-
PDF
- Split View
-
Views
-
Cite
Cite
Merijn E de Swart, Mathilde C M Kouwenhoven, Tessa Hellingman, Babette I Kuiper, Cathelijne Gorter de Vries, Machteld Leembruggen-Vellinga, Niels K Maliepaard, Ernest J Wouda, Bastiaan Moraal, David P Noske, Tjeerd J Postma, Esther Sanchez Aliaga, Bernard M J Uitdehaag, William P Vandertop, Barbara M Zonderhuis, Geert Kazemier, Philip C de Witt Hamer, Maaike Schuur, A multidisciplinary neuro-oncological triage panel reduces the time to referral and treatment for patients with a brain tumor, Neuro-Oncology Practice, Volume 8, Issue 5, October 2021, Pages 559–568, https://doi.org/10.1093/nop/npab040
Close - Share Icon Share
Abstract
Regional collaboration and appropriate referral management are crucial in neuro-oncological care. Lack of electronic access to medical records across health care organizations impedes interhospital consultation and may lead to incomplete and delayed referrals. To improve referral management, we have established a multidisciplinary neuro-oncological triage panel (NOTP) with digital image exchange and determined the effects on lead times, costs, and time investment.
A prospective cohort study was conducted from February 2019 to March 2020. All newly diagnosed patients referred to Brain Tumor Center Amsterdam were analyzed according to referral pathway: (1) standard referral (SR), (2) NOTP. The primary outcome was lead time, defined as time-to-referral, time-to-treatment, and total time (median days [interquartile range]). Secondary outcomes were costs and time investment.
In total, 225 patients were included, of whom 153 had SR and 72 NOTP referral. Patients discussed in the NOTP were referred more frequently for first neurosurgical consultation (44.7% vs 28.8%) or combined neurological and neurosurgical consultation (12.8% vs 2.5%, P = .002). Time-to-referral was reduced for NOTP referral compared to SR (1 [0.25-4] vs 6 [1.5-10] days, P < .001). Total time decreased from 27 [14-48] days for the standard group to 15 [12-38.25] days for the NOTP group (P = .040). Costs and time investment were comparable for both groups.
Implementation of digital referral to a multidisciplinary NOTP is feasible and leads to more swift patient-tailored referrals at comparable costs and time investment as SR. This quality improvement initiative has the potential to improve collaboration and coordination of multidisciplinary care in the field of neuro-oncology.
Neuro-oncology entails a heterogeneous group of patients with primary benign and malignant tumors arising from the brain parenchyma and surrounding structures, and secondary tumors arising from the spread of primary tumors elsewhere to the brain. The average annual age-adjusted incidence of all primary neuro-oncological diseases is low, with 23.41 per 100 000 inhabitants of which 7.08 are malignant and 16.33 benign.1 A substantial part of neuro-oncological diseases represents a significant health burden in terms of morbidity and mortality.2
Patients with a suspected neuro-oncological disorder are referred to specialized centers with expertise in neuro-oncology.3 Referrals can be sent through several means, mainly by mail, fax, secured e-mail, or weblink, whereby documents from the same referral are each often transferred through different methods. In case of emergency, referrals are usually made after a telephone consultation. After the referral letter and diagnostic imaging are received completely, an appointment at the outpatient clinic of the addressed specialty or an interfacility admission transfer is made.
This referral pathway has several limitations. First, due to a lack of a national electronic health record or electronic health information exchange (HIE) in the Netherlands, patient information and diagnostic imaging are not accessible during telephone consultation and impede the consultation and advice.4,5 Second, patient information in portable document format (PDF) and imaging on CD-ROM provided through fax, mail or secured e-mail could lead to incomplete referrals and delayed consultation.6,7 Timely referrals in cancer care need attention since a prolonged lead time could affect emotional distress, treatment outcome, and survival.8–10 Emotional distress, and particularly increased anxiety, in the diagnostic phase of cancer, is a known major burden in patients confronted with the mere possibility of a cancer diagnosis.11,12 Patients with brain tumors have an elevated level of distress as a result of the functional sequelae and the unfavorable prognosis.13,14 Thereby, this population is vulnerable due to the possibility of rapidly progressive symptoms as a result of tumor growth in an eloquent brain area, a considerable mass effect, or obstructive hydrocephalus. Third, the current referral route might be ambiguous for referring neurologists, potentially leading to preventable delays and distress for patients.
Telehealth has previously been described as an opportunity to optimize consultations and referrals.15 Examples of telehealth are online consultation of virtual tumor boards, digital expert panels, and digital triage panels.16–22 We set out to develop a multidisciplinary neuro-oncological triage panel (NOTP) with standardized digital exchange of patient information and imaging on an online platform to improve the quality of referral in terms of accessibility for referring neurologists and timely referral for patients with neuro-oncological diseases.
