-
PDF
- Split View
-
Views
-
Cite
Cite
Esther L Meerwijk, Rachel Sayko Adams, Mary Jo Larson, Krista B Highland, Alex H S Harris, Dose of Exercise Therapy Among Active Duty Soldiers With Chronic Pain Is Associated With Lower Risk of Long-Term Adverse Outcomes After Linking to the Veterans Health Administration, Military Medicine, Volume 188, Issue 7-8, July/August 2023, Pages e1948–e1956, https://doi.org/10.1093/milmed/usac074
Close - Share Icon Share
ABSTRACT
Research in soldiers who had been deployed to Iraq or Afghanistan suggests that nonpharmacological treatments may be protective against adverse outcomes. However, the degree to which exercise therapy received in the U.S. Military Health System (MHS) among soldiers with chronic pain is associated with adverse outcomes after soldiers transition to the Veterans Health Administration (VHA) is unclear. The objective of this study was to determine if exercise therapy received in the MHS among soldiers with chronic pain is associated with long-term adverse outcomes after military separation and enrollment into the VHA and whether this association is moderated by prescription opioid use before starting exercise therapy.
We conducted a longitudinal cohort study of electronic medical records of active duty Army soldiers with documented chronic pain after an index deployment to Iraq or Afghanistan (years 2008-2014) who subsequently enrolled in the VHA (N = 93,967). Coarsened exact matching matched 37,310 soldiers who received exercise therapy and 28,947 soldiers who did not receive exercise therapy in the MHS. Weighted multivariable Cox proportional hazard models tested for differences in adverse outcomes between groups with different exercise therapy exposure vs. no exercise therapy.
Exercise therapy was identified by procedure codes on ambulatory records in the MHS and expressed as the number of exercise therapy visits in 1 year after the first diagnosis with a chronic pain condition. The number of visits was then stratified into seven dose groups.
The primary outcomes were weighted proportional hazards for: (1) alcohol and drug disorders, (2) suicide ideation, (3) intentional self-injury, and (4) all-cause mortality. Outcomes were determined based on ICD-9 and ICD-10 diagnoses recorded in VHA healthcare records from enrollment till September 30, 2020.
Our main analysis indicated significantly lower hazard ratios (HRs) for all adverse outcomes except intentional self-injury, for soldiers with at least eight visits for exercise therapy, compared to soldiers who received no exercise therapy. In the proportional hazard model for any adverse outcome, the HR was 0.91 (95% CI 0.84-0.99) for soldiers with eight or nine exercise therapy visits and 0.91 (95% CI 0.86-0.96) for soldiers with more than nine visits. Significant exercise therapy × prior opioid prescription interactions were observed. In the group that was prescribed opioids before starting exercise therapy, significantly lower HRs were observed for soldiers with more than nine exercise therapy visits, compared to soldiers who received no exercise therapy, for alcohol and drug disorders (HR = 0.85, 95% CI 0.77-0.92), suicide ideation (HR = 0.77, 95% CI 0.66-0.91), and for self-injury (HR = 0.58, 95% CI 0.41-0.83).
Exercise therapy should be considered in the multimodal treatment of chronic pain, especially when pain is being managed with opioids, as it may lower the risk of serious adverse outcomes associated with chronic pain and opioid use. Our findings may generalize only to those active duty soldiers with chronic pain who enroll into VHA after separating from the military.
The U.S. Interagency Taskforce and multiple clinical practice guidelines champion the use of multimodal approaches to manage acute and chronic pain.1–3 Multimodal pain management, which includes nonpharmacological treatments like exercise therapy, is generally associated with improvements in mental and physical functioning, however, effects are inconsistent across treatment modalities and pain conditions.4,5 Exercise therapy may also reduce the risk of opioid initiation and continuation in the first 90 days after a musculoskeletal pain diagnosis.6 Although recent research in soldiers who had been deployed to Iraq or Afghanistan suggests that nonpharmacological treatments may be protective against adverse outcomes,7 the degree to which exercise therapy received in the U.S. Military Health System (MHS) among soldiers with chronic pain is associated with adverse outcomes after soldiers transition to care in the Veterans Health Administration (VHA) is unclear.
Exercise therapy covers a wide range of therapeutic procedures that include, among others, treadmill, isokinetic exercise, lumbar stabilization, stretching, strengthening, neuromuscular re-education, gait training, and aquatic exercise. In the MHS, exercise therapy is frequently used for acute and chronic pain.8,9 In a cohort of soldiers with low-back pain, 63% had received exercise therapy during their pain episode, and in a cohort of soldiers with chronic pain who used VHA services, 92% had received exercise therapy during their prior military service.7,10 A recent meta-analysis reported a significant increase in the risk of nonserious adverse outcomes (e.g., pain or fatigue) for exercise therapy compared to non-exercise controls, especially in patients with back pain or musculoskeletal issues11; issues that are common among active duty soldiers who deployed to Iraq or Afghanistan.12 The evidence did not indicate a change in risk for serious adverse outcomes. As literature on the association between exercise therapy for chronic pain and serious adverse outcomes is scarce and knowledge about the association between exercise therapy and longer-term adverse outcomes could further justify its inclusion in the multimodal treatment of chronic pain, the purpose of this study was to determine the association between long-term serious adverse outcomes and receipt of exercise therapy in soldiers with chronic pain.
Specifically, the purpose of the current analysis was to (1) determine whether exercise therapy received during military service in soldiers with chronic pain was associated with a lower likelihood of serious adverse outcomes after military separation and transition to the VHA, and (2) determine how the dose of exercise therapy was associated with the likelihood of serious adverse outcomes after transition to the VHA. We hypothesized that exercise therapy would be significantly associated with a lower risk of serious adverse outcomes only at higher doses. As soldiers may have been prescribed opioids for pain management and prescription opioids have been associated with increased risk for adverse outcomes,13–15 we also tested the hypothesis that the association between adverse outcomes and exercise therapy dose was moderated by prescription opioid use before starting exercise therapy. Addressing our objectives using a combination of MHS and VHA data allows for longer observation windows and creates an opportunity to assess the cross-system impact of exercise therapy in soldiers with chronic pain.
Methods
Study data were drawn from the Substance Use and Psychological Injury Combat Study (SUPIC), an observational, longitudinal study of Army soldiers returning from an index deployment in support of the Afghanistan/Iraq conflicts between October 2007 and September 2014.16 We used a longitudinal cohort design to study active duty soldiers with chronic pain after their index deployment, who separated from the military and used health care as an enrollee in the VHA before October 2020. Soldiers with chronic pain were identified through their healthcare records in the MHS Data Repository and other DoD sources compiled by SUPIC and included direct care in the MHS and purchased care (i.e., care provided by civilian providers and paid for by DoD). MHS data were included through the end of 2015. The design of the study was quasi-experimental and included matching to balance observed characteristics between soldiers who did and did not receive exercise therapy.
