-
PDF
- Split View
-
Views
-
Cite
Cite
Mina Suh, Naimisha Movva, Xiaohui Jiang, Heidi Reichert, Susan T Pastula, Naomi C Sacks, Cara Frankenfeld, Jon P Fryzek, Eric A F Simões, Healthcare Utilization Among Infants Covered by Medicaid and Newly Diagnosed With Respiratory Syncytial Virus, Open Forum Infectious Diseases, Volume 11, Issue 4, April 2024, ofae174, https://doi.org/10.1093/ofid/ofae174
Close - Share Icon Share
Abstract
Infants covered by Medicaid have higher respiratory syncytial virus (RSV) hospitalization rates than those with commercial insurance, but findings are limited to the inpatient setting. This birth cohort study describes healthcare encounters for RSV across all settings among infants covered by Medicaid and the Children's Health Insurance Program.
Medicaid claims for infants born and residing in Arizona (AZ), California (CA), Florida (FL), Michigan (MI), North Carolina (NC), New York (NY), and Texas (TX) were analyzed for first diagnosis of RSV in 2016–2018 using International Classification of Diseases, Tenth Revision codes. Encounters on the day of first diagnosis were examined by setting in 7 states and by setting and race in CA, FL, and NC.
A total of 80 945 infants were diagnosed with RSV in 7 states in 2016–2018. The highest encounter rates for first RSV diagnosis were in the emergency department (ED) in 5 states (11.0–33.4 per 1000 in AZ, CA, FL, MI, and NY) and outpatient setting in 2 states (54.8 and 68.5 per 1000 in TX and NC). Significantly higher outpatient encounter rates were found in CA and NC for White infants compared to non-White infants. In NC, ED encounter rates were significantly higher for non-White infants than White infants, whereas in CA, the rates were comparable. In these 2 states, hospitalization rates were similar across groups. In FL, compared with White infants, non-White infants had significantly higher encounter rates in each setting on the day of first RSV diagnosis.
This is the first study to describe the burden of RSV by setting and race. Medicaid infants who are newly diagnosed with RSV have the highest burden in ED and outpatient settings.
Respiratory syncytial virus (RSV) is a common virus that impacts nearly all young children [1, 2]. Globally, RSV is the leading cause of infant hospitalizations and lower respiratory tract infections including bronchiolitis [2–5]. In the United States (US), RSV epidemiology and associated healthcare utilization (HCU) among infants have been shown to vary by sociodemographic factors such as insurance type [6]. In recent studies using nationally representative datasets in the US, infants with Medicaid coverage were observed to have more than twice the RSV-associated hospitalizations and deaths compared to those covered by commercial insurance, indicating potential healthcare disparities [3, 7].
However, reasons for this difference are unknown, and much of the RSV literature landscape is focused on the inpatient hospital setting only [6, 8]. To improve our understanding of RSV and associated HCU among infants covered by state Medicaid programs, a birth cohort study was conducted to examine diagnoses of RSV and bronchiolitis in 7 states in the US across all settings. Our particular interest was in the healthcare settings in which infants covered by Medicaid were seen on the day of first RSV or bronchiolitis diagnosis. Historically, laboratory testing for RSV was conducted primarily in the inpatient hospital setting [8]. Hence, bronchiolitis was evaluated as an upper estimate of RSV.
METHODS
This birth cohort study utilized the Transformed Medicaid Statistical Information System Analytic Files from the US Centers for Medicare and Medicaid Services (CMS). These data contain eligibility and demographic information for all Medicaid and Children's Health Insurance Program (CHIP) beneficiaries. The files also comprise claims with service utilization data, including International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) diagnosis codes as well as information on healthcare setting and date of care. We used the place of service code on each claim to identify the setting of care and categorized visits as inpatient, emergency department (ED), and outpatient.
Medicaid and CHIP programs are state-specific with states administering their own Medicaid programs within the US federal guidelines [9, 10]. CHIP provides healthcare benefits to children of families who do not qualify for Medicaid based on income but do not have the means to purchase their own commercial insurance [10]. Some states have expanded their Medicaid programs to cover all individuals below income thresholds; others have used a combination of both types of programs to provide coverage [10]. Hence, all state-specific analyses conducted include both Medicaid and CHIP populations. Therefore, throughout this article, the term “Medicaid” will refer to coverage under both Medicaid and CHIP programs. We followed infants born in 7 geographically diverse states (Arizona [AZ], California [CA], Florida [FL], Michigan [MI], North Carolina [NC], New York [NY], and Texas [TX]) and having first diagnosis of RSV/bronchiolitis in their first year of life for the years 2016–2018. These states were selected because they had data available for multiple years and were of good quality according to the Medicaid.gov DQAtlas [11].
The eligibility criteria were (1) infants born from 1 January 2016 through 30 November 2017 and residing in 1 of the included states; and (2) had continuous enrollment in Medicaid from birth through age 12 months (13 months if diagnosed at 12 months of age). The end year of the study was 2018 due to our predefined eligibility criteria and CMS data availability.
