-
PDF
- Split View
-
Views
-
Cite
Cite
Jehan Z Budak, Kathleen Volkman, Brian R Wood, Shireesha Dhanireddy, Building HIV Workforce Capacity Through a Residency Pathway: Outcomes and Challenges, Open Forum Infectious Diseases, Volume 5, Issue 12, December 2018, ofy317, https://doi.org/10.1093/ofid/ofy317
Close - Share Icon Share
Abstract
To help address the impending HIV physician shortage, we launched an HIV Medicine Pathway within our Internal Medicine Residency in 2008. Between 2015 and 2017, surveys showed a decrease in the number of graduates providing primary care for people living with HIV. We suggest evaluation of long-term outcomes from similar training programs and stronger support for HIV primary care career development.
The need for high-quality primary care for people living with HIV (PLWH) is a pressing public health issue in the United States. Despite an increasing prevalence of PLWH, providers are leaving the workforce, and there are limited HIV-specific training opportunities for physicians and advanced practitioners [1–4]. Inadequate exposure to HIV primary care during medical training results in few qualified providers entering this workforce. Most postgraduate training programs provide little exposure to outpatient HIV care. In 1 survey of internal medicine (IM) residents, 92% had provided inpatient HIV care for more than 10 PLWH, but only 13% had provided outpatient care for more than 10 PLWH [5]. In another survey, IM program directors reported HIV education to be a priority; however, only 47% of programs offered an HIV rotation [6].
In 2008, we created an HIV Medicine Pathway within the University of Washington (UW) IM Residency program with the goal of training IM residents to provide comprehensive care for PLWH. We are aware of only 9 other HIV primary care training opportunities, of varying structure, within US IM residency programs. There are limited data on graduate outcomes and the quality of general IM training for residents in these tracks [7].
The purpose of this report is to assess pathway graduate satisfaction with training in both HIV medicine and general IM and to evaluate retention in the HIV workforce over time.
PROGRAM DESCRIPTION
The HIV Medicine Pathway at UW, an option for both categorical and primary care residents, is part of the 3-year, Accreditation Council of Graduate Medical Education (ACGME)–accredited IM Residency program. On average, 2–4 residents apply during postgraduate year (PGY) 1, and 2–3 selected residents participate in the pathway during their PGY2 and PGY3 years. The track is tailored to individuals who have expressed an interest in HIV primary care, particularly in resource-limited settings. The structure of the pathway is outlined in Figure 1. Residents in the pathway fulfill their ACGME continuity clinic requirement at the Madison Clinic, an academic, Ryan White–funded HIV primary care clinic at Harborview Medical Center in Seattle, Washington (a UW-affiliated county hospital). The clinic serves as the medical home for approximately 2800 PLWH, the majority of whom are from underserved populations. The pathway has minimal cost, as it utilizes preexisting clinical and educational resources. Graduating residents are eligible to complete the American Academy of HIV Medicine (AAHIVM) certification examination.
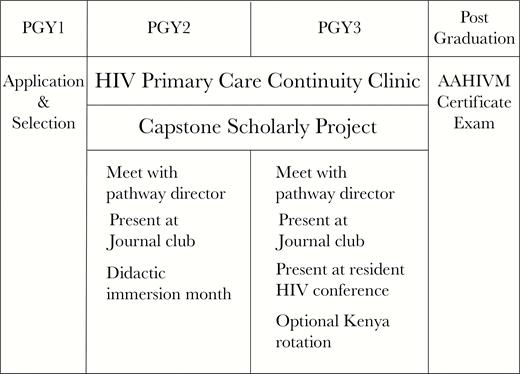
Curricular map for HIV medicine pathway residents. Abbreviations: AAHIVM, American Academy of HIV Medicine; PGY, postgraduate year.
PROGRAM EVALUATION
Twelve trainees completed the pathway between 2008 and 2017. In May 2015, we administered an anonymous electronic survey to pathway residents and graduates regarding practice habits and attitudes toward the pathway. All residents (5) and graduates (7) responded to the survey. Among the graduates surveyed in 2015, 5/7 (71%) were providing care for ≥20 PLWH (the eligibility cutoff to take the AAHIVM certificate exam). Five of 7 (71%) replied that they had attained AAHIVM certification, and 1/7 (14%) had completed fellowship training and obtained board certification in infectious diseases (ID). All respondents (12/12) reported that they would choose to participate in the HIV pathway again and that they anticipated care for PLWH to be part of their future careers.
In March 2017, we administered an anonymous electronic survey to the same 12 individuals surveyed in May 2015. In the follow-up survey, 12 of 12 respondents were pathway graduates. Again, 100% responded, and all felt the HIV pathway was adequate training to provide longitudinal HIV care. Ten of 12 graduates (83%) felt the HIV pathway was adequate training to provide general outpatient IM care to HIV-seronegative adults. Two of 12 (17%) respondents felt the pathway did not provide adequate training in general IM due to deficiencies in women’s health and geriatric medicine. At the time of the 2017 survey, 8/12 (60%) graduates had attained AAHIVM certification.