Cohort Description
From the SUPIC active duty cohort (N = 576,516), we included 139,575 soldiers who met the criteria for chronic pain that occurred: (1) while in the MHS after returning from the index deployment ending between October 2007 and September 2014, and (2) before their first separation from the DoD after returning from the index deployment observed till September 2015. The remaining soldiers either did not separate from the military (n = 293,521), did not have any MHS records (n = 17,911), or did not meet the criteria for chronic pain (n = 125,509). Figure 1 shows exclusion criteria that were applied (2,756 used VHA before separating, 29,109 did not link to VHA before 2020, 11,175 linked to VHA within 1 year of a chronic pain diagnosis, 1,199 had missing data), after which 93,967 active duty soldiers remained who separated from the military and linked to VHA before 2020 within 1 year after meeting our criteria for chronic pain. Linkage to VHA was defined as the first healthcare utilization as a VHA enrollee, while ignoring visits for administrative or immunization purposes (i.e., visits with VHA stop codes 674 and 710).
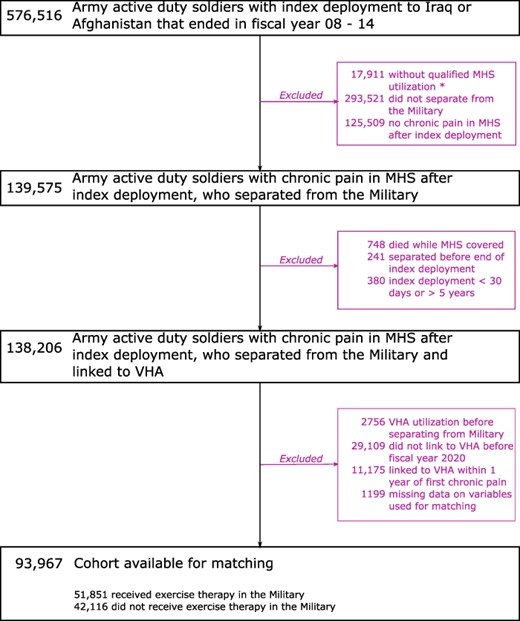
Exclusion criteria applied to active duty U.S. Army service members from the SUPIC cohort. *Qualified MHS utilization refers to any data that we used to determine diagnoses, procedures, medication use, pain ratings, hospitalizations, etc.
Chronic pain was operationalized as a recurrence at least 90 days apart of a diagnosis within any of ten clusters of International Statistical Classification of Diseases and Related Health Problems (ICD-9) diagnoses known to be associated with pain (e.g., nontraumatic joint disorders, musculoskeletal disorders). Similar diagnoses clusters have been previously used to identify chronic pain in health record data.12,17 In addition to diagnoses in a soldier’s MHS records, any 60-days supply of opioids prescribed in a 3-months period or a 90-days supply in 12 months was taken as an indication of chronic pain.18 Prescription opioids included codeine, dihydrocodeine, fentanyl, hydrocodone, hydromorphone, meperidine, methadone, morphine, oxycodone, oxymorphone, and tapentadol—excluding injectable opioids and drugs used to treat addictions (e.g., buprenorphine).
Exposure Variable: Receipt of Exercise Therapy in the MHS
For each soldier, we determined if they received exercise therapy in the MHS for 1 year after their index deployment following the first diagnosis with a chronic pain condition (see Fig. 2). Exercise therapy was identified in the MHS using ICD-9 diagnosis code V65.41, Current Procedural Terminology codes 97110, 97112, 97113, 97116, 97150, 97530, and Healthcare Common Procedure Coding System codes 4242F and S9451. Exercise therapy dose was expressed as the number of exercise therapy visits during the first year after diagnosis of a chronic pain condition. The decision to restrict to the first year after meeting criteria for chronic pain was based on the observation that most of the soldiers who did receive exercise therapy started therapy within 6 months after first meeting those criteria and our assumption that therapy would be especially offered during the initial period after meeting criteria for chronic pain. The number of visits was then stratified into seven groups reflecting increasing dose: (1) no visits, (2) one visit, (3) two or three visits, (4) four or five visits, (5) six or seven visits, (6) eight or nine visits, and (7) more than nine visits for exercise therapy. We opted to categorize the number of visits as this captures potential nonlinear effects without having to model those effects in a mathematical way.
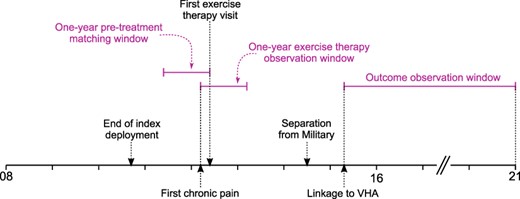
Timeline of events and study observation windows. The end of the index deployment was before 2015 and separation from the Military was observed till 2016. The time between first chronic pain and linkage to VHA was at least 1 year, to ensure a one-year observation window of exercise therapy. Linkage to VHA was before 2020, to ensure observation of adverse outcomes for at least 1 year.
Prescription opioid use to test the potential moderator effect with exercise therapy was operationalized as any days with prescribed opioids (yes/no) observed for 1 year preceding the start of exercise therapy. For soldiers who did not receive exercise therapy, prescription opioid use was determined for the year starting 6 months before first meeting our chronic pain criteria to ensure that soldiers with and without exercise therapy were observed during an overlapping period of time. This period was chosen, as most of the soldiers who did receive exercise therapy had started therapy within 6 months after first meeting the chronic pain criteria.
Dependent Variables: Serious Adverse Outcomes in the VHA
Serious adverse outcomes after soldiers linked to VHA included alcohol and drug use disorders (yes/no) and all-cause mortality and were based on inpatient and outpatient clinical encounters registered in the VHA corporate data warehouse. As chronic pain and opioid use are associated with increased risk of suicide, we also included suicide ideation (yes/no) and nonlethal intentional self-injury (yes/no), including opioid overdose.19,20 Soldiers who died after transition to the VHA were included in analyses for all-cause mortality only. All-cause mortality was based on the “deceased” flag as recorded in VHA healthcare records. The other adverse outcomes were based on ICD-9 and ICD-10 diagnosis codes recorded in VHA healthcare records. The specific codes are listed in Table S1 (Supplemental Material). All adverse outcomes were observed till September 2020.
Coarsened Exact Matching
Coarsened exact matching (CEM) is a nonparametric method to create a balance between groups (e.g., treatment vs. control) and thereby improving causal inference for observational data.21 Contrary to propensity score-based methods, the balance achieved by CEM on one covariate is independent of other covariates. We matched soldiers who did and did not receive exercise therapy during their military service on age, gender, race/ethnicity, rank, the fiscal year in which their index deployment ended, first quarter with chronic pain, and clinical variables during the year before they started exercise therapy: number of hospitalizations, number of visits for mental health/substance use services, maximum pain intensity, opioid prescriptions expressed as daily milligram morphine equivalents (MME), and number of visits for nonpharmacological treatments other than exercise therapy. Pain intensity was assessed on a 0-10 scale and captured during outpatient direct care visits (low: highest pain score 1-3, moderate: highest pain score 4-6, severe: highest pain score 7-10). Clinical variables for soldiers who did not receive exercise therapy were determined for the year starting 6 months before and ending 6 months after first meeting the criteria for chronic pain, to ensure that matching variables for groups with and without exercise therapy were observed during an overlapping time period so as to reduce the effect of unobserved variables. We used a one-to-many approach in which soldiers who did not receive exercise therapy could be matched to multiple soldiers who did receive exercise therapy. This process returns weights for each soldier, which were used in the analyses.
