-
PDF
- Split View
-
Views
-
Cite
Cite
Josh Halfpap, Laura Riebel, Angela Tognoni, Michael Coller, Robert G Sheu, Michael D Rosenthal, Improving Access and Decreasing Healthcare Utilization for Patients With Acute Spine Pain: Five-Year Results of a Direct Access Clinic, Military Medicine, Volume 188, Issue 7-8, July/August 2023, Pages e2340–e2346, https://doi.org/10.1093/milmed/usac064
Close - Share Icon Share
ABSTRACT
Spine pain is one of the largest and costliest burdens to our healthcare systems. While evidence-based guidelines for spine pain have been established, and continue to evolve, the actual management of this condition continues to burden the healthcare system. This has led to increased costs due to inefficient entry to healthcare, utilization of treatments unsupported by clinical guidelines, and patient navigation through our healthcare systems. The purpose of this study was to assess the healthcare utilization and related outcomes for Active Duty Service Members (ADSM) receiving healthcare services in a novel acute spine pain clinic (ASPC) during the first 5 years of operation at a large Military Treatment Facility.
In 2014 the Physical Medicine and Rehabilitation and Physical Therapy (PT) services designed a novel acute spine clinic intended to directly receive ADSM with acute spine symptoms for an initial evaluation by a Physical Therapist. The inclusion criteria into the ASPC were: ADSM, pain less than or equal to 7 days, no more than three prior episodes of acute spine pain in the past 3 years, and not currently receiving care from Chiropractic, Pain Management, or PT services. The exclusion criteria were: significant and/or progressive neurological deficits, bowel or bladder dysfunction, unstable vital signs or fever, hematuria or extensive trauma.
A total of 1,215 patients presented to the ASPC for evaluation between 2014 and 2019. The most common chief complaint was acute pain in the lumbar spine (73%), followed by cervical spine pain (15%), and thoracic spine pain (12%) represented the fewest. The average number of PT visits per patient was 3.5 (range 1-13) with 61.1% utilizing three or fewer visits. Over 95% of cases returned to work the same day as their initial evaluation. Sixty-six percent returned to work without restriction the same day as their initial evaluation. Light duty recommendations were provided to 412 (33.9%) patients ranging from one to 30 days, with greater than 85% of the light duty being less than 14 days. Recommendations to not return to work (sick-in-quarters) were issued to 56 (4.6%) patients. The sick-in-quarters recommendations were for a 24-hour period in 48 cases, 48 hours for seven cases, and 72 hours for one case. All encounters in which the patient first sought care at the ASPC for low back pain met the Healthcare Effectiveness Data Set standard for low back pain care of having no imaging within 28 days of the first encounter for nonspecific low back pain. A medical record review of 100 randomly selected patients within 12 months of the initial evaluation demonstrated decreased utilization of medication, imaging, and referral to surgical services.
This innovative approach demonstrates the potential benefits of rapid access to treatment and education for patients with acute spine pain by a Physical Therapist. Modeling this approach at Military Treatment Facilities may lead to decreased utilization of medications, radiology services, specialty care referrals, and reduced cost of care provided to individuals with acute spine pain.
INTRODUCTION
Spine pain is one of the largest and costliest burdens to our healthcare systems.1,2 Low back pain (LBP) alone results in an average of 2.7 million Emergency Department visits annually in the USA with 17.8% of uncomplicated LBP patients receiving unnecessary x-rays.3 Immense discussion and debate have emerged to determine optimal management for individuals with spine pain.4–6 The challenge of how to optimally treat patients with acute or chronic spine pain has led to various theories and methodologies advocating for numerous strategies for integrated care. However, current healthcare models are fractured as patients get consulted from specialty to specialty receiving various short-term treatment methods from siloed services who often disagree on diagnosis, management, and have poor communication channels.7,8 Most importantly, this leads to disjointed services where patients may receive conflicting diagnosis, education, and management. These effects of the current model of healthcare (aside from higher costs to the health care system) negatively impact the primary stakeholder of which the system is designed to help, the patient.
