Views
-
Cite
Cite
Pranavi Sreeramoju, Reducing Infections “Together”: A Review of Socioadaptive Approaches, Open Forum Infectious Diseases, Volume 6, Issue 2, February 2019, ofy348, https://doi.org/10.1093/ofid/ofy348
Close - Share Icon Share
Abstract
Reducing healthcare-associated infections often requires the use of both technical and adaptive strategies. The experiences of Semmelweis and Nightingale teach us the importance of social adaptation of technical interventions. Because most infection prevention interventions require widespread participation by healthcare personnel, it is helpful for infectious diseases physicians to learn principles of diffusion of innovations theory and apply them to influence different groups. Comprehensive unit-based program has been successful in reducing device-associated infections. Positive deviance as a socioadaptive approach may be promising. These and other approaches such as social network analysis, relational coordination, link nurses, and stop the line policies need to be further evaluated in future studies. Future research on socioadaptive interventions needs to focus on developing tools and strategies for diagnosing local context and study how these interventions might influence culture of safety. Strategies to sustain momentum of improvement efforts in different healthcare settings need to be refined and further developed through additional research.
Healthcare-associated infections (HAIs) continue to be a public health burden, in spite of acceleration of efforts to reduce their occurrence since publication of “Crossing the Quality Chasm” by the Institute of Medicine [1]. Four percent of hospitalized patients were estimated to have developed an HAI during their hospital stay in 2011 in the United States, with estimated annual occurrence of over 721 000 HAI [2]. These infections cost the US economy over 28 billion dollars in excess healthcare costs [3]. Significant progress has been made over the years, with the proportion of hospitalized patients who develop HAI dropping to 3.2% in 2015 [4]. Per the Centers for Diseases Control and Prevention, which oversees surveillance of these infections through the National Health Safety Network [5], the rate of central line-associated bloodstream infections (CLABSIs) have been reduced by 40%, catheter-associated urinary tract infections (CAUTIs) have been reduced by 46%, surgical site infections (SSIs) after 10 procedures have been reduced by 18%, hospital-onset methicillin-resistant Staphylococcus aureus (MRSA) have been reduced by 9%, and hospital-onset Clostridium difficile infection (CDI) have been reduced by 15%, over a span of 10 years from 2006 to 2016 [6].
Although several evidence-based, best practices to reduce HAI exist, reducing HAI often requires the use of practices beyond known best practices [7]. Both technical solutions (such as making alcohol hand sanitizer and hand washing sinks available and making central line insertion kits available) and adaptive solutions (such as programs to engage clinicians and address social and cultural norms of clinical practice) are necessary. A national collaborative of regional HAI programs [8] identified several social and adaptive challenges encountered by clinicians engaged in improvement initiatives, including (1) initial resistance from several layers of the organization and the need to understand it to foster change and (2) challenges related to frontline staff engagement and empowerment. Because of studies like these, there is increasing recognition for HAI as a sociotechnical problem in the current decade. This review is for modern-day physicians and physicians in training who are expected to participate in interventions to reduce HAI and for those who serve as physician champions or even lead these initiatives, so that they gain a better understanding of socioadaptive approaches that help reduce these infections. Several principles and practices described in this review are also helpful for application in healthcare improvement initiatives not related to infection prevention.
The need for adaptation of an intervention to local social and cultural context is not new in the history of infection prevention. The most important lessons come from the experiences of Ignaz Semmelweis during the period between 1842 and 1847 [9] and those of Florence Nightingale from 1854 to 1860 [10]. Although some situations (eg, need to establish data infrastructures) may not need widespread support and the addition of socioadaptive interventions, situations that require widespread and particularly repetitive participation (eg, hand hygiene, healthcare personnel vaccination, isolation precautions for patients) do require the use of socioadaptive interventions. These interventions (1) help empower teams, (2) address implementation challenges, (3) offer solutions to overcome barriers, (4) promote safety culture, team building, and leadership, (5) promote engagement, (6) promote understanding of the technical components to the end-users, (7) allow translation of technical components into practice, and (8) permit modifications to fit local culture, population, and work flows [11, 12]. They are different from structured educational interventions in that they are much more interactive and promote active learning. These interventions do not substitute the need for science-based technical approaches or the need for proper workplace design and infrastructures that enable infection prevention to occur in healthcare facilities.
