-
PDF
- Split View
-
Views
-
Cite
Cite
James B Walsh, Andrea F McGlynn, Curtis L Hardy, George C Armas, Hadley M Sulpizio, Martin R Wright, Stretching and Self-Myofascial Release in Helicopter Aircrew to Reduce Neck and Back Pain (Phase 1), Military Medicine, Volume 188, Issue 7-8, July/August 2023, Pages e2109–e2117, https://doi.org/10.1093/milmed/usad015
Close - Share Icon Share
ABSTRACT
This prospective intervention study was designed to determine the efficacy of a standardized Preflight/Postflight Stretches (PPS) protocol to reduce subjective neck and back pain scores in helicopter aircrew. Aircrew transient back and neck pain is well documented, and there is currently no standardized preflight and postflight stretching protocol for Naval Aviation.
Subjects were recruited from two carrier air wing MH-60R squadrons at Naval Air Station Jacksonville. These carrier air wing squadrons were selected to control for size (number of aircrew), age, and operational tempo (number of flight hours). Subjects consisted of both pilots and enlisted aircrew. One squadron was designated as the control group, although the second squadron served as the intervention group. Subjects from both groups filled out the questionnaire. Only the intervention group completed the PPS protocol immediately after completing the questionnaire and before departing the squadron spaces for the aircraft outside. Upon landing, the aircrew completed a postflight debrief. Only the intervention group completed the PPS protocol after debrief. Both the intervention and control groups once again completed the questionnaire. Questionnaires were matched by using a generated anonymous subject ID. The amounts of change and pain levels were then compared using the Mann–Whitney test and the Fisher’s exact test, respectively.
The Kolmogorov–Smirnov test found the data to be nonparametric. The preflight and postflight overall (P ≤ .001), cervical (P ≤ .001), thoracic (P = .006), and lumbar (P = .004) differences between the control and intervention groups were found to be statistically significant when using the Mann–Whitney test. Preflight and postflight pain differences in the sacral region and “other” section were not found to be statistically significant (sacral, P = .618; others, P = .182). When evaluating the worsening of the pain level, 50 (92%) of the control flights in which PPS was not performed reported worse pain, compared to 21 (61.8%) in the intervention group where PPS was performed. The Fisher’s exact test found the association between performing PPS and the worsening in pain to be statistically significant (P = .001) in the overall, cervical, thoracic, and lumbar regions. Therefore, the hypothesis was accepted in regard to overall pain, as well as in the cervical, thoracic, and lumbar regions.
Aircrew back and neck pain because of flying is well documented. However, there is no standardized stretching protocol for aircrew to perform immediately preflight or postflight in U.S. Naval Aviation. This study demonstrated that PPS, a simple 5- to 7-min stretching routine, gives aircrew structure and can reduce postflight cervical, thoracic, lumbar, and overall pain. This phase proved to be safe as no adverse events were reported. The prehabilitation aspect could reduce conventional medical intervention, costly pharmacological management of neck and back pain, and be applied to other aviation populations in military and civilian communities.
INTRODUCTION
Aircrew transient back and neck pain is well documented.1,2,3 Between 50% and 90% of helicopter aircrew have experienced back pain.4 Among commercial helicopter operations in Norway, transient back pain was reported in 50% of pilots.5 The Royal Norwegian Air Force disclosed that 50.5% of helicopter aircrew experienced low back pain (LBP), and 48.6% admitted the pain influenced their work.6 Sixty-four percent of Australian military rotary wing pilots claimed back pain, and back pain interfered with 55% of the respondents’ concentration in flight.7 Polish military helicopter pilots reported that 70% had back pain.8 British Royal Navy helicopter pilots experienced a back pain prevalence of 82%.3 Another Royal Navy study showed that 80% of helicopter pilots had back pain in the prior 12 months of the study and 66% of these pilots admitted the back pain interfered with their flying duties.9 Of Royal Air Force helicopter pilots, 83% were affected by LBP at some point in their careers.4 Among Israeli utility helicopter pilots, 89.38% sustained back pain, as did 74.55% of attack helicopter pilots.1 Of U.S. Army helicopter aviators, 84.6% endured back pain at some point in their careers and 77.8% in the previous 12 months.10 Among U.S. Navy MH-60R and MH-60S helicopter aircrew, 88.1% experienced back pain during at least 50% of their flights, 41.9% admitted that their back pain was moderately distracting, and 34.4% admitted that their situational awareness was degraded because of LBP.2 With the abundance of documentation of back and neck pain, there have been conditioning protocols implemented; however, there are no standardized protocols for stretching immediately preflight or postflight within U.S. Naval Aviation.