While evidence-based guidelines for spine pain have been established, and continue to evolve, the actual management of this condition continues to burden the healthcare system. This has led to increased costs due to inefficient entry to healthcare, utilization of treatments unsupported by clinical guidelines, and patient navigation through our healthcare systems.9 For example, evidence continues to demonstrate an increase in the use of imaging for the evaluation of patients with LBP.10,11 One in four patients presenting to primary care, and one in three patients presenting to emergency departments for lower back pain continue to receive imaging despite guideline advice indicating imaging is only of added benefit with specific findings on physical examination.12
While research continues in search of an optimal mode of treatment and pathway management, some research teams are looking at ways to break down barriers to patients’ access to care and establish a consistent dialogue about treatment approaches between multiple specialties.4,6,13 Recent studies have shown a significant reduction in disability through early referral to PT.14–16 Additionally, research demonstrates treating back pain in the acute stage is effective for reducing cost, lost workdays, avoiding unnecessary imaging, decreasing medication use, and minimizing the risk of persistent pain.11,17
Traditional medical care is undergoing a transition from volume-based to value-based care.8 Integrated Practice Units (IPUs), a relatively new method described by Michael Porter in the Harvard Business Review, contends that organizing health care service structure around the patient will maximize value for patients.7 More specifically, “the real opportunity to drive major efficiencies and improvements in quality occurs through focusing on specific patient conditions and optimizing their care.”8
This report presents a modified IPU, an Acute Spine Pain Clinic (ASPC), aimed at achieving what Porter described as a model structured around the patient to deliver high-quality, evidence-based care.7 Prior to implementation of the ASPC, the usual pathway for patients with acute spine pain was through a same-day appointment, if available, with Primary Care or the Emergency Department. Patients not deemed to have urgent surgical needs or requiring immediate further workup for non-musculoskeletal pathologies would typically be given either (1) education and advice and follow-up with a primary care provider or (2) a referral to Physical Therapy (PT). Unfortunately, due to the high volume of referral to PT services, wait times for the initial evaluation period often takes 2-4 weeks.
Physical Therapists have a long history of treating nonsurgical back pain and have demonstrated their effectiveness and ability to initially evaluate patients with acute spine pain.4,15,16,18,19 To deliver the right care at the right time to patients, the novel ASPC was established in a large U.S. Naval Military Treatment Facility (MTF) in an attempt to deliver early and efficient access to high-quality, evidence-based, and patient-centered care for patients with acute spine pain.
The purpose of this descriptive study was to assess the healthcare utilization and related outcomes for Active Duty Service Members (ADSM) receiving healthcare services for acute spine pain in the ASPC during the first 5 years of operation.
METHODS
Setting and Participants
In 2014 the Physical Medicine and Rehabilitation (PM&R) and PT services collaborated to design a novel ASPC intended to directly receive ADSM with acute spine symptoms for an initial evaluation by a Physical Therapist. The clinic was located at an outlying branch clinic of a major MTF and received patients throughout the region empaneled to the MTF network.
Inclusion and Exclusion
The inclusion criteria into the ASPC were: ADSM, pain less than or equal to 7 days, no more than three prior episodes of acute spine pain in the past 3 years, and not currently receiving care from Chiropractic, Pain Management, or PT services. The exclusion criteria were: significant and/or progressive neurological deficits, bowel or bladder dysfunction, unstable vital signs or fever, hematuria, or extensive trauma. If any exclusion criteria were identified, the patient was referred to the ASPC PM&R Physician, another Physician, or to the Emergency Department for a same-day appointment as appropriate. See Table I for full inclusion and exclusion criteria. Some exclusion criteria are deemed relative due to the clinician basing their final decision with respect to the entirety of the individual case and overall scenario judgment. For example, a patient with pain radiating below the knee which is mild in nature, without a mechanism of injury, has not progressed since onset and has no other history to indicate serious pathology would most likely still be evaluated and treated in the ASPC. A patient presenting with acute and severe onset of pain radiating to the knee with a mechanism of injury and a clinical appearance of being unstable and progressive would likely be referred to the emergency department or provider as indicated.