Of 93,967 soldiers who were available for matching, 27,710 (29%) could not be matched, leaving 66,257 soldiers for final analysis: 37,310 who received exercise therapy in the military and 28,947 who did not receive exercise therapy in the military. Figure S1 shows standardized mean differences (SMD) in variables used for matching. After matching, the SMD was less than 0.02 for most variables and only slightly larger for daily MME (0.07) and number of visits for mental health services (0.06). Using Cohen’s operational definition for small effect sizes (SMD > 0.2) we observed that the remaining differences in group means were very small (<0.02 times the standard deviation in the treated group for most variables).22
Table S2 shows descriptive statistics comparing soldiers who were used for matching and who were not used for matching. Over the pre-treatment period, i.e., the 1 year before exercise therapy, soldiers who were not used for matching were older (31.6 vs. 27.8), had a higher proportion of women (23.1% vs. 8.7%), a lower proportion of non-Hispanic white soldiers (44.9 vs. 60.0%), a higher proportion who retired from the military (28.4% vs. 15.0%), a higher level of prescribed opioids (8.2 vs. 3.6 daily MME), more hospitalizations (0.21 vs. 0.04), more visits for mental health services (4.7 vs. 1.3), fewer visits for chiropractic care (0.50 vs. 0.04), and fewer visits for other physical therapy (0.22 vs. 0.02).
Analysis
Primary statistical analysis involved weighted multivariable Cox proportional hazard models to determine the association between exercise therapy dose and the outcomes, while controlling for marital status, reason for military separation, and the time between first MHS chronic pain diagnosis after the index deployment and linking to VHA. These additional covariates were not included in the matching procedure as they were unlikely to determine receipt of exercise therapy. Cox proportional hazard models estimated the relative difference in rates at which adverse outcomes occurred across time for each exercise therapy dose group, compared to soldiers who did not receive exercise therapy. We also used a proportional hazard model for any adverse outcome, where an adverse outcome was assumed to be present if any of the following were present: (1) alcohol and drug disorders, (2) suicide ideation, (3) intentional self-injury, or (4) all-cause mortality.
To address our hypothesis that the association between adverse outcomes and exercise therapy dose may depend on opioid prescription in the year preceding exercise therapy, we included an interaction term in the model for opioid prescription (yes/no) and exercise therapy group. Given a significant interaction, we proceeded with separate subgroup analyses for soldiers who did and did not receive prescription opioids before they started exercise therapy. For these analyses, we included tramadol as an opioid, as it is a short-acting synthetic drug with a lower risk profile. For subgroup analyses, we started with the cohort available for matching and then applied CEM within each subgroup (n = 20,345 for soldiers who were prescribed opioids and n = 38,222 for soldiers who were not prescribed opioids). Matching within subgroups resulted in balanced groups with minimal differences in matching variables (SMD < 0.03 in the group prescribed opioids, SMD < 0.09 in the group not prescribed opioids during the year before starting exercise therapy).
All analyses were done in R version 4.0.2 and CEM was done with the “matchit” function from the R package “MatchIt.”23 All weighted analyses were done with functions from the “Survey” package and P <.05 was considered statistically significant.
Approval for this study was granted by the Brandeis University Committee for Protection of Human Subjects, the Stanford University and VA Palo Alto Health Care System Institutional Review Boards, and the Human Research Protection Program at the Office of the Assistant Secretary of Defense for Health Affairs/ Defense Health Agency. The Defense Health Agency Privacy and Civil Liberties Office executed an annual Data Sharing Agreement.
Results
The weighted median time till VHA linkage after the one-year MHS observation period for exercise therapy was 1.9 years for soldiers who did receive exercise therapy and 2.6 years for soldiers who did not receive exercise therapy in the MHS. The weighted median follow-up time in the VHA was 7.0 years for soldiers who did receive exercise therapy and 6.3 years for soldiers who did not receive exercise therapy in the MHS.
Table I shows characteristics of matched soldiers in our main analysis, comparing soldiers with and without exercise therapy during the observation period for exercise therapy in the MHS. The soldiers were on average, 28 years old, predominantly male (92%); first met our criteria for chronic pain during the third quarter after their index deployment, and reported moderate or severe pain (47%) during the one-year pre-treatment. Soldiers who received exercise therapy during the observation window had statistically significant fewer visits for nonpharmacological treatment modalities other than exercise therapy (specifically, acupuncture and dry needling, spinal manipulation, transcutaneous electrical nerve stimulation, and chiropractic care) were more often diagnosed with mental disorders but had fewer visits for mental health care. Soldiers who received exercise therapy also had lower levels of prescribed opioids, both in days supply and mg morphine equivalents prior to the treatment observation window. Differences in the proportion of soldiers with alcohol use disorder and substance use disorder were not statistically significant, yet soldiers who received exercise therapy had significantly fewer visits for substance use services.
Weighted Comparison of Matched Soldiers Who Did (N = 37,310) and Soldiers Who Did Not Receive Exercise Therapy in the MHS (N = 28,947)
| . | Exercise Therapy . | . | |
|---|---|---|---|
| . | No . | Yes . | P . |
| Demographics and Military History | |||
| Age | 27.8 (0.07) | 27.8 (0.04) | 0.955 |
| Female sex, No. (%) | 2,249 (7.8) | 2,899 (7.8) | 1.000 |
| Race/ethnicity, No. (%) | 1.000 | ||
| White, not Hispanic | 17,827 (61.6) | 22,977 (61.6) | |
| Black, not Hispanic | 5,194 (17.9) | 6,694 (17.9) | |
| Hispanic | 2,416 (8.3) | 3,114 (8.3) | |
| Other | 3,511 (12.1) | 4,525 (12.1) | |
| Marital statusa, No. (%) | 0.385 | ||
| Married | 18,967 (65.5) | 24,154 (64.7) | |
| Never Married | 8,309 (28.7) | 10,963 (29.4) | |
| Other | 1,672 (5.8) | 2,193 (5.9) | |
