-
PDF
- Split View
-
Views
-
Cite
Cite
Steven J Hadeed, Katherine M Broadway, Kierstyn T Schwartz-Watjen, Bersabeh Tigabu, Ashley J Woodards, Anna L Swiatecka, Akeisha N Owens, Aiguo Wu, Notional Spread of Cholera in Haiti Following a Natural Disaster: Considerations for Military and Disaster Relief Personnel, Military Medicine, Volume 188, Issue 7-8, July/August 2023, Pages e2074–e2081, https://doi.org/10.1093/milmed/usac415
Close - Share Icon Share
ABSTRACT
Cholera remains a significant public health threat for many countries, and the severity largely varies by the population and local conditions that drive disease spread, especially in endemic areas prone to natural disasters and flooding. Epidemiological models can provide useful information to military planners for understanding disease spread within populations and the effectiveness of response options for preventing the transmission among deployed and stationed personnel. This study demonstrates the use of epidemiological modeling to understand the dynamics of cholera transmission to inform emergency planning and military preparedness in areas with highly communicable diseases.
Areas with higher probability for a potential cholera outbreak in Haiti followed by a natural disaster were identified. The hotspots were then used to seed an extended compartmental model, EpiGrid, to simulate notional spread scenarios of cholera originating in three distinct areas in Haiti. Disease parameters were derived from the 2010 cholera outbreak in Haiti, and disease spread was simulated over a 12-week period under uncontrolled and controlled spread.
For each model location, scenarios of mitigated (intervention with 30% transmission reduction via international aid) and unmitigated (without intervention) are simulated. The results depict the geographical spread and estimate the cumulative cholera infection for each notional scenario over the course of 3 months. Disease transmission differs considerably across origin site with an outbreak originating in the department of Nippes spanning the largest geographic area and resulting in the largest number of cumulative cases after 12 weeks under unmitigated (79,518 cases) and mitigated (35,667 cases) spread scenarios.
We modeled the notional re-emergence and spread of cholera following the August 2021 earthquake in Haiti while in the midst of the global COVID-19 pandemic. This information can help guide military and emergency response decision-making during an infectious disease outbreak and considerations for protecting military personnel in the midst of a humanitarian response. Military planners should consider the use of epidemiological models to assess the health risk posed to deployed and stationed personnel in high-risk areas.
INTRODUCTION
Cholera is an acute waterborne disease caused by the infection of the intestine from the pathogenic bacteria Vibrio cholerae.1 Globally, roughly 1.3 to 4.0 million cases and 21,000 to 143,000 deaths occur each year.2,3 However, the majority of individuals experience little to mild symptoms and often go unreported, with official cases accounting for 5% to 10% of actual cases.4,5 Roughly 10% of all people infected will develop severe symptoms characterized by profuse diarrhea and bacterial shedding.1
Cholera remains a serious public health burden for many countries across the globe and is often a function of low socioeconomic status and inadequate infrastructure of impoverished nations. Poor sanitation continues to be the major driver of cholera transmission in endemic areas. Even with proper sanitation, extreme flooding and natural disasters can severely damage local infrastructure and displace a large number of people living in suboptimal conditions.
The 2010 earthquake in Haiti devastated the country, killing roughly 230,000 people and injuring more than 300,000 people.6–8 Many of the homes and infrastructure around Port-au-Prince and the surrounding areas were destroyed, displacing hundreds of thousands of people to various parts of the country.9 Humanitarian efforts began shortly after the disaster with the arrival of international aid and additional support personnel from the United Nations Stabilization Mission in Haiti as part of further recovery and response efforts.10
As part of the United Nations Stabilization Mission, Vibrio cholerae O1 was unintentionally introduced into the country by Nepalese soldiers.7 This marked the first arrival of cholera in over a century,10,11 leading to one of the largest cholera outbreaks that resulted in over 800,000 cases and more than 10,000 deaths.7,8,12
Cholera has since become endemic in Haiti and has spread to the surrounding countries of the Dominican Republic and Cuba;13 however, no laboratory-confirmed cases have been reported in Haiti since the early 2019.14 This success is largely attributed to improvements in infrastructure, sanitation, and health surveillance.8 Despite these recovery efforts, the risk of cholera re-emergence still exists should Haiti experience another catastrophic natural disaster and disruption to sanitation infrastructure.