| Inclusion Criteria Active Duty Service Member Pain ≤ 7 Days Less than Three Prior Episodes of Acute Low Back Pain in 3 years Not currently treated by Physical Therapy, Chiropractic, or Pain Clinic |
| Exclusion Criteria Pending Referral to Pain Clinic for Non-Urgent Consultation Pain greater than 7 Days (Relative Exclusion)a Pain radiates below the knee (Relative Exclusion)a Prior Back Surgery History of Chronic Back Pain (Relative Exclusion)a Patient currently utilizing Opioid Medication Patient with past medical history of: Rheumatoid Arthritis, Inflammatory Disease, Autoimmune Disease History of recent Trauma/ or Falls (Relative Exclusion)a Immediate Referral to Emergency Department/Physician for Urgent Consultation Progressive neurological changes (Relative Exclusion)a Loss of bowel or bladder function Unstable Vital Signs, Fever Hematuria |
| Inclusion Criteria Active Duty Service Member Pain ≤ 7 Days Less than Three Prior Episodes of Acute Low Back Pain in 3 years Not currently treated by Physical Therapy, Chiropractic, or Pain Clinic |
| Exclusion Criteria Pending Referral to Pain Clinic for Non-Urgent Consultation Pain greater than 7 Days (Relative Exclusion)a Pain radiates below the knee (Relative Exclusion)a Prior Back Surgery History of Chronic Back Pain (Relative Exclusion)a Patient currently utilizing Opioid Medication Patient with past medical history of: Rheumatoid Arthritis, Inflammatory Disease, Autoimmune Disease History of recent Trauma/ or Falls (Relative Exclusion)a Immediate Referral to Emergency Department/Physician for Urgent Consultation Progressive neurological changes (Relative Exclusion)a Loss of bowel or bladder function Unstable Vital Signs, Fever Hematuria |
Relative exclusion factors are based on the entirety of the individual case and clinician judgment.
| Inclusion Criteria Active Duty Service Member Pain ≤ 7 Days Less than Three Prior Episodes of Acute Low Back Pain in 3 years Not currently treated by Physical Therapy, Chiropractic, or Pain Clinic |
| Exclusion Criteria Pending Referral to Pain Clinic for Non-Urgent Consultation Pain greater than 7 Days (Relative Exclusion)a Pain radiates below the knee (Relative Exclusion)a Prior Back Surgery History of Chronic Back Pain (Relative Exclusion)a Patient currently utilizing Opioid Medication Patient with past medical history of: Rheumatoid Arthritis, Inflammatory Disease, Autoimmune Disease History of recent Trauma/ or Falls (Relative Exclusion)a Immediate Referral to Emergency Department/Physician for Urgent Consultation Progressive neurological changes (Relative Exclusion)a Loss of bowel or bladder function Unstable Vital Signs, Fever Hematuria |
| Inclusion Criteria Active Duty Service Member Pain ≤ 7 Days Less than Three Prior Episodes of Acute Low Back Pain in 3 years Not currently treated by Physical Therapy, Chiropractic, or Pain Clinic |
| Exclusion Criteria Pending Referral to Pain Clinic for Non-Urgent Consultation Pain greater than 7 Days (Relative Exclusion)a Pain radiates below the knee (Relative Exclusion)a Prior Back Surgery History of Chronic Back Pain (Relative Exclusion)a Patient currently utilizing Opioid Medication Patient with past medical history of: Rheumatoid Arthritis, Inflammatory Disease, Autoimmune Disease History of recent Trauma/ or Falls (Relative Exclusion)a Immediate Referral to Emergency Department/Physician for Urgent Consultation Progressive neurological changes (Relative Exclusion)a Loss of bowel or bladder function Unstable Vital Signs, Fever Hematuria |
Relative exclusion factors are based on the entirety of the individual case and clinician judgment.
EXAMINERS
During operating hours (0730-0930) the clinic was staffed by one licensed Physical Therapist who was either a Board-Certified Clinical Specialist in Orthopedic or Sports PT. Board-certified PT specialists are required to attain at least 2,000 hours of direct patient care in the area of specialization, pass a written certification examination, and maintain requisite hours and continuing education required for renewal every 10 years. All providers serving on this project were federal health care workers with clinical privileges to evaluate and treat patients suffering from injury or disease with or without a referral, provide temporary duty limitations, order diagnostic laboratory and imaging studies, place patients sick-in-quarters, and refer patients to other practitioners as appropriate in accordance with local MTF policies. Additionally, they held the supplemental privilege to prescribe medication (in accordance with the local MTF Pharmacy and Therapeutics committee policies). Treatments following the initial evaluation were provided by the Physical Therapist, a licensed PT Assistant, or a U.S. Navy Physical Therapy Technician.
