-
PDF
- Split View
-
Views
-
Cite
Cite
Scott Santibanez, Leah S Fischer, Anusha Krishnadasan, Bethany Sederdahl, Toby Merlin, Gregory J Moran, David A Talan, for the EMERGEncy ID NET Study Group , EMERGEncy ID NET: Review of a 20-Year Multisite Emergency Department Emerging Infections Research Network, Open Forum Infectious Diseases, Volume 4, Issue 4, Fall 2017, ofx218, https://doi.org/10.1093/ofid/ofx218
Close - Share Icon Share
Abstract
As providers of frontline clinical care for patients with acute and potentially life-threatening infections, emergency departments (EDs) have the priorities of saving lives and providing care quickly and efficiently. Although these facilities see a diversity of patients 24 hours per day and can collect prospective data in real time, their ability to conduct timely research on infectious syndromes is not well recognized. EMERGEncy ID NET is a national network that demonstrates that EDs can also collect data and conduct research in real time. This network collaborates with the Centers for Disease Control and Prevention (CDC) and other partners to study and address a wide range of infectious diseases and clinical syndromes. In this paper, we review selected highlights of EMERGEncy ID NET’s history from 1995 to 2017. We focus on the establishment of this multisite research network and the network’s collaborative research on a wide range of ED clinical topics.
OVERVIEW OF EMERGENCY ID NET
History
In the early 1990s, the Institute of Medicine and CDC highlighted the need to address the ongoing threat of emerging infectious diseases [1, 2]. In 1995, the CDC funded and codeveloped with the Olive View–UCLA Department of Emergency Medicine EMERGEncy ID NET—a national network designed to study infectious diseases in patients treated in EDs that are acute, severe, affect at-risk populations, and are less likely to be captured by other public health surveillance.
A combination of different activities led to the selection of EMERGEncy ID NET sites. Potential sites were identified at emergency medicine national conferences where Olive View–UCLA primary investigators approached emergency physicians who worked at university-affiliated hospitals with similar interests in conducting infectious disease research. Other potential study sites had previous experience with multicenter studies that Olive View–UCLA directed. In 1995–1996, the final 11 university-affiliated medical centers were selected as network sites based on research experience, geographic and demographic diversity, hospital laboratory capabilities, and university affiliation with emergency medicine residency training programs [3]. Composition of the network has generally remained stable, with few site changes over time.
Operations
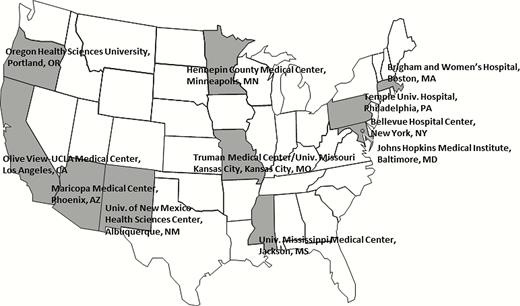
EMERGEncy ID NET currently consists of 11 geographically diverse university-affiliated urban EDs (Figure). The network’s administrative center—Olive View–UCLA Medical Center—oversees the network and manages study data. Collaborators from the CDC participate in the design, direction, and specialized laboratory testing of some studies.
EMERGEncy ID NET focuses on infectious disease problems that are particularly suited to study in EDs. These include infections in which patients are more acutely ill and preferentially come to the ED instead of offices or clinics, wounds and bites that might require surgery (eg, to drain an abscess or close a wound), or special treatments like postexposure prophylaxis. An executive committee of representatives from study sites, Olive View–UCLA Department of Emergency Medicine, and the CDC considers emerging infections likely to present to EDs, treatment practices, and new diagnostic methods. The executive steering committee and Principle Investigators at Olive View–UCLA develop a prioritized list, which is reviewed by CDC. Accepted study proposals are then developed further. Olive View–UCLA and CDC investigators develop data collection forms to obtain data during the course of standard patient care, structured in a multiple choice format to maximize data collection consistency and minimize completion time (ie, <5 minutes). Forms are shared with site investigators to evaluate and improve data query ambiguities, completion time, and practicality of survey. All protocols and forms are approved by institutional review boards [3].
Each site has a designated Principal Investigator who is a full-time emergency medicine faculty member (Appendix 1). Each site investigator establishes specific contacts with the hospital laboratory and local public health departments. Approved protocols and methodology are disseminated to appropriate staff, indicating the syndromes under study and their specific case definitions [3, 4].
Study patients undergo routine clinical evaluation. Depending on study site research resources and structure, either the examining provider, typically an emergency medicine resident, or a trained research coordinator determines whether the patient meets the study case definition. Data obtained during the ED visit are recorded in real time at the bedside on paper data sheets, then later entered on a secure web-based electronic data capture system called REDCap [5]. The REDCap databases are created, managed, and analyzed at Olive View–UCLA Medical Center. Limited follow-up data, such as the results of cultures or serologic studies from study site laboratories or clinical data from hospital admission records, are obtained from electronic medical review up to 4 weeks after ED presentation [3]. Some studies have follow-up telephone calls with study participants. Over its 20-year lifetime, EMERGEncy ID NET has seen widespread adoption of electronic medical records, which have facilitated collection of follow-up clinical and laboratory data. Often, specimens (eg, from wound, stool, blood, cerebrospinal fluid, or urine) are obtained with consent and saved for routine testing at site hospital laboratories and/or further molecular testing at off-site laboratories, for example, to evaluate new diagnostic tests not available at site laboratories.
Research coordinator coverage varies by site, with some sites relying on treating clinicians to remember to identify patients outside covered hours. There is therefore frequent messaging to remind clinicians of the syndromes under study—email blasts, announcements at clinical conferences, and signs posted in clinician work areas. Due to the constraints of emergency care, some patients with the syndromes under study are not enrolled. To account for this, study staff regularly perform audits of ED patient logs to identify missed cases and detect enrollment biases.
CLINICAL EPIDEMIOLOGIC RESEARCH
Since its establishment in 1995, EMERGEncy ID NET has published 22 peer-reviewed articles (Appendix 2). Studies have focused on the epidemiology, diagnosis, and treatment of infectious disease problems commonly encountered by EDs, such as wound, respiratory, gastrointestinal, urinary tract, and central nervous system infections. Findings have been disseminated to broad audiences through widely read scientific journals including the New England Journal of Medicine, Journal of the American Medical Association, Clinical Infectious Diseases, Emerging Infectious Diseases, and Annals of Emergency Medicine. In the next section, we highlight selected investigations by this research network.