The emergence of diarrheal diseases following natural disasters and during humanitarian crisis has been well documented.3 Pakistan experienced a large outbreak (n > 750) of acute watery diarrhea in an unplanned refugee camp of 1,800 people following a 2005 earthquake.15 A cyclone and tidal surge in the island of Sandwip off the coast of Bangladesh resulted in a devastating cholera epidemic causing over 12,000 cases and 51 deaths.16 Severe flooding in the West Bengal district of Malda was followed weeks later by an explosive cholera epidemic that resulted in over 16,000 cases and 276 deaths.17 The 2016 cholera outbreak in Yemen during the country’s on-going civil war lasted nearly 5 years and caused more than 2.5 million suspected and confirmed cases and resulted in around 4,000 deaths.18
The 2010 Haiti cholera outbreak was an unfortunate example for how a natural disaster in a vulnerable nation can be compounded by the introduction of a highly transmissible pathogen and also foreshadows the potential risks faced by nations in similar situations. Identifying vulnerable areas and evaluating the effectiveness of public health interventions are important for guiding response efforts in resource-limited areas following a natural disaster.
The most recent devastation from the 2021 magnitude 7.2 earthquake and tropical storm Grace left Haiti at risk for the possible re-emergence of cholera and other waterborne diseases, made worse by the COVID-19 pandemic. Shortly after the earthquake in the three most affected departments in southwestern Haiti, it was estimated that roughly 60% of the population did not have access to potable water and more than half a million children were at risk of waterborne diseases.19 Additionally, the earthquake severely damaged 56 piped water systems in the area and caused minor damages to more than 1,800 water systems.20 The World Food Program estimates that over three-quarters of the population in the affected areas live below the poverty line.21 The World Bank estimates that 96% of the Haitian population are at risk for natural disasters (hurricanes, earthquakes, and floods), which are expected to occur in greater frequency and severity under future climate changes.22
A large number of displaced people are still in need of appropriate housing. Following Hurricane Mathew in 2016, more than 140,000 displaced families are still in need of permanent housing. Nearly 33,000 people remain in temporary housing following the 2010 earthquake, and over 300,000 people live in informal housing settlements.23 An additional 12,000 people were displaced in 2020 due to gang violence and cyclones.23 Furthermore, access to clean and safe drinking water remains a significant challenge and hampers efforts to combat waterborne diseases as one-third of the Haitian population lack basic water services and access to potable water, and two-thirds of the population have limited or no access to sanitation services.14
COVID-19 has complicated efforts to address waterborne diseases and recovery efforts. Much of the countries’ limited resources have been allocated away from public health efforts to address communicable diseases toward fighting COVID-19, which can impede the progress against other diseases, including cholera.
The concurrent spread of an acute diarrheal and respiratory disease during a natural disaster is a likely future scenario faced by many developing nations that are already struggling to provide basic services and standards of living. Modeling various cholera transmission scenarios and evaluating the effectiveness of timely response efforts can inform international aid organizations supporting public health preparedness and response efforts in the country.
Military bases located in endemic areas following natural disaster must consider the health risk posed to stationed personnel and potential disruption to operations should a highly communicable disease outbreak occur in the local population. Diarrheal diseases have the potential to inhibit a soldier’s ability to fight and degrade their lethality for extended periods of time. During the Vietnam War, diarrheal illness was the most burdensome disease, nearly four times the incidence of malaria. Additionally, during Operation Desert Shield/Storm, more than half of soldiers reported a diarrheal episode and 20% were unable to perform their duties.24
Following a natural or man-made disaster, many nations offer to provide resources and deploy military personnel to assist with response and recovery efforts. Occasionally, the U.S. Department of Defense deploys personnel to disaster areas as part of their humanitarian assistance programs.25 Military personnel stationed or responding in relief efforts in endemic areas with displaced populations and poor infrastructure should consider the local conditions and transmission dynamics unique to the area when assessing the risk to deployed personnel and necessary steps for preventing exposure and disease.
Often cholera and other diarrheal illnesses go underreported, and the true disease burden and risk to military personnel are uncertain, which can complicate the response planning and disease prevention. It is estimated that diarrheal diseases can result in 3 to 10 days in lost productivity and limit the ability of service members to complete their duties.26 Diarrheal diseases continue to remain a public health threat to the general public but also to military units deployed across a range of environments.