FACTORS AFFECTING CLINICIAN BEHAVIOR
Although no clinician is expected to intentionally use poor infection prevention practices, he or she may encounter barriers at different levels, ie, at the level of patient, at the level of peer clinicians, within the multidisciplinary healthcare team, within the healthcare system or the broader environment, or during routine clinical practice. Several predictors of human behavior have been studied in literature [13], such as knowledge, motivation, intention, outcome expectancy, perceived threat, and prevailing norms, regarding the use of infection prevention practices. Several theories have been studied as well [14]. Cognitive theories suggest lack of knowledge of consequences for poor infection prevention practices. Adult learning theories suggest that the clinicians need to have first-hand experiences of complications. Behavioral theories suggest influences of feedback, incentives, and role modeling. Social influence theories suggest that peer pressure has an impact. Marketing theories suggest that there is insufficient messaging in the clinical practice environment. Finally, organizational theories suggest that poor practices are because of poor organization of processes in the healthcare system. To implement behavior change interventions, researchers may need to consider several of these theories, although they are not expected to learn about each one.
PRINCIPLES OF SOCIAL CHANGE AMONG CLINICIANS BASED ON DIFFUSION OF INNOVATIONS THEORY
The principles of diffusion of innovations theory [15, 16] are helpful to understand how a new practice or “change” spreads within an organization or a community of practice. These principles in turn help a physician champion or leader responsible for an improvement initiative to choose appropriate methods to help recruit clinicians to participate in intended change (see Figure 1). Innovators are the initial ~2.5% of people who are the origin of the new idea for change, and they do not need any “recruitment”. Early adopters, who make up approximately 13.5% of the organization, are the next to follow, and they are best recruited through word of mouth and one-to-one conversations. The early majority (~34%) are recruited through small group discussions, meetings, and special interest groups. The late majority (~34%) are recruited through campaigns. Laggards (~16%) are the last to adopt change. Many would focus on implementing change in all the other groups, which may eventually encourage the laggards to participate in intended change. Some organizations may implement accountability measures to make the laggards participate, but this measure is associated with a significant risk of generating resentment among healthcare personnel.
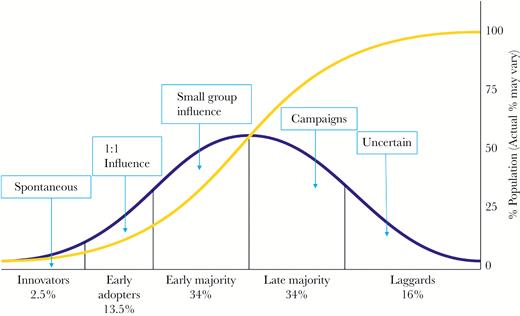
Influencing different groups based on diffusion of innovations theory.
ASSESSMENTS TO BE MADE BEFORE CHOOSING A SOCIOADAPTIVE INTERVENTION
Before embarking on an improvement initiative, the first assessment that needs to be made is whether social adaptation of the intervention is necessary at all. Once it is determined that socioadaptive intervention is a necessary part of the improvement initiative, the next assessment must be to gain an approximate idea of how much buy-in there is already among the intended participants in change. For example, if an initiative has the early majority on board already and needs the late majority to be recruited to ensure success of the initiative, implementing disciplinary measures may not be appropriate and may potentially have adverse consequences. Other assessments to be made include the overall organizational context, exisiting state of conversations, and relationships among the intended participants.