Infants with a first diagnosis of RSV within their first year of life in any setting (inpatient, ED, outpatient) were identified using ICD-10 diagnosis codes (B97.4, J12.1, J20.5, J21.0). Infants with a first bronchiolitis diagnosis within the first year of life were assessed using the ICD-10 codes for RSV plus J21.8, J21.9. We identified the first diagnosis of RSV or bronchiolitis by evaluating all healthcare encounters for up to 12 months from the date of birth (or 13 months if diagnosed at 12 months of age). Infants with >1 claim for a healthcare encounter with an RSV or bronchiolitis diagnosis on the same day were all counted. For the first RSV or bronchiolitis diagnosis, we calculated incidence rates per 1000 Medicaid live births and 95% confidence interval (CI). The statewide Medicaid birth totals from the National Center for Health Statistics birth data files [12], which may include CHIP beneficiaries as there is not a separation designation option for CHIP, were used as the denominators. We also calculated the healthcare encounter rates per 1000 Medicaid live births and 95% CI by subgroups of setting, race, and state.
For the first RSV or bronchiolitis diagnosis, we also calculated the percentage of incident cases seen in each setting and in each setting by race. To do so, we used total number of infants covered by Medicaid and diagnosed with RSV/bronchiolitis before age 1 year in each state as the denominators. As described above, a patient can be in multiple settings on the same date; hence, percentages will not add to 100% for each state. This allows us to understand the complete burden associated with first RSV or bronchiolitis diagnosis by setting.
The analyses of outcomes by setting and race used CA, FL, and NC data because the other remaining states had >20% of infants missing the race variable. Moreover, we analyzed data of infants with known race information and did not evaluate infants with missing/unknown race. White infants were non-Hispanic White, while non-White infants comprised Hispanic (all races), Black non-Hispanic, American Indian and Alaska Native non-Hispanic, Asian, and Hawaiian/Pacific Islander.
All analyses were conducted using SAS software, version 9.4. Data were visualized using Prism 10 for MacOS, version 10.0 and R Studio.
Patient Consent Statement
This study was categorized as exempt by the Ethical and Independent Review Services (E&I) Institutional Review Board as we analyzed de-identified data without personal identifiers (study ID 21004–01).
RESULTS
From 2016 to 2018, there were 1 445 937 live births covered by Medicaid across the 7 states. During this period, 291 112 infants covered by Medicaid had their first bronchiolitis diagnosis; among these infants, 80 945 had their first RSV diagnosis (Tables 1 and 2). The majority of infants covered by Medicaid and newly diagnosed with RSV were male (range: 52.3%–55.5%) and aged 1–6 months at diagnosis (range: 63.6%–68.0%) (Table 1). In CA, FL, NC, and TX, most infants were non-White (range: 44%–69%) (Table 1). For first bronchiolitis diagnosis, similar patterns were observed as the majority of infants were male (range: 55.7%–58%) and aged 1–6 months at diagnosis (range: 60.4%–68.4%); non-White infants comprised the majority in CA, FL, NC, and TX (range: 46%–71%) (Supplementary Table 1).
Number of Infants Covered by Medicaid With First Respiratory Syncytial Virus Diagnosisa by Sex, Age at Diagnosis, and Race in Each State, 2016–2018
| Characteristic . | Arizona . | California . | Florida . | Michigan . | North Carolina . | New York . | Texas . |
|---|---|---|---|---|---|---|---|
| Sex, No. (%) | |||||||
| Male | 2301 (52.3) | 3686 (55.2) | 7299 (54.0) | 1844 (54.1) | 5396 (54.5) | 5121 (55.5) | 17 842 (52.8) |
| Female | 2097 (47.7) | 2996 (44.8) | 6215 (46.0) | 1559 (45.7) | 4499 (45.5) | 4102 (44.5) | 15 954 (47.2) |
| Age at diagnosis, No. (%) | |||||||
| <1 mo | 385 (8.8) | 266 (4.0) | 971 (7.2) | 222 (6.5) | 487 (4.9) | 669 (7.2) | 1857 (5.5) |
| 1–6 mo | 2872 (65.3) | 4406 (65.9) | 9195 (68.0) | 2206 (64.7) | 6292 (63.6) | 6010 (65.1) | 22 302 (66.0) |
| 7–11 mo | 1143 (26.0) | 2010 (30.1) | 3350 (24.8) | 982 (28.8) | 3117 (31.5) | 2549 (27.6) | 9654 (28.6) |
| Race, No. (%) | |||||||
| White | 1672 (38.0) | 935 (14.0) | 3037 (22.5) | 700 (20.5) | 4260 (43.1) | 3032 (32.9) | 7589 (22.4) |
| Non-White | 1130 (25.7) | 4615 (69.1) | 7858 (58.1) | 631 (18.5) | 5623 (56.8) | 2746 (29.8) | 14 774 (43.7) |
| Missing/unknown | 1598 (36.3) | 1132 (16.9) | 2621 (19.4) | 2079 (61.0) | 13 (0.1) | 3450 (37.4) | 11 450 (33.9) |
| Characteristic . | Arizona . | California . | Florida . | Michigan . | North Carolina . | New York . | Texas . |
|---|---|---|---|---|---|---|---|
| Sex, No. (%) | |||||||
| Male | 2301 (52.3) | 3686 (55.2) | 7299 (54.0) | 1844 (54.1) | 5396 (54.5) | 5121 (55.5) | 17 842 (52.8) |
| Female | 2097 (47.7) | 2996 (44.8) | 6215 (46.0) | 1559 (45.7) | 4499 (45.5) | 4102 (44.5) | 15 954 (47.2) |
| Age at diagnosis, No. (%) | |||||||
| <1 mo | 385 (8.8) | 266 (4.0) | 971 (7.2) | 222 (6.5) | 487 (4.9) | 669 (7.2) | 1857 (5.5) |
| 1–6 mo | 2872 (65.3) | 4406 (65.9) | 9195 (68.0) | 2206 (64.7) | 6292 (63.6) | 6010 (65.1) | 22 302 (66.0) |
| 7–11 mo | 1143 (26.0) | 2010 (30.1) | 3350 (24.8) | 982 (28.8) | 3117 (31.5) | 2549 (27.6) | 9654 (28.6) |
| Race, No. (%) | |||||||
| White | 1672 (38.0) | 935 (14.0) | 3037 (22.5) | 700 (20.5) | 4260 (43.1) | 3032 (32.9) | 7589 (22.4) |
| Non-White | 1130 (25.7) | 4615 (69.1) | 7858 (58.1) | 631 (18.5) | 5623 (56.8) | 2746 (29.8) | 14 774 (43.7) |
| Missing/unknown | 1598 (36.3) | 1132 (16.9) | 2621 (19.4) | 2079 (61.0) | 13 (0.1) | 3450 (37.4) | 11 450 (33.9) |
Across the 7 states, 99.7% of the infants with first RSV diagnosis had Medicaid coverage, while <0.3% were covered by the Children's Health Insurance Program.