In this article, we model a “notional” scenario in which cholera was to hypothetically re-emerge following the August 2021 earthquake and tropical storm in Haiti while in the midst of the global COVID-19 pandemic. We then examine various factors that may limit an effective response effort to mitigate disease transmission. This information can help guide military decision-making and humanitarian response during an infectious disease outbreak following a natural disaster and considerations for protecting military personnel in the midst of a humanitarian response.
MATERIALS AND METHODS
Identification of Affected Areas and Hotspots
Infrastructure damage from the August 14, 2021, magnitude 7.2 earthquake in Haiti and subsequent flooding from tropical storm Grace (August 16, 2021) impacted the drinking water quality, increasing the potential for cholera outbreaks. As part of an international response, foreign nationals arrive in Haiti days after the earthquake to aid in response and recovery efforts.
Hotspot regions were identified within the administrative departments of Nippes, Sud, and Grand’Anse impacted by the earthquake and heavy rains (Fig. 1). Lakes, river, and coastal region intersections with high population areas were used to identify the areas with high probability of cholera outbreak. The publically available data products, Terra ASTER Global Digital Elevation Model27 and HOTOSM Waterways dataset,28 were used to define water-impacted regions.
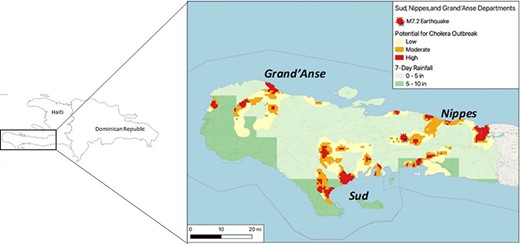
Cholera hotspot regions were identified based on areas of population density, proximity to potentially flooded waterways, and 7-day total rainfall data in Haiti.
The WorldPop 1-km gridded population density was used to determine the total population within the identified areas.29 Post-earthquake, NASA Global Precipitation Measurement 7-day rainfall accumulation was used for flooding impact.30 Population within 1 to 2 km of the potentially impacted waters were identified, and the affected regions were ranked based on population density, rainfall accumulation, and proximity to waterways. The highest ranked location from each of the three affected departments was used to seed the epidemiological model. In the notional scenario, an asymptomatic infected emergency response worker arrives in Haiti, serving as the index case. Each of the affected administrative departments was seeded based on the presumed arrival of this index case, in each department.
EpiGrid: Extended Compartmental Model, Specific Features, and Modifiable Parameters
EpiGrid31 is a geographically resolved compartmental model of disease progression and epidemic spread capable of deterministically or stochastically simulating a variety of diseases and their spread mechanism. In each geographical pixel, unmitigated disease progression is modeled starting from a susceptible state S and proceeding through presymptomatic, symptomatic, and severely ill states. For each unmitigated disease state, there is a corresponding mitigated disease progression state with progression rates differentiated by administrative district to reflect various local measures to control contagion and improve disease outcomes. The end states of the disease progression are the recovered and dead states. The model allows for recovery without passing through the severe disease state. Additionally, the population can be vaccinated, reflected in two successive states corresponding to an initially vaccinated and mature immune response. Contagion occurs from sick to susceptible population; the within-pixel contribution is the only well-mixed part; geographical spread of disease between pixels also occurs by several mechanisms. In this work, we modeled geographic spread of disease arising from two contributions, first, as locally diffusive spread of contagion with gravity weighting by the population in pixels and, second, as unidirectional travel of contagion along the major branches of the river system in Haiti, thus moving between geographical pixels. A cholera model initially developed by Los Alamos National Laboratories using R-programming and parameterized from the 2010 cholera outbreak in Haiti was used as the starting parameterization in this notional scenario. Details of this modeling tool have been discussed previously.31,32
Specific Model Parameters
The narrative of this notional scenario and the disease parameters are based off of the 2010 cholera outbreak with the added constraints of the COVID-19 pandemic, tropical storm Grace, and social unrest affecting response efforts and disease transmission (Table S1). The model started on August 20, 2021 (day 0), with the importation of an infected humanitarian relief worker. We modeled the spread of cholera under three identical but geographically distinct origin scenarios starting in Jeremie (Grand’Anse), Les Cayes (Sud), or Miragoane (Nippes) in the southern claw region of the island. All three scenarios start with the arrival of an infected relief worker (index case) who sheds V. cholerae in their feces. An open septic pit at a humanitarian camp is dumped into local waterways, resulting in environmental contamination and the initial source of transmission. Transmission modifications are applied uniformly across all three locations (Table S2) to mirror the transmission dynamics that occurred in the 2010 Haiti outbreak with the exception of a large-scale intervention taking place on day 49 of the simulation to curtail transmission.