Clinic Accessibility
The ASPC was accessible for direct (walk-in, including self-referral) access for 2 hours each business day. Alternatively, if a patient sought care for acute spine pain at other locations such as their designated PCP or Emergency Department, providers could contact the PT clinic and request patient evaluation in the ASPC the same or following business day.
Outcome Measures
Patient-reported outcome measures were collected at the initial evaluation and discharge. In addition to general healthcare history and a body chart, all patients completed the Fear Avoidance Beliefs Questionnaire (FABQ),20,21 the Numeric Pain Rating Scale (NPRS), and the Single Assessment Numeric Evaluation (SANE).22 Those patients with pain involving the mid-thoracic and lower regions of the spine completed the Oswestry Disability Index (ODI) while those with pain in the region of the cervical and upper thoracic region completed the Neck Disability Index (NDI).23,24
Patient Intervention
Patient intervention was applied per current guidelines for the treatment of acute spine pain.25–28 The diagnostic approach focused on a thorough history and physical examination to screen for serious pathology or underlying conditions (red flags), and included a common mental health screening, the Patient Health Questionnaire-2 (PHQ-2).29 Patients were treated using interventions that focused on active (e.g., exercise prescription) versus passive (e.g., heat, transcutaneous electrical nerve stimulation, or ultrasound) intervention and pharmacologic therapy when needed.30–32 To minimize the risk of acute pain becoming chronic, emphasis was placed on patient education using a biopsychosocial framework focusing on reassurance, prognosis, advice to remain active, and information on self-care options.33,34 Patients identified with elevated fear-avoidance, as indicated by their outcome measure score on the FABQ, received education throughout each encounter on safe and positive movements.
STATISTICAL ANALYSIS
Healthcare utilization related to spine pain for each patient was assessed over a period of 12 months beginning with the initial ASPC evaluation. Primary factors assessed for all patients were the number of PT visits and the amount of lost duty/work time. For a random sample of 100 patients, utilization of radiology, medication, use of non-PT healthcare services, and a return to PT after discharge within one year was also assessed. Pearson’s correlations (Pearson’s r) were performed to evaluate the association between patient-reported questionnaires and pain at intake and the number of ASPC visits. Data were analyzed using retrospective chart review through the Armed Forces Health Longitudinal Technology Application (AHLTA), Microsoft Excel 2016 software, (Microsoft Corporation), and SPSS software, version 24.0 (IBM Corp., Armonk, NY, USA).
Ethical Approval
The study was approved by the investigational review board at Naval Medical Center San Diego, CA (CIP # NMCSD.2019.0048).
RESULTS
A total of 1,215 patients presented to the ASPC for evaluation between 2014 and 2019. The most common chief complaint was acute pain in the lumbar spine (73%), followed by cervical spine pain (15%), and thoracic spine (12%) represented the lowest percentage. The average number of PT visits per patient was 3.5 (range 1-13) with 61.1% utilizing three or fewer visits. Over 95% of cases returned to work the same day as their initial evaluation. Sixty-six percent returned to work without restriction the same day as their initial evaluation. Light duty recommendations were provided to 412 (33.9%) patients ranging from one to 30 days, with greater than 85% of the light duty being less than 14 days. Recommendations to not return to work (sick-in-quarters) were issued to 56 (4.6%) patients. The sick-in-quarters recommendations were for a 24-hour period in 48 cases, 48 hours for seven cases, and 72 hours for one case.
All encounters in which the patient first sought care at the ASPC for LBP met the Healthcare Effectiveness Data Set (HEDIS) standard for LBP of having no imaging within 28 days of the first encounter for nonspecific LBP.35
A thorough medical record review of 100 randomly selected patients who came to the ASPC was performed. Within 12 months of the initial ASPC evaluation, 22% sought care with their PCP for spine pain, 7% were referred to a surgical service (i.e., orthopedics or neurosurgery), and 9% were evaluated by a pain management provider. Eleven percent returned to PT within 1 year of discharge.