The aim of the current study was to determine the effects of a digital referral system in combination with a NOTP on lead times, costs of care, and time investments.
Methods
Context
The NOTP was established at Brain Tumor Center Amsterdam (BTCA), a hospital for tertiary referrals in the metropolitan region of Amsterdam, the Netherlands. This center is 1 of the 13 hospitals providing neurosurgical treatment for patients with neuro-oncological diseases in the Netherlands.
Standard Referral
In the majority of cases, patients presented with neurological symptoms at the outpatient clinic or at the emergency department of a general hospital. After magnetic resonance imaging (MRI), patients with suspected neuro-oncological disease were referred to the BTCA. Conventionally, standard referral (SR) was accomplished following 2 pathways: (1) via a referral letter in PDF through fax, mail, or secured e-mail sent by the secretary of the referring center to the secretary of the Department of Neurology or Neurosurgery in BTCA, or (2) through telephone or e-mail consultation with a neuro-oncologist or neurosurgeon on call, followed by an interfacility admission transfer or a referral via pathway 1. The imaging was frequently sent separately on a CD-ROM through mail or a secured weblink. When all data were received, a neurologist or neurosurgeon of the addressed specialty triaged the patient, and an appointment at the addressed outpatient clinic or an interfacility admission transfer was made (Figure 1A). In case of urgent referral, incomplete imaging data were sometimes requested to be sent ahead by e-mail. The complete imaging data were then sent by express courier. After examination of the patient at BTCA, patients were discussed in the neuro-oncological tumor board meeting (TBM) twice a week to determine the diagnosis and personalized treatment plan including neurosurgery, radiotherapy, and chemotherapy or best supportive care. Prior to the quality improvement initiative, all patients were referred according to SR.
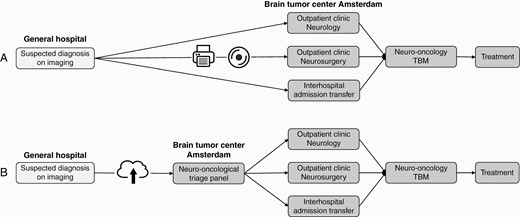
Referral pathways. (A) Pathway of the standard referral. (B) Pathway of NOTP referral. Abbreviations: NOTP, neuro-oncological triage panel; TBM, tumor board meeting.
Quality Improvement Initiative: Neuro-Oncological Triage Panel
In collaboration with the referring hospitals in the Amsterdam region, digital referral to a multidisciplinary NOTP was developed to improve the SR pathway, to facilitate access to neuro-oncological care, and to avoid delay in referrals, as part of the Moving towards Regional Oncology Networks program of the Dutch Ministry of Health, Welfare and Sport.23
Referral of a patient with suspected neuro-oncological disease to the NOTP included the following steps: (1) the referring neurologist acquired patient’s informed consent to transfer medical information and imaging to BTCA, (2) the referring neurologist collected the required patient information for the registration form (see Supplementary Figure S1), (3) the referring neurologist uploaded the completed registration form and imaging on the digital data sharing platform EVOCS® (Fysicon BV, Oss, the Netherlands, part of Canon Medical Systems Corporation, Ōtawara, Tochigi, Japan), (4) the panelists of the NOTP, consisting of a neurologist, neurosurgeon and neuroradiologist with expertise in neuro-oncology, received an e-mail notification when a new referral was uploaded, (5) 3 times per week the panelists met to reach consensus on the radiological differential diagnosis and consultation advice, (6) within 2 working days, the final conclusion including revision of imaging and an appointment at the outpatient clinic of the preferred specialist for consultation (neurologist or neurosurgeon) or interfacility admission transfer was sent to the referring neurologist (Figure 1B). In cases of ambiguity about the performance status, patients were referred to the outpatient clinic neurology. The workflow was not considered suitable for emergency referrals.
The NOTP meeting was planned and integrated into a preexisting neuroradiology meeting, in which neurosurgeons and neuro-radiologists already participated 3 times a week. Since the implementation of the NOTP, neurologists have alternately participated in the meeting in cases of new referrals. Safety and privacy aspects of e-consultation were previously examined and published.24 EVOCS® was contracted as a secured online data-sharing platform with a pay-per-view license to share patient information and diagnostic imaging between participating centers in the region. All participants received login codes to access the platform. The registration form was developed prior to the start of the NOTP in order to receive all essential information to be able to discuss the patient case and provide a substantiated advice. Invitational meetings were organized prior to the start of the NOTP to inform the referring neurologists. During these meetings, procedures were defined and neurologists and residents were trained to share data.