Movement of People
Following the destruction from the earthquake and deteriorating living conditions, we model the movement of people away from the affected areas near waterways toward the surrounding rural communes during the early phase of the model, similar to the displacement of people who fled the Artibonite delta in 2010 at the start of the epidemic.11 Starting on day 7, the distance traveled by people was increased from 2 to 6 km to represent the displacement of people away from the affected areas10 and was decreased back down to 2 km on day 25 once people had resettled. Displacement of people from urban to rural areas was modeled by setting gravity weighting to zero (Table S2).
Transmission from Waterways: Waterway/Rainfall
The 2021 earthquake was followed by tropical storm Grace 2 days later that increased rainfall and flooding. Tropical storm Grace resulted in approximately 10 inches of rainfall in the southwestern portion of Haiti,33 similar to levels of rainfall from hurricane Tomas in 2010.34 River transmission is incorporated into this model to represent the destruction of critical infrastructure and subsequent reliance on the river for water with improper sanitation.
Transmission Modification
Unmitigated cholera spread was modeled as a worst-case scenario for disease transmission in the absence of public health countermeasures and the persistent reliance on contaminated waterways. Public health response efforts were delayed in the model and did not take effect until 7 weeks (day 49) following the start of the outbreak, assuming Haiti had reduced capacity to respond due to resource constraints and being focused on addressing COVID-19. During the first 4 days of the outbreak, the transmission rate (beta) was increased by 700% to represent a rapid spread from a point source contamination comparable to the 2010 outbreak in Haiti (Table S2).
A systematic review by Fewtrell et al.35 found that sanitation services can reduce the risk of diarrheal disease transmission by 25% to 37%. Source-based interventions have been found to have a less effect at reducing diarrhea; however, interventions such as chlorination at the household level may reduce the risk of diarrhea by 23%, and flocculation and disinfection sachets can reduce the risk by 31%.36 Point-of-use (POU) filtration has been found to significantly reduce the risk of diarrheal disease (52%) with ceramic filters (61% reduction), sand filtration (53% reduction), and LifeStraw (31% reduction) being moderately effective.36 Solar disinfection by placing bottled water in direct sunlight for at least 6 hours reduced the risk of diarrheal disease by nearly one-third (38%).36
The transmission was modified over a 12-week projection period to represent changes in response efforts, health care, and improvement in access to potable water through boil advisories/hand hygiene and the distribution of POU filters and chlorination kits. Based on the previous studies, we estimate that the combined effects of these interventions would result in an overall reduction in disease transmission by 30%, starting on week 7 of the outbreak with the arrival of resources and partial restoration of transportation and distribution networks.
RESULTS
Geographic spread of cholera over a 12-week projection period was initiated in Jeremie in the department of Grand’Anse, Miragoane in the department of Nippes, and Les Cayes in the department of Sud (Fig. 2).
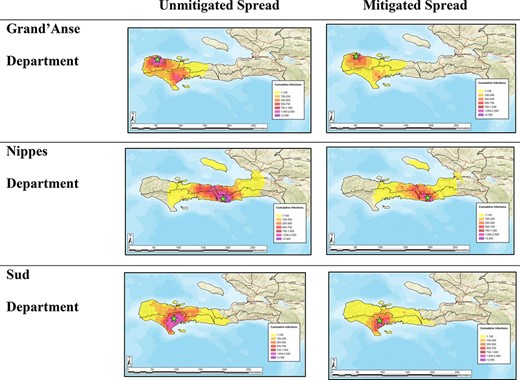
Cumulative geographic spread of cholera cases after 12 weeks with and without mitigations employed.