Wound Infections
MRSA Emergence as the Most Common Cause of Skin Infections
An EMERGEncy ID NET study showed methicillin-resistant Staphylococcus aureus (MRSA) to be the most common identifiable cause of skin and soft-tissue infections among patients presenting to EDs in 11 US cities. Within 6 months of recognizing a dramatically increased proportion of cases at Olive View–UCLA, EMERGEncy ID NET investigators developed an institutional review board–approved protocol and enrolled participants in 1 month’s time in August 2004. Providers obtained clinical information and cultures from adults with acute, purulent skin and soft-tissue infections. S. aureus isolates underwent antimicrobial susceptibility testing, pulsed-field gel electrophoresis, detection of toxin genes, and typing of the staphylococcal cassette chromosome mec (SCCmec), which carries the mecA gene encoding methicillin resistance. S. aureus was isolated from 320 of 422 (76%) enrolled patients. The overall MRSA prevalence was 59% (range across sites, 15%–74%). Previously, MRSA was only rarely found to be associated with typical skin and soft-tissue infections in the community. Of MRSA isolates, 100% were susceptible to trimethoprim-sulfamethoxazole, 95% to clindamycin, 92% to tetracycline, and 60% to fluoroquinolones. In 100 of 175 (57%) patients with MRSA who received antibiotics, antimicrobial therapy was discordant with susceptibility testing. This study informed ED physicians to include MRSA coverage in their empirical therapy for skin and soft-tissue infections [6].
In August 2008, EMERGEncy ID NET reassessed skin and soft-tissue infections in order to track changes in prevalence, clonal types, antimicrobial resistance patterns, and clinician-prescribing practices. Of note, it was observed that MRSA infections remained common (overall prevalence, 59%; with a 38%–84% range across sites) and that providers had appropriately shifted from predominant use of MRSA-inactive to MRSA-active empiric antimicrobials, demonstrating the translatability of the network’s research to clinical practice [7].
EMERGEncy ID NET’s work in the area of MRSA skin and soft-tissue infections subsequently led to the network’s collaboration with the National Institute of Allergy and Infectious Diseases to conduct clinical trials of off-patent antibiotics commonly used to treat these infections. A follow-up study showed that in ED patients with an uncomplicated abscess treated with surgical drainage, the addition of trimethoprim-sulfamethoxazole was more likely than placebo to effect cure and prevent need for additional antibiotic treatment and/or drainage and new skin site infections [8].
Rabies Postexposure Prophylaxis
In a study of bite wound infections, EMERGEncy ID NET examined from July 1996 to July 1998 the use and appropriateness of rabies postexposure prophylaxis (RPEP) [9]. With data on 2030 animal bites, investigators found that in 1857 (91.5%) of the exposures, appropriate management was provided. RPEP was used for 136 (6.7%) of the 1857 animal bites, and it was considered inappropriate in 54 cases (40% of those in which it was given). RPEP was considered inappropriately withheld from 119 cases (6.3% of those not receiving RPEP). These findings suggest that RPEP was actually underutilized, following guidelines would result in an overall increase in RPEP use, and improved coordination with public health officials and clarification of RPEP guidelines could improve clinical practice and utilization of RPEP.
Urinary Tract Infections
EMERGEncy ID NET conducted 2 studies describing the prevalence of antimicrobial resistance among pathogens causing urinary tract infections, specifically acute pyelonephritis. The first study, conducted in 2000 to 2004, included 689 adults with confirmed pyelonephritis. Rates of fluoroquinolone-resistant Escherichia coli infection were low, ranging from 1% to 3% among patients with uncomplicated pyelonephritis (ie, patients with no identified risk factors) to 5% to 6% among those with complicated infections (ie, patients with a current or preexisting functional or anatomical urinary tract abnormality or a current immunocompromising condition, or who were pregnant or male). No infections due to extended-spectrum β-lactamase-producing (ESBL) strains, which are resistant to commonly available broad spectrum penicillins and cephalosporins, as well as other antibiotic classes, were found [10]. However, a second recently completed investigation, conducted during 2012 to 2014, found that fluoroquinolone resistance rates in certain locations and among groups with antibiotic resistance risk factors had increased to levels requiring an additional antibiotic or switching to an agent from a different antibiotic class for empirical treatment. Fluoroquinolone resistance was 6.3% (range by site, 0.0%–23.1%) among patients with uncomplicated pyelonephritis and 19.9% (range, 0.0%–50.0%) among patients with complicated pyelonephritis. Further, the recent study found that ESBL-producing E. coli have now emerged in some US communities, including among individuals lacking health care or antibiotic exposure. Of note, about one-half of all patients in this study were treated with oral antibiotics as outpatients. At present, no oral antimicrobials are available with consistent in vitro activity to empirically treat acute pyelonephritis due to ESBL-producing E. coli, highlighting the importance of emerging antimicrobial resistance and the need for research into new treatments for resistant infections [11]. These findings indicate that ED providers should make treatment decisions on the basis of their local antibiogram, including consideration of empirical treatment with a carbapenem or another agent found to be consistently active, for persons at high risk for both antimicrobial drug resistance and severe sepsis. Future plans include investigation of urosepsis to further understand the problem of emerging bacterial antibiotic resistance, including ESBLs and carbapenem-resistant Enterobacteriaceae (CRE).
Respiratory Infections
MRSA Pneumonia
Emergence of MRSA skin infections in the community prompted investigation of how prominent a role this pathogen might play in pneumonia. A study published in 2012 showed that although MRSA was a common cause of skin infections, it uncommonly caused community-acquired pneumonia (CAP). Of 627 adults hospitalized with CAP who were enrolled during the winter/spring of 2006 and 2007, 595 (95%) had respiratory and/or blood cultures performed. MRSA was identified in 14 (2.4%; range, 0%–5%) patients and 5% of those admitted to the intensive care unit. Features significantly associated with isolation of MRSA included patient history of MRSA infection or colonization; nursing home admission in the previous year; close contact in the previous month with someone with a skin infection; multiple infiltrates or cavities on chest radiograph; and comatose state, intubation, receipt of vasopressors, or death in the emergency department [12]. While uncommon, MRSA was second only to Streptococcus pneumoniae as an identified cause of pneumonia and was notably more common among those with specific risk factors and severe clinical presentations, supporting guidelines for empirical coverage for severe CAP [13].
Tuberculosis Disease Screening
Tuberculosis (TB) transmission has been documented in settings where health care workers and patients come in contact with persons with active pulmonary TB. During the period in which newer TB diagnostics tests were available but not yet widely in practice, and prompted by concerns about the limited number of isolation rooms and a desire to improve the predictive value—positive and negative—of decisions to isolate, EMERGEncy ID NET investigators used a prospective case series to create and assess performance of a decision instrument. This instrument used patient data and chest radiographs to sharpen the indications and improve efforts to predict which pneumonia patients do not need admission to a TB isolation bed. Of 5079 pneumonia patients admitted through the ED, 224 (4.4%) had pulmonary TB according to sputum cultures or tissue staining. The instrument consisted of factors that predicted which patients did not have pulmonary TB using clinical data. Specifically, TB was unlikely if none of the following criteria were present: TB history or previous positive tuberculin skin test result; immigrant status; homelessness; recent incarceration; recent weight loss; and apical infiltrate or cavitary lesion on chest radiograph. The instrument had a sensitivity of 96.4% and negative predictive value of 99.7% [14].