Implementation
The NOTP was implemented in hospitals in 3 phases to evaluate and optimize the workflow before further regional expansion. In the first implementation phase, 3 general hospitals were connected to the EVOCS®-network and the neurologists of these centers could digitally refer patients to the NOTP. On March 19, 2019, the first patient was referred digitally. After 6 months, the workflow and satisfaction of the participating centers were evaluated via site visits. After evaluation, minor modifications were made to the registration form. In the second implementation phase between January and February 2020, digital access to the NOTP was expanded to 2 other general hospitals. In the third implementation phase since November 2020, extension to another 3 hospitals is in progress. Digital referral to the NOTP was encouraged in the participating centers, however, conventional referral according to the SR pathway remained feasible. The referral pathway of choice was at referring neurologist’s discretion.
Study Design
Between February 1, 2019 and March 16, 2020, a prospective cohort study was conducted to evaluate the effects of the NOTP referral in comparison with SR. We included all newly diagnosed patients referred to the BTCA and were discussed in the neuro-oncological TBM. Patients with a deviant workup were excluded from analysis (Figure 2). The included patients were categorized according to the referral pathway into 2 groups: (1) SR as control group, (2) NOTP referral as intervention group. The revised Standards for QUality Improvement Reporting Excellence (SQUIRE) guidelines were used to report the implementation of the quality improvement initiative and the executed study.25
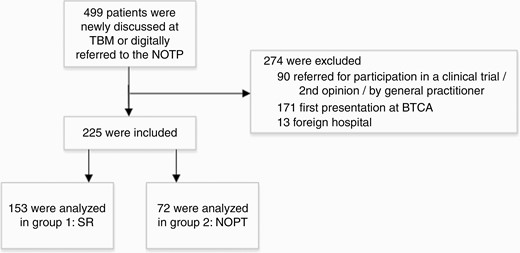
Flowchart of patient selection. Abbreviations: BTCA, Brain Tumor Center Amsterdam; NOTP, neuro-oncological triage panel; TBM, tumor board meeting.
Outcome Measures
Baseline characteristics comprised patient and tumor characteristics and were collected from the referral letters and medical records. The primary outcome measures were lead times. Three lead times were considered: (1) time-to-referral, defined as the time between the date of the first scan and the date of receiving the referral letter, (2) time-to-treatment, defined as the time between the date of receiving the referral letter and the date of start of treatment, (3) total time, defined as the time between date of the first scan and the date of start of treatment. The start of treatment was defined as the date of first treatment (date of surgery, first radiation, or first chemotherapy) or the date at which the decision was made with the patient to not undergo treatment, such as a wait and scan policy, the postponement of treatment on the patient’s request, treatment to be conducted elsewhere, or best supportive care.
The secondary outcome measures were costs of information exchange and time investments by the health care professionals. Costs were defined as costs of imaging transfer, on CD-ROM by standard and urgent mail or via EVOCS®. Cost prices were obtained from the central mail department of participating hospitals. Time investments were defined as the mean of estimated time investment per activity of participating medical specialists and secretaries and were obtained per interview.
Statistical Analysis
SRs were compared with NOTP referrals. Normally distributed continuous baseline characteristics were reported as mean and standard deviation [SD] and compared using independent t tests. Categorical baseline characteristics were reported as numbers and percentages and compared using chi-square tests. Lead times were described as median (interquartile range [IQR]) and compared between the 2 groups using Mann-Whitney U tests because the outcome distributions did not follow a normal distribution. We separately analyzed treatment strategy (treatment vs no treatment). A P value of <.05 was considered to be statistically significant. Statistical analysis of data was performed using IBM® SPSS® Statistics 26.0 software (SPSS Inc., Chicago, IL, USA).
Ethical Considerations
The study was conducted in the context of the Healthcare Quality, Complaints and Disputes Act with approval of the heads of Departments of Neurology and Neurosurgery. Afterwards, ethical approval was granted by the Medical Ethics Review Committee of Amsterdam UMC location VUmc (METc VUmc 2019.584).