The etiology of helicopter back pain has also been extensively studied.9–14 Many contributing factors have been examined including, but not limited to, previous back injury, body mass index/obesity, family history, and age.15 Probably the most studied factors are posture, such as the “helo hunch” (increased flexion of the spine), cockpit design and ergonomics, low-frequency whole-body vibration (WBV), and flight hours.5,15,16 Sitting alone has not been found to be a significant risk factor; however, when sitting is coupled with WBV and awkward posture, the risk of LBP increases by 400%.16 Not everyone agrees that WBV causes LBP. Vibrational versus non-vibrational flying using a simulator found no differences in reported back pain, suggesting that posture is the number one contributor to back pain.14 Although the research is mixed, some studies have shown that there is a significant positive correlation between hours flown in the prior 12 months of the study and spinal pain.5 “Prototypical” rotary wing back pain begins during or shortly after take-off and is typically experienced in the lumbar region. The pain is usually described as dull and achy and typically resolves after landing or within hours.15 Some researchers describe helicopter LBP as transient. Transient pain related to flying is described as “temporary, dull, non-radiating that has an onset during flying and ceases sometime after flying.”5 Since 85-90% of LBP is idiopathic and resolves within hours of flight, an accurate and precise diagnosis is often difficult to determine.15
Pelham et al. describe the kinesiology of the helicopter pilots in a seated position. The spine is in a forward flexed, kyphotic position. This posture shifts the center of mass forward, putting a significant load at the fulcrum point in the lumbar and lower thoracic spines. In this condition, the spinal extensors are contracting, and over time the spinal extensors fatigue, putting the load on the vertebral ligaments and joints.14 Furthermore, with the pilots’ center of mass shifted forward, large forces are placed on thoracic and lumbar discs at the fulcrum point. A compressive force is placed on the anterior edge of the disc although a separating force is placed at the posterior aspect of the disc. This force pushes the soft nucleus pulposus of the disc posteriorly and, in turn, puts pressure on the posterior portion of the annulus fibrosus, causing breakdown over time.14
Most applicable to the current study, while sitting in a “helo hunch,” the pelvis is shifted posteriorly compared to a neutral position. The pilot’s body weight is fully supported and balanced on the ischial tuberosities.14 With the weakening of the erector spinae and multifidus, the hip muscles and hamstrings can lose flexibility. Loss of flexibility in the hips and hamstrings can restrict lumbar flexion and prevent the hips from rotating to a neutral position. The decrease in hip and hamstring range of motion (ROM) causes mechanical stress on the lower back, which results in pain.14 A 2015 study compared the lumbar spine and hip flexibility of pilots with and without LBP. Unsurprisingly, pilots with LBP had greater side-to-side asymmetry in hip ROM.17
With all of these potential vulnerabilities and postural deficiencies, the desire for solutions and mitigating strategies is great. Current modalities to treat back pain include heat, massage, acupuncture, physical therapy, and spinal manipulation. Other treatment options also include yoga and tai chi.18 Although medication is an option, it is not a preferred treatment because of aircrew flight status.
As athletes stretch, warm up, and cool down for practices or competitions, the authors felt that this could translate to aircrew. Athletes’ routines can incorporate stretches as well as muscle energy. Muscle energy involves an isometric contraction with a contraction/relaxation technique to improve flexibility.19 Another modality is myofascial release, which is a manual therapy designed to knead and warm up the fascia to reduce restrictive barriers and fibrous adhesions. Additionally, it is thought to promote blood flow to low blood flow areas.20 When performed autonomously, using their own body weight and foam rollers, it is called self-myofascial release (SMR).20 The research on SMR is limited. However, the available research demonstrates positive results on increasing joint ROM. A 2013 study found that post-workout SMR on the anterior, lateral, posterior, and medial aspects of the thigh and gluteal muscles resulted in an increase in passive hip and quadriceps ROM compared to control.20 Foam rolling in combination with static stretching resulted in an increase in passive hip flexion ROM when compared to control (no intervention), foam rolling only, and static stretching only.21 In a 2015 literature review, five studies indicated that SMR increased joint ROM although one study was inconclusive.22 Oklahoma State University offensive linemen were studied in 2015, revealing that an 8-min foam roller protocol utilizing SMR of the hamstrings, quadriceps, gluteus maximus, and gastrocnemius was found to have a 15.6% increase in hip flexion ROM compared to the control group.23 A 2016 study found that foam rolling the hamstrings from the ischial tuberosities to the popliteal fossa resulted in an increased ROM for hip flexion and hip extension.24
The Preflight/Postflight Stretches (PPS) protocol was developed to reduce and potentially alleviate transient back pain associated with flight. Preflight/postflight stretches use a combination of static stretches, muscle energy, and SMR designed to increase hip ROM and promote hip symmetry. It was designed to encourage proper posture in-flight, to flow from one stretch into the next, and to take about 5 to 7 min. The purpose of this pilot study was to evaluate the efficacy of this simple PPS protocol as a means of reducing the deleterious effects of LBP. The authors hypothesized that the performance of PPS would significantly reduce subjective pain scores in helicopter aircrew.