aRSV diagnoses were identified using the International Classification of Diseases, Tenth Revision codes B97.4, J12.1, J20.5, J21.0.
Number of Infants Covered by Medicaid With First Respiratory Syncytial Virus Diagnosisa by Sex, Age at Diagnosis, and Race in Each State, 2016–2018
| Characteristic . | Arizona . | California . | Florida . | Michigan . | North Carolina . | New York . | Texas . |
|---|---|---|---|---|---|---|---|
| Sex, No. (%) | |||||||
| Male | 2301 (52.3) | 3686 (55.2) | 7299 (54.0) | 1844 (54.1) | 5396 (54.5) | 5121 (55.5) | 17 842 (52.8) |
| Female | 2097 (47.7) | 2996 (44.8) | 6215 (46.0) | 1559 (45.7) | 4499 (45.5) | 4102 (44.5) | 15 954 (47.2) |
| Age at diagnosis, No. (%) | |||||||
| <1 mo | 385 (8.8) | 266 (4.0) | 971 (7.2) | 222 (6.5) | 487 (4.9) | 669 (7.2) | 1857 (5.5) |
| 1–6 mo | 2872 (65.3) | 4406 (65.9) | 9195 (68.0) | 2206 (64.7) | 6292 (63.6) | 6010 (65.1) | 22 302 (66.0) |
| 7–11 mo | 1143 (26.0) | 2010 (30.1) | 3350 (24.8) | 982 (28.8) | 3117 (31.5) | 2549 (27.6) | 9654 (28.6) |
| Race, No. (%) | |||||||
| White | 1672 (38.0) | 935 (14.0) | 3037 (22.5) | 700 (20.5) | 4260 (43.1) | 3032 (32.9) | 7589 (22.4) |
| Non-White | 1130 (25.7) | 4615 (69.1) | 7858 (58.1) | 631 (18.5) | 5623 (56.8) | 2746 (29.8) | 14 774 (43.7) |
| Missing/unknown | 1598 (36.3) | 1132 (16.9) | 2621 (19.4) | 2079 (61.0) | 13 (0.1) | 3450 (37.4) | 11 450 (33.9) |
| Characteristic . | Arizona . | California . | Florida . | Michigan . | North Carolina . | New York . | Texas . |
|---|---|---|---|---|---|---|---|
| Sex, No. (%) | |||||||
| Male | 2301 (52.3) | 3686 (55.2) | 7299 (54.0) | 1844 (54.1) | 5396 (54.5) | 5121 (55.5) | 17 842 (52.8) |
| Female | 2097 (47.7) | 2996 (44.8) | 6215 (46.0) | 1559 (45.7) | 4499 (45.5) | 4102 (44.5) | 15 954 (47.2) |
| Age at diagnosis, No. (%) | |||||||
| <1 mo | 385 (8.8) | 266 (4.0) | 971 (7.2) | 222 (6.5) | 487 (4.9) | 669 (7.2) | 1857 (5.5) |
| 1–6 mo | 2872 (65.3) | 4406 (65.9) | 9195 (68.0) | 2206 (64.7) | 6292 (63.6) | 6010 (65.1) | 22 302 (66.0) |
| 7–11 mo | 1143 (26.0) | 2010 (30.1) | 3350 (24.8) | 982 (28.8) | 3117 (31.5) | 2549 (27.6) | 9654 (28.6) |
| Race, No. (%) | |||||||
| White | 1672 (38.0) | 935 (14.0) | 3037 (22.5) | 700 (20.5) | 4260 (43.1) | 3032 (32.9) | 7589 (22.4) |
| Non-White | 1130 (25.7) | 4615 (69.1) | 7858 (58.1) | 631 (18.5) | 5623 (56.8) | 2746 (29.8) | 14 774 (43.7) |
| Missing/unknown | 1598 (36.3) | 1132 (16.9) | 2621 (19.4) | 2079 (61.0) | 13 (0.1) | 3450 (37.4) | 11 450 (33.9) |
Across the 7 states, 99.7% of the infants with first RSV diagnosis had Medicaid coverage, while <0.3% were covered by the Children's Health Insurance Program.
aRSV diagnoses were identified using the International Classification of Diseases, Tenth Revision codes B97.4, J12.1, J20.5, J21.0.
