-
PDF
- Split View
-
Views
-
Cite
Cite
Camille Lanaret, Dany Anglicheau, Audard Vincent, Celine Lambert, Lionel Couzi, Matthias Buchler, Sophie Ohlmann, Dominique Bertrand, Rérolle Jean-Philippe, Antoine Thierry, Nicolas Maillard, Betoul Schvartz, Leonard Golbin, Vincent Pernin, Didier Ducloux, Nicolas Bouvier, Coralie Poulain, Anne Elisabeth Heng, Clarisse Greze, Paolo Malvezzi, Frank Martinez, Nassim Kamar, Cyril Garrouste, P1757
RITUXIMAB FOR RECURRENCE OF PRIMARY FOCAL SEGMENTAL GLOMERULOSCLEROSIS AFTER KIDNEY TRANSPLANTATION: RESULTS OF A NATIONWIDE STUDY, Nephrology Dialysis Transplantation, Volume 35, Issue Supplement_3, June 2020, gfaa142.P1757, https://doi.org/10.1093/ndt/gfaa142.P1757Close - Share Icon Share
Abstract
The indication of rituximab (RTX) in the treatment of primary focal segmental glomerulosclerosis (FSGS) recurrence after kidney transplantation (KT) remains controversial. The objective of our study was to evaluate the benefit and tolerability of adding RTX to the standard of care (SOC) comprising plasmapheresis (PP), corticosteroids, and high-dose anticalcineurins for the treatment of FSGS recurrence after KT.
This retrospective, multicenter study reports on 148 patients, transplanted between 31 December 2004 and 31 December 2018, aged 39.9 + 13.4 years, who developed FSGS recurrence at 7 [3–23] days. In all 109 patients received a SOC (Group 1). RTX was introduced in this group after more than 28 days of SOC for failure or for therapeutic intensification (n = 19, Group 1a), or for early discontinuation of PP (n = 12, Group 1b); 39 patients received RTX associated at the outset with SOC (Group 2).
We observed 46.6% complete remission (CR) and 33.1% partial remission (PR). Ten-year graft survival was 65.6% [51.4–76.6] and 13.4% [3.4–30.0] in responders and non-responders respectively. There was no difference in CR + PR rate between G1 (82.5%) and G2 (71.8%), p = 0.08, confirmed by propensity score +4.3% (95% CI [−9.0%-17.5%], p = 0.53). Following addition of RTX (Group 1a), we observed a CR rate of 26.3% and a PR rate of 31.6%. Patients with and without RTX experienced similar rejection rates (18.6% and 28.2%, p = 0.17) and infection rates (71.4% and 79.5%, p = 0.40). In multivariate analysis, the infections were associted with hypogammaglobulinemia <5g/l (OR = 8.04, 95% CI [1.65,39.25], p = 0.01).
Rituximab could be used in cases of SOC failure or in remission patients for early weaning of plasmapheresis, without increasing infectious risk.
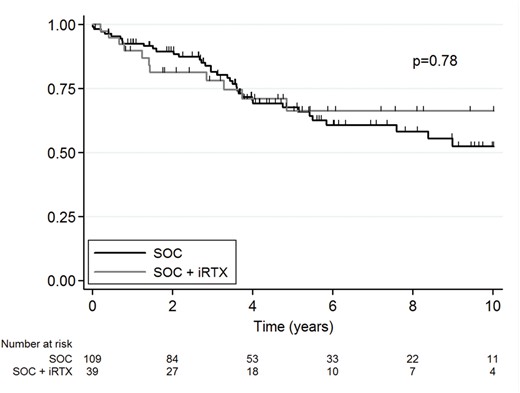
Figure1 Allograft survival rate after SOC (black line) or immediate rituximab in addition to SOC (grey line) for recurrence of FSGS.
Abbreviations: iRTX, immediate Rituximab ; SOC standard of care
- renal transplantation
- adrenal corticosteroids
- glucocorticoids
- focal glomerulosclerosis
- graft survival
- plasmapheresis
- rejection (psychology)
- survival rate
- weaning
- infections
- mineralocorticoids
- rituximab
- hypogammaglobulinemia
- study report
- standard of care
- allografting
- complete remission
- disease remission
- partial response





Comments