Gastrointestinal Infections
E. coli O157:H7 and Shiga Toxin–Producing E. coli
Nationally, 5% to 10% of patients with Shiga toxin–producing E. coli (STEC) diarrhea develop hemolytic-uremic syndrome (HUS) and potential long-term complications, which has led to current recommendations from the Infectious Diseases Society of America, CDC, and others to culture bloody stools. Following outbreaks of E. coli O157:H7 and STEC from July 1996 through September 1998, with some cases leading to HUS and death, EMERGEncy ID NET investigators evaluated the prevalence of STEC, Campylobacter, Salmonella, Shigella, and other species among children and adults presenting to all site EDs with bloody diarrhea. Stool cultures were obtained in a prospective study of 873 patients with a history of bloody stools or bloody stools evident on examination. Among cases in which an enteric pathogen was identified, STEC or possible STEC (a Shiga toxin–positive fecal specimen and a stool culture that did not yield a pathogen) was found in 14 (8.3%). Compared with patients infected with other enteric pathogens, those with STEC were less likely to have fever and more likely to have visible blood in stools. STEC infection represented 2.6% of all acute bloody diarrhea cases in this study. However, serious STEC-associated complications such as HUS, and the presence of other enteropathogens such as Campylobacter, Salmonella, Shigella, Vibrio, Yersinia, Plesiomonas, and STEC species, support the practice of obtaining stool cultures in patients with bloody diarrhea [15, 16].
Clostridium difficile
While Clostridium difficile infection (CDI) is recognized in people exposed to antibiotic treatment and health care settings, its prevalence has not been well studied in lower-risk populations including peripartum women, younger persons, and those without antibiotic use. In a study conducted from November 2010 to April 2013, EMERGEncy ID NET investigators evaluated ED patients age ≥2 years with diarrhea (≥3 episodes/24 hours) and no vomiting to determine the prevalence of CDI, including among patients who lack traditional CDI risk factors. Study investigators confirmed C. difficile infection by a C. difficile–positive stool culture result and positive toxin assay. Among 422 participants, the prevalence of CDI was 10.2% and varied by site from 1.8% to 29.4%. The proportion of all participants without any CDI risk factors was 59.2%, and among these participants, the prevalence of CDI was 6.9%. Patients with CDI had higher rates of hospitalization and intensive care unit admission than those without CDI. With the recent availability of rapid and accurate polymerase chain reaction (PCR) stool testing, this study supports consideration of CDI among ED patients presenting with diarrhea, particularly among those with greater illness severity, and including those without traditional risk factors [17].
Central Nervous System Infections
Patients with possible meningitis often present to EDs. Lumbar puncture is a standard diagnostic evaluation. Many patients have abnormal cerebrospinal fluid but no specific infectious agent is identified. And there are limitations to PCR-based techniques for novel pathogens because in the absence of known genetic sequences, it is difficult to develop appropriate primers for sequence amplification. To better understand the epidemiology of meningoencephalitis presenting to EDs, a current study involves approximately 1000 pediatric and adult patients for whom a lumbar puncture was performed [18].
In this study population, EMERGEncy ID NET investigators evaluated the role of advanced molecular testing (AMT; eg, metagenomics) to identify pathogens in patients suspected of meningoencephalitis and other patients with presentations resulting in lumbar puncture. Preliminary findings suggest that, despite the sophistication of AMT, it cannot detect pathogens it does not target or that are present in small numbers or that have been eliminated from the CSF by the immune response. Despite the theoretical potential for microarray and metagenomics sequencing to detect thousands of different agents, the agents probably must be present at high levels for detection [19].
DISCUSSION
In its first 2 decades, the establishment of EMERGEncy ID NET as a multisite network has led to studies that address a wide range of infectious diseases and clinical syndromes. A key part of EMERGEncy ID NET’s success has been its ability to rapidly anticipate, detect, and discover newly emerging infections. For example, this network was instrumental in identifying the emergence of community-acquired MRSA skin and soft-tissue infections. In the initial MRSA study, the network was able to develop a protocol to test hypotheses within less than 6 months. The presence of 11 high-volume ED sites enabled investigators to complete enrollment in only 1 month. While MRSA in the community was a known cause of purulent skin and soft-tissue infections in the United States, EMERGEncy ID NET was the first to observe that MRSA had become broadly prevalent, which could be very valuable in studying future emerging infectious threats.
Another value of an ED-based network is its ability to identify areas for improvement and inform ED physician practice. For example, the early MRSA study informed ED physicians that they should include MRSA coverage in empiric therapy for purulent skin and soft-tissue infections. Another study suggested that RPEP was underutilized and that improved coordination with public health officials and clarification of RPEP guidelines were needed. Other investigations focused on encouraging antibiotic stewardship and examining inappropriate antibiotic use for upper respiratory tract infections, diarrhea, and lacerations [20–22].
Some efforts have aimed at improving ED physician practice with regard to infection control. The TB study was able to generate a clinical tool to help with isolation decisions. Many of the newer TB diagnostic tests were not yet widely in practice at the time the TB decision instrument was envisioned. The goal at that time was to try to sharpen clinical predictors of TB to better inform isolation decisions. Today, many EDs and hospitals are moving toward the use of newer rapid diagnostic tests for TB such as the Food and Drug Administration–approved Cepheid Xpert MTB/RIF (Xpert) Nucleic Acid Amplification (NAA) test when making decisions to discontinue airborne infection isolation [23–25].
The establishment of EMERGEncy ID NET as a pioneer in ED research has led to several spin-off studies that are not officially part of the network. As noted, the National Institutes of Health–funded study involving five EMERGEncy ID NET sites demonstrated that, in US settings where MRSA was prevalent, trimethoprim–sulfamethoxazole treatment resulted in a higher cure rate among patients with a drained cutaneous abscess than placebo, lower rates of subsequent surgical drainage, skin infections at new sites, and infections in household members [26]. These findings have important implications for clinical practice.
A final important question is how EMERGEncy ID NET can continue to adapt and evolve going forward. Key elements of today’s health care environment are the importance of antimicrobial resistance and stewardship [27], the potential of new molecular tools, and better electronic exchange of information. The network is well positioned to address these new issues. For example, the CSF study investigated the use of modern molecular tools to address the diagnosis of central nervous system syndromes. EDs could also be useful clinical settings to evaluate rapid molecular diagnostic tests that may allow more accurate and timely diagnosis, more directed treatment, and improved stewardship, and could be a useful venue to test new sepsis definitions and case-finding methods as they apply to the ED.