| Rank, No. (%) | 1.000 | ||
| Enlisted | 28,077 (97.0) | 36,189 (97.0) | |
| Warrant officer | 161 (0.6) | 208 (0.6) | |
| Commissioned Officer | 708 (2.4) | 913 (2.4) | |
| Index cohort, No. (%) | 1.000 | ||
| 2008 | 5,509 (19.0) | 7,101 (19.0) | |
| 2009 | 8,857 (30.6) | 11,416 (30.6) | |
| 2010 | 8,098 (28.0) | 10,438 (28.0) | |
| 2011 | 3,719 (12.8) | 4,794 (12.8) | |
| 2012 | 2,058 (7.1) | 2,652 (7.1) | |
| 2013 | 587 (2.0) | 756 (2.0) | |
| 2014 | 119 (0.4) | 153 (0.4) | |
| Days deployed before indexa | 137 (2.4) | 122 (1.0) | <0.001 |
| Days deployed during indexa | 353 (1.5) | 343 (0.8) | <0.001 |
| Reason for military separationa, No. (%) | <0.001 | ||
| Expiration of enlistment | 6,927 (23.9) | 7,753 (20.8) | |
| Disability | 9,859 (34.1) | 17,349 (46.5) | |
| Retirement | 4,612 (15.9) | 5,130 (13.7) | |
| Misconduct | 1,308 (4.5) | 1,178 (3.2) | |
| Poor performance | 3,748 (12.9) | 3,343 (9.0) | |
| Other | 2,493 (8.6) | 2,557 (6.9) | |
| Military Health System Clinical Historyb | |||
| Days till first chronic pain diagnosisa | 203 (2.2) | 195 (1.4) | <0.001 |
| Mental disordersa, proportion with | |||
| Adjustment disorder | 0.49 | 0.53 | <0.001 |
| Depressive disorders | 0.35 | 0.39 | <0.001 |
| Anxiety disorders | 0.41 | 0.44 | <0.001 |
| Posttraumatic stress disorder | 0.29 | 0.34 | <0.001 |
| Traumatic brain injury | 0.31 | 0.36 | <0.001 |
| Alcohol use disorder | 0.17 | 0.17 | 0.420 |
| Substance use disorder | 0.17 | 0.18 | 0.109 |
| Number of visits for mental health services | 1.36 (0.0) | 1.03 (0.0) | <0.001 |
| Number of visits for SUD services, No. (%) | 0.03 (0.0) | 0.02 (0.0) | 0.008 |
| Number of hospitalizations | 0.04 (0.0) | 0.03 (0.0) | 0.016 |
| Daily mg morphine equivalents | 14.0 (0.2) | 11.8 (0.1) | <0.001 |
| Days supply opioidsa | 6 (0.2) | 5 (0.1) | <0.001 |
| Days supply tramadola | 3 (0.1) | 2 (0.1) | <0.001 |
| First quarter with chronic pain after index | 2.7 (0.0) | 2.7 (0.0) | 0.205 |
| Highest reported pain level, No. (%) | 1.000 | ||
| None (0) | 2,381 (8.2) | 3,069 (8.2) | |
| Low (1-3) | 2,014 (7.0) | 2,596 (7.0) | |
| Moderate (4-6) | 6,488 (22.4) | 8,362 (22.4) | |
| Severe (7-10) | 6,979 (24.1) | 8,995 (24.1) | |
| Unknown | 11,085 (38.3) | 14,288 (38.3) | |
| Number of visits for NPT | |||
| Exercise therapy | 0.04 | 0.09 | <0.001 |
| Acupuncture | 0.05 | 0.00 | 0.032 |
| Biofeedback | 0.12 | 0.01 | 0.088 |
| Massage | 0.06 | 0.01 | 0.455 |
| Laser therapy | 0.01 | 0.00 | 1.000 |
| Spinal manipulation | 0.04 | 0.01 | 0.021 |
| TENS | 0.07 | 0.01 | <0.001 |
| Ultrasonography | 0.05 | 0.00 | 0.526 |
| Heat treatment | 0.04 | 0.00 | 0.387 |
| Traction | 0.01 | 0.00 | 1.000 |
| Lumbar support | 0.01 | 0.00 | 1.000 |
| Other physical therapy | 0.22 | 0.02 | 0.446 |
| Chiropractic care | 0.50 | 0.04 | <0.001 |
| . | Exercise Therapy . | . | |
|---|---|---|---|
| . | No . | Yes . | P . |
| Demographics and Military History | |||
| Age | 27.8 (0.07) | 27.8 (0.04) | 0.955 |
| Female sex, No. (%) | 2,249 (7.8) | 2,899 (7.8) | 1.000 |
| Race/ethnicity, No. (%) | 1.000 | ||
| White, not Hispanic | 17,827 (61.6) | 22,977 (61.6) | |
| Black, not Hispanic | 5,194 (17.9) | 6,694 (17.9) | |
| Hispanic | 2,416 (8.3) | 3,114 (8.3) | |
| Other | 3,511 (12.1) | 4,525 (12.1) | |
| Marital statusa, No. (%) | 0.385 | ||
| Married | 18,967 (65.5) | 24,154 (64.7) | |
| Never Married | 8,309 (28.7) | 10,963 (29.4) | |
| Other | 1,672 (5.8) | 2,193 (5.9) | |
| Rank, No. (%) | 1.000 | ||
| Enlisted | 28,077 (97.0) | 36,189 (97.0) | |
| Warrant officer | 161 (0.6) | 208 (0.6) | |
| Commissioned Officer | 708 (2.4) | 913 (2.4) | |
| Index cohort, No. (%) | 1.000 | ||
| 2008 | 5,509 (19.0) | 7,101 (19.0) | |
| 2009 | 8,857 (30.6) | 11,416 (30.6) | |
| 2010 | 8,098 (28.0) | 10,438 (28.0) | |
| 2011 | 3,719 (12.8) | 4,794 (12.8) | |
| 2012 | 2,058 (7.1) | 2,652 (7.1) | |
| 2013 | 587 (2.0) | 756 (2.0) | |
| 2014 | 119 (0.4) | 153 (0.4) | |
| Days deployed before indexa | 137 (2.4) | 122 (1.0) | <0.001 |
| Days deployed during indexa | 353 (1.5) | 343 (0.8) | <0.001 |
| Reason for military separationa, No. (%) | <0.001 | ||
| Expiration of enlistment | 6,927 (23.9) | 7,753 (20.8) | |
| Disability | 9,859 (34.1) | 17,349 (46.5) | |
| Retirement | 4,612 (15.9) | 5,130 (13.7) | |
| Misconduct | 1,308 (4.5) | 1,178 (3.2) | |
| Poor performance | 3,748 (12.9) | 3,343 (9.0) | |
| Other | 2,493 (8.6) | 2,557 (6.9) | |
| Military Health System Clinical Historyb | |||
| Days till first chronic pain diagnosisa | 203 (2.2) | 195 (1.4) | <0.001 |
| Mental disordersa, proportion with | |||
| Adjustment disorder | 0.49 | 0.53 | <0.001 |
| Depressive disorders | 0.35 | 0.39 | <0.001 |
| Anxiety disorders | 0.41 | 0.44 | <0.001 |
| Posttraumatic stress disorder | 0.29 | 0.34 | <0.001 |
| Traumatic brain injury | 0.31 | 0.36 | <0.001 |
| Alcohol use disorder | 0.17 | 0.17 | 0.420 |
| Substance use disorder | 0.17 | 0.18 | 0.109 |
| Number of visits for mental health services | 1.36 (0.0) | 1.03 (0.0) | <0.001 |
| Number of visits for SUD services, No. (%) | 0.03 (0.0) | 0.02 (0.0) | 0.008 |
| Number of hospitalizations | 0.04 (0.0) | 0.03 (0.0) | 0.016 |
| Daily mg morphine equivalents | 14.0 (0.2) | 11.8 (0.1) | <0.001 |
| Days supply opioidsa | 6 (0.2) | 5 (0.1) | <0.001 |
| Days supply tramadola | 3 (0.1) | 2 (0.1) | <0.001 |
| First quarter with chronic pain after index | 2.7 (0.0) | 2.7 (0.0) | 0.205 |
| Highest reported pain level, No. (%) | 1.000 | ||
| None (0) | 2,381 (8.2) | 3,069 (8.2) | |
| Low (1-3) | 2,014 (7.0) | 2,596 (7.0) | |
| Moderate (4-6) | 6,488 (22.4) | 8,362 (22.4) | |
| Severe (7-10) | 6,979 (24.1) | 8,995 (24.1) | |
| Unknown | 11,085 (38.3) | 14,288 (38.3) | |
| Number of visits for NPT | |||
| Exercise therapy | 0.04 | 0.09 | <0.001 |
| Acupuncture | 0.05 | 0.00 | 0.032 |
| Biofeedback | 0.12 | 0.01 | 0.088 |
| Massage | 0.06 | 0.01 | 0.455 |
| Laser therapy | 0.01 | 0.00 | 1.000 |
| Spinal manipulation | 0.04 | 0.01 | 0.021 |
| TENS | 0.07 | 0.01 | <0.001 |
| Ultrasonography | 0.05 | 0.00 | 0.526 |
| Heat treatment | 0.04 | 0.00 | 0.387 |
| Traction | 0.01 | 0.00 | 1.000 |
| Lumbar support | 0.01 | 0.00 | 1.000 |
| Other physical therapy | 0.22 | 0.02 | 0.446 |
| Chiropractic care | 0.50 | 0.04 | <0.001 |
Values are mean (standard error), unless indicated otherwise. All categories for categorical variables are mutually exclusive. “Index” refers to the first deployment to Iraq or Afghanistan that ended between 2008 and 2014. The P-value was based on the chi-square test for categorical variables and t-test for continuous variables.
