-
PDF
- Split View
-
Views
-
Cite
Cite
Colleen Meaney, Matthew Perdue, Mohamad Umar, Jerimiah Walker, Hydrofluoric Acid, an Unexpected Surprise, Military Medicine, Volume 188, Issue 7-8, July/August 2023, Pages e2793–e2796, https://doi.org/10.1093/milmed/usac179
Close - Share Icon Share
ABSTRACT
We report the case of a 37-year-old man presenting with pain out of proportion to the exam with hydrofluoric acid burns to his upper extremities after he spilled a wheel-stripping compound on his forearms while working at his powder coating business. His burns initially appeared mild and superficial, but over the course of several days, these evolved from simple erythema to significant partial thickness tissue destruction and ulceration. He required substantial topical, intradermal, and intravenous therapies to control the unseen burning process during his index visit to the emergency department. We transferred the patient to a burn center given the location of his burns and the causative agent. The burn center clinicians observed him over the course of two nights and then discharged him with instructions to come for multiple follow-up visits during the subsequent month. Following nonoperative management, he had an uneventful recovery with full function retained in the affected extremities. Hydrofluoric acid burns require prompt treatment with calcium to neutralize the burning process, despite a potentially benign initial appearance. The emergency clinician should use an aggressive diagnostic and therapeutic approach to patients presenting with pain out of proportion to their exam, as this finding is associated with various serious underlying pathology.
CASE PRESENTATION
A 37-year-old right-hand–dominant male presented to the emergency department of a military treatment facility in central Texas with acute onset pain in his arms after accidentally splashing Benco B17, a wheel-stripping compound containing dichloromethane, phenol, formic acid, and notably hydrofluoric acid at a concentration of 10%, on his arms while moving a container of the solution. The injury occurred off-post from the military treatment facility at the patient’s nonmilitary civilian occupation.
History
The patient presented with progressively worsening burning pain in both forearms and hands, worse to his dominant right arm and wrist. Additionally, he denied inhalation of the compound. The patient sustained chemical burns to his right forearm, wrist, hand, and thumb and left wrist, hand, and thumb. Aside from pain on a scale of 5 out of 10, the patient had no other symptoms. He denied difficulty breathing, chest pain, numbness, tingling, weakness, fever, or chills. The patient had no history of diabetes, heart disease, lung disease, renal disease, hypertension, gastrointestinal disease, or neurological disease. Of note, the patient’s last tetanus immunization was more than 10 years ago.
Physical Examination
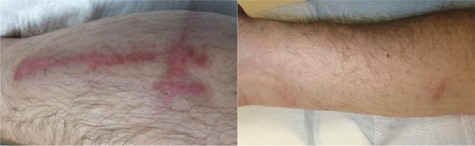
The patient was alert and appeared in no acute distress aside from significant pain but was otherwise well appearing. He was hemodynamically stable with a blood pressure of 134/90 mmHg, heart rate of 83 beats per minute, respirations of 20 breaths per minute, a temperature of 98.3°F, and SpO2 of 100% on room air. His skin showed no abrasions or lacerations; however, his right forearm revealed mixed first- and second-degree burns with intact vesicles. The patient’s right wrist had a second-degree burn to the volar joint line. Additionally, his hands had minor first-degree burns to the dorsal surfaces. Pictures from the day of injury were not available; however, Figure 1 shows the patient’s right upper extremity injuries on day 7 closely resembling their appearance. We estimated that his total body surface area burned at 5%, with 4% on the right upper extremity. He had no sensory or motor deficits on examination, and his extremities were without evidence of compartment syndrome. Examination of the head, eyes, ears, nose, and throat yielded no concerns, specifically no evidence of burns or airway compromise. Examinations of the neurological system, heart, lungs, abdomen, and lower extremities were unremarkable.

Management and Outcome
Upon placement in the exam room, the patient continued the irrigation process that had begun during triage of his upper extremities in the sink. The patient presented with pain out of proportion to his benign-appearing burns, and his pain did not improve despite irrigation. Once we identified hydrofluoric acid as an ingredient on the product information label, we created a calcium gluconate gel by mixing 40 mL of 10% calcium gluconate intravenous (IV) solution with water-soluble surgical lubrication. We applied the gel to the affected areas on both upper extremities. Despite topical calcium therapy, his pain increased from a 5 to an 8 out of 10, and the painful areas enlarged without the enlargement of the visible injuries.