Table II displays the outcome measure scores and correlation with the number of total visits per patient in a subsample (N = 100). Table III reports the rates of medication and imaging usage in the subsample population (N = 100) compared reported industry standard rates of patients reporting to emergency departments for acute LBP.
Intake Patient-Reported Outcome Measures Taken at Initial Evaluation and Correlation with the Number of Total Visits per Patient in a Subsample (N = 100)
| . | Mean (SD) . | R . |
|---|---|---|
| FABQPA | 18.1 (5.59) | 0.07 |
| FABQW | 14.3 (10.0) | 0.15 |
| ODI | 43.2% (17.5) | 0.14 |
| NDI | 37.4% (16.2) | 0.13 |
| SANE | 45.1% (20.9) | −0.06 |
| . | Mean (SD) . | R . |
|---|---|---|
| FABQPA | 18.1 (5.59) | 0.07 |
| FABQW | 14.3 (10.0) | 0.15 |
| ODI | 43.2% (17.5) | 0.14 |
| NDI | 37.4% (16.2) | 0.13 |
| SANE | 45.1% (20.9) | −0.06 |
SD = Standard deviation.
r = Pearson’s Correlation Coefficient.
Intake Patient-Reported Outcome Measures Taken at Initial Evaluation and Correlation with the Number of Total Visits per Patient in a Subsample (N = 100)
| . | Mean (SD) . | R . |
|---|---|---|
| FABQPA | 18.1 (5.59) | 0.07 |
| FABQW | 14.3 (10.0) | 0.15 |
| ODI | 43.2% (17.5) | 0.14 |
| NDI | 37.4% (16.2) | 0.13 |
| SANE | 45.1% (20.9) | −0.06 |
| . | Mean (SD) . | R . |
|---|---|---|
| FABQPA | 18.1 (5.59) | 0.07 |
| FABQW | 14.3 (10.0) | 0.15 |
| ODI | 43.2% (17.5) | 0.14 |
| NDI | 37.4% (16.2) | 0.13 |
| SANE | 45.1% (20.9) | −0.06 |
SD = Standard deviation.
r = Pearson’s Correlation Coefficient.
In a Subsample (N = 100), a Comparison of Orders between PTs, Non-PT Providers, and Worldwide ED Reported Rates
| . | PTa . | Non-PTa . | ED Industry rates (SD)b . |
|---|---|---|---|
| Medications | 26% | 20% | 47.4-72.0%44 |
| Radiographs | 7% | 28% | 26.1% (18.2, 35.8)40 |
| Complex Imaging | 1% | 12% | 8.2% (4.4, 15.6)12 |
| . | PTa . | Non-PTa . | ED Industry rates (SD)b . |
|---|---|---|---|
| Medications | 26% | 20% | 47.4-72.0%44 |
| Radiographs | 7% | 28% | 26.1% (18.2, 35.8)40 |
| Complex Imaging | 1% | 12% | 8.2% (4.4, 15.6)12 |
Taken from N = 100 subsample.
ED = Emergency Department.
In a Subsample (N = 100), a Comparison of Orders between PTs, Non-PT Providers, and Worldwide ED Reported Rates
| . | PTa . | Non-PTa . | ED Industry rates (SD)b . |
|---|---|---|---|
| Medications | 26% | 20% | 47.4-72.0%44 |
| Radiographs | 7% | 28% | 26.1% (18.2, 35.8)40 |
| Complex Imaging | 1% | 12% | 8.2% (4.4, 15.6)12 |
| . | PTa . | Non-PTa . | ED Industry rates (SD)b . |
|---|---|---|---|
| Medications | 26% | 20% | 47.4-72.0%44 |
| Radiographs | 7% | 28% | 26.1% (18.2, 35.8)40 |
| Complex Imaging | 1% | 12% | 8.2% (4.4, 15.6)12 |
Taken from N = 100 subsample.
ED = Emergency Department.