Not included in the matching algorithm.
Clinical variables were determined over the one-year pre-treatment window (see Fig. 2).
Abbreviations: NPT, Nonpharmacological Treatment; SUD, Substance Use Disorder; TENS: Transcutaneous Electrical Nerve Stimulation.
Weighted Comparison of Matched Soldiers Who Did (N = 37,310) and Soldiers Who Did Not Receive Exercise Therapy in the MHS (N = 28,947)
| . | Exercise Therapy . | . | |
|---|---|---|---|
| . | No . | Yes . | P . |
| Demographics and Military History | |||
| Age | 27.8 (0.07) | 27.8 (0.04) | 0.955 |
| Female sex, No. (%) | 2,249 (7.8) | 2,899 (7.8) | 1.000 |
| Race/ethnicity, No. (%) | 1.000 | ||
| White, not Hispanic | 17,827 (61.6) | 22,977 (61.6) | |
| Black, not Hispanic | 5,194 (17.9) | 6,694 (17.9) | |
| Hispanic | 2,416 (8.3) | 3,114 (8.3) | |
| Other | 3,511 (12.1) | 4,525 (12.1) | |
| Marital statusa, No. (%) | 0.385 | ||
| Married | 18,967 (65.5) | 24,154 (64.7) | |
| Never Married | 8,309 (28.7) | 10,963 (29.4) | |
| Other | 1,672 (5.8) | 2,193 (5.9) | |
| Rank, No. (%) | 1.000 | ||
| Enlisted | 28,077 (97.0) | 36,189 (97.0) | |
| Warrant officer | 161 (0.6) | 208 (0.6) | |
| Commissioned Officer | 708 (2.4) | 913 (2.4) | |
| Index cohort, No. (%) | 1.000 | ||
| 2008 | 5,509 (19.0) | 7,101 (19.0) | |
| 2009 | 8,857 (30.6) | 11,416 (30.6) | |
| 2010 | 8,098 (28.0) | 10,438 (28.0) | |
| 2011 | 3,719 (12.8) | 4,794 (12.8) | |
| 2012 | 2,058 (7.1) | 2,652 (7.1) | |
| 2013 | 587 (2.0) | 756 (2.0) | |
| 2014 | 119 (0.4) | 153 (0.4) | |
| Days deployed before indexa | 137 (2.4) | 122 (1.0) | <0.001 |
| Days deployed during indexa | 353 (1.5) | 343 (0.8) | <0.001 |
| Reason for military separationa, No. (%) | <0.001 | ||
| Expiration of enlistment | 6,927 (23.9) | 7,753 (20.8) | |
| Disability | 9,859 (34.1) | 17,349 (46.5) | |
| Retirement | 4,612 (15.9) | 5,130 (13.7) | |
| Misconduct | 1,308 (4.5) | 1,178 (3.2) | |
| Poor performance | 3,748 (12.9) | 3,343 (9.0) | |
| Other | 2,493 (8.6) | 2,557 (6.9) | |
| Military Health System Clinical Historyb | |||
| Days till first chronic pain diagnosisa | 203 (2.2) | 195 (1.4) | <0.001 |
| Mental disordersa, proportion with | |||
| Adjustment disorder | 0.49 | 0.53 | <0.001 |
| Depressive disorders | 0.35 | 0.39 | <0.001 |
| Anxiety disorders | 0.41 | 0.44 | <0.001 |
| Posttraumatic stress disorder | 0.29 | 0.34 | <0.001 |
| Traumatic brain injury | 0.31 | 0.36 | <0.001 |
| Alcohol use disorder | 0.17 | 0.17 | 0.420 |
| Substance use disorder | 0.17 | 0.18 | 0.109 |
| Number of visits for mental health services | 1.36 (0.0) | 1.03 (0.0) | <0.001 |
| Number of visits for SUD services, No. (%) | 0.03 (0.0) | 0.02 (0.0) | 0.008 |
| Number of hospitalizations | 0.04 (0.0) | 0.03 (0.0) | 0.016 |
| Daily mg morphine equivalents | 14.0 (0.2) | 11.8 (0.1) | <0.001 |
| Days supply opioidsa | 6 (0.2) | 5 (0.1) | <0.001 |
| Days supply tramadola | 3 (0.1) | 2 (0.1) | <0.001 |
| First quarter with chronic pain after index | 2.7 (0.0) | 2.7 (0.0) | 0.205 |
| Highest reported pain level, No. (%) | 1.000 | ||
| None (0) | 2,381 (8.2) | 3,069 (8.2) | |
| Low (1-3) | 2,014 (7.0) | 2,596 (7.0) | |
| Moderate (4-6) | 6,488 (22.4) | 8,362 (22.4) | |
| Severe (7-10) | 6,979 (24.1) | 8,995 (24.1) | |
| Unknown | 11,085 (38.3) | 14,288 (38.3) | |
| Number of visits for NPT | |||
| Exercise therapy | 0.04 | 0.09 | <0.001 |
| Acupuncture | 0.05 | 0.00 | 0.032 |
| Biofeedback | 0.12 | 0.01 | 0.088 |
| Massage | 0.06 | 0.01 | 0.455 |
| Laser therapy | 0.01 | 0.00 | 1.000 |
| Spinal manipulation | 0.04 | 0.01 | 0.021 |
| TENS | 0.07 | 0.01 | <0.001 |
| Ultrasonography | 0.05 | 0.00 | 0.526 |
| Heat treatment | 0.04 | 0.00 | 0.387 |
| Traction | 0.01 | 0.00 | 1.000 |
| Lumbar support | 0.01 | 0.00 | 1.000 |
| Other physical therapy | 0.22 | 0.02 | 0.446 |
| Chiropractic care | 0.50 | 0.04 | <0.001 |
| . | Exercise Therapy . | . | |
|---|---|---|---|
| . | No . | Yes . | P . |
| Demographics and Military History | |||
| Age | 27.8 (0.07) | 27.8 (0.04) | 0.955 |
| Female sex, No. (%) | 2,249 (7.8) | 2,899 (7.8) | 1.000 |
| Race/ethnicity, No. (%) | 1.000 | ||
| White, not Hispanic | 17,827 (61.6) | 22,977 (61.6) | |