Number of Infants Covered by Medicaid With First Diagnosis of Respiratory Syncytial Virus and Bronchiolitis in First Year of Life and Incidence Rates, 2016–2018
| States . | RSVa . | Bronchiolitisa . | ||
|---|---|---|---|---|
| Incident Cases, No. . | Incidence Rate (95% CI) per 1000 Medicaid Live Birthsb . | Incident Cases, No. . | Incidence Rate (95% CI) per 1000 Medicaid Live Birthsb . | |
| Arizona | 4400 | 52.2 (50.6–53.8) | 19 573 | 232.2 (228.6–235.9) |
| California | 6682 | 16.8 (16.4–17.2) | 35 902 | 90.1 (89.2–91.1) |
| Florida | 13 516 | 64.8 (63.7–66.0) | 38 163 | 183.1 (181.1–185.1) |
| Michigan | 3410 | 37.4 (36.1–38.7) | 11 441 | 125.4 (123.0–127.8) |
| North Carolina | 9896 | 100.4 (98.3–102.5) | 26 824 | 272.1 (268.5–275.8) |
| New York | 9228 | 43.2 (42.3–44.1) | 42 417 | 198.7 (196.6–200.8) |
| Texas | 33 813 | 96.2 (95.1–97.3) | 116 792 | 332.3 (330.1–334.5) |
| Total (7 states) | 80 945 | … | 291 112 | … |
| States . | RSVa . | Bronchiolitisa . | ||
|---|---|---|---|---|
| Incident Cases, No. . | Incidence Rate (95% CI) per 1000 Medicaid Live Birthsb . | Incident Cases, No. . | Incidence Rate (95% CI) per 1000 Medicaid Live Birthsb . | |
| Arizona | 4400 | 52.2 (50.6–53.8) | 19 573 | 232.2 (228.6–235.9) |
| California | 6682 | 16.8 (16.4–17.2) | 35 902 | 90.1 (89.2–91.1) |
| Florida | 13 516 | 64.8 (63.7–66.0) | 38 163 | 183.1 (181.1–185.1) |
| Michigan | 3410 | 37.4 (36.1–38.7) | 11 441 | 125.4 (123.0–127.8) |
| North Carolina | 9896 | 100.4 (98.3–102.5) | 26 824 | 272.1 (268.5–275.8) |
| New York | 9228 | 43.2 (42.3–44.1) | 42 417 | 198.7 (196.6–200.8) |
| Texas | 33 813 | 96.2 (95.1–97.3) | 116 792 | 332.3 (330.1–334.5) |
| Total (7 states) | 80 945 | … | 291 112 | … |
Across the 7 states, 99.7% of the infants with first bronchiolitis or RSV diagnosis had Medicaid coverage, while <0.3% were covered by the Children's Health Insurance Program.
Abbreviations: CI, confidence interval; RSV, respiratory syncytial virus.
aRSV and bronchiolitis diagnoses were identified using the International Classification of Diseases, Tenth Revision codes B97.4, J12.1, J20.5, J21.0 for RSV; RSV codes plus J21.8, J21.9 for bronchiolitis.
bThe total number of live births covered by Medicaid across the 7 states in 2016–2018 was 1 445 937. Live births covered by Medicaid in each state were used as the denominator for the incidence rates.
Number of Infants Covered by Medicaid With First Diagnosis of Respiratory Syncytial Virus and Bronchiolitis in First Year of Life and Incidence Rates, 2016–2018
| States . | RSVa . | Bronchiolitisa . | ||
|---|---|---|---|---|
| Incident Cases, No. . | Incidence Rate (95% CI) per 1000 Medicaid Live Birthsb . | Incident Cases, No. . | Incidence Rate (95% CI) per 1000 Medicaid Live Birthsb . | |
| Arizona | 4400 | 52.2 (50.6–53.8) | 19 573 | 232.2 (228.6–235.9) |
| California | 6682 | 16.8 (16.4–17.2) | 35 902 | 90.1 (89.2–91.1) |
| Florida | 13 516 | 64.8 (63.7–66.0) | 38 163 | 183.1 (181.1–185.1) |
| Michigan | 3410 | 37.4 (36.1–38.7) | 11 441 | 125.4 (123.0–127.8) |
| North Carolina | 9896 | 100.4 (98.3–102.5) | 26 824 | 272.1 (268.5–275.8) |
| New York | 9228 | 43.2 (42.3–44.1) | 42 417 | 198.7 (196.6–200.8) |
| Texas | 33 813 | 96.2 (95.1–97.3) | 116 792 | 332.3 (330.1–334.5) |
| Total (7 states) | 80 945 | … | 291 112 | … |
| States . | RSVa . | Bronchiolitisa . | ||
|---|---|---|---|---|
| Incident Cases, No. . | Incidence Rate (95% CI) per 1000 Medicaid Live Birthsb . | Incident Cases, No. . | Incidence Rate (95% CI) per 1000 Medicaid Live Birthsb . | |
| Arizona | 4400 | 52.2 (50.6–53.8) | 19 573 | 232.2 (228.6–235.9) |
| California | 6682 | 16.8 (16.4–17.2) | 35 902 | 90.1 (89.2–91.1) |
| Florida | 13 516 | 64.8 (63.7–66.0) | 38 163 | 183.1 (181.1–185.1) |
| Michigan | 3410 | 37.4 (36.1–38.7) | 11 441 | 125.4 (123.0–127.8) |
| North Carolina | 9896 | 100.4 (98.3–102.5) | 26 824 | 272.1 (268.5–275.8) |
| New York | 9228 | 43.2 (42.3–44.1) | 42 417 | 198.7 (196.6–200.8) |
| Texas | 33 813 | 96.2 (95.1–97.3) | 116 792 | 332.3 (330.1–334.5) |
| Total (7 states) | 80 945 | … | 291 112 | … |
Across the 7 states, 99.7% of the infants with first bronchiolitis or RSV diagnosis had Medicaid coverage, while <0.3% were covered by the Children's Health Insurance Program.