METHODS
Preflight/postflight stretch is a prospective intervention study designed to determine the efficacy of a standardized protocol of preflight and postflight stretching to reduce subjective neck and back pain scores in helicopter aircrew. The PPS protocol was reviewed and approved by the Naval Medical Center Portsmouth Institutional Review Board (IRB).
Subjects
Subjects were recruited from two carrier air wing MH-60R squadrons located at Naval Air Station Jacksonville. These carrier air wing squadrons were selected to control for size (number of aircrew), age, and operational tempo (number of flight hours). Subjects consisted of both pilots and enlisted aircrew. One squadron was designated as the control group, although the second squadron served as the intervention group. Aircrew of each squadron were presented information of the study and given the opportunity to participate voluntarily. For inclusion in the study, subjects were required to be qualified for flight duties by medical authorities (i.e., in an “up” aeromedical status). Any subject not medically qualified to perform flight duties (i.e., in a “down” aeromedical status) was excluded from the study. The medical “down” status could be for a portion or the entirety of the study. There were no other inclusion or exclusion criteria for this pilot study. Subjects from both squadrons were encouraged to complete the anonymous questionnaire both preflight and postflight.
Questionnaire
The pain questionnaire included aircrew demographics used to generate an anonymous subject identification. Data elements collected include whether PPS was performed, the questionnaire was completed preflight or postflight, flight length in hours, and the subject’s pain assessment.
The pain questionnaire provided a visual representation of the Universal Pain Assessment Tool (UPAT), which is utilized globally in the medical field. The UPAT was used to rate patients’ pain by having them choose a number between 0 and 10. To assist in the pain rating, the UPAT includes a verbal descriptor scale, the Wong–Baker Facial Grimace Scale, and activity tolerance. The verbal descriptor scale explains that no pain is a 0 and worst possible pain is a 10. The Wong–Baker Facial Grimace Scale ranges from 0, which is alert/smiling, through 10, which is eyes closed/crying. The activity tolerance ranged from no pain through bed-rest required.
The questionnaire provides a schematic of the spine with a posterior view and a lateral view.25 The spine schematic was divided into cervical (neck), thoracic (mid back), lumbar (low back), and sacral (buttocks) regions. This section also had a table that asked them to rate their subjective pain from 0 to 10 based on the UPAT. An additional row allowed the aircrew to write in additional areas of pain (e.g., knee). The purpose of this additional row was to track second-order pain for future studies.
Procedures
On the day of each flight event, the aircrew first conducted their preflight brief. Next, subjects from both the intervention and control groups filled out the questionnaire. Only the intervention group completed the PPS protocol immediately after completing the questionnaire and before departing the squadron spaces for the aircraft outside. Upon landing, the aircrew completed a postflight debrief. Only the intervention group completed the PPS protocol after debrief. Both the intervention and control groups once again completed the questionnaire.
Intervention
The intervention squadron received a PPS “starter kit” consisting of three foam rollers, three yoga mats, and three yoga straps, along with an in-person demonstration and video detailing proper PPS execution and technique. The intervention squadron was also issued handouts and electronic copies of the PPS protocol (Figs. 1 and 2).