| Black, not Hispanic | 5,194 (17.9) | 6,694 (17.9) | |
| Hispanic | 2,416 (8.3) | 3,114 (8.3) | |
| Other | 3,511 (12.1) | 4,525 (12.1) | |
| Marital statusa, No. (%) | 0.385 | ||
| Married | 18,967 (65.5) | 24,154 (64.7) | |
| Never Married | 8,309 (28.7) | 10,963 (29.4) | |
| Other | 1,672 (5.8) | 2,193 (5.9) | |
| Rank, No. (%) | 1.000 | ||
| Enlisted | 28,077 (97.0) | 36,189 (97.0) | |
| Warrant officer | 161 (0.6) | 208 (0.6) | |
| Commissioned Officer | 708 (2.4) | 913 (2.4) | |
| Index cohort, No. (%) | 1.000 | ||
| 2008 | 5,509 (19.0) | 7,101 (19.0) | |
| 2009 | 8,857 (30.6) | 11,416 (30.6) | |
| 2010 | 8,098 (28.0) | 10,438 (28.0) | |
| 2011 | 3,719 (12.8) | 4,794 (12.8) | |
| 2012 | 2,058 (7.1) | 2,652 (7.1) | |
| 2013 | 587 (2.0) | 756 (2.0) | |
| 2014 | 119 (0.4) | 153 (0.4) | |
| Days deployed before indexa | 137 (2.4) | 122 (1.0) | <0.001 |
| Days deployed during indexa | 353 (1.5) | 343 (0.8) | <0.001 |
| Reason for military separationa, No. (%) | <0.001 | ||
| Expiration of enlistment | 6,927 (23.9) | 7,753 (20.8) | |
| Disability | 9,859 (34.1) | 17,349 (46.5) | |
| Retirement | 4,612 (15.9) | 5,130 (13.7) | |
| Misconduct | 1,308 (4.5) | 1,178 (3.2) | |
| Poor performance | 3,748 (12.9) | 3,343 (9.0) | |
| Other | 2,493 (8.6) | 2,557 (6.9) | |
| Military Health System Clinical Historyb | |||
| Days till first chronic pain diagnosisa | 203 (2.2) | 195 (1.4) | <0.001 |
| Mental disordersa, proportion with | |||
| Adjustment disorder | 0.49 | 0.53 | <0.001 |
| Depressive disorders | 0.35 | 0.39 | <0.001 |
| Anxiety disorders | 0.41 | 0.44 | <0.001 |
| Posttraumatic stress disorder | 0.29 | 0.34 | <0.001 |
| Traumatic brain injury | 0.31 | 0.36 | <0.001 |
| Alcohol use disorder | 0.17 | 0.17 | 0.420 |
| Substance use disorder | 0.17 | 0.18 | 0.109 |
| Number of visits for mental health services | 1.36 (0.0) | 1.03 (0.0) | <0.001 |
| Number of visits for SUD services, No. (%) | 0.03 (0.0) | 0.02 (0.0) | 0.008 |
| Number of hospitalizations | 0.04 (0.0) | 0.03 (0.0) | 0.016 |
| Daily mg morphine equivalents | 14.0 (0.2) | 11.8 (0.1) | <0.001 |
| Days supply opioidsa | 6 (0.2) | 5 (0.1) | <0.001 |
| Days supply tramadola | 3 (0.1) | 2 (0.1) | <0.001 |
| First quarter with chronic pain after index | 2.7 (0.0) | 2.7 (0.0) | 0.205 |
| Highest reported pain level, No. (%) | 1.000 | ||
| None (0) | 2,381 (8.2) | 3,069 (8.2) | |
| Low (1-3) | 2,014 (7.0) | 2,596 (7.0) | |
| Moderate (4-6) | 6,488 (22.4) | 8,362 (22.4) | |
| Severe (7-10) | 6,979 (24.1) | 8,995 (24.1) | |
| Unknown | 11,085 (38.3) | 14,288 (38.3) | |
| Number of visits for NPT | |||
| Exercise therapy | 0.04 | 0.09 | <0.001 |
| Acupuncture | 0.05 | 0.00 | 0.032 |
| Biofeedback | 0.12 | 0.01 | 0.088 |
| Massage | 0.06 | 0.01 | 0.455 |
| Laser therapy | 0.01 | 0.00 | 1.000 |
| Spinal manipulation | 0.04 | 0.01 | 0.021 |
| TENS | 0.07 | 0.01 | <0.001 |
| Ultrasonography | 0.05 | 0.00 | 0.526 |
| Heat treatment | 0.04 | 0.00 | 0.387 |
| Traction | 0.01 | 0.00 | 1.000 |
| Lumbar support | 0.01 | 0.00 | 1.000 |
| Other physical therapy | 0.22 | 0.02 | 0.446 |
| Chiropractic care | 0.50 | 0.04 | <0.001 |
Values are mean (standard error), unless indicated otherwise. All categories for categorical variables are mutually exclusive. “Index” refers to the first deployment to Iraq or Afghanistan that ended between 2008 and 2014. The P-value was based on the chi-square test for categorical variables and t-test for continuous variables.
Not included in the matching algorithm.
Clinical variables were determined over the one-year pre-treatment window (see Fig. 2).
Abbreviations: NPT, Nonpharmacological Treatment; SUD, Substance Use Disorder; TENS: Transcutaneous Electrical Nerve Stimulation.
Table II shows the results of our main analysis, indicating significantly lower hazard ratios (HRs) for all adverse outcomes except intentional self-injury, for soldiers with at least eight visits for exercise therapy, compared to soldiers who received no exercise therapy. In the proportional hazard model for any adverse outcome, the HR was 0.91 (95% CI 0.84-0.99) for soldiers with eight or nine exercise therapy visits and 0.91 (95% CI 0.86-0.96) for soldiers with more than nine visits.