Abbreviations: CI, confidence interval; RSV, respiratory syncytial virus.
aRSV and bronchiolitis diagnoses were identified using the International Classification of Diseases, Tenth Revision codes B97.4, J12.1, J20.5, J21.0 for RSV; RSV codes plus J21.8, J21.9 for bronchiolitis.
bThe total number of live births covered by Medicaid across the 7 states in 2016–2018 was 1 445 937. Live births covered by Medicaid in each state were used as the denominator for the incidence rates.
The incidence rates for the first RSV diagnosis in the first year of life ranged from 16.8 (95% CI, 16.4–17.2) per 1000 Medicaid live births in CA to 100.4 (95% CI, 98.3–102.5) per 1000 Medicaid live births in NC (Table 2). The incidence rates for the first bronchiolitis diagnosis in the first year of life ranged from 90.1 (95% CI, 89.2–91.1) per 1000 Medicaid live births in CA to 332.3 (95% CI, 330.1–334.5) per 1000 Medicaid live births in TX (Table 2).
Healthcare Encounters for RSV and Bronchiolitis by Setting in 7 States: Infants Covered by Medicaid
Healthcare encounter rates per 1000 Medicaid live births on the day of first RSV diagnosis were highest in the ED in 5 states (11.0–33.4 per 1000 in AZ, CA, FL, MI, and NY) and in the outpatient setting in the remaining 2 states (54.8 and 68.5 per 1000 in TX and NC, respectively) (Figure 1A). On the day of first bronchiolitis diagnosis, healthcare encounter rates per 1000 Medicaid live births were highest in the outpatient setting in all 7 states (49.5–224.7 per 1000) (Figure 1B).
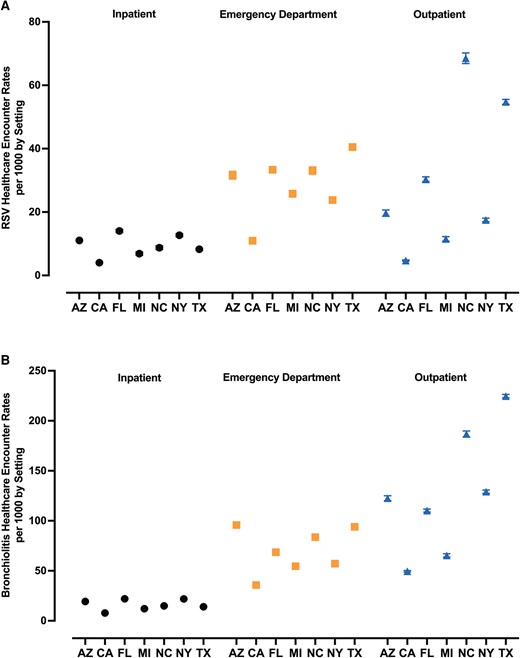
On the day of first diagnosis, highest respiratory syncytial virus (RSV) (A) and bronchiolitis (B) healthcare encounter rates per 1000 Medicaid live births were observed in the emergency department and outpatient settings, 2016–2018. Denominator: Total number of live births covered by Medicaid in each state. Across the 7 states, 99.7% of the infants with first bronchiolitis or RSV diagnosis had Medicaid coverage, while <0.3% were covered by the Children's Health Insurance Program. RSV and bronchiolitis diagnoses were identified using the International Classification of Diseases, Tenth Revision codes B97.4, J12.1, J20.5, J21.0 for RSV, and RSV codes plus J21.8, J21.9 for bronchiolitis. Abbreviations: AZ, Arizona; CA, California; FL, Florida; MI, Michigan; NC, North Carolina; NY, New York; RSV, respiratory syncytial virus; TX, Texas.
Among incident RSV cases, 52%–69% had an ED encounter on the day of their first RSV diagnosis in 5 states (AZ, CA, FL, MI, and NY) (Figure 2A). In the remaining 2 states (TX and NC), a substantial proportion had an ED encounter on the day of their first RSV diagnosis (TX: 42%; NC: 33%), but a larger proportion had an outpatient encounter (TX: 57%; NC: 68%) (Figure 2A). Across the 7 states, 9%–29% of incident cases had a hospitalization for RSV on the day of their first RSV diagnosis (Figure 2A). Among incident bronchiolitis cases, encounters on the day of diagnosis were highest in outpatient settings in all 7 states (52%–69%) with fewer infants having an ED encounter (28%–44%) or inpatient admission (4%–12%) (Figure 2B).
