-
PDF
- Split View
-
Views
-
Cite
Cite
Quinn T Ostrom, Di Lu, Rong Lu, Matthew C Baker, Prevalence of autoimmunity and atopy in US adults with glioblastoma and meningioma, Neuro-Oncology, Volume 24, Issue 10, October 2022, Pages 1807–1809, https://doi.org/10.1093/neuonc/noac145
Close - Share Icon Share
Atopic disease and autoimmunity arise due to aberrant immune function and are present in ~40% and ~10% of the US population, respectively.1,2 Prior research has identified significant protective associations between respiratory allergies and glioma, the most common type of malignant brain tumor, as well as suggestive protective associations between autoimmunity and glioma.3,4 The association between risk of meningioma, the most common type of nonmalignant brain tumor, and any atopic or autoimmune conditions has been mixed in prior studies.3,4 In this retrospective case–control study, we used insurance claims data to estimate the relative prevalence of prediagnostic atopic and autoimmune conditions in a large cohort of US adults.
This study was conducted using the Clinformatics® Data Mart Database (MN), a de-identified database derived from a large adjudicated claims data warehouse, under a protocol approved by the Stanford University Institutional Review Board5. Glioblastoma cases were defined by individuals ≥18 years of age diagnosed with glioblastoma (ICD-9 codes 191.0–191.9 or ICD-10 codes C71.0-C71.9), who had received at least one prescription for temozolomide with at least 3 years of continuous enrollment from December 5, 2003 to December 6, 2020. Individuals with meningioma (ICD-9 codes 192.1, 192.3, 225.2, 225.4, and 237.6 or ICD-10 codes C70.0–C70.9, D32.0, D32.1, D32.9, D42.0, D42.1, and D42.9) with at least 3 years of continuous enrollment were matched to glioblastoma cases using a propensity score in a 1:1 ratio based on age, sex, race, Charlson Comorbidity Index,6 follow-up time, and enrollment start year. Atopic conditions (including allergies, eczema, and asthma) and autoimmune conditions were defined using ICD-9/ICD-10 codes used at least 6 months prior to diagnosis of glioblastoma or meningioma. The outcomes were compared using the chi-squared or Fisher’s exact test, as appropriate. All analyses were performed in SAS version 9.4 (SAS Institute).
Out of 66,228,181 total individuals in the cohort, 17,348 were identified as having a malignant brain tumor with at least 3 years of enrollment. Out of these, 4,286 individuals (24.7%) met the treatment inclusion criteria for glioblastoma during the period. There were 22,812 identified meningioma cases before matching. Prior to matching, glioblastoma cases were younger and more likely to be male and white as compared to meningioma (Figure 1A).
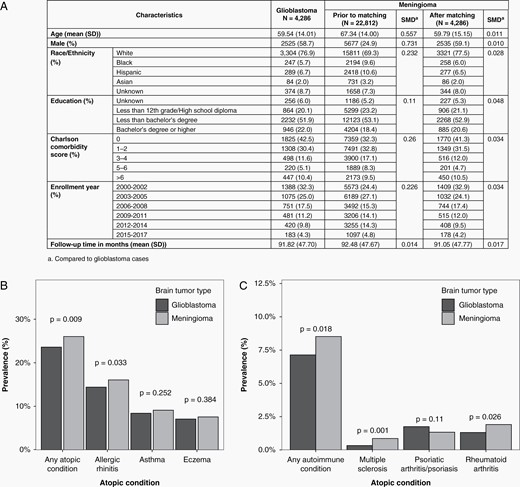
(A) Characteristics of included patients, and frequency of (B) atopic and (C) autoimmune conditions by brain tumor type.
Atopic conditions were more common in individuals with meningioma as compared to glioblastoma (26.04% vs 23.61%, P = 0.009) (Figure 1B). All atopic conditions occurred more frequently in meningioma cases than glioblastoma cases. The most common atopic condition was allergic rhinitis, which was identified in 16.08% of meningioma cases and 14.42% of glioblastoma cases (P = 0.033).
Autoimmune conditions were present in 8.52% of meningioma cases and 7.14% of glioblastoma cases (P = 0.018) (Figure 1C). The most common autoimmune condition was rheumatoid arthritis (1.91% of meningioma cases and 1.31% of glioblastoma cases, P = 0.026). Though rare overall, multiple sclerosis was identified in a higher proportion of meningioma cases (0.86%) as compared to glioblastoma cases (0.33%, P = 0.001). While most autoimmune conditions had higher prevalence in meningioma case as compared to glioblastoma cases, psoriasis/psoriatic arthritis was more frequently identified in individuals with glioblastoma (1.75% of glioblastoma cases and 1.33% of meningioma cases, P = 0.110).
Overall, prevalence of atopic disease and autoimmunity in glioblastoma and meningioma cases was lower than what has previously been observed in the general population. All atopic conditions, and most autoimmune conditions, occurred less frequently in individuals with glioblastoma as compared to those with meningioma. The results of this study support prior research demonstrating that atopy and autoimmunity may play a protective role against the development of a primary brain tumor, and that this protective effect may be stronger in glioblastoma as compared to meningioma.
Acknowledgments
Data for this project were accessed using the Stanford Center for Population Health Sciences Data Core. The PHS Data Core is supported by a National Institutes of Health (NIH) National Center for Advancing Translational Science Clinical and Translational Science Award (UL1 TR001085) and from Internal Stanford funding. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH. We thank John Jarve and Jacque Jarve for their generous support of immunology and rheumatology clinical research at Stanford University.
Funding
This manuscript is partially supported by the Biostatistics Shared Resource (BSR) of the NIH-funded Stanford Cancer Institute: P30CA124435. Additional funding provided by P50CA190991 (QTO).
Conflict of interest statement. None declared.
Authorship statement. Conceptualization: Q.T.O. and M.C.B.; data curation: D.L.; formal analysis: D.L.; methodology: D.L. and R.L.; project administration: M.C.B.; resources: M.C.B.; supervision: M.C.B.; visualization: Q.T.O.; writing—original draft: Q.T.O.; and writing—review and editing: Q.T.O., D.L., R.L., and M.C.B.
References
Stanford Center for Population Health Sciences. Optum SES (v4.0). Redivis. (Dataset). 2021. Accessed March 24, 2022. https://doi.org/10.57761/bykd-vz30.




