-
PDF
- Split View
-
Views
-
Cite
Cite
Rana F. Hamdy, Ella Magun, Shikha Saxena, Ana Maria Cardenas, Brian T. Fisher, Bloodstream Infections in Children Following Solid Organ Transplantation, Open Forum Infectious Diseases, Volume 3, Issue suppl_1, December 2016, 2304, https://doi.org/10.1093/ofid/ofw172.1851
Close - Share Icon Share
Background. Infections in the early period following solid organ transplantation (SOT) are associated with substantial morbidity and mortality. The epidemiology of bloodstream infections (BSI) in children following SOT has not been well described. The objective of this study is to describe the incidence, timing, and microbiologic distribution of BSIs in children who have undergone SOT.
Methods. We conducted a retrospective cohort study of children < 19 years of age who underwent SOT at the Children's Hospital of Philadelphia between 2000 and 2013. Patients were followed for 180 days after transplantation or until death. Demographics, transplant information, and blood culture data were systematically collected from all SOT patients through structured chart review. Subsequent positive cultures with the same organism from the same patient within 30 days and polymicrobial infections were excluded.
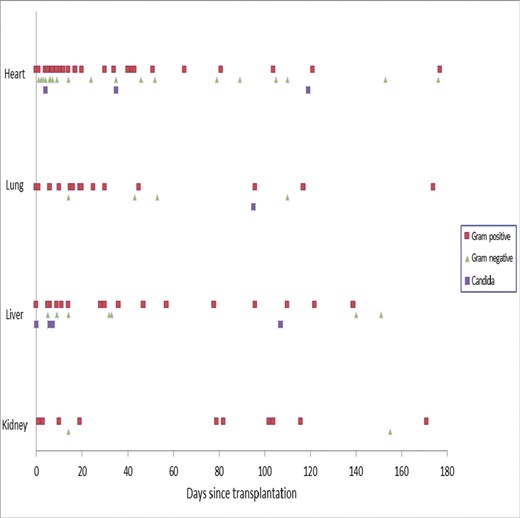
Figure: Distribution of bloodstream pathogens, by time after transplant
Results. Among the 613 children who underwent SOT in the 13-year time period (145 heart, 46 lung, 170 liver, and 252 kidney transplant recipients), 135 BSI episodes were identified. The incidence rate of BSI was highest for lung (2.8 episodes per 1,000 patient-days) and heart (2.64 per 1,000 patient-days) recipients, followed by liver (1.2 per 1,000 patient-days) and was lowest among kidney recipients (0.38 per 1,000 patient days). The median time from transplantation to first BSI was 11 days overall: 8 days for heart, 19 days for lung, 12.5 days for liver, and 79 days for kidney recipients. Gram-positive bacteria accounted for 88/135 (65%) of BSIs: 62 (46%) were due to coagulase-negative staphylococci, 13 (9.6%) were due to Enterococcus species, and 5 (3.7%) were due to Staphylococcus aureus. Gram-negative bacteria accounted for 35 (25.9%) BSIs: 12 (8.9%) Pseudomonas aeruginosa, 6 (4.4%) Enterobacter species, and 4 (3%) due to Escherichia coli. Candidemia accounted for 9 (6.7%) BSIs.
Conclusion. The timing, frequency, and epidemiology of BSI varied across organ type. BSIs were more frequent and occurred earlier after transplant among lung and heart recipients. As BSIs have significant potential morbidity for the patient and the donor organ, these data can be leveraged to inform organ specific interventions to reduce and manage BSI.
Disclosures. B. T. Fisher, Merck & Co.: Investigator, Research grant Pfizer Inc.: Investigator, Research grant Ansun BioPharma: Investigator, Research grant
Author notes
Session: 251. Transplants: Infection Epidemiology and Outcome in Solid Organ Transplantation
Saturday, October 29, 2016: 12:30 PM





Comments