Although the clinical landscape continues to evolve over time, what is not changing is that patients with potentially infectious diseases will continue to be seen in EDs. The first 2 decades of EMERGEncy ID NET demonstrated that EDs are a critically important setting to the detection of emerging infections and the translation of clinical epidemiological research to improve practices and clinical outcomes.
Acknowledgements
The authors would like to thank the following individuals for their participation in EMERGEncy ID NET.
Site and co-investigators: William Mower, MD, PhD, Matthew Sullivan, MD, Fredrick M. Abrahamian, DO, Sam Ong, MD, Eric Gross, MD, MPH, Bisan Salhi, MD, Katherine Heilpern, MD, Jeremy Hess, MD, David Karras, MD, Michelle Biros, MD, Lala Dunbar, MD, Sukhjit Takhar, MD, Charles Pollack, MD, Jeffrey Runge, MD, Paul Cheney, MD, Stephen Rothrock, MD, John O’Brian, MD, Diane Citron, BS, Ellie Goldstein, MD, Sydney Finegold, PhD.
Project Directors: Janet Nakase, MPH, Michael Newdow, MD, MPH.
Study coordinators: Guy Merchant, MFA, Kavitha Pathmarajah, MPH, Eva Gonzalez, BS, Mary Mulrow, RN, MA, MN, Silas Bussman, MBA, MPH, Vernon Kalugdnan, RN, Stephen Peterson, BS, Seth Pitts, BS, Kamil Narayan, MPH, Ada Rubin, MPA, Laurie Kemble, BHS, CCRC, Danielle Beckham, RN, MSN, BSN, Niccole Neal, RN, BSN, CRC, Annick Yagapen, MPH, Carol Von Hofen, RN, Kathleen Hatala, RN, Shelley Fuentes, Debbi Sibley, BS, Ashley Colucci, Jackeline Hernandez, MD, Hope Cruse, MS, Sarah Usher, Audrey Hendrickson, MPH, CCRP, Kimberly Dehnkamp, RN, Britney Zeglin, BS, Guruprasad Jambaulikar, MBBS, MPH.
CDC: Rachel Gorwitz, MD, PhD, Brandi Limbago, PhD, Matthew Kuehnert, MD, William Jarvis, MD, Larry Slutsker, MD, MPH, Melissa Arvay, PhD, Laura Conn, MPH.
The authors would also like to thank Neela Goswami, MD, Clifford McDonald, MD, Satish Pillai, MD, MPH, and Robert Pinner, MD, for helpful reviews of this article.
Financial support. D. Talan, G. Moran, and A. Krishnadasan have received institutional grant funding from the CDC (5U01CK000480). All other authors have no reported disclosures.
Disclosure. The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of CDC.
Potential conflicts of interest. All authors: no reported conflicts of interest. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
APPENDIX 1. EMERGENCY ID NET STUDY GROUP SITE PRINCIPAL INVESTIGATORS AND ANNUAL EMERGENCY DEPARTMENT CENSUS
| Site . | Site Principal Investigator, 2017 . | Annual Emergency Department Census . |
|---|---|---|
| Bellevue Hospital Center, New York, NY | William Chiang, MD | 102000 |
| Brigham and Women’s Hospital, Boston, MA | Daniel Pallin, MD, MPH | 60000 |
| Hennepin County Medical Center, Minneapolis, MN | Johanna Moore, MD | 91000 |
| Johns Hopkins Medical Institute, Baltimore, MD | Richard Rothman, MD, PhD | 68000 |
| Maricopa Medical Center, Phoenix, AZ | Frank LoVecchio, DO, MPH | 73000 |
| Olive View–UCLA Medical Center, Los Angeles, CA | Gregory Moran, MD | 64000 |
| Oregon Health Sciences Medical Center, Portland, OR | Jonathan Jui, MD, MPH | 48700 |
| Temple University Hospital, Philadephia, PA | Manish Garg, MD | 90600 |
| University of Kansas City/Truman Medical Center, Kansas City, MO | Mark Steele, MD | 62000 |
| University of Mississippi Medical Center, Jackson, MS | Alan Jones, MD | 115000 |
| University of New Mexico Health Sciences Medical Center, Albuquerque, NM | Jon Femling, MD, PhD | 99000 |
| Site . | Site Principal Investigator, 2017 . | Annual Emergency Department Census . |
|---|---|---|
| Bellevue Hospital Center, New York, NY | William Chiang, MD | 102000 |
| Brigham and Women’s Hospital, Boston, MA | Daniel Pallin, MD, MPH | 60000 |
| Hennepin County Medical Center, Minneapolis, MN | Johanna Moore, MD | 91000 |
| Johns Hopkins Medical Institute, Baltimore, MD | Richard Rothman, MD, PhD | 68000 |
| Maricopa Medical Center, Phoenix, AZ | Frank LoVecchio, DO, MPH | 73000 |
| Olive View–UCLA Medical Center, Los Angeles, CA | Gregory Moran, MD | 64000 |
| Oregon Health Sciences Medical Center, Portland, OR | Jonathan Jui, MD, MPH | 48700 |
| Temple University Hospital, Philadephia, PA | Manish Garg, MD | 90600 |
| University of Kansas City/Truman Medical Center, Kansas City, MO | Mark Steele, MD | 62000 |
| University of Mississippi Medical Center, Jackson, MS | Alan Jones, MD | 115000 |
| University of New Mexico Health Sciences Medical Center, Albuquerque, NM | Jon Femling, MD, PhD | 99000 |
| Site . | Site Principal Investigator, 2017 . | Annual Emergency Department Census . |
|---|---|---|
| Bellevue Hospital Center, New York, NY | William Chiang, MD | 102000 |
| Brigham and Women’s Hospital, Boston, MA | Daniel Pallin, MD, MPH | 60000 |
| Hennepin County Medical Center, Minneapolis, MN | Johanna Moore, MD | 91000 |
| Johns Hopkins Medical Institute, Baltimore, MD | Richard Rothman, MD, PhD | 68000 |
| Maricopa Medical Center, Phoenix, AZ | Frank LoVecchio, DO, MPH | 73000 |
| Olive View–UCLA Medical Center, Los Angeles, CA | Gregory Moran, MD | 64000 |
| Oregon Health Sciences Medical Center, Portland, OR | Jonathan Jui, MD, MPH | 48700 |
| Temple University Hospital, Philadephia, PA | Manish Garg, MD | 90600 |
| University of Kansas City/Truman Medical Center, Kansas City, MO | Mark Steele, MD | 62000 |
| University of Mississippi Medical Center, Jackson, MS | Alan Jones, MD | 115000 |
| University of New Mexico Health Sciences Medical Center, Albuquerque, NM | Jon Femling, MD, PhD | 99000 |
| Site . | Site Principal Investigator, 2017 . | Annual Emergency Department Census . |
|---|---|---|
| Bellevue Hospital Center, New York, NY | William Chiang, MD | 102000 |
| Brigham and Women’s Hospital, Boston, MA | Daniel Pallin, MD, MPH | 60000 |
| Hennepin County Medical Center, Minneapolis, MN | Johanna Moore, MD | 91000 |
| Johns Hopkins Medical Institute, Baltimore, MD | Richard Rothman, MD, PhD | 68000 |