Role of Overall Organizational Context
It is important to gain some idea of the overall organizational context at the time of participating in or leading an improvement initiative. Context helps explain secular trends in outcomes. Don Berwick [17], a renowned expert in healthcare quality, is a proponent of the Context-Methods-Observation model for describing quality improvement initiatives. For example, at Parkland Health and Hospital System, the overarching context for initiatives to improve quality and patient safety during the period September 2011 to July 2013 [18] was a systems improvement agreement with the Centers for Medicare and Medicaid Services. Hand hygiene improvement initiatives were aggressively implemented during this time period. Because all clinicians need to practice hand hygiene during clinical care, and the early majority were already practicing hand hygiene, the organizational need was to recruit the late majority and the laggards to practice hand hygiene. To accomplish this, both campaigns and accountability measures were utilized.
Role of Conversations
Suchman [19] proposes conceptualizing an organization as a set of conversations. This model, he argues, allows the change leader to think of organizational change as something that requires mindful participation instead of having an unrealistic expectation of control. There are patterns to what healthcare personnel are saying and thinking and how people are interacting. Through several iterations and reciprocal interactions, very small changes can amplify and spread. Diversity of thought, he argues, needs to be accompanied by responsiveness to change or else people may hold rigidly to certain thought patterns and practices and the change initiative may fail. By influencing the nature of conversations, change is allowed to occur in organizations. Jordan et al [20] propose that conversations that are informal and unplanned as healthcare personnel go about their daily work (1) have an important role in shaping healthcare interventions, and (2) have the ability to facilitate or block the success of an intervention.
Effective leadership and teamwork processes need to promote healthy productive conversations among frontline personnel and also make it safe for personnel to speak up. In one study, implementation of leadership rounds led to frontline staff engagement, fostered open problem-solving, reduced barriers to implementation, and, subsequently [21], led to measurable reduction in healthcare-associated infections. Psychological safety is built through framing the work as a learning situation, acknowledging that mistakes can happen, and modeling curiosity. Psychological safety and learning climate have been shown to be positively associated with patient safety.
Role of Relationships
Relationships among healthcare personnel are important for ongoing learning, sensemaking, and improvisation. If one takes this approach, one could view adopters of change in healthcare organizations as active transformers of ideas and plans as opposed to passive receivers of interventions. For relationships to be effective in clinical practice, they need to be characterized by trust, mindfulness, sensitivity to the task on hand, and respect [22]. Because preexisting relationships can be a barrier or a facilitator of intervention attempts, those leading change must determine whether the relationships are conducive to productive conversation.
Relational coordination is a concept that is well studied in airline industry, and it is an emerging concept in healthcare. Gittell et al [23] found that there are 7 aspects of relationships between team members that predicted positive outcomes. They showed that a relational coordination score that is an aggregate of measurements on (1) timeliness, (2) accuracy, (3) frequency, and (4) problem-solving nature of communication and (5) respect, (6) goals, and (7) knowledge shared with team members strongly predicted fewer passenger complaints, fewer late arrivals, and fewer baggage handling errors. They repeated their work in different settings, such as knee replacement surgery, and found that the results are reproducible. In one study related to HAI [24], however, RC scores were not different between hospital units with high or low rates of device-associated infections. This lack of effect may be due to study limitations or due to lack of sufficient interdependence between the healthcare personnel to accomplish the task of catheter care (ie, each clinician does the right practice independently of another clinician).
TYPES OF SOCIOADAPTIVE APPROACHES USED TO REDUCE HEALTHCARE-ASSOCIATED INFECTIONS
In this decade, we have seen increased development and application of socioadaptive approaches to reduce healthcare-associated infections. There is a need for further research in this area. Some approaches that have been tried thus far are described below.
Comprehensive Unit-Based Safety Program
Comprehensive unit-based safety program (CUSP) is the leading socioadaptive approach currently and has had increasing adoption in healthcare facilities during this decade. The components of CUSP are educating healthcare personnel on science of safety, identifying defects, engaging executives, having multidisciplinary conversations on learning from defects, and implementing teamwork tools. The questions that guide learning from defects are as follows: What happened? Why did it happen? What will we do to reduce the risk of recurrence? How will we know the risk is reduced?