Grand’Anse Department
A cholera outbreak originating in Jeremie, Grand’Anse, is expected to be localized to the southwestern portion of the country (7,224 km2) and result in an estimated 58,742 total cases of cholera under unmitigated spread (Fig. 3A). The implementation of mitigation strategies on week 7 corresponding to a 30% reduction in transmission is expected to result in 13.3% fewer cases of cholera by week 8 and 42.5% and 61.9% fewer cases by weeks 10 and 12, respectively (Table I).
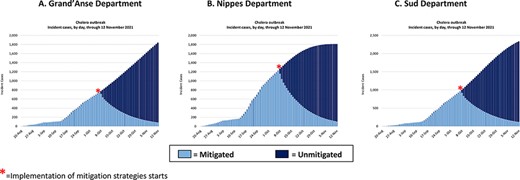
Estimated incident cases over 12 weeks, with the primary infection occurring in (A) Jeremie, Grand’Anse department, (B) Miragoane, Nippes department, and (C) Les Cayes, Sud department. * = Implementation of mitigation strategies starts.
Biweekly Predicted Number of Cumulative Cases in Both Unmitigated and Mitigated Scenarios Across Grand’Anse, Nippes, and Sud Department
| . | . | Grand’Anse department . | Nippes department . | Sud department . | |||
|---|---|---|---|---|---|---|---|
| Simulation week . | Date . | Unmitigated spread . | Mitigated spread . | Unmitigated spread . | Mitigated spread . | Unmitigated spread . | Mitigated spread . |
| 0 | August 20, 2021 | 0 | 0 | 0 | 0 | 0 | 0 |
| 2 | September 3, 2021 | 531 | 531 | 761 | 761 | 442 | 442 |
| 4 | September 17, 2021 | 2148 | 2148 | 3266 | 3266 | 2154 | 2154 |
| 6 | October 1, 2021 | 8168 | 8168 | 13,376 | 13,376 | 9408 | 9408 |
| 8 | October 15, 2021 | 19,218 | 16,666 | 31,230 | 27,310 | 23,787 | 20,410 |
| 10 | October 29, 2021 | 35,891 | 20,650 | 54,382 | 33,353 | 46,436 | 25,840 |
| 12 | November 12, 2021 | 58,742 | 22,364 | 79,518 | 35,667 | 76,561 | 28,225 |
| . | . | Grand’Anse department . | Nippes department . | Sud department . | |||
|---|---|---|---|---|---|---|---|
| Simulation week . | Date . | Unmitigated spread . | Mitigated spread . | Unmitigated spread . | Mitigated spread . | Unmitigated spread . | Mitigated spread . |
| 0 | August 20, 2021 | 0 | 0 | 0 | 0 | 0 | 0 |
| 2 | September 3, 2021 | 531 | 531 | 761 | 761 | 442 | 442 |
| 4 | September 17, 2021 | 2148 | 2148 | 3266 | 3266 | 2154 | 2154 |
| 6 | October 1, 2021 | 8168 | 8168 | 13,376 | 13,376 | 9408 | 9408 |
| 8 | October 15, 2021 | 19,218 | 16,666 | 31,230 | 27,310 | 23,787 | 20,410 |
| 10 | October 29, 2021 | 35,891 | 20,650 | 54,382 | 33,353 | 46,436 | 25,840 |
| 12 | November 12, 2021 | 58,742 | 22,364 | 79,518 | 35,667 | 76,561 | 28,225 |
Biweekly Predicted Number of Cumulative Cases in Both Unmitigated and Mitigated Scenarios Across Grand’Anse, Nippes, and Sud Department
| . | . | Grand’Anse department . | Nippes department . | Sud department . | |||
|---|---|---|---|---|---|---|---|
| Simulation week . | Date . | Unmitigated spread . | Mitigated spread . | Unmitigated spread . | Mitigated spread . | Unmitigated spread . | Mitigated spread . |
| 0 | August 20, 2021 | 0 | 0 | 0 | 0 | 0 | 0 |
| 2 | September 3, 2021 | 531 | 531 | 761 | 761 | 442 | 442 |
| 4 | September 17, 2021 | 2148 | 2148 | 3266 | 3266 | 2154 | 2154 |
| 6 | October 1, 2021 | 8168 | 8168 | 13,376 | 13,376 | 9408 | 9408 |
| 8 | October 15, 2021 | 19,218 | 16,666 | 31,230 | 27,310 | 23,787 | 20,410 |
| 10 | October 29, 2021 | 35,891 | 20,650 | 54,382 | 33,353 | 46,436 | 25,840 |
| 12 | November 12, 2021 | 58,742 | 22,364 | 79,518 | 35,667 | 76,561 | 28,225 |
| . | . | Grand’Anse department . | Nippes department . | Sud department . | |||
|---|---|---|---|---|---|---|---|
| Simulation week . | Date . | Unmitigated spread . | Mitigated spread . | Unmitigated spread . | Mitigated spread . | Unmitigated spread . | Mitigated spread . |
| 0 | August 20, 2021 | 0 | 0 | 0 | 0 | 0 | 0 |
| 2 | September 3, 2021 | 531 | 531 | 761 | 761 | 442 | 442 |
| 4 | September 17, 2021 | 2148 | 2148 | 3266 | 3266 | 2154 | 2154 |
| 6 | October 1, 2021 | 8168 | 8168 | 13,376 | 13,376 | 9408 | 9408 |
| 8 | October 15, 2021 | 19,218 | 16,666 | 31,230 | 27,310 | 23,787 | 20,410 |