| Maricopa Medical Center, Phoenix, AZ | Frank LoVecchio, DO, MPH | 73000 |
| Olive View–UCLA Medical Center, Los Angeles, CA | Gregory Moran, MD | 64000 |
| Oregon Health Sciences Medical Center, Portland, OR | Jonathan Jui, MD, MPH | 48700 |
| Temple University Hospital, Philadephia, PA | Manish Garg, MD | 90600 |
| University of Kansas City/Truman Medical Center, Kansas City, MO | Mark Steele, MD | 62000 |
| University of Mississippi Medical Center, Jackson, MS | Alan Jones, MD | 115000 |
| University of New Mexico Health Sciences Medical Center, Albuquerque, NM | Jon Femling, MD, PhD | 99000 |
APPENDIX 2. EMERGENCY ID NET PUBLICATIONS AND COMMENTARIES
| 1. Abrahamian FA, Talan DA, Krishnadasan A, et al; EMERGEncy ID NET Study Group. Clostridium difficile infection among US emergency department patients with diarrhea and no vomiting. Ann Emerg Med 2017; 70:19–27. 2. Talan, DA, Takhar SS, Krishnadasan A, Abrahamian FM, Mower WR, Moran GJ; for the EMERGEncy ID NET Study Group. Fluoroquinolone-resistant and extended-spectrum β-lactamase–producing Escherichia coli infections in patients with pyelonephritis, United States. Emerg Inf Dis 2016; 22:1594–1603. 3. Albrecht V, Limbago B, Moran G, Krishnadasan A, Gorwitz R, McDougal L, Talan DA; for the EMERGEncy ID NET Study Group. Staphylococcus aureus colonization and strain type at various body sites among patients with a closed abscess and uninfected controls at U.S. emergency departments. J Clin Microbiol 2015; 53:1371–15. 4. Crisp JG, Takhar SS, Moran GJ, et al; for the EMERGEncy ID NET Study Group. Inability of polymerase chain reaction, pyrosequencing, and culture of infected and uninfected site skin biopsy specimens to identify the cause of cellulitis. Clin Infect Dis 2015; 61:1679–87. 5. Talan, DA, Salhi B, Moran GJ, et al. Factors associated with the decision to hospitalize emergency department patients with a skin and soft tissue infection. West J Emerg Med 2014; 16:89–97. 6. Moran GJ, Krishnadasan A, Gorwitz RJ, et al; for the EMERGEncy ID NET Study Group. Prevalence of methicillin-resistant staphylococcus aureus as an etiology of community-acquired pneumonia. Clin Infect Dis 2012; 54:1126–33. Commentary: Mandell LA, Wunderink R. Methicillin-resistant Staphylococcus aureus and community-acquired pneumonia: an evolving relationship. Clin Infect Dis 2012; 54:1134–6. 7. Ong S, Moran GJ, Krishnadasan A, Talan DA; for the EMERGEncy ID NET Study Group. Antibiotic prescribing practices of emergency physicians and patient expectations for uncomplicated lacerations. West J Emerg Med 2011; 12:375–380. 8. Talan DA, Krishnadasan A, Gorwitz RJ, et al; for the EMERGEncy ID NET Study Group. Comparison of staphylococcus aureus from skin and soft-tissue infections in US emergency department patients, 2004 and 2008. Clin Infect Dis 2011; 53:144–9. 9. Talan DA, Krishnadasan A, Abrahamian FM, Stamm WE, Moran GJ; for the EMERGEncy ID NET Study Group. Prevalence and risk factor analysis of trimethoprim-sulfamethoxazole- and fluoroquinolone-resistant Escherichia coli infection among emergency department patients with pyelonephritis. Clin Infect Dis 2008; 47:1150–8. Commentary: Lautenbach E. Finding the path of least antimicrobial resistance in pyelonephritis. Clin Infect Dis 2008; 47:1159–61. 10. Moran GJ, Barrett TW, Mower WR, et al; for the EMERGEncy ID NET Study Group. Decision instrument for the isolation of pneumonia patients with suspected pulmonary tuberculosis admitted through US emergency departments. Ann Emerg Med 2009; 53:625–32. 11. Ong S, Nakase J, Moran GJ, Karras DJ, Kuehnert MJ, Talan DA; for the EMERGEncy ID NET Study Group. Antibiotic use for emergency department patients with upper respiratory infections: prescribing practices, patient expectations, and patient satisfaction. Ann Emerg Med 2007; 50:213–20. 12. Steele MT, Ma OJ, Nakase J, et al; for the EMERGEncy ID NET Study Group. Epidemiology of animal exposures presenting to emergency departments. Acad Emerg Med 2007; 14:398–403. 13. Moran GJ, Krishnadasan A, Gorwitz RJ, et al; for the EMERGEncy ID NET Study Group. Methicillin-resistant S. aureus infections among patients in the emergency department. N Engl J Med 2006; 355:666–74. Commentary: Grayson ML. The treatment triangle for staphylococcal infections. N Engl J Med 2006; 355:724–27. 14. Karras DJ, Ong S, Moran GJ, et al; for the EMERGEncy ID NET Study Group. Antibiotic use for emergency department patients with acute diarrhea: prescribing practices, patient expectations, and patient satisfaction. Ann Emerg Med 2003; 42:835–42. 15. Talan DA, Abrahamian FM, Moran GJ, Citron DM, Tan JO, Goldstein EJC; for the EMERGEncy ID NET Study Group. Clinical presentation and bacteriologic analysis of infected human bites in patients presenting to emergency departments. Clin Infect Dis 2003; 37:1481–9. 16. Ong S, Talan DA, Moran GJ, et al; for the EMERGEncy ID NET Study Group. Neurocysticercosis in radiographically imaged seizure patients in U.S. emergency departments. Emerg Infect Dis 2002; 8:608–13. 17. Mower WR, Biros MH, Talan DA, Moran GJ, Ong S; EMERGEncy ID NET. Selective tomographic imaging of patients with new-onset seizure disorders. Acad Emerg Med 2002; 9:43–7. 18. Talan DA, Moran GJ, Newdow M, et al; for the EMERGEncy ID NET Study Group. Etiology of bloody diarrhea among patients presenting to United States emergency departments: prevalence of Escherichia coli 0157:H7 and other enteropathogens. Clin Infect Dis 2001; 32:573–80. 19. Moran GJ, Talan DA, Mower W, et al; for the EMERGEncy ID NET Study Group. Appropriateness of rabies postexposure prophylaxis treatment for animal exposures. JAMA 2000; 284:1001–7. 20. Talan DA, Moran GJ, Mower WR, et al. EMERGEncy ID NET: an emergency department-based emerging infections sentinel network. Clin Infect Dis 1999; 28:401–2. 21. Talan DA, Moran GJ, Mower WR, et al; for the EMERGEncy ID NET Study Group. EMERGEncy ID NET: an emergency department-based emerging infections sentinel network. Ann Emerg Med 1998; 32:703–11. 22. Moran GJ, Kyriacou DN, Newdow MA, Talan DA. Emergency department sentinel surveillance for emerging infectious diseases. Ann Emerg Med 1995; 26:351–4. Commentary: Garrison HG, Runyan CW, Tintinalli JE, et al. Emergency department surveillance: an examination of issues and a proposal for a national strategy. Ann Emerg Med 1994; 24:849–56. |