For this reason, we administered 100 µg of fentanyl intravenously in anticipation of an IV Bier’s block with simultaneous subcutaneous, intradermal calcium gluconate infiltrations. We performed Bier’s block by placing a tourniquet just proximal to the right elbow and then administering diluted calcium gluconate (10 mL of 10% calcium gluconate in 40 mL of normal saline) through an IV distal to the tourniquet. We left the tourniquet in place for 20 minutes. During the 20 minutes with the tourniquet, we prepared a 5% calcium gluconate subcutaneous/intradermal solution using a 1:1 mixture of 10% calcium gluconate and normal saline and obtained a venous blood gas, a comprehensive metabolic panel, and an electrocardiograph. The patient’s neurovascular function remained intact following removal of the tourniquet used for Bier’s block. We performed the local injections in the areas the patient pointed to as painful. He reported relief in these areas within seconds, and we continued this process throughout the upper extremities until he denied pain. The initial local subcutaneous/intradermal injections required 40 mL of the calcium gluconate/normal saline mixture. However, over the next several minutes, his pain returned in margins outside of the visible burns indicating expansion of the burn under the epidermis. We injected an additional 10 mL in the new areas alleviating his pain. We used pain resolution as the indicator that we had neutralized the burning process. His electrolytes, including ionized calcium, were unremarkable, as was his EKG. The patient received a total of 100 µg of fentanyl, 1 L of normal saline, 40 mL of 10% calcium gluconate topically, 10 mL of 10% calcium gluconate IV, and 50 mL of 5% calcium gluconate intradermally/subcutaneously. Additionally, his tetanus vaccine was updated.
At this point, we consulted the on-call burn surgeon at our receiving burn center because of chemical burns to his hands and wrist. Approximately 1 hour later, before his transfer, we administered an additional 100 µg of fentanyl to help limit pain due to the mechanical irritation of his burned skin during transport. The patient was admitted to the burn unit for two nights for observation, and he did not require surgical intervention. Occupational therapy treated the patient and noted no signs of contractures and, importantly, no difficulties with activities of daily living. He was treated with PolyMem dressings, and his wounds were cleansed with Vashe Wound solution. His wounds continued to evolve over the next 2 weeks, eventually ulcerating (Fig. 2). After approximately 1 month, he was released from outpatient burn clinic routine care with instructions to follow up on an as-needed basis (Fig. 3).

DISCUSSION
Hydrofluoric acid (HFA) is a corrosive chemical that can cause significant dermatologic injury and has the potential for systemic involvement and death.1 It is found in glass and microchip etching materials and many different cleaning agents for glasses and metals, including rust removers, toilet bowl cleaners, air conditioner cleaners, and jewelry cleansers.1,2 Chemical burns are responsible for only 10% of all cutaneous burns but responsible for nearly 30% of burn deaths.3 Early recognition of potential HFA exposure and proper treatment of HFA burns is paramount in preventing severe systemic injury.1,4
HFA burns are associated with significant pain, and hospital admission may be required for pain control.5 Patients with HFA burns often present with pain out of proportion to physical exam findings.6 Evidence of a burn may not be visible immediately following HFA contact with skin. However, the erythema or other signs of HFA exposure may appear hours to days later due to HFA crossing the lipid membranes and diffusing into deeper tissues, as demonstrated by our patient’s wound progression over 2 weeks. HFA exposure causes liquefactive necrosis of soft tissue. The fluoride ions dissociate and bind with calcium and magnesium ions when exposed to the skin. The resulting calcium fluoride compound can cause tissue necrosis and cell death. Hyperkalemia from apoptosis has the potential to cause cardiac arrhythmias and possible death.1 Other electrolyte abnormalities associated with HFA burns include hypocalcemia and hypomagnesemia.7 Clinicians should also evaluate patients exposed to HFA with an electrocardiograph and serial labs for electrolyte disturbances.
Although HFA exposures are an uncommon cause of burns in the U.S. military, there is potential for exposure, not only from traditional sources. HFA is a byproduct of the breakdown of 1,1,1,2,3,3,3-heptafluoropropane, a hydrofluorocarbon used in automatic fire suppression systems used in military vehicles.8 Additionally, HFA is a toxic industrial chemical and is an easily accessible chemical that can be used in terrorism as a chemical weapon.8,9 Furthermore, clinicians in the deployed setting may find themselves responsible for providing emergency care to nonmilitary personnel (e.g., host nation citizens, third-country nationals, and contract personnel) presenting with injuries from an unknown origin with an unclear mechanism of injury. Treatment for HFA burns can be complicated, as in our case, if commercial preparations of calcium gluconate pastes/gels are not readily available, requiring clinicians to make various applications as we did.