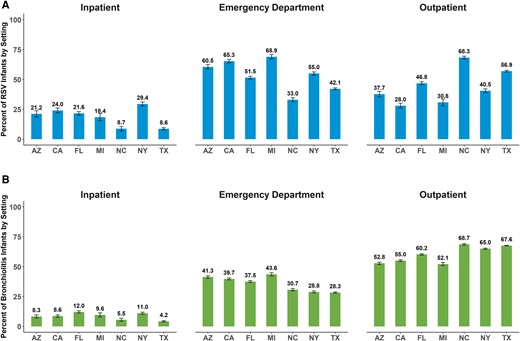
Among infants covered by Medicaid, first diagnosis of respiratory syncytial virus (RSV) (A) and bronchiolitis (B) occurred more often in the emergency department and outpatient settings than the inpatient setting, 2016–2018. Denominator: Total number of infants covered by Medicaid and diagnosed with RSV/bronchiolitis before age 1 year in each state. Across the 7 states, 99.7% of the infants with first bronchiolitis or RSV diagnosis had Medicaid coverage, while <0.3% were covered by the Children's Health Insurance Program. RSV and bronchiolitis diagnoses were identified using International Classification of Diseases, Tenth Revision codes B97.4, J12.1, J20.5, J21.0 for RSV, and RSV codes plus J21.8, J21.9 for bronchiolitis. Abbreviations: AZ, Arizona; CA, California; FL, Florida; MI, Michigan; NC, North Carolina; NY, New York; RSV, respiratory syncytial virus; TX, Texas.
Healthcare Encounters for RSV and Bronchiolitis by Setting and Race in CA, FL, and NC: Infants Covered by Medicaid
When healthcare encounters of incident RSV and bronchiolitis cases were examined by setting and race in CA, FL, and NC, several patterns emerged. In CA, the highest encounter rates per 1000 Medicaid live births on the day of first RSV diagnosis were in the ED for both non-White and White infants (Figure 3A). In CA, ED encounter rates per 1000 were comparable between non-White and White infants (9.3 [95% CI, 8.9–9.6] vs 9.7 [95% CI, 8.9–10.4], respectively), as well as hospitalization rates (3.5 [95% CI, 3.3–3.7] vs 3.0 [95% CI, 2.6–3.5] per 1000, respectively). For outpatient encounters, White infants had significantly higher rates (5.2 [95% CI, 4.6–5.7] per 1000 Medicaid live births) than non-White infants (3.7 [95% CI, 3.5–3.9]).
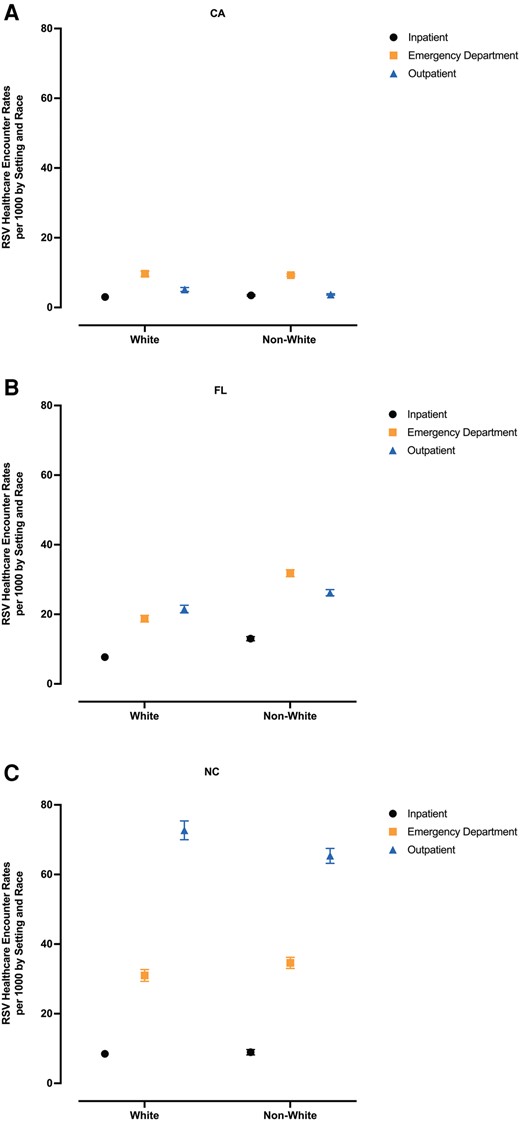
On the day of first diagnosis, among White- and non-White Medicaid infants born in California (A), Florida (B), and North Carolina (C), highest respiratory syncytial virus (RSV) healthcare encounter rates per 1000 Medicaid live births were in the emergency department and outpatient settings, 2016–2018. Denominator: Total number of live births covered by Medicaid in each state. Across the 7 states, 99.7% of the infants with first RSV diagnosis had Medicaid coverage, while <0.3% were covered by the Children's Health Insurance Program. RSV diagnoses were identified using International Classification of Diseases, Tenth Revision codes B97.4, J12.1, J20.5, J21.0. States with overall race data as >20% missing were not evaluated (Arizona, Michigan, New York, Texas). White infants: non-Hispanic White. Non-White infants: Hispanic (all races), Black non-Hispanic, American Indian and Alaska Native non-Hispanic, Asian, Hawaiian/Pacific Islander. Abbreviations: CA, California; FL, Florida; NC, North Carolina; RSV, respiratory syncytial virus.