At the time of the 2017 survey, 2/12 (17%) graduates were providing care to ≥20 PLWH. Those who provided care for <20 PLWH were asked to comment on barriers to finding or sustaining jobs as primary care HIV internists. Reported barriers varied, but several trends emerged. First, working in low-prevalence areas or settings was a theme. Two respondents worked at the Veterans Administration (VA) Puget Sound Medical Center, where there is a relatively low number of PLWH. One respondent worked in a rural setting where disease burden was low, and another pathway graduate was in a general IM practice recruiting PLWH. Second, the majority of pathway graduates felt that additional fellowship training was necessary, as available jobs in urban areas were filled by and/or perceived to be seeking only ID-trained providers. At the time of the survey, 2 graduates not providing care to ≥20 PLWH reported that they planned to enter an ID fellowship. Finally, geography may have been a barrier, as 83% of pathway graduates surveyed remained in the Pacific Northwest region and were potentially competing for the same positions.
DISCUSSION
Specialized training pathways or tracks within residency programs might mitigate expected workforce shortages and offer residents an opportunity to focus on areas of clinical interest, but there are few HIV-focused pathways within residency programs, and little is known about their outcomes. The purpose of this analysis was to assess UW HIV Medicine pathway graduate outcomes in mitigating expected shortages in the HIV provider workforce.
Between 2015 and 2017, among those who graduated from the pathway, we found that the number providing HIV primary care to ≥20 PLWH decreased from 71% (5/7) to 17% (2/12). We found this decrease in workforce to be concerning. Data from other graduate medical education (GME) pathways show high satisfaction with such training programs and favorable graduate outcomes regarding longitudinal care for PLWH, findings that are similar to our 2015 survey [7, 8]. The decrease noted in the UW cohort, however, suggests that early graduate outcomes data may not be predictive of long-term outcomes and that such surveys should be repeated over time.
We asked pathway graduates no longer caring for >20 PLWH to comment on perceived barriers to finding or sustaining jobs in HIV primary care. The most cited reason was the perception that fellowship training was a necessary credential or that graduates felt they had to compete with ID-trained physicians. We anticipate that the 2 graduates currently in an ID fellowship will re-enter this workforce and increase the percentage caring for ≥20 PLWH from 17% to 30%, yet this still represents attrition from 71% in the IM-trained provider workforce. Given the provider workforce shortages that already exist in the fields of IM primary care and ID, we must address practice barriers for primary care providers trained in HIV medicine and support the career development of residency pathway graduates.
Future Directions
Although we found that graduates of the program perceived themselves as well prepared for general IM after residency, future directions could involve comparison of pathway with nonpathway participants using quantitative information (eg, in-service training exams, board examination scores, etc.). In the meantime, survey responses provide valuable feedback that can be used to modify pathway curricula for participants in this and similar programs, such as increasing the availability of training in outpatient women’s health and geriatric medicine.
The next step in addressing the HIV provider workforce shortage will be to assess the level of postgraduation attrition in other HIV pathway programs. We invite colleagues in other HIV pathways, both IM and family medicine, to investigate whether GME HIV pathway graduates continue to provide care to PLWH following the completion of residency training. We suggest more robust career development programs and better linkage of HIV primary care physicians to HIV-related jobs, particularly in high-prevalence locations. In addition, continuing medical education, including use of existing resources such as through the National HIV Curriculum or Project ECHO, may contribute to retention in the workforce [9–11]. If other studies confirm that graduates are likely to settle in practice where they are trained, then we should locate HIV primary care training tracks in the areas of greatest need, and programs may need to assess applicants for their willingness to practice in high-prevalence areas. If graduates are unable to find appropriate employment or recruit patients without subspecialty certification, key stakeholders may need to help health systems develop models to despecialize HIV primary care or incentivize the hiring of graduates with alternate credentials, such as AAHIVM certification.
CONCLUSIONS
A dedicated HIV pathway during IM residency offers a cost-effective, high-impact curriculum that trains providers to be proficient in HIV care. We found that UW HIV Medicine Pathway graduates enjoyed their experience and felt adequately prepared to provide HIV primary care, and most felt sufficiently trained to provide primary care for HIV-seronegative adults. Despite this, we found attrition in the number of UW HIV Medicine Pathway graduates providing HIV primary care over a 2-year period, mostly due to perceptions that an ID fellowship is necessary to find jobs in HIV primary care.
Limitations to this analysis include a small single-center sample group and potential selection bias. However, this analysis is unique in that it presents survey results examining pathway participant perceptions of a GME pathway at 2 different time points and explores perceived barriers to obtaining work in HIV primary care for internists. The results demonstrate that residency HIV training tracks offer a viable method to train competent HIV primary care providers, though the results also indicate that more robust career development following graduation is needed to ensure retention within this workforce.
Prior presentations: Poster presentations of survey data were shared at the ID Week Conference in San Diego, California, in October 2015 and 2017.
Acknowledgments
The authors would like to acknowledge and thank the University of Washington Internal Medicine Residency Program administration for support in the creation and maintenance of the HIV Medicine Residency pathway.
Financial support. No funding was received for this manuscript.
Potential conflicts of interest. All authors: no reported conflicts of interest. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References





Comments