Forward deployed units may find themselves dealing with even more limited supplies. Fortunately, a topical calcium gel can be created utilizing more common calcium preparations, such as chewable calcium carbonate tablets and a water-soluble surgical lubricant, which medics should have on hand. Five ounces of a water-soluble lubricant (SurgiLube) can be mixed with 10 g of calcium carbonate tablets (TUMS).10
Initial management of HFA burns is irrigation with water for at least 15 minutes to remove HFA that is still on the skin and dilute any residual HFA.7 Calcium gluconate is the treatment of choice for HFA exposures as it neutralizes the burning process by binding with the fluoride ion preventing further tissue necrosis and provides pain relief.1 The literature recommends the topical application of calcium gluconate gel 2.5% following irrigation. The gel is applied and massaged into the skin every 30 minutes.6 Successful treatment is demonstrated by improvement in pain.6 Calcium gluconate gel is sold commercially, but if not available in the emergency department, the clinician can prepare the mixture with 75 mL of water-soluble lubricant and 25 mL of 10% calcium gluconate, or 100 mL water-soluble lubricant plus 2.5 g of calcium gluconate.6 In many cases, patients with refractory pain from HFA exposures may require intradermal, IV, and then intra-arterial infiltration of calcium gluconate. Intradermal infiltration consists of a 5%-10% solution with no more than 0.5 mL injected per square centimeter.6,11 Calcium gluconate can then be administered intravenously with a Bier block, with a tourniquet placed proximal to the site of dermal injury. The IV calcium gluconate can be prepared by combining 10 mL of 10% calcium gluconate in 30-40 mL of normal saline and left in place for 20-25 minutes.12 Next, if pain continues, 10 mL of 10% calcium gluconate can be diluted in 50 mL of normal saline and infused over 4 hours.13 If pain continues, dialysis or surgical intervention may be required, outside the scope of an emergency medicine clinician.6,7
Our patient had a chemical burn involving the hands and wrists, necessitating specialty burn care. The American Burn Association states that the following 10 items require a referral to a burn center:
1. Partial thickness burns greater than 10% total body surface area.
2. Burns that involve the face, hands, feet, genitalia, perineum, or major joints.
3. Third-degree burns in any age group.
4. Electrical burns, including lightning injury.
5. Chemical burns.
6. Inhalation injury.
7. Burn injury in patients with preexisting medical disorders that could complicate management, prolong recovery, or affect mortality.
8. Any patient with burns and concomitant trauma (such as fractures) in which the burn injury poses the greatest risk of morbidity or mortality. In such cases, if the trauma poses the greater immediate risk, the patient may be initially stabilized in a trauma center before being transferred to a burn unit. Physician judgment will be necessary in such situations and should be in concert with the regional medical control plan and triage protocols.
9. Burned children in hospitals without qualified personnel or equipment for the care of children.
10. Burn injury in patients who will require special social, emotional, or rehabilitative intervention.14
CONCLUSION
In this case, the patient was aware that his chemical burn involved hydrofluoric acid; however, an emergency medicine clinician must have a high suspicion for an HFA burn in patients presenting with pain out of proportion to the exam following chemical exposure. Pain out of proportion to clinical exam is associated with various serious pathologies, as was in our case, and for this reason, should be approached with an aggressive diagnostic and therapeutic treatment plan. As with most chemical exposures, irrigation is the first step in removing the irritant. The endpoint for intervention with the various calcium preparations is neutralization of the burning process as indicated by symptomatic improvement in the patient’s pain. Including HFA burns in differential diagnoses is essential, especially when deployed forward, because patients may present with an unclear mechanism of injury unrelated to current military operations. Treatment options include creating a paste with readily available chewable calcium carbonate tablets and water-soluble lubricant to neutralize the burning process. Chemical burns require at least a consult to a burn center, if not a transfer.
FUNDING
None declared.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
Author notes
The views presented in this article are strictly those of the authors and do not necessarily represent the views of the United States of America, the Department of Defense, or the United States Army or its components.