Several studies have demonstrated the effectiveness of CUSP as an addition to the technical bundle of strategies to reduce device-associated infections. Berenholtz et al [25] reported improvements in CLABSI rates in 1071 intensive care units (ICUs) from 44 states in the United States, which participated in the national collaborative cohort study, “On the CUSP: Stop BSI” sponsored by the Agency for Healthcare Research and Quality (AHRQ). Through implementation of central line bundle that includes hand hygiene, use of chlorhexidine skin preparation, full barrier drape over the patient, sterile attire worn by the person placing the central line and daily review of necessity, along with the socioadaptive bundle, CUSP, the CLABSI rate in these ICUs decreased significantly from 1.96 to 1.15 per 1000 catheter-days at 16–18 months after implementation. Saint et al [26] implemented CUSP along with urinary catheter bundle to reduce CAUTI in 926 hospital units (60% wards, 40% ICUs) nationally through a similar program sponsored by the AHRQ, “On the CUSP: Stop CAUTI”, and demonstrated significant reduction in CAUTI from 2.40 to 2.05 infections per 1000 catheter-days at 12 months after implementation. Mody et al [12] repeated this intervention in 404 nursing homes and demonstrated improvement in CAUTI rate among residents from 6.42 to 3.33 per catheter-days over a 30-month period. However, implementation of CUSP does require presence of strong unit-based leadership structure as well as presence of psychological safety and conditions that allow open and transparent discussions during multidisciplinary team meetings.
Positive Deviance
Positive deviance (PD) [27–30] is a strategy that has gained attention in recent years. It was previously used to successfully solve seemingly intractable and complex social and public health problems. Through intentional inquiry, the PD approach explores social aspects of infection prevention practices among healthcare personnel. In addition to identifying barriers and potential solutions, the approach focuses on identifying and deploying peer role models to generate positive peer pressure and mobilize change. With the PD approach, change begins at the bottom of the organization and spreads upward and laterally throughout the organization. However, for this change to happen, initial permission from the organizational leadership may be needed. In a PD model of change, the frontline personnel have ownership and change happens from “inside out”, instead of having “buy-in” for change ideas presented from outside the group, typically from higher levels of the organizational leadership structure.
Unlike CUSP, implementation of PD does not need strong unit-based leadership structures or structured and scheduled meetings. The inquiry is conducted initially by an external team, with the goal of arousing curiosity among the healthcare personnel so that they continue the dialogues long after the external team ceases involvement. The following open-ended questions are asked of the personnel so that they reflect and evaluate their practices and come forth with solutions. How do you know or recognize when healthcare-associated infection is present? How do you protect yourself, patients and others from transmission of any microorganisms? What prevents you from taking these actions all the time? Is there any group or anyone you know who is able to overcome the barriers frequently and effortlessly? How? Do you have any ideas? What initial steps need to be pursued to make it happen? Any volunteers? Who else needs to be involved?
In the national veterans affairs initiative to reduce MRSA infections [31], PD was used successfully in addition to active surveillance and contact isolation precautions, to reduce healthcare-associated MRSA infections from 1.64 per 1000 patient-days to 0.62 per 1000 patient-days. In a study done at a safety net academic hospital [32], implementation of the PD approach for 9 months in 3 medicine wards was associated with positive impact on culture of safety. Because of a parallel hand hygiene campaign during the study period, secular trends in HAI reduction outweighed the study’s ability to detect difference in HAI reduction due to PD. The composite rate of HAI (CLABSI, CAUTI, CDI, and hospital-associated pneumonia) decreased in 3 control wards from 4.8 to 2.8 infections per 1000 patient-days, whereas the HAI rate in wards where the healthcare personnel received PD intervention reduced from 5.0 to 2.1 infections per 1000 patient days. More research is necessary to evaluate PD as a viable socioadaptive approach for wider use.