In FL, compared with White infants, non-White infants had significantly higher encounter rates per 1000 Medicaid live births in each setting on the day of first RSV diagnosis (Figure 3B). ED encounter rates per 1000 were significantly higher for non-White infants than for White infants (31.8 [95% CI, 30.8–32.8] vs 18.7 [95% CI, 17.8–19.7], respectively), as were hospitalization rates (13.0 [95% CI, 12.4–13.6] vs 7.7 [95% CI, 7.1–8.3]) and outpatient encounter rates (26.2 [95% CI, 25.3–27.1] vs 21.5 [95% CI, 20.4–22.6]).
In NC, compared with White infants, non-White infants had significantly higher ED encounter rates per 1000 Medicaid live births (31.0 [95% CI, 29.3–32.7] vs 34.6 [95% CI, 33.0–36.2], respectively) (Figure 3C). However, hospital admission rates per 1000 Medicaid live births were comparable between the racial groups (White: 8.5 [95% CI, 7.6–9.4] vs non-White: 8.9 [95% CI, 8.2–9.7]), while White infants had significantly a higher outpatient encounter rate per 1000 Medicaid live births (72.7 [95% CI, 70.0–75.4] vs non-White: 65.4 [95% CI, 63.2–67.5]).
On the day of first bronchiolitis diagnosis, the highest encounter rates per 1000 Medicaid live births were in the outpatient setting for both White and non-White infants in CA, FL, and NC (Supplementary Table 2). In all 3 states and settings, non-White infants had significantly higher encounter rates per 1000 Medicaid live births compared with White infants, except for the outpatient setting in NC where the rates were comparable.
Among incident RSV cases in CA, FL, and NC, the majority of healthcare encounters on the day of RSV diagnosis were for non-White infants (Figure 4). The percentage of non-White infants with encounters in each setting-state combination ranged from 55% to 71% (vs White infants: 12%–45%). The proportion of outpatient encounters for White infants (17%–45%) was higher than those in the ED and inpatient settings (12%–41%).
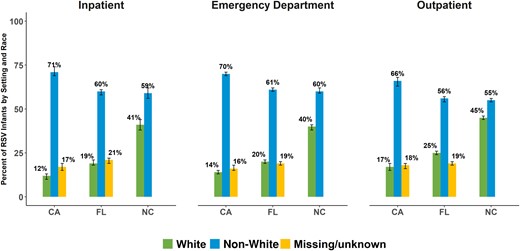
Among infants covered by Medicaid, more healthcare encounters for respiratory syncytial virus (RSV) on the day of first diagnosis were for non-White than White infants across all healthcare settings, 2016–2018. Denominator: Total number of infants covered by Medicaid and diagnosed with RSV before age 1 year in specific setting and state. Across the 7 states, 99.7% of the infants with first RSV diagnosis had Medicaid coverage, while <0.3% were covered by the Children's Health Insurance Program. RSV diagnoses were identified using the International Classification of Diseases, Tenth Revision codes B97.4, J12.1, J20.5, J21.0. States with overall race data as >20% missing were not evaluated (Arizona, Michigan, New York, Texas). For North Carolina infants with missing/unknown race, data suppression is in effect due to the Centers for Medicare and Medicaid Services reporting policy. White infants: non-Hispanic White. Non-White infants: Hispanic (all races), Black non-Hispanic, American Indian and Alaska Native non-Hispanic, Asian, Hawaiian/Pacific Islander. Abbreviations: CA, California; FL, Florida; NC, North Carolina; RSV, respiratory syncytial virus.
Consistent with RSV, among incident bronchiolitis cases in CA, FL, and NC, the proportion of healthcare encounters was higher for non-White infants, compared with White infants in each state and setting (57%–73% vs 12%–42%) (Supplementary Figure 1). In contrast to RSV, however, the proportions of non-White and White infants with healthcare encounters on the day of first bronchiolitis diagnosis were similar in each setting in CA and FL, while the percentage of outpatient encounters for White infants in NC (42%) was larger compared with the inpatient (38%) and ED (32%) settings.
DISCUSSION
This is the first study evaluating the RSV burden among infants with Medicaid coverage in all healthcare settings. Across 7 geographically diverse states, this birth cohort study followed >80 000 infants with a first RSV diagnosis within the first year of life from 2016 to 2018. These infants are 1 of the largest infant RSV populations ever studied. On the day of first RSV/bronchiolitis diagnosis, we also provided healthcare encounter rates per 1000 Medicaid live births in each setting. The results of this study demonstrate the importance of considering all healthcare settings to describe RSV-associated healthcare encounters among infants covered by Medicaid. On the day of their first diagnosis with RSV, infants born in AZ, CA, FL, MI, or NY and covered by Medicaid were seen most frequently in the ED, whereas those born in TX and NC were seen most often in the outpatient setting.
When we examined healthcare encounters on the day of diagnosis for the first incident RSV cases by race in CA, FL, and NC, we found that ED and outpatient encounter rates were highest for both non-White and White infants, as they were for the overall infant study population across all 7 states. We also found that non-White infants newly diagnosed with RSV had comparable or higher rates of ED encounters and hospitalizations. In FL, for example, hospitalization and ED encounter rates were significantly higher for non-White infants compared with White infants. Similarly, ED encounter rates were significantly higher for non-White infants in NC, compared with White infants. The higher rates of ED encounters in 2 of 3 states may reflect a need for emergent care as well as disparities in access to primary care outpatient treatment [13, 14]. The significantly higher rates of hospitalizations in 1 study state, coupled with significantly lower rates of outpatient encounters in 2 of 3 states, may also reflect greater illness severity among non-White compared with White infants covered by Medicaid and diagnosed with RSV. Additionally, the large proportions of non-White infants with healthcare encounters on the day of first RSV diagnosis in all 3 states reflects the need for preventive measures and early delivery of care in this vulnerable population.