Results
Referral Patterns and Triage
Out of 82 TBMs, 225 referred patients fulfilled the inclusion criteria, of whom 153 had a standard and 72 had an NOTP referral (Figure 2). The baseline characteristics of the patients were not significantly different between the 2 groups (Table 1). Focal neurological deficit was the most frequent first symptom in both groups. High-grade glioma, brain metastases, meningioma, and primary brain tumor-not-specified were the most frequent diagnoses at referral in both groups. After revision of imaging and discussion in either the NOTP or the neuro-oncology TBM, the suspected diagnosis was changed in 19 (26.4%) digitally referred patients and in 40 (26.1%) standardly referred patients (P > .05). In 12 triage patients and 11 standardly referred patients, this adjustment within suspected diagnosis had an impact on further diagnostic workup or treatment. The following advices were given after discussion in the NOTP: first consultation at outpatient clinic neurology (n = 20, 27.8%), first consultation at outpatient clinic Neurosurgery (n = 21, 29.2%), a combined first consultation at the outpatient clinic Neurology and Neurosurgery (n = 6, 8.3%), interfacility admission transfer (n = 12, 16.7%) and no referral (n = 10, 13.9%). Motivations for no referral were no suspicion of neuro-oncological disease (n = 1), treatment in other multidisciplinary team advised (n = 4), and best supportive care by the referring neurologist (n = 5). Outpatient clinic visits were prevented in these patients. Three patients with panel’s advice for neurosurgical referral were not eligible for surgery after assessment at the outpatient clinic as Karnofsky Performance Score (KPS) was worse than assumed based on available patient information. Three digitally referred patients required an urgent interfacility admission transfer and were not discussed in the NOTP. In the outpatient clinic referrals, triage patients were more frequently referred for first neurosurgical consultation (SR = 28.8% vs NOTP = 44.7%) and for a combined neurological and neurosurgical consultation (SR = 2.5% vs NOTP = 12.8%) compared to standardly referred patients, and less frequently for first neurological consultation (SR = 68.6% vs NOTP = 42.6%, P = .002). Interfacility admission transfers did not differ between the 2 groups (SR 22.9% vs NOTP 24.2%, P = .860).
| . | SR . | NOTP . | P . |
|---|---|---|---|
| . | n = 153 (%) . | n = 72 (%) . | . |
| Age (yr, SD) | 60.3 (15.1) | 63.0 (15.3) | .220 |
| Female | 75 (49.0) | 42 (58.3) | .201 |
| Presenting symptoms | |||
| Focal neurological deficit | 44 (28.8) | 29 (40.3) | |
| Cognitive decline/behavioral changes | 30 (19.6) | 13 (18.1) | |
| Seizure | 25 (16.3) | 13 (18.1) | .329 |
| Headache | 15 (9.8) | 6 (8.3) | |
| Falls | 8 (5.2) | 5 (6.9) | |
| Incidental finding | 12 (7.8) | 3 (4.2) | |
| Other | 19 (12.4) | 3 (4.2) | |
| Karnofsky performance score | |||
| <70 | 27 (17.6) | 18 (25.0) | .190 |
| ≥70 | 126 (82.4) | 54 (75.0) | |
| Corticosteroid use | 53 (34.6) | 22 (30.6) | .214 |
| History of oncological disease | 26 (17.0) | 13 (18.1) | .852 |
| Suspected diagnosis by referring neurologist | |||
| Primary brain tumor NS | 44 (28.8) | 14 (19.4) | |
| Meningioma | 37 (24.2) | 10 (13.9) | |
| High-grade glioma | 37 (24.2) | 17 (23.6) | |
| Metastases | 16 (10.5) | 16 (22.2) | .06 |
| Low-grade glioma | 6 (3.9) | 6 (8.3) | |
| CNS lymphoma | 6 (3.9) | 6 (8.3) | |
| Spine tumor | 5 (3.3) | 3 (4.2) | |
| Pituitary tumor | 2 (1.3) | 0 |
| . | SR . | NOTP . | P . |
|---|---|---|---|
| . | n = 153 (%) . | n = 72 (%) . | . |
| Age (yr, SD) | 60.3 (15.1) | 63.0 (15.3) | .220 |
| Female | 75 (49.0) | 42 (58.3) | .201 |
| Presenting symptoms | |||
| Focal neurological deficit | 44 (28.8) | 29 (40.3) | |
| Cognitive decline/behavioral changes | 30 (19.6) | 13 (18.1) | |
| Seizure | 25 (16.3) | 13 (18.1) | .329 |
| Headache | 15 (9.8) | 6 (8.3) | |
| Falls | 8 (5.2) | 5 (6.9) | |
| Incidental finding | 12 (7.8) | 3 (4.2) | |
| Other | 19 (12.4) | 3 (4.2) | |
| Karnofsky performance score | |||
| <70 | 27 (17.6) | 18 (25.0) | .190 |
| ≥70 | 126 (82.4) | 54 (75.0) | |
| Corticosteroid use | 53 (34.6) | 22 (30.6) | .214 |
| History of oncological disease | 26 (17.0) | 13 (18.1) | .852 |
| Suspected diagnosis by referring neurologist | |||
| Primary brain tumor NS | 44 (28.8) | 14 (19.4) | |
| Meningioma | 37 (24.2) | 10 (13.9) | |
| High-grade glioma | 37 (24.2) | 17 (23.6) | |
| Metastases | 16 (10.5) | 16 (22.2) | .06 |
| Low-grade glioma | 6 (3.9) | 6 (8.3) | |
| CNS lymphoma | 6 (3.9) | 6 (8.3) | |
| Spine tumor | 5 (3.3) | 3 (4.2) | |
| Pituitary tumor | 2 (1.3) | 0 |
Abbreviations: CNS lymphoma, central nervous system lymphoma; NOTP, neuro-oncological triage panel; NS, not specified; SR, standard referral.