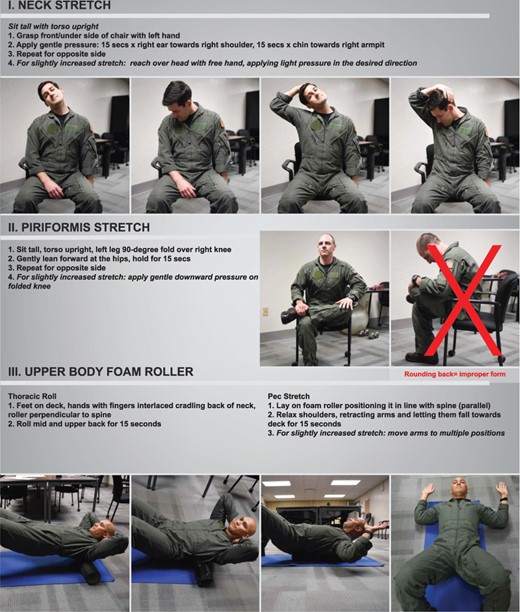
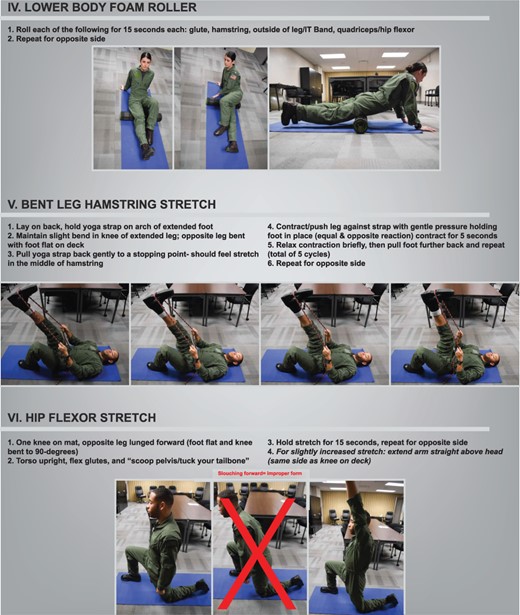
Preflight/postflight stretches consisted of six sections based on anonymous surveys of the U.S. Naval helicopter community and previous neck pain and LBP research. The first section included common neck and trapezius stretches designed to combat the stress placed on the neck by the helmet and night vision devices. The second section targeted the piriformis muscle. Poor posture and ergonomics can put pressure on the piriformis muscles and can affect the sciatic nerve. The seated position was chosen rather than supine techniques to increase stability and to allow for a deeper stretch. The third section utilized a foam roller for SMR of the thoracic region in combination with a pectoral stretch. The purpose of the SMR of the thoracic region is to counter poor posture or “helo hunch” by reducing restrictive barriers and fibrous adhesions.20,22 The pectoral stretch was included as that region tends to be restricted in the “helo hunch” position and worsened with the flight vest. The fourth section consisted of SMR using the foam roller on leg and gluteal muscles.20,22,24 While still on the floor, the fifth section stretched the hamstrings with the yoga strap utilizing the muscle energy/contract–relax method. The muscle energy technique was chosen as the subject could perform the stretch individually and muscle energy has shown to improve hamstring flexibility.19 The sixth section was a hip flexor stretch. This stretch was chosen to increase hip flexor ROM and to improve LBP by counteracting the subjects’ hip flexion position from sitting in flight.26 The kneeling position was chosen rather than the standing for increased stability while performing the stretch.
Statistical Analysis
Standard descriptive statistics were calculated. The Kolmogorov–Smirnov test determined parametric distributions, and the t-test or Mann–Whitney was used accordingly. Associations between PPS being performed and the flight groups were tested using Fisher’s exact. All analyses were conducted using IBM SPSS Statistics for Windows, Version 24.0. Armonk, NY: IBM Corp. Testing had to reach two-sided alpha of .05% in order to be deemed statistically significant.
RESULTS
A total of 243 questionnaires were collected over the 4-week study. Three questionnaires were excluded because of incomplete information. The 140 preflight and 100 postflight questionnaires were matched by subject ID and flight date, resulting in 88 matched responses. There were 54 matched responses from the control group and 34 from the intervention group. From these, it was determined that there were 42 subjects, of which 20 (47.60%) responded once, 9 (21.43%) responded twice, 7 (16.67%) responded three times, and the remaining 6 (14.30%) subjects responded four to six times during this period.
Flight length was reported in 44 (50%) of the 88 questionnaires or 22 from each group. As these were standard flights, the average length of time was approximately 4 h. This was confirmed by the summary data, in which the control average (SD) length of time = 3.82 (0.664), the intervention average (SD) length of time = 3.91 (0.526), and the t-test showed no statistically significant difference.
In the questionnaire, each question ascertained the comfort level for the five different anatomical regions that may be affected by flight, as well as one for overall pain. For each question, the amount of change between subject preflight- and postflight-reported pain scores was calculated. These pre-to-post-flight pain differences were found to be nonparametric (P < .001). Comparisons were conducted between the control group using the Mann–Whitney test. In addition, a YES/NO indicator was created to reflect whether the subject pain level had worsened postflight, based on these change amounts. This was then evaluated with Fisher’s exact test (Supplemental Table 1).
