-
PDF
- Split View
-
Views
-
Cite
Cite
Chanu Rhee, Maximilian Jentzsch, Sameer S Kadri, Christopher Seymour, Derek Angus, David Murphy, Greg Martin, Raymund Dantes, Lauren Epstein, Anthony E Fiore, John A Jernigan, Robert L Danner, David K Warren, Edward Septimus, Jason Hickok, Russell Poland, Robert Jin, David Fram, Richard Schaaf, Rui Wang, Michael Klompas, 1659. Variation in Identifying Sepsis and Organ Dysfunction Using Administrative Versus Clinical Data and Impact on Hospital Outcome Comparisons, Open Forum Infectious Diseases, Volume 5, Issue suppl_1, November 2018, Pages S49–S50, https://doi.org/10.1093/ofid/ofy209.119
Close - Share Icon Share
Abstract
Administrative claims data are commonly used for sepsis surveillance, research, and quality improvement. However, variations in diagnosis, documentation, and coding practices may confound efforts to benchmark hospital sepsis outcomes using claims data.
We evaluated the sensitivity of claims data for sepsis and organ dysfunction relative to clinical data from the electronic health records of 193 US hospitals. Sepsis was defined clinically using markers of presumed infection (blood cultures and antibiotic administrations) and concurrent organ dysfunction. Organ dysfunction was measured using laboratory data (acute kidney injury, thrombocytopenia, hepatic injury), vasopressor administrations (shock), or mechanical ventilation (respiratory failure). Correlations between hospitals’ sepsis incidence and mortality rates by claims (using “explicit” ICD-9-CM codes for severe sepsis or septic shock) versus clinical data were measured by the Pearson correlation coefficient (r) and relative hospital rankings using either data source were compared. All estimates were reliability-adjusted to account for random variation using hierarchical logistic regression modeling.
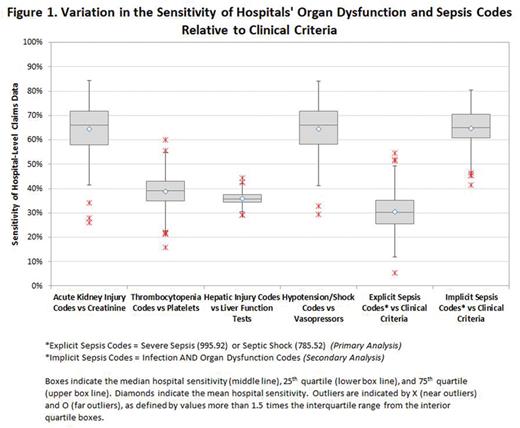
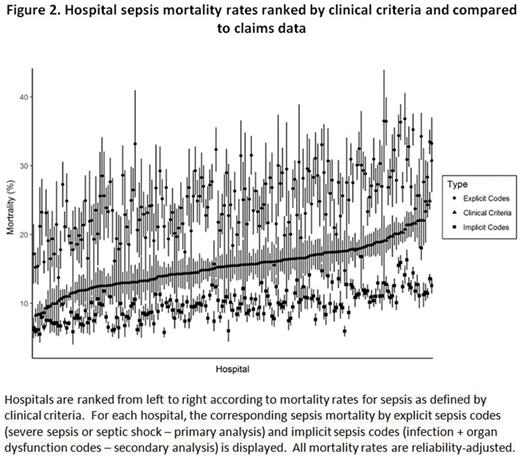
The study cohort included 4.3 million adult hospitalizations in 2013 or 2014. The sensitivity of hospitals’ claims data for sepsis and organ dysfunction was low and variable: median sensitivity 30% (range 5–54%) for sepsis, 66% (range 26–84%) for acute kidney injury, 39% (range 16–60%) for thrombocytopenia, 36% (range 29–44%) for hepatic injury, and 66% (range 29–84%) for shock (Figure 1). There was only moderate correlation between claims and clinical data for hospitals’ sepsis incidence (r = 0.64) and mortality rates (r = 0.61), and relative hospital rankings for sepsis mortality differed substantially using either method (Figure 2). Of 48 (46%) hospitals, 22 ranked in the lowest sepsis mortality quartile by claims shifted to higher mortality quartiles using clinical data.
Variation in the completeness and accuracy of claims data for identifying sepsis and organ dysfunction limits their use for comparing hospital sepsis rates and outcomes. Sepsis surveillance using objective clinical data may facilitate more meaningful hospital comparisons.
All authors: No reported disclosures.
Session: 174. SHEA Featured Oral Abstract
Friday, October 5, 2018: 3:55 PM
- antibiotics
- sepsis
- vasoconstrictor agents
- liver injuries
- septic shock
- renal failure, acute
- adult
- benchmarking
- disclosure
- respiratory insufficiency
- shock
- thrombocytopenia
- infections
- diagnosis
- mortality
- organ failure
- international classification of diseases
- sepsis, severe
- mechanical ventilation
- electronic medical records
- surveillance, medical
- blood culture
- pearson correlation coefficient
- quality improvement
- administrative claims, healthcare





Comments