Adjusted Cox Proportional Hazard Ratios (95% CI) for Adverse Outcomes in the VHA in Soldiers Who Did (N = 37,310) and Did Not (N = 28,947) Receive Exercise Therapy after First Meeting Our Criteria for Chronic Pain in the Military
| Exercise therapy . | Any adverse outcome . | Alcohol and drug disorders . | Suicide ideation . | Self-Injury . | All-cause mortality . |
|---|---|---|---|---|---|
| 19,103 events . | 17,496 events . | 4,965 events . | 1,131 events . | 987 events . | |
| 1 visit (n = 7,355) | 1.02 (0.96-1.08) | 1.03 (0.97-1.10) | 1.02 (0.91-1.15) | 0.96 (0.75-1.23) | 0.73 (0.54-1.00)* |
| 2-3 (n = 6,850) | 0.96 (0.90-1.02) | 0.96 (0.91-1.03) | 0.90 (0.79-1.01) | 0.95 (0.73-1.22) | 0.75 (0.54-1.03) |
| 4-5 (n = 4,707) | 0.97 (0.91-1.04) | 0.98 (0.92-1.05) | 0.85 (0.74-0.97)* | 0.83 (0.62-1.11) | 0.72 (0.51-1.03) |
| 6-7 (n = 3,713) | 0.96 (0.90-1.04) | 0.95 (0.88-1.02) | 0.98 (0.85-1.13) | 1.11 (0.83-1.48) | 0.68 (0.46-0.99)* |
| 8-9 (n = 2,739) | 0.91 (0.84-0.99)* | 0.90 (0.83-0.99)* | 0.83 (0.70-0.97)* | 0.70 (0.48-1.02) | 0.62 (0.40-0.95)* |
| >9 visits (n = 11,946) | 0.91 (0.86-0.96)*** | 0.91 (0.86-0.97)** | 0.85 (0.76-0.95)** | 0.78 (0.61-1.00) | 0.72 (0.52-0.98)* |
| Exercise therapy . | Any adverse outcome . | Alcohol and drug disorders . | Suicide ideation . | Self-Injury . | All-cause mortality . |
|---|---|---|---|---|---|
| 19,103 events . | 17,496 events . | 4,965 events . | 1,131 events . | 987 events . | |
| 1 visit (n = 7,355) | 1.02 (0.96-1.08) | 1.03 (0.97-1.10) | 1.02 (0.91-1.15) | 0.96 (0.75-1.23) | 0.73 (0.54-1.00)* |
| 2-3 (n = 6,850) | 0.96 (0.90-1.02) | 0.96 (0.91-1.03) | 0.90 (0.79-1.01) | 0.95 (0.73-1.22) | 0.75 (0.54-1.03) |
| 4-5 (n = 4,707) | 0.97 (0.91-1.04) | 0.98 (0.92-1.05) | 0.85 (0.74-0.97)* | 0.83 (0.62-1.11) | 0.72 (0.51-1.03) |
| 6-7 (n = 3,713) | 0.96 (0.90-1.04) | 0.95 (0.88-1.02) | 0.98 (0.85-1.13) | 1.11 (0.83-1.48) | 0.68 (0.46-0.99)* |
| 8-9 (n = 2,739) | 0.91 (0.84-0.99)* | 0.90 (0.83-0.99)* | 0.83 (0.70-0.97)* | 0.70 (0.48-1.02) | 0.62 (0.40-0.95)* |
| >9 visits (n = 11,946) | 0.91 (0.86-0.96)*** | 0.91 (0.86-0.97)** | 0.85 (0.76-0.95)** | 0.78 (0.61-1.00) | 0.72 (0.52-0.98)* |
The analyses were weighted using weights resulting from coarsened exact matching of soldiers who did and did not receive exercise therapy in the Military. The Cox proportional hazard ratios were adjusted for marital status at the end of the index deployment, reason for separating from the Military, and time between first chronic pain diagnosis and linking to VHA. The hazard ratios are with reference to soldiers who did not receive exercise therapy.
*P < .05, **P < .01, ***P < .001.
Adjusted Cox Proportional Hazard Ratios (95% CI) for Adverse Outcomes in the VHA in Soldiers Who Did (N = 37,310) and Did Not (N = 28,947) Receive Exercise Therapy after First Meeting Our Criteria for Chronic Pain in the Military
| Exercise therapy . | Any adverse outcome . | Alcohol and drug disorders . | Suicide ideation . | Self-Injury . | All-cause mortality . |
|---|---|---|---|---|---|
| 19,103 events . | 17,496 events . | 4,965 events . | 1,131 events . | 987 events . | |
| 1 visit (n = 7,355) | 1.02 (0.96-1.08) | 1.03 (0.97-1.10) | 1.02 (0.91-1.15) | 0.96 (0.75-1.23) | 0.73 (0.54-1.00)* |
| 2-3 (n = 6,850) | 0.96 (0.90-1.02) | 0.96 (0.91-1.03) | 0.90 (0.79-1.01) | 0.95 (0.73-1.22) | 0.75 (0.54-1.03) |
| 4-5 (n = 4,707) | 0.97 (0.91-1.04) | 0.98 (0.92-1.05) | 0.85 (0.74-0.97)* | 0.83 (0.62-1.11) | 0.72 (0.51-1.03) |
| 6-7 (n = 3,713) | 0.96 (0.90-1.04) | 0.95 (0.88-1.02) | 0.98 (0.85-1.13) | 1.11 (0.83-1.48) | 0.68 (0.46-0.99)* |
| 8-9 (n = 2,739) | 0.91 (0.84-0.99)* | 0.90 (0.83-0.99)* | 0.83 (0.70-0.97)* | 0.70 (0.48-1.02) | 0.62 (0.40-0.95)* |
| >9 visits (n = 11,946) | 0.91 (0.86-0.96)*** | 0.91 (0.86-0.97)** | 0.85 (0.76-0.95)** | 0.78 (0.61-1.00) | 0.72 (0.52-0.98)* |
| Exercise therapy . | Any adverse outcome . | Alcohol and drug disorders . | Suicide ideation . | Self-Injury . | All-cause mortality . |
|---|---|---|---|---|---|
| 19,103 events . | 17,496 events . | 4,965 events . | 1,131 events . | 987 events . | |
| 1 visit (n = 7,355) | 1.02 (0.96-1.08) | 1.03 (0.97-1.10) | 1.02 (0.91-1.15) | 0.96 (0.75-1.23) | 0.73 (0.54-1.00)* |
| 2-3 (n = 6,850) | 0.96 (0.90-1.02) | 0.96 (0.91-1.03) | 0.90 (0.79-1.01) | 0.95 (0.73-1.22) | 0.75 (0.54-1.03) |
| 4-5 (n = 4,707) | 0.97 (0.91-1.04) | 0.98 (0.92-1.05) | 0.85 (0.74-0.97)* | 0.83 (0.62-1.11) | 0.72 (0.51-1.03) |
| 6-7 (n = 3,713) | 0.96 (0.90-1.04) | 0.95 (0.88-1.02) | 0.98 (0.85-1.13) | 1.11 (0.83-1.48) | 0.68 (0.46-0.99)* |
| 8-9 (n = 2,739) | 0.91 (0.84-0.99)* | 0.90 (0.83-0.99)* | 0.83 (0.70-0.97)* | 0.70 (0.48-1.02) | 0.62 (0.40-0.95)* |
| >9 visits (n = 11,946) | 0.91 (0.86-0.96)*** | 0.91 (0.86-0.97)** | 0.85 (0.76-0.95)** | 0.78 (0.61-1.00) | 0.72 (0.52-0.98)* |
The analyses were weighted using weights resulting from coarsened exact matching of soldiers who did and did not receive exercise therapy in the Military. The Cox proportional hazard ratios were adjusted for marital status at the end of the index deployment, reason for separating from the Military, and time between first chronic pain diagnosis and linking to VHA. The hazard ratios are with reference to soldiers who did not receive exercise therapy.
*P < .05, **P < .01, ***P < .001.