The Mann–Whitney test determined that the preflight and postflight overall (P ≤ .001), cervical (P ≤ .001), thoracic (P = .006), and lumbar (P = .004) differences between the control and intervention groups were statistically significant (Fig. 3 and Table I). Preflight and postflight pain differences in the sacral region and “other” sections were not found to be statistically significant. When evaluating pain level postflight, 13 (38.2%) of the intervention group were found to have the same or an improved level of pain, compared to only 4 (7.4%) of the control group. Testing this with the Fisher’s exact test, there was a significant association between overall pain level and PPS performed, P = .001. The Fisher’s exact test found the association between performing PPS and the change in pain level to be statistically significant (P = .001). Therefore, we can confidently accept the hypothesis that PPS will mitigate some of the pain found in the aircrew in regard to the pain overall and in the cervical, thoracic, and lumbar regions.
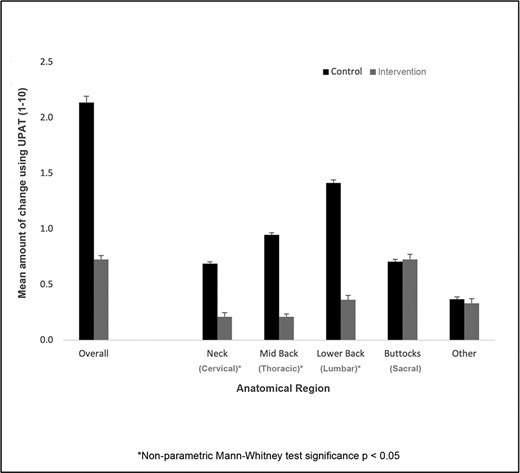
Mean amount of change utilizing the Universal Pain Assessment Tool.
Preflight, Postflight, and Change in Pain Scores Utilizing the Universal Pain Assessment Tool
| . | Control group (n = 54) . | Intervention group (n = 34) . | ||||
|---|---|---|---|---|---|---|
| Fields | Mean | Median | Std. Dev | Mean | Median | Std. Dev |
| Preflight overall | 1.26 | 1 | 1.53 | 1.91 | 2 | 1.40 |
| Preflight neck | 0.59 | 0 | 1.12 | 0.94 | 0 | 1.43 |
| Preflight mid back | 0.76 | 0 | 1.10 | 0.76 | 0 | 1.13 |
| Preflight lower back | 0.67 | 0 | 1.18 | 1.56 | 1 | 1.52 |
| Preflight buttocks | 0.24 | 0 | 0.78 | 0.44 | 0 | 1.05 |
| Preflight other | 0.35 | 0 | 0.95 | 0.38 | 0 | 0.79 |
| Postflight overall | 3.13 | 3 | 2.21 | 2.71 | 3 | 1.38 |
| Postflight neck | 1.30 | 0 | 1.56 | 1.15 | 0.5 | 1.44 |
| Postflight mid back | 1.68 | 1 | 1.76 | 1.00 | 0 | 1.48 |
| Postflight lower back | 1.94 | 1.5 | 1.97 | 1.94 | 2 | 1.67 |
| Postflight buttocks | 0.89 | 0 | 1.34 | 1.21 | 1 | 1.49 |
| Postflight other | 0.74 | 0 | 1.55 | 0.79 | 0 | 1.47 |
| Change overall* | 2.00 | 2 | 1.90 | 0.68 | 1 | 1.31 |
| Change neck* | 0.73 | 0 | 0.94 | 0.22 | 0 | 0.87 |
| Change mid back* | 1.00 | 1 | 1.23 | 0.38 | 0 | 1.39 |
| Change lower back* | 1.33 | 1 | 1.37 | 0.75 | 0 | 1.57 |
| Change buttocks | 0.67 | 0 | 1.25 | 0.34 | 0 | 1.36 |
| Change other | 0.39 | 0 | 1.33 | 0.79 | 0 | 1.47 |
| . | Control group (n = 54) . | Intervention group (n = 34) . | ||||
|---|---|---|---|---|---|---|
| Fields | Mean | Median | Std. Dev | Mean | Median | Std. Dev |
| Preflight overall | 1.26 | 1 | 1.53 | 1.91 | 2 | 1.40 |
| Preflight neck | 0.59 | 0 | 1.12 | 0.94 | 0 | 1.43 |
| Preflight mid back | 0.76 | 0 | 1.10 | 0.76 | 0 | 1.13 |
| Preflight lower back | 0.67 | 0 | 1.18 | 1.56 | 1 | 1.52 |
| Preflight buttocks | 0.24 | 0 | 0.78 | 0.44 | 0 | 1.05 |
| Preflight other | 0.35 | 0 | 0.95 | 0.38 | 0 | 0.79 |
| Postflight overall | 3.13 | 3 | 2.21 | 2.71 | 3 | 1.38 |
| Postflight neck | 1.30 | 0 | 1.56 | 1.15 | 0.5 | 1.44 |
| Postflight mid back | 1.68 | 1 | 1.76 | 1.00 | 0 | 1.48 |
| Postflight lower back | 1.94 | 1.5 | 1.97 | 1.94 | 2 | 1.67 |
| Postflight buttocks | 0.89 | 0 | 1.34 | 1.21 | 1 | 1.49 |
| Postflight other | 0.74 | 0 | 1.55 | 0.79 | 0 | 1.47 |
| Change overall* | 2.00 | 2 | 1.90 | 0.68 | 1 | 1.31 |
| Change neck* | 0.73 | 0 | 0.94 | 0.22 | 0 | 0.87 |
| Change mid back* | 1.00 | 1 | 1.23 | 0.38 | 0 | 1.39 |
| Change lower back* | 1.33 | 1 | 1.37 | 0.75 | 0 | 1.57 |
| Change buttocks | 0.67 | 0 | 1.25 | 0.34 | 0 | 1.36 |
| Change other | 0.39 | 0 | 1.33 | 0.79 | 0 | 1.47 |
*The Mann–Whitney test statistical significance P < .05.