| . | SR . | NOTP . | P . |
|---|---|---|---|
| . | n = 153 (%) . | n = 72 (%) . | . |
| Age (yr, SD) | 60.3 (15.1) | 63.0 (15.3) | .220 |
| Female | 75 (49.0) | 42 (58.3) | .201 |
| Presenting symptoms | |||
| Focal neurological deficit | 44 (28.8) | 29 (40.3) | |
| Cognitive decline/behavioral changes | 30 (19.6) | 13 (18.1) | |
| Seizure | 25 (16.3) | 13 (18.1) | .329 |
| Headache | 15 (9.8) | 6 (8.3) | |
| Falls | 8 (5.2) | 5 (6.9) | |
| Incidental finding | 12 (7.8) | 3 (4.2) | |
| Other | 19 (12.4) | 3 (4.2) | |
| Karnofsky performance score | |||
| <70 | 27 (17.6) | 18 (25.0) | .190 |
| ≥70 | 126 (82.4) | 54 (75.0) | |
| Corticosteroid use | 53 (34.6) | 22 (30.6) | .214 |
| History of oncological disease | 26 (17.0) | 13 (18.1) | .852 |
| Suspected diagnosis by referring neurologist | |||
| Primary brain tumor NS | 44 (28.8) | 14 (19.4) | |
| Meningioma | 37 (24.2) | 10 (13.9) | |
| High-grade glioma | 37 (24.2) | 17 (23.6) | |
| Metastases | 16 (10.5) | 16 (22.2) | .06 |
| Low-grade glioma | 6 (3.9) | 6 (8.3) | |
| CNS lymphoma | 6 (3.9) | 6 (8.3) | |
| Spine tumor | 5 (3.3) | 3 (4.2) | |
| Pituitary tumor | 2 (1.3) | 0 |
| . | SR . | NOTP . | P . |
|---|---|---|---|
| . | n = 153 (%) . | n = 72 (%) . | . |
| Age (yr, SD) | 60.3 (15.1) | 63.0 (15.3) | .220 |
| Female | 75 (49.0) | 42 (58.3) | .201 |
| Presenting symptoms | |||
| Focal neurological deficit | 44 (28.8) | 29 (40.3) | |
| Cognitive decline/behavioral changes | 30 (19.6) | 13 (18.1) | |
| Seizure | 25 (16.3) | 13 (18.1) | .329 |
| Headache | 15 (9.8) | 6 (8.3) | |
| Falls | 8 (5.2) | 5 (6.9) | |
| Incidental finding | 12 (7.8) | 3 (4.2) | |
| Other | 19 (12.4) | 3 (4.2) | |
| Karnofsky performance score | |||
| <70 | 27 (17.6) | 18 (25.0) | .190 |
| ≥70 | 126 (82.4) | 54 (75.0) | |
| Corticosteroid use | 53 (34.6) | 22 (30.6) | .214 |
| History of oncological disease | 26 (17.0) | 13 (18.1) | .852 |
| Suspected diagnosis by referring neurologist | |||
| Primary brain tumor NS | 44 (28.8) | 14 (19.4) | |
| Meningioma | 37 (24.2) | 10 (13.9) | |
| High-grade glioma | 37 (24.2) | 17 (23.6) | |
| Metastases | 16 (10.5) | 16 (22.2) | .06 |
| Low-grade glioma | 6 (3.9) | 6 (8.3) | |
| CNS lymphoma | 6 (3.9) | 6 (8.3) | |
| Spine tumor | 5 (3.3) | 3 (4.2) | |
| Pituitary tumor | 2 (1.3) | 0 |
Abbreviations: CNS lymphoma, central nervous system lymphoma; NOTP, neuro-oncological triage panel; NS, not specified; SR, standard referral.
Lead Times
Referral to the NOTP was associated with a statistically significant decrease in median time-to-referral and total time (Figure 3A). Median total time was 15 days (IQR: 12-38.25) for patients referred to the NOTP in comparison with 27 days (IQR: 14-48) for patients referred through the standard pathway (P = .040). The effect of the NOTP was mainly observed in expediting the time-to-referral. Median lead time from first scan to referral was reduced from 6 days (IQR: 1.5-10) to 1 day (IQR: 0.25-4) (P < .001). Median time-to-treatment did not reduce significantly after implementation of the NOTP (P = .324). In subanalyses on treatment strategies (treatment and no treatment), differences in time-to-referral in both subgroups were observed in favor of the NOTP (Figure 3B). No statistically significant differences in time-to-treatment and total time were observed when taking treatment strategies into account.