| 10 | October 29, 2021 | 35,891 | 20,650 | 54,382 | 33,353 | 46,436 | 25,840 |
| 12 | November 12, 2021 | 58,742 | 22,364 | 79,518 | 35,667 | 76,561 | 28,225 |
Nippes Department
An outbreak originating in the department of Nippes in the city of Miragoane is expected to result in the greatest number of cholera infections, spanning the largest geographical area (11,757 km2) (Fig. 3B). An unmitigated outbreak is expected to result in 79,518 cumulative cases of cholera by week 12, while mitigated transmission will result in 55.1% fewer cumulative cases, totaling 35,667 cases (Table I).
Sud Department
An unmitigated cholera outbreak originating in the city of Les Cayes in the department of Sud is expected to span 8,774 km2 (Fig. 3C) and results in 76,561 total cases after 12 weeks. The implementation of mitigation strategies at week 7 is expected to result in 14.2% fewer cases by week 8, 44.4% fewer cases by week 10, and 63.1% less cases by week 12, totaling 28,225 cumulative cases (Table I).
DISCUSSION
Cholera remains a significant public health burden in many developing nations across the globe. Climate change is expected to exacerbate waterborne diseases through limited access to potable water, favorable growth conditions for pathogens, increasing frequency of natural disasters, and increasing population growth and informal housing settlements in densely populated urban settings. Natural disasters continue to occur in greater frequency worldwide, leading to mass population displacement, destruction of infrastructure, and transformation of the environment, resulting in a post-disaster phase where waterborne diseases, infectious spread, and epidemics occur.37
Diarrheal diseases remain a significant health threat to military readiness, with bacterial pathogens being the causative agent for the majority of cases.24 Diarrhea among military personnel closely resembles traveler’s diarrhea in the general public and the risk of which has been found to be similar among both long-term travelers and military personnel. The disease burden from diarrheal illness exceeded the burden from respiratory illness and injury during Operation Iraqi Freedom and Operation Enduring Freedom in delpoyed military personnel in which 76.8% and 54.4% of soldiers diarrheal reported symptoms, respectively.38 Although cholera has not been directly implicated in major outbreaks among military personnel, diarrheal diseases remain a significant public health threat in disaster and conflict areas that can significantly restrict operational capabilities and readiness of military units, especially when treatment options are not widely available.
Epidemiological models capturing disease spread can be used for planning purposes, situational awareness, and decision support. To aid in post-event natural disaster preparedness, we generated notional scenarios of cholera spread in Haiti following the earthquake in August 2021. Cholera remains a significant public health threat for many countries, especially in underdeveloped nations that are prone to natural disasters and flooding. A cholera outbreak in Haiti can have devastating effects on the local population, and the severity can largely be determined by the population and the local conditions that drive disease spread.
Our models show that notional epidemic spread and severity differ across outbreak locations, with an outbreak originating in department of Nippes estimated to result in the largest number of cholera cases and span the largest geographical area. Similarly, spread originating in the department of Sud is expected to reach a high number of cases similar to that in Nippes but over a smaller geographic area. The implementation of public health interventions corresponding to a reduction in disease transmission by 30% is expected to result in 43,851 (−55.1%) fewer cases in the department of Nippes and 48,336 (−63.1%) fewer cumulative cases in Sud department by week 12.