Social Network Analysis
Tracing social networks is an important aspect of contact tracing and outbreak investigation in infectious diseases and public health. The idea of analyzing social networks in healthcare settings to influence results of intervention and monitor success of HAI reduction initiatives is relatively new [32, 33]. Networks of relationships are important both for a baseline assessment and for evaluating the impact of intervention. It is important to know who works with who (current or collaboration network), who actually has active projects with who (project network), who would like to work with who (potential or future network), and who seeks ideas from who (innovation or ideas network). Two studies on HAI prevention used social networks to gather qualitative information. In a study to examine the influence of PD approach on healthcare personnel [32], it was found that the bedside nurse, charge nurse, hospital unit manager, patient care technician, and the hospital unit clerk were the most connected in a hospital unit, suggesting that any intervention needing dissemination of information is likely to be more successful when these personnel are empowered and harnessed for implementation success.
Link Nurses and Local Liaisons
Several hospital infection programs utilize local liaisons in the form of unlicensed assistive personnel, physician champions, and link nurses [34, 35]. They act as a link between their own clinical unit and the infection prevention team. Because of their visibility in their own clinical unit or service, they have a greater chance of being accepted by healthcare personnel in the clinical area they are representing, and they may have a greater ability to influence local change in infection prevention practices. Sopirala et al [35] successfully implemented a link nurse program in several hospitals in Ohio and demonstrated reduction in healthcare-associated MRSA bloodstream infections by 41%.
Stop the Line Policies
When healthcare personnel are willing to speak up about errors or opportunities for improvement without fear of retaliation, the safety culture in hospitals tends to be stronger. In a qualitative study in 6 hospitals [36], a positive, nonpunitive culture for speaking up was associated with lower CLABSI rates. Management and organizational factors that contributed to creating a nonpunitive environment for speaking up were as follows: active seeking of feedback by leaders from the frontline healthcare personnel, training of employees to speak up, and availability of multiple reporting and communication tools.
| Situation . | Suggested Intervention . |
|---|---|
| If strong and transparent unit structure with trained managers comfortable analyzing defects | Comprehensive Unit-Based Safety Program |
| If change needed from grassroots | Positive Deviance |
| If teams strong, but issues between teams or issues between individuals | Relational Coordination |
| If processes relatively stable, but local monitoring and support needed | Link Nurses |
| If need to learn patterns of social networking to influence those who are most connected | Social Network Analysis |
| If bedside reminders needed and safety culture is strong | Stop the Line Policies |
| Situation . | Suggested Intervention . |
|---|---|
| If strong and transparent unit structure with trained managers comfortable analyzing defects | Comprehensive Unit-Based Safety Program |
| If change needed from grassroots | Positive Deviance |
| If teams strong, but issues between teams or issues between individuals | Relational Coordination |
| If processes relatively stable, but local monitoring and support needed | Link Nurses |
| If need to learn patterns of social networking to influence those who are most connected | Social Network Analysis |
| If bedside reminders needed and safety culture is strong | Stop the Line Policies |
Table 1 illustrates a suggestion based on the best available expert opinion for matching choice of socioadaptive intervention to the local situation to optimize success of improvement initiative.
| Situation . | Suggested Intervention . |
|---|---|
| If strong and transparent unit structure with trained managers comfortable analyzing defects | Comprehensive Unit-Based Safety Program |
| If change needed from grassroots | Positive Deviance |
| If teams strong, but issues between teams or issues between individuals | Relational Coordination |
| If processes relatively stable, but local monitoring and support needed | Link Nurses |
| If need to learn patterns of social networking to influence those who are most connected | Social Network Analysis |
| If bedside reminders needed and safety culture is strong | Stop the Line Policies |
| Situation . | Suggested Intervention . |
|---|---|
| If strong and transparent unit structure with trained managers comfortable analyzing defects | Comprehensive Unit-Based Safety Program |
| If change needed from grassroots | Positive Deviance |
| If teams strong, but issues between teams or issues between individuals | Relational Coordination |
| If processes relatively stable, but local monitoring and support needed | Link Nurses |
| If need to learn patterns of social networking to influence those who are most connected | Social Network Analysis |
| If bedside reminders needed and safety culture is strong | Stop the Line Policies |
Table 1 illustrates a suggestion based on the best available expert opinion for matching choice of socioadaptive intervention to the local situation to optimize success of improvement initiative.