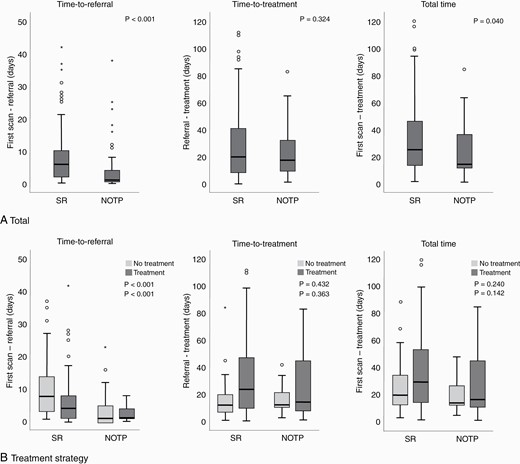
Lead times. Abbreviations: NOTP, neuro-oncological triage panel; SR, standard referral; οoutlyer; *extreme outlier.
Time Investment and Costs
The overall estimated time investment of the digital referral pathway and the SR pathway were comparable (60 vs 65-75 minutes) (Table 2). The time effort of the referring neurologist was slightly increased in the digital referral system (7 vs 5 minutes). The time effort for the consultant neurologist was reduced in the NOTP with respect to the SR (3 vs 5-15 minutes). The estimated costs of the digital referral system were comparable to SR (Table 2).
| Staff/Activity . | Time Estimate (min) . | Costs (Eur) . |
|---|---|---|
| Digital referral to NOTP | ||
| Fill in the registration form by referring neurologist | 5 | |
| Upload patient case in EVOCS® by referring neurologist | 2 | |
| Send imaging via EVOCS® | 10 | 8.41/scana |
| Import patient case in electronic health record by secretary | 30 | |
| Discussion in NOTP | 3 | |
| Write advisory report with panel advice | 10 | |
| Scheduling outpatient clinic appointment by hospital secretary | 10 | |
| Total time | 60 | |
| Standard referral | ||
| Writing the referral letter by referring neurologist | 5 | |
| Secretary referring hospital | 15 | |
| Send imaging via mail | 0-2 days | 20.50/CD-ROM (standard) 29.50-49.50/CD-ROM (urgent) |
| Import referral letter and imaging by hospital secretary | 30 | |
| Triage by neurologist/neurosurgeon | 5-15 | |
| Scheduling outpatient clinic appointment by hospital secretary | 10 | |
| Total time | 65-75 |
| Staff/Activity . | Time Estimate (min) . | Costs (Eur) . |
|---|---|---|
| Digital referral to NOTP | ||
| Fill in the registration form by referring neurologist | 5 | |
| Upload patient case in EVOCS® by referring neurologist | 2 | |
| Send imaging via EVOCS® | 10 | 8.41/scana |
| Import patient case in electronic health record by secretary | 30 | |
| Discussion in NOTP | 3 | |
| Write advisory report with panel advice | 10 | |
| Scheduling outpatient clinic appointment by hospital secretary | 10 | |
| Total time | 60 | |
| Standard referral | ||
| Writing the referral letter by referring neurologist | 5 | |
| Secretary referring hospital | 15 | |
| Send imaging via mail | 0-2 days | 20.50/CD-ROM (standard) 29.50-49.50/CD-ROM (urgent) |
| Import referral letter and imaging by hospital secretary | 30 | |
| Triage by neurologist/neurosurgeon | 5-15 | |
| Scheduling outpatient clinic appointment by hospital secretary | 10 | |
| Total time | 65-75 |
Abbreviations: Eur, Euro; NOTP, neuro-oncological triage panel.
aOn average, 2-3 scans per patient were sent.