| 1. Abrahamian FA, Talan DA, Krishnadasan A, et al; EMERGEncy ID NET Study Group. Clostridium difficile infection among US emergency department patients with diarrhea and no vomiting. Ann Emerg Med 2017; 70:19–27. 2. Talan, DA, Takhar SS, Krishnadasan A, Abrahamian FM, Mower WR, Moran GJ; for the EMERGEncy ID NET Study Group. Fluoroquinolone-resistant and extended-spectrum β-lactamase–producing Escherichia coli infections in patients with pyelonephritis, United States. Emerg Inf Dis 2016; 22:1594–1603. 3. Albrecht V, Limbago B, Moran G, Krishnadasan A, Gorwitz R, McDougal L, Talan DA; for the EMERGEncy ID NET Study Group. Staphylococcus aureus colonization and strain type at various body sites among patients with a closed abscess and uninfected controls at U.S. emergency departments. J Clin Microbiol 2015; 53:1371–15. 4. Crisp JG, Takhar SS, Moran GJ, et al; for the EMERGEncy ID NET Study Group. Inability of polymerase chain reaction, pyrosequencing, and culture of infected and uninfected site skin biopsy specimens to identify the cause of cellulitis. Clin Infect Dis 2015; 61:1679–87. 5. Talan, DA, Salhi B, Moran GJ, et al. Factors associated with the decision to hospitalize emergency department patients with a skin and soft tissue infection. West J Emerg Med 2014; 16:89–97. 6. Moran GJ, Krishnadasan A, Gorwitz RJ, et al; for the EMERGEncy ID NET Study Group. Prevalence of methicillin-resistant staphylococcus aureus as an etiology of community-acquired pneumonia. Clin Infect Dis 2012; 54:1126–33. Commentary: Mandell LA, Wunderink R. Methicillin-resistant Staphylococcus aureus and community-acquired pneumonia: an evolving relationship. Clin Infect Dis 2012; 54:1134–6. 7. Ong S, Moran GJ, Krishnadasan A, Talan DA; for the EMERGEncy ID NET Study Group. Antibiotic prescribing practices of emergency physicians and patient expectations for uncomplicated lacerations. West J Emerg Med 2011; 12:375–380. 8. Talan DA, Krishnadasan A, Gorwitz RJ, et al; for the EMERGEncy ID NET Study Group. Comparison of staphylococcus aureus from skin and soft-tissue infections in US emergency department patients, 2004 and 2008. Clin Infect Dis 2011; 53:144–9. 9. Talan DA, Krishnadasan A, Abrahamian FM, Stamm WE, Moran GJ; for the EMERGEncy ID NET Study Group. Prevalence and risk factor analysis of trimethoprim-sulfamethoxazole- and fluoroquinolone-resistant Escherichia coli infection among emergency department patients with pyelonephritis. Clin Infect Dis 2008; 47:1150–8. Commentary: Lautenbach E. Finding the path of least antimicrobial resistance in pyelonephritis. Clin Infect Dis 2008; 47:1159–61. 10. Moran GJ, Barrett TW, Mower WR, et al; for the EMERGEncy ID NET Study Group. Decision instrument for the isolation of pneumonia patients with suspected pulmonary tuberculosis admitted through US emergency departments. Ann Emerg Med 2009; 53:625–32. 11. Ong S, Nakase J, Moran GJ, Karras DJ, Kuehnert MJ, Talan DA; for the EMERGEncy ID NET Study Group. Antibiotic use for emergency department patients with upper respiratory infections: prescribing practices, patient expectations, and patient satisfaction. Ann Emerg Med 2007; 50:213–20. 12. Steele MT, Ma OJ, Nakase J, et al; for the EMERGEncy ID NET Study Group. Epidemiology of animal exposures presenting to emergency departments. Acad Emerg Med 2007; 14:398–403. 13. Moran GJ, Krishnadasan A, Gorwitz RJ, et al; for the EMERGEncy ID NET Study Group. Methicillin-resistant S. aureus infections among patients in the emergency department. N Engl J Med 2006; 355:666–74. Commentary: Grayson ML. The treatment triangle for staphylococcal infections. N Engl J Med 2006; 355:724–27. 14. Karras DJ, Ong S, Moran GJ, et al; for the EMERGEncy ID NET Study Group. Antibiotic use for emergency department patients with acute diarrhea: prescribing practices, patient expectations, and patient satisfaction. Ann Emerg Med 2003; 42:835–42. 15. Talan DA, Abrahamian FM, Moran GJ, Citron DM, Tan JO, Goldstein EJC; for the EMERGEncy ID NET Study Group. Clinical presentation and bacteriologic analysis of infected human bites in patients presenting to emergency departments. Clin Infect Dis 2003; 37:1481–9. 16. Ong S, Talan DA, Moran GJ, et al; for the EMERGEncy ID NET Study Group. Neurocysticercosis in radiographically imaged seizure patients in U.S. emergency departments. Emerg Infect Dis 2002; 8:608–13. 17. Mower WR, Biros MH, Talan DA, Moran GJ, Ong S; EMERGEncy ID NET. Selective tomographic imaging of patients with new-onset seizure disorders. Acad Emerg Med 2002; 9:43–7. 18. Talan DA, Moran GJ, Newdow M, et al; for the EMERGEncy ID NET Study Group. Etiology of bloody diarrhea among patients presenting to United States emergency departments: prevalence of Escherichia coli 0157:H7 and other enteropathogens. Clin Infect Dis 2001; 32:573–80. 19. Moran GJ, Talan DA, Mower W, et al; for the EMERGEncy ID NET Study Group. Appropriateness of rabies postexposure prophylaxis treatment for animal exposures. JAMA 2000; 284:1001–7. 20. Talan DA, Moran GJ, Mower WR, et al. EMERGEncy ID NET: an emergency department-based emerging infections sentinel network. Clin Infect Dis 1999; 28:401–2. 21. Talan DA, Moran GJ, Mower WR, et al; for the EMERGEncy ID NET Study Group. EMERGEncy ID NET: an emergency department-based emerging infections sentinel network. Ann Emerg Med 1998; 32:703–11. 22. Moran GJ, Kyriacou DN, Newdow MA, Talan DA. Emergency department sentinel surveillance for emerging infectious diseases. Ann Emerg Med 1995; 26:351–4. Commentary: Garrison HG, Runyan CW, Tintinalli JE, et al. Emergency department surveillance: an examination of issues and a proposal for a national strategy. Ann Emerg Med 1994; 24:849–56. |