Abbreviations: Std. Dev, standard deviation.
Preflight, Postflight, and Change in Pain Scores Utilizing the Universal Pain Assessment Tool
| . | Control group (n = 54) . | Intervention group (n = 34) . | ||||
|---|---|---|---|---|---|---|
| Fields | Mean | Median | Std. Dev | Mean | Median | Std. Dev |
| Preflight overall | 1.26 | 1 | 1.53 | 1.91 | 2 | 1.40 |
| Preflight neck | 0.59 | 0 | 1.12 | 0.94 | 0 | 1.43 |
| Preflight mid back | 0.76 | 0 | 1.10 | 0.76 | 0 | 1.13 |
| Preflight lower back | 0.67 | 0 | 1.18 | 1.56 | 1 | 1.52 |
| Preflight buttocks | 0.24 | 0 | 0.78 | 0.44 | 0 | 1.05 |
| Preflight other | 0.35 | 0 | 0.95 | 0.38 | 0 | 0.79 |
| Postflight overall | 3.13 | 3 | 2.21 | 2.71 | 3 | 1.38 |
| Postflight neck | 1.30 | 0 | 1.56 | 1.15 | 0.5 | 1.44 |
| Postflight mid back | 1.68 | 1 | 1.76 | 1.00 | 0 | 1.48 |
| Postflight lower back | 1.94 | 1.5 | 1.97 | 1.94 | 2 | 1.67 |
| Postflight buttocks | 0.89 | 0 | 1.34 | 1.21 | 1 | 1.49 |
| Postflight other | 0.74 | 0 | 1.55 | 0.79 | 0 | 1.47 |
| Change overall* | 2.00 | 2 | 1.90 | 0.68 | 1 | 1.31 |
| Change neck* | 0.73 | 0 | 0.94 | 0.22 | 0 | 0.87 |
| Change mid back* | 1.00 | 1 | 1.23 | 0.38 | 0 | 1.39 |
| Change lower back* | 1.33 | 1 | 1.37 | 0.75 | 0 | 1.57 |
| Change buttocks | 0.67 | 0 | 1.25 | 0.34 | 0 | 1.36 |
| Change other | 0.39 | 0 | 1.33 | 0.79 | 0 | 1.47 |
| . | Control group (n = 54) . | Intervention group (n = 34) . | ||||
|---|---|---|---|---|---|---|
| Fields | Mean | Median | Std. Dev | Mean | Median | Std. Dev |
| Preflight overall | 1.26 | 1 | 1.53 | 1.91 | 2 | 1.40 |
| Preflight neck | 0.59 | 0 | 1.12 | 0.94 | 0 | 1.43 |
| Preflight mid back | 0.76 | 0 | 1.10 | 0.76 | 0 | 1.13 |
| Preflight lower back | 0.67 | 0 | 1.18 | 1.56 | 1 | 1.52 |
| Preflight buttocks | 0.24 | 0 | 0.78 | 0.44 | 0 | 1.05 |
| Preflight other | 0.35 | 0 | 0.95 | 0.38 | 0 | 0.79 |
| Postflight overall | 3.13 | 3 | 2.21 | 2.71 | 3 | 1.38 |
| Postflight neck | 1.30 | 0 | 1.56 | 1.15 | 0.5 | 1.44 |
| Postflight mid back | 1.68 | 1 | 1.76 | 1.00 | 0 | 1.48 |
| Postflight lower back | 1.94 | 1.5 | 1.97 | 1.94 | 2 | 1.67 |
| Postflight buttocks | 0.89 | 0 | 1.34 | 1.21 | 1 | 1.49 |
| Postflight other | 0.74 | 0 | 1.55 | 0.79 | 0 | 1.47 |
| Change overall* | 2.00 | 2 | 1.90 | 0.68 | 1 | 1.31 |
| Change neck* | 0.73 | 0 | 0.94 | 0.22 | 0 | 0.87 |
| Change mid back* | 1.00 | 1 | 1.23 | 0.38 | 0 | 1.39 |
| Change lower back* | 1.33 | 1 | 1.37 | 0.75 | 0 | 1.57 |
| Change buttocks | 0.67 | 0 | 1.25 | 0.34 | 0 | 1.36 |
| Change other | 0.39 | 0 | 1.33 | 0.79 | 0 | 1.47 |
*The Mann–Whitney test statistical significance P < .05.
