-
PDF
- Split View
-
Views
-
Cite
Cite
Alexia Y Zhang, Sarah Shrum, Sabrina Williams, Brittany Vonbank, Sherry Hillis, Devra Barter, Sarah Petnic, Lee H Harrison, Ghinwa Dumyati, Erin C Phipps, Rebecca Pierce, William Schaffner, Monica M Farley, Rajal K Mody, Tom Chiller, Brendan R Jackson, Snigdha Vallabhaneni, 1722. The Changing Epidemiology of Candidemia in the United States: Injection Drug Use as an Emerging Risk Factor for Candidemia, Open Forum Infectious Diseases, Volume 5, Issue suppl_1, November 2018, Pages S53–S54, https://doi.org/10.1093/ofid/ofy209.128
Close - Share Icon Share
Abstract
Known risk factors for candidemia include diabetes, malignancy, antibiotics, total parenteral nutrition (TPN), prolonged hospitalization, abdominal surgery, and central venous catheters. Injection drug use (IDU) is not a common risk factor. We used data from CDC Emerging Infections Program’s candidemia surveillance to assess prevalence of IDU among candidemia cases and compare IDU and non-IDU cases.
Active, population-based candidemia surveillance was conducted in 45 counties in 9 states during January–December 2017. Data from 2014 to 2016 were available from 4 states and were used to look for trends. A case was defined as blood culture with Candida in a surveillance area resident. We collected clinical information, including IDU in the past 12 months. Differences between IDU and non-IDU cases were tested using logistic regression.
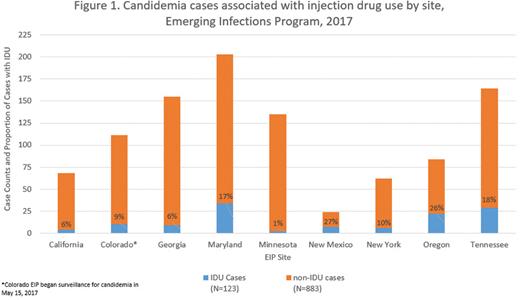
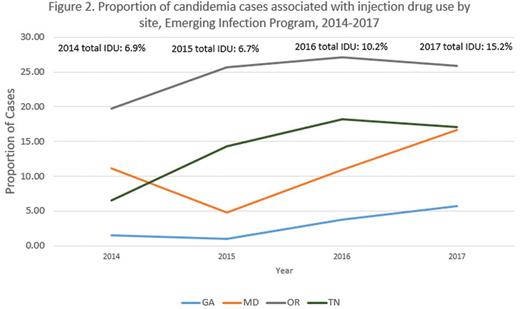
Of 1,018 candidemia cases in 2017, 123 (12%) occurred in the context of recent IDU (1% in Minnesota and 27% in New Mexico) (Figure 1). In the 4 states with pre-2017 data, the proportion of IDU cases increased from 7% in 2014 to 15% in 2017, with the proportion in Tennessee nearly tripling from 7% to 18% (Figure 2). IDU cases were younger than non-IDU cases (median 34 vs. 62 years, P < 0.001). Compared with non-IDU cases, IDU cases were less likely to have diabetes (16% vs. 35%; OR 0.4, CI 0.2–0.6), malignancies (7% vs. 30%; OR 0.2, CI 0.1–0.3), abdominal surgery (6% vs. 19%; OR 0.3, CI 0.1–0.6), receive TPN (6% vs. 27%; OR 0.2, CI 0.1–0.4) and were more likely to have hepatitis C (96% vs. 47%; OR 16.1, CI 10.4–24.9), be homeless (13% vs. 1%; OR 17.8, CI 7.1–44.6), and have polymicrobial blood cultures (33% vs. 17%; OR 2.4, CI 1.6–3.6). Median time from admission to candidemia was 0.5 vs. 3 days and in-hospital mortality was 7% vs. 28% for IDU and non-IDU cases, respectively.
In 2017, 1 in 8 candidemia cases had a history of IDU, including a quarter of cases in some sites. The proportion of such cases increased since 2014. IDU cases lacked many of the typical risk factors for candidemia, suggesting that IDU may be an independent risk factor. Given the growing opioid epidemic, further study is necessary to elucidate how people who inject drugs acquire candidemia and design effective interventions for prevention.
All authors: No reported disclosures.
Session: 200. Public Health: Epidemiology and Outbreaks
Saturday, October 6, 2018: 8:45 AM
- antibiotics
- diabetes mellitus
- diabetes mellitus, type 2
- cancer
- epidemiology
- hepatitis c
- centers for disease control and prevention (u.s.)
- emerging communicable diseases
- disclosure
- homeless persons
- hospital mortality
- internship and residency
- new mexico
- total parenteral nutrition
- tennessee
- candidemia
- intravenous drug users
- abdominal surgery
- homelessness
- surveillance, medical
- blood culture
- candida
- medical residencies
- central venous catheters
- prevention
- opioid epidemic





Comments