DISCUSSION
The ASPC, led by Physical Therapists, demonstrated safe triage and effective treatment of acute spine pain in a military population. More than 95% of patients returned to work the same day as the ASPC evaluation thereby minimizing lost workdays. Historical data on return to work rates in the military population with acute back pain is not evident from a review of the literature. There is one civilian report that states 80-90% improve within 3 months with LBP.36 Our report may be one of the first to report return to work rates in a population with acute spine pain. Additionally, healthcare utilization with respect to number of PT visits, use of medication, radiology, and referral to specialty services was significantly reduced as compared to traditional referral-based models.15,37
Average scores on the ODI, NDI, and SANE scores were consistent with moderate (range mild to severe) levels of patient-reported pain and disability.22–24 The FABQ was developed to help quantify fear of pain and patient beliefs about the need to change behavior to avoid pain in individuals with LBP. The FABQ comprises two sections: Physical Activity and Work. Patients’ average score on the work component was 14.3 (high = > 34) and was not associated with an elevated fear-avoidance related to returning to work. Scores for the fear of return to physical activity section averaged 18.1 (high = > 15) demonstrating an elevated level of fear regarding the patient’s outlook on returning to physical activity. Although the ASPC utilized commonly recommended patient-reported questionnaires, there was a very low correlation between scores on these measures and the number of visits utilized by patients. The limited prognostic ability of the FABQ for individuals with acute LBP (less than 6 months) has been reported previously which suggests there may be low predictive value in using the questionnaires as a prognostic component in the evaluation and management of individuals with acute spine pain.38 See Table II for full data. Prescription of medications in the ASPC was similar to MTF primary care origination of care but lower than civilian ED prescription rates. (Table III). Ordering of imaging was substantially lower in the ASPC as compared to primary care (same MTF) utilization and as compared to civilian sector reports (Table III).35,39
New and emerging evidence since the inception of this study demonstrates similar results for this patient population.14,15,37 For patients with spine pain who receive early and unrestricted access to PT, they are likely to require fewer visits, and have a lower risk of subsequent high-cost healthcare services such as imaging, medication, and referral to specialty services.11,16,40,41 The true value of the success of any clinic lies in getting the patient the right care at the right time, and the appropriate amount of visits.
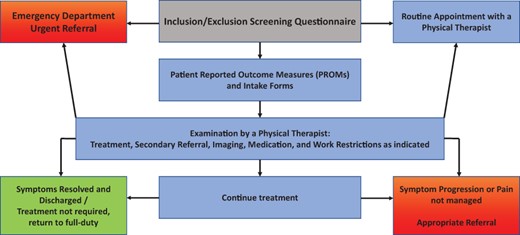
The positive results from the ASPC led to expansion from one location in 2014 to three locations by 2016. Modifications to the initial ASPC IPU were implemented over the course of the first 2 years. During the design of the initial process, it was believed an early and defined filter should be in place to send the patient to the PM&R specialist if the patient’s pain was not improving or not responding to management at a specified pace and time frame. However, based upon feedback from team members, and in consideration of providers’ level of clinical privileges, and initial successful outcomes, the process evolved to a pragmatic shared decision-making process between the patient and provider versus a formulated set number of visits as to when the patient required further referral to specialty services (Fig. 1).
It is important to note an important benefit and outcome of this clinic. Emergency department and primary care providers reached out to the ASPC staff to acknowledge the benefit of this type of clinic which reduced unnecessary work volume, improved the ability to be seen and evaluated and treated the same day without referral wait times.
Limitations of this report include the retrospective nature, limited data available, and utilization of less than 10% of the cases for more detailed analyses. Additionally, the likelihood that emergency departments may see more complex cases than the ASPC may result in higher utilization of complex imaging and medication.
CASE EXAMPLES
The vast majority of patients that reported to the ASPC had common neuromusculoskeletal conditions (e.g., strain, sprain, and radicular pain) that were effectively treated in the ASPC. Three cases are presented which comprise the red flag conditions encountered during the review period. Other cases whose symptoms did not resolve sufficiently or progressed were often referred for additional consultation while being concurrently treated in the ASPC. Concurrent referral and management were done for approximately 25 patients (2%). This was most commonly due to the presentation of mental health conditions (positive PHQ-2 screening, referred to Mental Health), severe pain unresponsive to ASPC intervention (referred to PM&R or Pain Clinic), and significant or worsening sensory and/or motor deficits (referred to Neurosurgery, Orthopedic Spine, or the Emergency Department). These cases highlight the capability of PTs to safely triage and manage more severe cases which would otherwise overwhelm Emergency Departments or Primary Care clinics, or delay necessary care through standard referral wait times.