| Staff/Activity . | Time Estimate (min) . | Costs (Eur) . |
|---|---|---|
| Digital referral to NOTP | ||
| Fill in the registration form by referring neurologist | 5 | |
| Upload patient case in EVOCS® by referring neurologist | 2 | |
| Send imaging via EVOCS® | 10 | 8.41/scana |
| Import patient case in electronic health record by secretary | 30 | |
| Discussion in NOTP | 3 | |
| Write advisory report with panel advice | 10 | |
| Scheduling outpatient clinic appointment by hospital secretary | 10 | |
| Total time | 60 | |
| Standard referral | ||
| Writing the referral letter by referring neurologist | 5 | |
| Secretary referring hospital | 15 | |
| Send imaging via mail | 0-2 days | 20.50/CD-ROM (standard) 29.50-49.50/CD-ROM (urgent) |
| Import referral letter and imaging by hospital secretary | 30 | |
| Triage by neurologist/neurosurgeon | 5-15 | |
| Scheduling outpatient clinic appointment by hospital secretary | 10 | |
| Total time | 65-75 |
| Staff/Activity . | Time Estimate (min) . | Costs (Eur) . |
|---|---|---|
| Digital referral to NOTP | ||
| Fill in the registration form by referring neurologist | 5 | |
| Upload patient case in EVOCS® by referring neurologist | 2 | |
| Send imaging via EVOCS® | 10 | 8.41/scana |
| Import patient case in electronic health record by secretary | 30 | |
| Discussion in NOTP | 3 | |
| Write advisory report with panel advice | 10 | |
| Scheduling outpatient clinic appointment by hospital secretary | 10 | |
| Total time | 60 | |
| Standard referral | ||
| Writing the referral letter by referring neurologist | 5 | |
| Secretary referring hospital | 15 | |
| Send imaging via mail | 0-2 days | 20.50/CD-ROM (standard) 29.50-49.50/CD-ROM (urgent) |
| Import referral letter and imaging by hospital secretary | 30 | |
| Triage by neurologist/neurosurgeon | 5-15 | |
| Scheduling outpatient clinic appointment by hospital secretary | 10 | |
| Total time | 65-75 |
Abbreviations: Eur, Euro; NOTP, neuro-oncological triage panel.
aOn average, 2-3 scans per patient were sent.
Discussion
This study shows that implementation of digital referral through a multidisciplinary NOTP in our region improved referral management by (1) providing standardized patient information together with diagnostic imaging and by (2) reducing lead times, without increasing the costs of information exchange and health care professionals’ time effort. Discussion of patients in the triage panel resulted in an expedited advice to the referring neurologist and patient, and patient-tailored referrals including prevention of extra outpatient clinic visits.
To our knowledge, this study was the first quality improvement initiative in the field of neuro-oncological care that improved referral management with an online imaging platform and triage panel. Previous studies have demonstrated the beneficial effects of triage systems on lead times in various oncological and elective care pathways.21,22,26–29 Common et al implemented a Thoracic Triage Panel to expedite lung cancer diagnosis and treatment initiation.21 They reported a reduction in median lead time from first abnormal imaging to biopsy from 61.5 to 36 days and to treatment initiation from 118.0 to 80.0 days. Patterson et al realized an e-mail triage panel to optimize general practitioner referrals to the neurologist.22 With e-mail triage, lead time decreased from 72 weeks to 4 weeks. Besides reduced lead times to referral and treatment, the NOTP has expedited the evaluation by a radiologist with expertise in neuro-oncology. The diagnosis differed in a quarter of all patients after the assessment of an expert radiologist. In standard care, patients are discussed at the TBM after the first appointment. Since patients in the NOTP group are discussed prior to their first appointment and time-to-referral has reduced, the NOTP could also expedite the time-to-diagnosis. Overall, despite the wide variety of (oncological) diseases and the heterogeneity of design, triage panels appear to be effective in improving timelines of care.
Timely and appropriate referrals need attention because prolonged lead times could affect emotional distress, and impair treatment outcome and survival. In the diagnostic phase of cancer, emotional distress is an established major burden in patients confronted with the suspicion of oncological disease.11,12 Brain tumor patients have an increased level of distress due to the neurological deficit and the poor prognosis.13,14 There is a lack of literature on the effect of referral time on emotional distress among brain tumor patients. In the field of lung cancer care, however, Brocken et al reported that an expedited diagnostic evaluation had a positive effect on distress of patients with suspected lung carcinoma.8 Despite emotional distress was not taking into account as outcome measure in this study, we believe that reduced timings could positively affect emotional burden in brain tumor patients. Besides the effect on emotional distress, prolonged lead times could also affect the treatment outcome and survival in cancer patients.30–32 However, the exact impact of lead times on outcome and survival in neuro-oncological care remains unclear since the available literature is limited. Although, 1 study demonstrated that earlier diagnosis was associated with a worse overall survival in patients with a grade IV malignant brain tumor.33 Their findings were explained by tumor biology since phenotype influences the type, frequency, and severity of patient’s symptoms. An aggressive phenotype is more likely to induce a more rapid progression of symptoms. Another study showed that expedited lead time to surgical treatment was associated with improved survival in patients with a grade IV malignant brain tumor who presented with seizures and no other symptoms.10 Nevertheless, more research on this topic needs to be undertaken before the association between lead times and emotional distress, treatment outcome, and survival in patients with a brain tumor is more clearly understood.