Significant opioid prescription × exercise therapy interactions were observed for alcohol/drug disorders and all-cause mortality (see Tables S4-S8 for the full interaction models). While the opioid prescription interactions for self-injury and suicide ideation were not statistically significant, we considered the P-values small enough (P = .06) to warrant inclusion in subgroup analysis.24 In the group prescribed opioids in the year prior to exercise therapy initiation, significantly lower HRs were observed for alcohol and drug disorders (HR = 0.85, 95% CI 0.77-0.92), suicide ideation (HR = 0.77, 95% CI 0.66-0.91), and self-injury (HR = 0.58, 95% CI 0.41-0.83) for soldiers with more than nine exercise therapy visits (weighted median 17 [10-232] visits), compared to soldiers who received no exercise therapy. No significant HRs were observed at other exercise therapy doses in this group. The daily morphine equivalents in this group in the year before exercise therapy was 9.1 mg, which is considered low by conventional standards.25 Contrary to our main analysis, there were no significant differences in the opioid group between soldiers with and without exercise therapy in the MHS in terms of prescribed opioid days supply or number of visits for mental health and substance use services (see Table S3). The prescribed daily morphine equivalents in this group were significantly higher for soldiers who did receive exercise therapy (9.6 vs. 8.6 mg).
In the group that was not prescribed opioids before they started exercise therapy, the only statistically significant outcome was for all-cause mortality (HR = 0.59, 95% CI 0.39-0.91) in soldiers with one exercise therapy visit.
Discussion
The purpose of this study was to determine whether exercise therapy received in the MHS among soldiers with chronic pain after an index deployment to Afghanistan/Iraq was associated with a lower likelihood of adverse outcomes after transition to the VHA. Our main analysis indicated protective associations of exercise therapy for soldiers with at least eight visits for exercise therapy, compared to soldiers who received no exercise therapy, but these associations depended on whether soldiers were prescribed opioids or not before they started exercise therapy. In soldiers prescribed opioids during the year before they started exercise therapy, the results show a 15% lower likelihood of alcohol and drug use disorders, 23% lower likelihood of suicide ideation, and 43% lower likelihood of self-injury for soldiers with more than nine visits for exercise therapy compared to soldiers who did not receive exercise therapy. These findings are consistent with general literature that describes the positive effect, for example through biochemical mechanisms, of exercise on mental health,26 however, in our study this positive effect is most likely achieved through pain reduction. The fact that we observe these associations in soldiers prescribed opioids before starting exercise therapy and not in those who were not prescribed opioids supports the premise for our analyses that opioid prescriptions are associated with an increased likelihood of adverse outcomes (e.g., alcohol and drug use disorders, self-injury). There is literature to suggest that worse pain interference is associated with a lower likelihood of engaging in exercise therapy.25 It may be that some level of opioid use alleviates chronic pain just enough for soldiers to engage meaningfully in exercise therapy sessions. In our analyses, the MME daily dose was low, about 10 MME.
It is striking that exercise therapy in soldiers with chronic pain would have a protective effect against adverse outcomes that may last years after therapy has ended. In our cohort the mean follow-up time was well over 6 years. We hypothesize that if exercise therapy enables soldiers to effectively manage their chronic pain, it may remove a trigger for suicide ideation and the impetus to self-medicate with alcohol or drugs, thereby lowering chances of intentional as well accidental self-injury (e.g., falls, overdoses, motor vehicle accidents, suicide). Our results imply that exercise therapy as pain management may be protective against long-term adverse outcomes for soldiers who were started on prescribed opioids, but not for soldiers who were not prescribed opioids.
Study Limitations
Our results are consistent with a causal effect of exercise therapy, but other explanations do exist. Most importantly, we assumed that by matching soldiers with and without exercise therapy unobserved variables would be randomly distributed across both groups. If, for example, soldiers who did not receive exercise therapy experienced more life stressors (e.g., relationship problems, unemployment after military separation) this may have increased their likelihood for alcohol and drug use, suicide ideation, and self-injury. Also, small differences remained after matching, showing higher healthcare utilization in soldiers who did not receive exercise therapy (e.g., more hospitalizations and more visits for mental health care and substance use services), but those differences were opposite or not significant in the group that was prescribed opioids. The matching process resulted in exclusion of 29% of our cohort from final analyses, reducing generalizability of our findings. Additionally, our findings generalize only to those active duty soldiers with chronic pain who enroll into VHA after separating from the military. Results may differ for military members in other service branches and for soldiers who leave the military but who do not enroll and seek care in the VHA.27 Codes for exercise therapy were aggregated at the level of days that therapy was received. We did not have data on the number of units of therapy that were received on those days. Also, while we matched soldiers on nonpharmacological treatment modalities received before they started exercise therapy, it is not uncommon for exercise therapy to be provided along with other interventions during rehabilitation visits. This implies that the observed effects could to some extent be due to other interventions. The moderation effect of opioids was based on prescribed opioids. Whether opioids were actually taken remains unknown. This means that some soldiers in the opioids group should have been analyzed in the “no opioids” group, which suggests that the observed HRs may be closer to 1.0 than reported here. As our outcome measures were based on diagnosis codes found in electronic health records, the observed level of adverse outcomes is likely an underestimate of the actual number of adverse outcomes.
Conclusions
Within the boundaries of these limitations, exercise therapy for chronic pain at higher doses (more than nine visits) appears to lower the likelihood of serious adverse outcomes when chronic pain is managed with prescription opioids. Further research is necessary to replicate these findings in other service members (e.g., reserve component, national guard), and to identify the active ingredients of exercise therapy and the mechanism through which exercise therapy affects the lower likelihood of adverse outcomes. Additionally, further research should study whether other nonpharmacological treatments (e.g., joint manipulation, electrical nerve stimulation, massage) might show similar reductions in adverse outcomes in populations who did and did not start opioid therapy. Overall, the apparent protective association of exercise therapy for longer-term adverse outcomes should further justify its inclusion in multimodal pain management and treatment strategies, especially when chronic pain is managed with prescription opioids.
Acknowledgments
We thank AXIOM Resource Management, Inc., for compiling the DoD data used in these analyses, and the Defense Health Agency’s Privacy and Civil Liberties Office, who provided access to the DoD data. Chester Buckenmaier, III, M.D. of the Uniformed Services University was the DoD data sponsor.
Supplementary Material
Supplementary Material is available at Military Medicine online.
Funding
This study was funded by the National Center for Complementary and Integrative Health (NCCIH; R01 AT008404) and the National Institute on Drug Abuse (NIDA; R01 DA030150). Dr. Sox-Harris’s effort was supported in part by a grant from the Veterans Affairs (HSR&D RCS 14-232). The funding organizations had no role in study design; in the collection, analysis and interpretation of the data; in the writing of the report; or in the decision to submit the article for publication.
Conflict Of Interest Statement
All authors report “no conflicts of interest”.
References
Author notes
Preliminary results from this study were presented by the corresponding author at the AcademyHealth virtual Annual Research Meeting, June 2021.
The views expressed are solely those of the authors and do not reflect the official policy or position of the Veterans Health Administration, Uniformed Services University, U.S. Army, U.S. Navy, U.S. Air Force, the DoD, the U.S. Government, the Henry M. Jackson Foundation for the Advancement of Military Medicine, Inc, or the NIH.