Abbreviations: Std. Dev, standard deviation.
DISCUSSION
In order to fly an aircraft, pilots and aircrew perform extensive pre- and post-flight inspections of the aircraft to ensure its safety and material readiness for flight. Similar to an aircraft, the human body is a complex system that should be sustained with pre- and post-flight maintenance. This study did replicate that flying in a helicopter causes back and neck pain as previously documented.1–5 Thus, the PPS protocol was designed to support a culture of body maintenance to sustain a career in aviation with reduced pain and injury. As significant pre-to-post-flight differences were observed in overall pain, as well as in the cervical, thoracic, and lumbar regions, this pilot study suggests that PPS, a simple 5- to 7-min stretching routine, may reduce postflight cervical, thoracic, lumbar, and overall pain related to helicopter flight.
The lack of in-flight pain assessment is a limitation to this study. The provided questionnaire asks for preflight and postflight pain levels. However, it does not ask for in-flight pain levels. An in-flight questionnaire or pain analysis would require an increased acceptance of risk on behalf of the participant and would require tasking outside of their normal flight duties. This increased risk was determined to be too high for the purposes of this study. An additional limitation is the nature of self-reported subjective pain and the effect of recall bias for the subjects. All of the training events were flown in one single type of aircraft platform (MH-60R) in the same geographical location (east coast), contributing to selection bias.
Restricted ROM in the neck, back, and hips has shown to be related to pain.21,26 Whether functional ROM was increased by PPS was not a part of this study. Moreover, it is unclear whether the reduction in subjective ratings of pain pre- and post-flight were because of a possible increase in ROM or because of an increase in awareness of body position and posture, and there could have been a placebo effect on the subjects in the intervention group. Finally, the control and intervention groups had differing baseline pain averages. This could be attributed to the squadrons being on different operational phases and thus having different outside stressors. Stressors could potentially exacerbate any existing pain in the subjects.
Future studies will include longer study time, increased sample size, and collection of information such as age, gender, crew position, flight history, smoking status, history of back pain, and recent use of analgesics. Additionally, PPS will be adjusted toward specific aviation platforms and modified for the regions that did not achieve statistical significance (e.g., sacral region). Future phases will also include measurements of spine ROM and in-flight posture using both analog and electronic devices.
Recent clinical guidelines as listed through the American College of Physicians have emphasized the importance of a non-pharmacological approach to management of patient pain.18 The prehabilitation aspect of the PPS protocol reduces conventional medical intervention and pharmacological management of back pain. As previously discussed, LBP is one of the most consistently documented types of back pain in rotary aircrew, with perceived negative effects on in-flight situational awareness.2,7,9 Although designed for helicopter aircrew, the present PPS protocol could easily be utilized by other military and civilian communities (fighter, turboprop, tilt rotor, etc.). The PPS protocol promotes a prehabilitation model for all aviation populations.
Losing flight hours because of back pain has a financial cost and the protocol could increase mission readiness by reducing lost flights because of back-related injuries. The financial investment in training aircrew is significant, but increasing physical readiness increases manpower readiness. However, back pain also has a human cost. The reduction in treatment costs for aircrew, and even more importantly—the reduced attrition of highly trained personnel—is a tangible return on the small investment of time and effort associated with the PPS protocol. Reducing back pain for aircrew can enable a lifetime of service.