| 1. Abrahamian FA, Talan DA, Krishnadasan A, et al; EMERGEncy ID NET Study Group. Clostridium difficile infection among US emergency department patients with diarrhea and no vomiting. Ann Emerg Med 2017; 70:19–27. 2. Talan, DA, Takhar SS, Krishnadasan A, Abrahamian FM, Mower WR, Moran GJ; for the EMERGEncy ID NET Study Group. Fluoroquinolone-resistant and extended-spectrum β-lactamase–producing Escherichia coli infections in patients with pyelonephritis, United States. Emerg Inf Dis 2016; 22:1594–1603. 3. Albrecht V, Limbago B, Moran G, Krishnadasan A, Gorwitz R, McDougal L, Talan DA; for the EMERGEncy ID NET Study Group. Staphylococcus aureus colonization and strain type at various body sites among patients with a closed abscess and uninfected controls at U.S. emergency departments. J Clin Microbiol 2015; 53:1371–15. 4. Crisp JG, Takhar SS, Moran GJ, et al; for the EMERGEncy ID NET Study Group. Inability of polymerase chain reaction, pyrosequencing, and culture of infected and uninfected site skin biopsy specimens to identify the cause of cellulitis. Clin Infect Dis 2015; 61:1679–87. 5. Talan, DA, Salhi B, Moran GJ, et al. Factors associated with the decision to hospitalize emergency department patients with a skin and soft tissue infection. West J Emerg Med 2014; 16:89–97. 6. Moran GJ, Krishnadasan A, Gorwitz RJ, et al; for the EMERGEncy ID NET Study Group. Prevalence of methicillin-resistant staphylococcus aureus as an etiology of community-acquired pneumonia. Clin Infect Dis 2012; 54:1126–33. Commentary: Mandell LA, Wunderink R. Methicillin-resistant Staphylococcus aureus and community-acquired pneumonia: an evolving relationship. Clin Infect Dis 2012; 54:1134–6. 7. Ong S, Moran GJ, Krishnadasan A, Talan DA; for the EMERGEncy ID NET Study Group. Antibiotic prescribing practices of emergency physicians and patient expectations for uncomplicated lacerations. West J Emerg Med 2011; 12:375–380. 8. Talan DA, Krishnadasan A, Gorwitz RJ, et al; for the EMERGEncy ID NET Study Group. Comparison of staphylococcus aureus from skin and soft-tissue infections in US emergency department patients, 2004 and 2008. Clin Infect Dis 2011; 53:144–9. 9. Talan DA, Krishnadasan A, Abrahamian FM, Stamm WE, Moran GJ; for the EMERGEncy ID NET Study Group. Prevalence and risk factor analysis of trimethoprim-sulfamethoxazole- and fluoroquinolone-resistant Escherichia coli infection among emergency department patients with pyelonephritis. Clin Infect Dis 2008; 47:1150–8. Commentary: Lautenbach E. Finding the path of least antimicrobial resistance in pyelonephritis. Clin Infect Dis 2008; 47:1159–61. 10. Moran GJ, Barrett TW, Mower WR, et al; for the EMERGEncy ID NET Study Group. Decision instrument for the isolation of pneumonia patients with suspected pulmonary tuberculosis admitted through US emergency departments. Ann Emerg Med 2009; 53:625–32. 11. Ong S, Nakase J, Moran GJ, Karras DJ, Kuehnert MJ, Talan DA; for the EMERGEncy ID NET Study Group. Antibiotic use for emergency department patients with upper respiratory infections: prescribing practices, patient expectations, and patient satisfaction. Ann Emerg Med 2007; 50:213–20. 12. Steele MT, Ma OJ, Nakase J, et al; for the EMERGEncy ID NET Study Group. Epidemiology of animal exposures presenting to emergency departments. Acad Emerg Med 2007; 14:398–403. 13. Moran GJ, Krishnadasan A, Gorwitz RJ, et al; for the EMERGEncy ID NET Study Group. Methicillin-resistant S. aureus infections among patients in the emergency department. N Engl J Med 2006; 355:666–74. Commentary: Grayson ML. The treatment triangle for staphylococcal infections. N Engl J Med 2006; 355:724–27. 14. Karras DJ, Ong S, Moran GJ, et al; for the EMERGEncy ID NET Study Group. Antibiotic use for emergency department patients with acute diarrhea: prescribing practices, patient expectations, and patient satisfaction. Ann Emerg Med 2003; 42:835–42. 15. Talan DA, Abrahamian FM, Moran GJ, Citron DM, Tan JO, Goldstein EJC; for the EMERGEncy ID NET Study Group. Clinical presentation and bacteriologic analysis of infected human bites in patients presenting to emergency departments. Clin Infect Dis 2003; 37:1481–9. 16. Ong S, Talan DA, Moran GJ, et al; for the EMERGEncy ID NET Study Group. Neurocysticercosis in radiographically imaged seizure patients in U.S. emergency departments. Emerg Infect Dis 2002; 8:608–13. 17. Mower WR, Biros MH, Talan DA, Moran GJ, Ong S; EMERGEncy ID NET. Selective tomographic imaging of patients with new-onset seizure disorders. Acad Emerg Med 2002; 9:43–7. 18. Talan DA, Moran GJ, Newdow M, et al; for the EMERGEncy ID NET Study Group. Etiology of bloody diarrhea among patients presenting to United States emergency departments: prevalence of Escherichia coli 0157:H7 and other enteropathogens. Clin Infect Dis 2001; 32:573–80. 19. Moran GJ, Talan DA, Mower W, et al; for the EMERGEncy ID NET Study Group. Appropriateness of rabies postexposure prophylaxis treatment for animal exposures. JAMA 2000; 284:1001–7. 20. Talan DA, Moran GJ, Mower WR, et al. EMERGEncy ID NET: an emergency department-based emerging infections sentinel network. Clin Infect Dis 1999; 28:401–2. 21. Talan DA, Moran GJ, Mower WR, et al; for the EMERGEncy ID NET Study Group. EMERGEncy ID NET: an emergency department-based emerging infections sentinel network. Ann Emerg Med 1998; 32:703–11. 22. Moran GJ, Kyriacou DN, Newdow MA, Talan DA. Emergency department sentinel surveillance for emerging infectious diseases. Ann Emerg Med 1995; 26:351–4. Commentary: Garrison HG, Runyan CW, Tintinalli JE, et al. Emergency department surveillance: an examination of issues and a proposal for a national strategy. Ann Emerg Med 1994; 24:849–56. |