Digital availability of the information infrastructure for referrals was an unanticipated benefit for the demands during the coronavirus disease 2019 (COVID-19) outbreak. The recent pandemic has led to interruption or delay in the treatment of patients with neuro-oncological disease since elective medical care has been necessarily de-prioritized to meet the demands of this pandemic.34,35 During this public health crisis, the physical outpatient access was significantly curtailed and video-/teleconsultation became essential.36 Referral to the triage panel contributed to a multidisciplinary treatment advice balanced on the acuity of medical needs with available resources, to prioritize patient cases, and to select appropriate patients for outpatient clinic access. The triage panel has continued with minor modifications since the pandemic, for example, participation of a radiation oncologist in the panel. Referral to the NOTP comprised half of all neuro-oncological referrals during this period. However, in the face of this unprecedented situation with judicious use of health care resources and subsequent change in patient journeys, this period was not included in the currently reported analyses.
The strengths of this quality improvement initiative are the fit in daily practice and the potential for future care, specifically in terms of sustainability and generalizability. First, the NOTP meeting was included in a preexisting neuroradiology meeting, so the panelists’ time efforts were minimalized and in line with daily activities. Second, despite the cooperation with EVOCS® as the secured online platform for this project, digital patient data sharing across health care facilities by HIE will be available and operating in health care facilities in the Netherlands soon. HIE enables access to and exchange of patient data and imaging across all departments of health care facilities after patients’ informed consent.37,38 This could support regional and national collaboration between hospitals in oncological and non-oncological care without project funding. Moreover, developments in global deployment of HIE have taken place.39–43 Despite the wide range in degree of implementation and efficacy between countries, HIE provides opportunities to optimize referral management worldwide. Therefore, we aimed to provide a helpful blueprint for online consultation of the triage panel that is generalizable to multidisciplinary oncological and non-oncological referral pathways.
Several lessons were learned from this project and they include the indispensability of telephone consultation, the unsuitability for emergency referrals after regular working hours, and the necessity of information and communication technology (ICT) cooperation. First, telephone consultation could be important to provide diagnostic and treatment advices in anticipation of the panel’s advice and in transferring patient cases in need of urgent referral. For example, cases with suspicion of a central nervous system lymphoma or glioblastoma with severe and quickly neurological deterioration may require an immediate interfacility admission transfer for accelerated additional diagnostics or intervention. In order to facilitate emergent referrals, the urgency of referral (including a reference to the telephone numbers of the neurologist and neurosurgeon on call for referrals within 24 hours) is included in the registration form. Nevertheless, in a few cases in this study, high urgent referrals were online registered without notifying the neurologist or neurosurgeon on call. Second, digital uploading of imaging was not suitable for emergency consultation and urgent interfacility admission transfers after regular working hours as the import of the imaging in the Picture Archiving and Communication System (PACS) of the BTCA could not be accomplished due to logistic considerations. Nevertheless, NOTP referrals could be digitally uploaded by the referring neurologists after regular working hours and are processed the following working day. Finally, implementation of EVOCS® could not be achieved in all referring hospitals because the implementation of Cross-enterprise Document Sharing (XDS, Forcare, Philips Healthcare, Eindhoven, the Netherlands) interfered. In 1 participating hospital, the restart of EVOCS® was disturbed after the disconnection of the PACS. Through the implementation of XDS, access to the NOTP will be enlarged. Ideally, or maybe even necessary, the same HIE system is used nationally (or even worldwide). Therefore, the anticipation of available digital exchange systems is recommended for future projects.
Limitations of the present study included potential selection bias and allocation bias of patients referred to the NOTP. Digital referral was accessible for the 3 partnering referring hospitals in the first implementation phase. The neurology staff and residents of these hospitals received login codes for online access to register patient cases and were aware of the quality improvement initiative. This could positively affect lead times. In addition, a few patients from these hospitals were referred according to the SR pathway after the implementation of the triage panel. The distribution among both groups may therefore be influenced. However, patient and tumor characteristics between the intervention and control groups did not differ significantly. Explanations could be the turnover of residents and referrals conducted by the secretaries in the referring hospitals. Therefore, regular training and informing the referring partners is essential to maintain digital referral. In future, the ultimate goal is to achieve digital access to the triage panel regardless of the hospital of diagnosis.
In conclusion, we have shown that the implementation of digital referral to a multidisciplinary NOTP in neuro-oncological care was feasible and valuable. The panel improved referral management by digital transfer of patient information, patient-tailored referrals, and a reduction in lead times. This blueprint is generalizable to other care processes in neuro-oncological care that require the collaboration and coordination of multiple medical specialties. Future studies evaluating the effects of the triage panel on emotional distress, treatment outcome, and survival are suggested.
Funding
This work was supported by Dutch Organization for Health Research and Development (ZonMw), as part of the Moving towards Regional Oncology Networks program (grant: Citrien Fund (Citrienfonds), project number 839205003).
Conflict of interest statement. The authors declare that there is no conflict of interest, besides the governmental funding of the project.