SOCIOADAPTIVE INTERVENTIONS AND CULTURE OF SAFETY
Culture of safety in healthcare settings is largely measured using the Hospital Survey of Patient Safety Climate tool [37] and, less commonly, using the Safety Attitudes Questionnaire [38]. They measure different aspects of safety culture such as teamwork, management support, and frequency of events reported. A detailed review of culture of safety is beyond the scope this review. Although socioadaptive interventions have been developed in response to social and cultural challenges encountered by implementation teams, their impact on culture of safety is not clear. Meddings et al [39] analyzed the results of two national collaboratives and found that use of CUSP reduced CAUTI and CLABSI without having a measurable impact on culture of safety. In yet another study, Pronovost et al [40] evaluated the impact of CUSP to improve reliability and improve culture in the Keystone ICU project to reduce CLABSI, and team check-up surveys done among ICU teams before and after CUSP intervention demonstrated significant improvement in several aspects of context of care related to patient safety. The CUSP is useful in guiding organizations in learning from important mistakes that cannot be measured as rates. A single institution study using PD showed a positive impact on culture of safety in 3 wards compared with control wards [32]. Healthcare-associated infection reduction can be achieved without a corresponding improvement in culture of safety, although improvement in culture of safety may be necessary for sustainment.
An additional approach to improve the patient safety culture in organizations is “just culture” [41], which provides leaders a framework for evaluating behavior choices of healthcare personnel who fail to use safe patient care practices (eg, hand hygiene). Per just culture, these negative behaviors are classified by human error (inadvertent action), at-risk behavior (behavior that is mistakenly believed to be justified), and reckless behavior (behavior choice that consciously ignores a substantial risk). Classifying unsafe behaviors in this manner allows leaders to apply fair consequences for these behaviors. Although consoling the staff member may be adequate for inadvertent actions, coaching is needed for at-risk behaviors and punishment may be necessary for reckless behavior. Just culture principles help organizations deal with difficult situations in which the generally appropriate focus on systems needs to be shifted towards individual accountability. Just culture principles help change organizational culture towards greater patient safety.
SUSTAINING CHANGE
Sustainment of improvements in HAI rates is necessary to ensure continued patient safety. Sustainability is accomplished once the daily workflows embed an innovation or initiative and the initiative loses its separate identity and becomes the norm. Planning for sustainability needs to happen early in the development of an improvement project. The AHRQ published a model for sustaining and spreading safety interventions [42] to help guide organizations in this direction. Per this model, leadership commits to bold improvement goals. The hospital develops and sustains a strong culture of safety. The safety program has champions who motivate individuals to continue to impove. Interdisciplinary teams create and sustain effective safety practices. Staff learn both technical and adaptive interventions. Frontline staff are empowered to raise safety concerns. Key outcomes are continuously monitored and communicated. Success is communicated and rewarded. Changes that are implemented are incorporated into daily work flows. The publication also provides a sustainability assessment tool and sustainability planning template to help assess project elements and other factors that may influence sustainability and develop an action plan. Ultimately, an organization’s ability to learn determines its growth and survival. The combined knowledge and wisdom of healthcare personnel, patients, families, and patient safety and infection prevention experts helps an organization become a true learning organization.
CONCLUSIONS AND FUTURE DIRECTION
In summary, socioadaptive interventions are necessary additions to technical interventions in an overall multicomponent strategy to reduce healthcare-associated infections. Assessment of local social and cultural context and needs is key to choosing the right socioadaptive approach for any improvement initiative. Future research on socioadaptive interventions needs to be multidisciplinary and focus on identifying tools and strategies for diagnosing local context and study how these interventions might influence culture of safety in a measurable manner. Additional research is needed to develop strategies to sustain momentum of improvement efforts in different healthcare settings.
Acknowledgment
Potential conflicts of interest. All authors: No reported conflicts of interest. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest.
References
Reduction in the prevalence of healthcare-associated infections in U.S. acute care hospitals, 2015 versus 2011. Available at: https://idsa.confex.com/idsa/2017/webprogram/Paper63280.html.





Comments