CONCLUSION
Aircrew back and neck pain because of flying is well documented. However, in U.S. Naval Aviation, there is no standardized stretching protocol for aircrew to perform immediately pre- or post-flight. This study demonstrated that PPS, a simple 5- to 7-min stretching routine, gives aircrew structure and can reduce postflight cervical, thoracic, lumbar, and overall pain. This phase proved to be safe as no adverse events were reported. The prehabilitation aspect could reduce conventional medical intervention, reduce costly pharmacological management of neck and back pain, and be applied to other aviation populations in military and civilian communities.
ACKNOWLEDGMENTS
The authors would like to acknowledge Almer B. Mendoza of Naval Hospital Jacksonville for his contributions to the project. (Permission obtained from the person named in the Acknowledgment.)
SUPPLEMENTARY MATERIAL
Supplementary Material is available at Military Medicine online.
FUNDING
Funded by U.S. Navy.
CONFLICT OF INTEREST STATEMENT
None declared.
CLINICAL TRIAL REGISTRATION
Not applicable; not necessary per Naval Medical Center Portsmouth IRB.
INSTITUTIONAL REVIEW BOARD (HUMAN SUBJECTS)
This study was approved by the Naval Medical Center, Portsmouth, VA IRB (NHJX.2019.0100) in compliance with all applicable federal regulations governing the protection of human subjects. Research data derived from an approved Naval Medical Center, Portsmouth, VA IRB.
INSTITUTIONAL ANIMAL CARE AND USE COMMITTEE (IACUA)
Not applicable.
INDIVIDUAL AUTHOR CONTRIBUTION STATEMENT
J.B.W. and M.R.W. designed the stretching protocol. J.B.W., G.C.A., C.L.H., and H.M.S. designed the research. J.B.W., M.R.W., and G.C.A. drafted the original manuscript. G.C.A. collected the data. A.F.M. analyzed the data. C.L.H., H.M.S., and A.F.M. reviewed and edited the manuscript. All authors read and approved the final manuscript. All authors have provided consent for publication.
DATA AVAILABILITY
The data that support the findings of this study are available from the corresponding author, upon reasonable request.
INSTITUTIONAL CLEARANCE
Institutional clearance approved.
REFERENCES
Author notes
Walsh J, Armas G, Church A, Hardy C, Le P, McGlynn A, Pickerill G, Wright M. (May 2022). Pre-flight and Postflight Stretches (PPS): An approach to mitigating back pain and neck pain in the helicopter community (Phase 1 and 2). Naval Medical Center Portsmouth IRB protocol approved. Presentation for Navy-Wide 2022 Academic Research Competition, San Diego, CA.
Honorable Mention; Category 1A (Staff IRB Clinical Research conducted under the jurisdiction of the Clinical Investigation Department)
Walsh J, Armas G, Church A, Hardy C, Le P, McGlynn A, Pickerill G, Wright M. (May 2022). Pre-flight and Postflight Stretches (PPS): An approach to mitigating back pain and neck pain in the helicopter community (Phase 1 and 2). Naval Medical Center Portsmouth IRB protocol approved. Presentation for 37th Annual Naval Medical Forces Atlantic Academic Research Competition Naval Medical Center Portsmouth, Portsmouth, VA.
1st Place; Category 1A (Staff IRB Clinical Research conducted under the jurisdiction of the Clinical Investigation Department)
Walsh J, Armas G, Church A, Hardy C, Le P, McGlynn A, Pickerill G, Wright M. (August 2021). Pre-flight and Post-flight Stretches (PPS): An approach to mitigating back pain and neck pain in the helicopter community (Phase 1 and 2). Naval Medical Center Portsmouth IRB protocol approved. Main Stage Presentation for Aerospace Medical Association 91st Annual Scientific Meeting, Denver, CO.
Finalist for being in the top 5% of the performances from a field of 153 contestants; Space Medicine Association Jeff Myers Young Investigator Award Competition.
Walsh J, Armas G, Hardy C, Mendoza A, McGlynn A, Sulpizio H, Wright M. (March 2021). Pre-flight and Postflight Stretches (PPS): An approach to mitigating back pain and neck pain in the helicopter community (Phase 1). Naval Medical Center Portsmouth IRB protocol approved. Poster presented in the Rise with Research at the 2021 Uniformed Services Academy of Family Physicians Annual Meeting, Virtual.
The authors are military service members or employees of the Federal Government. This work was prepared as part of official duties. Title 17 U.S. code 105 provides that “Copyright protection under this title is not available for any work of the United States Government.” Title 17 U.S. code 101 defines a U.S. Government work as a work prepared by a military service member or employee of the U.S. Government as part of that person’s official duties.
The views expressed are solely those of the authors and do not reflect the official policy or position of the U.S. Army, U.S. Navy, U.S. Air Force, the DoD, or the U.S. Government.