This study has several strengths. The datasets prepared by CMS and used in this study represent the largest collection of state-specific claims for RSV and bronchiolitis in the US [15]. This is a large population at risk of serious illnesses from RSV that should be followed to identify potential obstacles to care that are specific to this group of infants. This study analyzed infants across 7 geographically diverse states, presenting novel insights into the characteristics of infants with newly diagnosed RSV. Another strength of this study includes comprehensively describing the RSV epidemiology among infants covered by Medicaid in 7 states across all healthcare settings. Furthermore, we have described patterns of HCU by race in each setting for 3 states. Studies have reported multiple healthcare encounters after the initial RSV infection [16, 17], highlighting the subsequent effects for the patients and health systems. As these datasets are at the infant level and standardized to facilitate complete follow-up from birth and across all settings, we have the potential to further examine subsequent illnesses associated with the index RSV diagnosis and HCU including the use of intensive care and mechanical ventilation among Medicaid infants.
This study has limitations. For the calculation of rates, we used statewide Medicaid birth totals from the National Center for Health Statistics birth data files [12] as the denominators. We did not consider potential discontinuation of enrollment in Medicaid and losses in the denominator numbers. Although information specific to infants is not described in the literature, Medicaid disenrollment data for children indicate that noncontinuous enrollment is substantial with >20% loss [18, 19]. In our cohort of infants with RSV or bronchiolitis, we observed that 17% overall were dropped for noncontinuous enrollment in Medicaid; thus, our rates may be underestimating the impacts of RSV. Not all providers may test for RSV. Laboratory testing is primarily conducted in the inpatient setting; consequently, RSV is likely to be underestimated, especially outside the inpatient hospital setting [6, 8]. There also may be potential differences in RSV laboratory testing patterns by race. With increased laboratory testing that has emerged with coronavirus disease 2019 (COVID-19), additional studies are needed to further explain HCU patterns in context of RSV laboratory testing practice among infants covered by Medicaid. For the healthcare encounter rates by race in each state and setting, we did not include infants with unknown race. Within CMS, discussions are ongoing regarding the quality of race data with incomplete information reported for approximately 19% of Medicaid beneficiaries [20]. As missing race information may introduce bias in these datasets and thereby the health research findings in this population, substantial efforts are underway to improve the quality of this variable in the Medicaid data [20]. In addition, bronchiolitis is defined by ICD-10 RSV codes plus codes for unspecified bronchiolitis, but some cases may not be related to RSV. Finally, these data are for the pre-COVID-19 era; additional studies will need to be conducted in the COVID-19 era.
CONCLUSIONS
In conclusion, these results provide additional insights regarding RSV-associated HCU for infants covered by Medicaid. While we found high rates of HCU across race, we also observed differences in RSV by race, emphasizing the importance of equitable access to preventive measures. In the US, a new monoclonal antibody (nirsevimab) and maternal vaccine were recently approved to prevent RSV in infants and young children [21–23]. Notably, with nirsevimab and maternal vaccines, potential issues of equity in access were discussed and shortages with rationing were reported in the 2023–2024 winter season [24–26]. Medicaid programs covered 41% of US live births in 2021 (>3.6 million) [27]; continued evidence generation in this large population group will be needed to address the equity domain in the US Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices Evidence to Recommendations Framework. This study highlights the need to ensure access to preventive measures for infants with Medicaid coverage across all healthcare settings. Without equitable access to these preventive measures, our efforts to lessen the burden of RSV among infants may be hindered.
Supplementary Data
Supplementary materials are available at Open Forum Infectious Diseases online. Consisting of data provided by the authors to benefit the reader, the posted materials are not copyedited and are the sole responsibility of the authors, so questions or comments should be addressed to the corresponding author.
Notes
Author contributions. M. S., N. M., H. R., and J. P. F. conceptualized and designed the study. M. S. drafted the initial manuscript. H. R., N. M., and J. P. F. critically reviewed and revised the manuscript. X. J. and S. T. P. designed the data collection instruments, collected data, carried out the initial analyses, and critically reviewed and revised the manuscript. N. C. S. and C. F. critically reviewed and revised the manuscript. E. A. F. S. conceptualized and designed the study and critically reviewed and revised the manuscript for important intellectual content. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Previous presentations. Pediatric Academic Societies Meeting, Washington, DC, April 2023 (oral abstract); International Society of Pharmacoepidemiology Annual Conference, Halifax, Canada, August 2023 (poster).
Data sharing. De-identified individual participant data will not be made available. Per agreement with the Centers for Medicare and Medicaid Services, no data are to be shared outside of the organization.
References
Author notes
Potential conflicts of interest. EpidStrategies received funding from Sobi, Sanofi, and AstraZeneca to conduct research on respiratory syncytial virus. M. S., N. M., X. J., H. R., S. T. P., N. C. S., C. F., and J. P. F. are employees of EpidStrategies. E. A. F. S. received research funding from AstraZeneca, Merck, and Pfizer, and is a member of a data and safety monitoring board for GSK.





Comments