| 1. Abrahamian FA, Talan DA, Krishnadasan A, et al; EMERGEncy ID NET Study Group. Clostridium difficile infection among US emergency department patients with diarrhea and no vomiting. Ann Emerg Med 2017; 70:19–27. 2. Talan, DA, Takhar SS, Krishnadasan A, Abrahamian FM, Mower WR, Moran GJ; for the EMERGEncy ID NET Study Group. Fluoroquinolone-resistant and extended-spectrum β-lactamase–producing Escherichia coli infections in patients with pyelonephritis, United States. Emerg Inf Dis 2016; 22:1594–1603. 3. Albrecht V, Limbago B, Moran G, Krishnadasan A, Gorwitz R, McDougal L, Talan DA; for the EMERGEncy ID NET Study Group. Staphylococcus aureus colonization and strain type at various body sites among patients with a closed abscess and uninfected controls at U.S. emergency departments. J Clin Microbiol 2015; 53:1371–15. 4. Crisp JG, Takhar SS, Moran GJ, et al; for the EMERGEncy ID NET Study Group. Inability of polymerase chain reaction, pyrosequencing, and culture of infected and uninfected site skin biopsy specimens to identify the cause of cellulitis. Clin Infect Dis 2015; 61:1679–87. 5. Talan, DA, Salhi B, Moran GJ, et al. Factors associated with the decision to hospitalize emergency department patients with a skin and soft tissue infection. West J Emerg Med 2014; 16:89–97. 6. Moran GJ, Krishnadasan A, Gorwitz RJ, et al; for the EMERGEncy ID NET Study Group. Prevalence of methicillin-resistant staphylococcus aureus as an etiology of community-acquired pneumonia. Clin Infect Dis 2012; 54:1126–33. Commentary: Mandell LA, Wunderink R. Methicillin-resistant Staphylococcus aureus and community-acquired pneumonia: an evolving relationship. Clin Infect Dis 2012; 54:1134–6. 7. Ong S, Moran GJ, Krishnadasan A, Talan DA; for the EMERGEncy ID NET Study Group. Antibiotic prescribing practices of emergency physicians and patient expectations for uncomplicated lacerations. West J Emerg Med 2011; 12:375–380. 8. Talan DA, Krishnadasan A, Gorwitz RJ, et al; for the EMERGEncy ID NET Study Group. Comparison of staphylococcus aureus from skin and soft-tissue infections in US emergency department patients, 2004 and 2008. Clin Infect Dis 2011; 53:144–9. 9. Talan DA, Krishnadasan A, Abrahamian FM, Stamm WE, Moran GJ; for the EMERGEncy ID NET Study Group. Prevalence and risk factor analysis of trimethoprim-sulfamethoxazole- and fluoroquinolone-resistant Escherichia coli infection among emergency department patients with pyelonephritis. Clin Infect Dis 2008; 47:1150–8. Commentary: Lautenbach E. Finding the path of least antimicrobial resistance in pyelonephritis. Clin Infect Dis 2008; 47:1159–61. 10. Moran GJ, Barrett TW, Mower WR, et al; for the EMERGEncy ID NET Study Group. Decision instrument for the isolation of pneumonia patients with suspected pulmonary tuberculosis admitted through US emergency departments. Ann Emerg Med 2009; 53:625–32. 11. Ong S, Nakase J, Moran GJ, Karras DJ, Kuehnert MJ, Talan DA; for the EMERGEncy ID NET Study Group. Antibiotic use for emergency department patients with upper respiratory infections: prescribing practices, patient expectations, and patient satisfaction. Ann Emerg Med 2007; 50:213–20. 12. Steele MT, Ma OJ, Nakase J, et al; for the EMERGEncy ID NET Study Group. Epidemiology of animal exposures presenting to emergency departments. Acad Emerg Med 2007; 14:398–403. 13. Moran GJ, Krishnadasan A, Gorwitz RJ, et al; for the EMERGEncy ID NET Study Group. Methicillin-resistant S. aureus infections among patients in the emergency department. N Engl J Med 2006; 355:666–74. Commentary: Grayson ML. The treatment triangle for staphylococcal infections. N Engl J Med 2006; 355:724–27. 14. Karras DJ, Ong S, Moran GJ, et al; for the EMERGEncy ID NET Study Group. Antibiotic use for emergency department patients with acute diarrhea: prescribing practices, patient expectations, and patient satisfaction. Ann Emerg Med 2003; 42:835–42. 15. Talan DA, Abrahamian FM, Moran GJ, Citron DM, Tan JO, Goldstein EJC; for the EMERGEncy ID NET Study Group. Clinical presentation and bacteriologic analysis of infected human bites in patients presenting to emergency departments. Clin Infect Dis 2003; 37:1481–9. 16. Ong S, Talan DA, Moran GJ, et al; for the EMERGEncy ID NET Study Group. Neurocysticercosis in radiographically imaged seizure patients in U.S. emergency departments. Emerg Infect Dis 2002; 8:608–13. 17. Mower WR, Biros MH, Talan DA, Moran GJ, Ong S; EMERGEncy ID NET. Selective tomographic imaging of patients with new-onset seizure disorders. Acad Emerg Med 2002; 9:43–7. 18. Talan DA, Moran GJ, Newdow M, et al; for the EMERGEncy ID NET Study Group. Etiology of bloody diarrhea among patients presenting to United States emergency departments: prevalence of Escherichia coli 0157:H7 and other enteropathogens. Clin Infect Dis 2001; 32:573–80. 19. Moran GJ, Talan DA, Mower W, et al; for the EMERGEncy ID NET Study Group. Appropriateness of rabies postexposure prophylaxis treatment for animal exposures. JAMA 2000; 284:1001–7. 20. Talan DA, Moran GJ, Mower WR, et al. EMERGEncy ID NET: an emergency department-based emerging infections sentinel network. Clin Infect Dis 1999; 28:401–2. 21. Talan DA, Moran GJ, Mower WR, et al; for the EMERGEncy ID NET Study Group. EMERGEncy ID NET: an emergency department-based emerging infections sentinel network. Ann Emerg Med 1998; 32:703–11. 22. Moran GJ, Kyriacou DN, Newdow MA, Talan DA. Emergency department sentinel surveillance for emerging infectious diseases. Ann Emerg Med 1995; 26:351–4. Commentary: Garrison HG, Runyan CW, Tintinalli JE, et al. Emergency department surveillance: an examination of issues and a proposal for a national strategy. Ann Emerg Med 1994; 24:849–56. |





Comments