Case #1
A 33-year-old Active Duty U.S. Navy male reported to the ASPC with a complaint of acute LBP for 2 days and left lower quadrant pain for 1 day. On subjective examination the patient reported having a history of hematemesis and “black tarry stools” intermittently over the previous 9 months and received brief treatments without resolution of symptoms. The patient was currently taking cyclobenzaprine (10 mg), and ibuprofen (800 mg). Due to the red flags, a musculoskeletal examination was deferred, the Physical Therapist contacted the Primary Care Manager who then evaluated the patient within 1 hour. The patient was subsequently referred to and seen by a Gastroenterologist 5 days later. Further workup and testing revealed Gastric Antral Ectasia for which he was successfully treated for with medication.
Case #2
A 26-year-old Active Duty U.S. Coast Guard male visited the Emergency Department due to a flare-up of his chronic central LBP. The Emergency Department ordered radiographs that demonstrated an 8 mm lucency at the right L3 transverse process with no further workup during the encounter. Between the Emergency Department visit and the ASPC evaluation the patient developed acute radiating symptoms in the right posterior thigh, leg, and plantar aspect of his foot and the patient voiced concern about his operational suitability to the Physical Therapist due to a pending deployment in 2 months. On examination at the ASPC his neurological exam was normal. Due to the severity of the pain, possible correlation to his indefinite plain films and pending deployment his Primary Care Manager was notified and Magnetic Resonance Imaging (MRI) of the lumbar spine was ordered. His MRI results were unremarkable. Although the patient was unable to participate in deployment, after 5 months of PT the patient was discharged symptom free and returned to a fully deployable status.
Case #3
A 51-year-old Active Duty U.S. Navy male presented to the ASPC due to persistent neck pain for 5 days after a fall in shallow water while surfing. The patient reported impacting the head resulting in forceful right lateral flexion without loss of consciousness and fleeting pain radiating into the right upper extremity. In accordance with the Canadian Cervical Spine Rule, the PT ordered radiographs of the cervical spine which indicated subtle C4-5 anterior subluxation and widening of the interspinous space.42 Following consultation with neuroradiology a computed tomography (CT) scan was performed revealing a fracture of the right pedicle and lamina at C4 and suggestion of associated injury to the vertebral artery. A magnetic resonance angiogram immediately following the CT confirmed a right vertebral artery dissection at the C4 level with absence of flow-related enhancement. The patient underwent an C3-C5 anterior cervical discectomy and fusion. At 4 months following surgery he reported no pain or neurovascular symptoms and had resumed pre-injury exercise activities (swimming and surging) and resumed military service without limitations.43
CONCLUSIONS
This innovative approach demonstrates the potential benefits of rapid access to treatment and education for patients with acute spine pain and provides support for early intervention pathways conducted by Physical Therapists. Modeling this approach at Military Treatment Facilities may lead to a decreased utilization of medications, radiology services, specialty care referrals, and reduce cost of care provided for individuals with acute spine pain. Furthermore, no adverse events or outcomes have been reported throughout the duration of this report.
ACKNOWLEDGMENT
None declared.
FUNDING
None declared.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
Author notes
A portion of this manuscript material was presented in a 20-minute presentation at the American Physical Therapy Association’s Combined Sections Meeting (CSM) in Denver Colorado in February 2020.
The views expressed are solely those of the authors and do not reflect the official policy or position of the U.S. Navy, the DoD, or the U.S. Government.
- patient referral
- patient evaluation
- fever
- hematuria
- health services accessibility
- intestines
- low back pain
- lumbar vertebra
- military personnel
- pain
- surgical procedures, operative
- wounds and injuries
- pain management
- chiropractic
- diagnostic imaging
- guidelines
- radiology specialty
- spine
- vital signs
- acute pain
- health care systems
- evidence-based practice
- health care use
- physical therapists
- job reentry
- medical records review
- spine pain
- chief complaint