These notional modeling scenarios demonstrate the variability in disease transmission of cholera originating in different populations and locations in Haiti. Understanding the disease dynamics across high-risk regions and the effectiveness of timely public health interventions is important for emergency planning and response efforts by military personnel participating in humanitarian relief efforts. The allocation of POU filters and water treatment kits to access points throughout high-risk areas will allow public health interventions to be employed in a timely manner to minimize disease spread and maximize their effectiveness against cholera and other waterborne diseases following a natural disaster.
Our epidemiological model has many strengths, including the ability to incorporate transmission modifications to reflect government response and natural disease progression, time-varying public health interventions and medical treatment, and providing spatial and temporally resolved data. Despite these strengths, there are several limitations that include the reliance on past outbreaks to parameterize current or future models which may not be representative of the heterogeneity of disease parameters and the social and behavioral factors of the local population that drive transmission. Additionally, we assumed that an aggregate reduction in disease transmission from public health interventions was applied uniformly across the modeling areas which may not be reflective of real-world response or the efficacy of specific interventions.
Although cholera has not been reported in Haiti since 2019, the risk for epidemic spread remains possible as the pathogen is believed to have become endemic in coastal and brackish waters throughout the island. Climate change is expected to cause future sea level rise, warmer surface temperatures, salt water intrusion, flooding, and tropical storms, all of which may contribute to the re-emergence of cholera in Haiti. The frequent tropical storms and flooding throughout the island, and the delayed response and limited capacity of the country to respond effectively during and after a disaster event, make Haiti susceptible to future outbreaks.
Haiti has received large humanitarian aid to bolster the country’s ability to address the basic public health needs of the population, including access to safe drinking water and sanitation, but these efforts remain hindered by resource limitations. Epidemiological modeling can serve as a useful tool for identifying areas prone to natural disaster and disease spread and assessing the effects of public health interventions and the timing of these interventions on mitigating disease spread. This article demonstrates that the implementation of public health interventions, such as chlorination, POU filtration, promotion of hand hygiene, and boiling of water, can significantly reduce the number of infections and greatly limit disease spread. Additionally, the timing of interventions is critical for the effective public health response. Stockpiling of water purification kits in high-risk areas can greatly enhance preparedness and response efforts should a cholera outbreak occur in Haiti. Overall, the information gleaned from epidemiological modeling can greatly support planning, situational awareness, and operations during natural disasters.
ACKNOWLEDGMENTS
The authors would like to give many thanks to Maritime Planning Associates for supplying the cholera hotspot analysis and Los Alamos National Laboratory for support with the EpiGrid modeling tool.
SUPPLEMENTARY MATERIAL
SUPPLEMENTARY MATERIAL is available at Military Medicine online.
FUNDING
This research was funded by the Defense Threat Reduction Agency (HDTRA1-19-0007).
CONFLICT OF INTEREST STATEMENT
None declared.
DATA AVAILABILITY
Not applicable.
CLINICAL TRIAL REGISTRATION
Not applicable.
INSTITUTIONAL REVIEW BOARD (HUMAN SUBJECTS)
Not applicable.
INSTITUTIONAL ANIMAL CARE AND USE COMMITTEE (IACUC)
Not applicable.
INSTITUTIONAL CLEARANCE
Approved for public release.
INDIVIDUAL AUTHOR CONTRIBUTION STATEMENT
S.J.H., K.M.B., A.L.S., and K.S.W. contributed to the conceptualization, methodology, and software used in the study; S.J.H. and K.M.B. contributed to the formal analysis, writing of the original draft preparation, and visualization; S.J.H., K.M.B., A.W., A.N.O., A.L.S., K.S.W., and A.J.W. contributed to the writing of review and editing; A.W., K.S.W., and A.N.O. contributed to supervision and project administration; and A.W. and A.N.O. contributed to funding acquisition.
REFERENCES
Author notes
This work was presented at the 3rd Symposium on Tropical Medicine and Infectious Diseases in Hamburg, Germany, on August 25, 2022.
The views expressed in this article are those of the authors and do not reflect the official policy or position of the Defense Threat Reduction Agency, Department of Defense, or the U.S. Government.



