-
PDF
- Split View
-
Views
-
Cite
Cite
Bradley M Ritland, Jacob A Naylor, Alexxa F Bessey, Tina M Burke, Julie M Hughes, Stephen A Foulis, Walter J Sowden, Janna Mantua, Association Between Self-Reported Sleep Quality and Musculoskeletal Injury in Male Army Rangers, Military Medicine, Volume 188, Issue 7-8, July/August 2023, Pages e1882–e1886, https://doi.org/10.1093/milmed/usab488
Close - Share Icon Share
ABSTRACT
Musculoskeletal injuries and insufficient sleep are common among U.S. Army Rangers. There has been limited research into whether indices of sleep differ between injured and uninjured Rangers. The purpose of this study was to investigate the association between self-reported sleep and musculoskeletal injury in Rangers.
A total of 82 Army Rangers (male, 25.4 ± 4.0 years) were asked if they currently have any musculoskeletal injuries; completed the Pittsburgh Sleep Quality Index (PSQI), the Insomnia Severity Index (ISI), and the Stanford Sleepiness Scale; and were asked about their average sleep quality/sleep duration over the preceding week. Rangers were then dichotomized into groups, one that reported a current musculoskeletal injury and another that did not.
The reported musculoskeletal injury prevalence was 15.9% (n = 13). The Rangers that reported an injury, compared to those that did not, had a significantly higher Global PSQI score (6.7 ± 3.7 versus 4.5 ± 2.7, P = .012) and ISI score (10.9 ± 3.7 versus 7.2 ± 4.1, P = .003), both indicative of poorer sleep. The group reporting an injury rated their average sleep quality over the preceding week significantly lower compared to those that did not report an injury (50.8 ± 17.5 versus 68.9 ± 18.3, P = .001). There was no significant group difference in the average nightly sleep duration (6.1 ± 1.0 hours versus 6.5 ± 0.9 hours, P = .099).
In this cohort of male Army Rangers, In this cohort of male Army Rangers, those with a musculoskeletal injury reported poorer sleep quality than uninjured Rangers. Sleep duration was not associated with reported injuries; however, both the injured group and uninjured group averaged less than the recommended amounts of sleep. Further investigation into the relationship between musculoskeletal injury and sleep in military personnel is warranted.
INTRODUCTION
Musculoskeletal injuries continue to be a significant health problem in military service members.1 Among units with U.S. Army Rangers, which are elite light infantry units within the Special Operation community that routinely conduct nighttime operations of high importance to national security, injury incidence has been reported to be up to 50%.2 Rangers are required to perform a number of tasks known to be associated with injury risk, such as long ruck marching with heavy loads3 and airborne operations,4 in varying environments and situations. Other factors such as musculoskeletal injury history, smoking, pain provocation, movement tests, and lower scores on physical performance measures are also associated with the risk for musculoskeletal injury in Rangers.2 Aside from any associated pain and functional impairments, there can be other varying negative health and performance consequences, such as not being able to perform the training required for the job or performing the job itself, in both a garrison and forward deployed environment. Considering the prevalence of injuries in Rangers and the potential associated negative consequences, an improved understanding of the mechanisms and risks associated with the injuries in this population remains warranted.
Previous research on the association between musculoskeletal injuries and sleep is limited, especially in a military population. One military study found an inverse relationship between sleep duration and injury risk when a large group of Special Operations soldiers were asked, “How many musculoskeletal injuries have you sustained in the past 12 months?” and “How many hours of actual sleep did you get at night (This may be different than the number of hours you spend in bed)?”.5 This inverse relationship between sleep duration and injury has also been observed in young athletes.6–8 However, a recent study that examined the relationship in older, college-aged, football players did not find an association between sleep duration, or sleep quality, and the risk of injury.9 Another study in college-aged cross-country runners found an association between poor sleep quality and higher risk for injury during the season,10 which is consistent with poor sleep quality having been associated with increased work injuries in other civilian settings.11 With both the paucity and the somewhat conflicting findings of existing studies, further exploration is needed to better understand the relationship between sleep and musculoskeletal injury, especially in populations where injury rates and insufficient sleep are high. The purpose of this study was to investigate the association between self-reported sleep (quality and duration) and musculoskeletal injuries in U.S. Army Rangers.
MATERIALS AND METHODS
This study was approved by a Scientific Institutional Review Board and the U.S. Army Special Operations Command Research Advisory Council. It was performed in accordance with the ethical standards of the 1964 Declaration of Helsinki. All participants provided written informed consent.
This study was part of a larger study investigating how reverse cycle (nighttime) operations in a military operational context impact the health and performance of Army Rangers. Data from the current study were from a “baseline” time point, during which Rangers were not actively engaged in an atypical sleep schedule and were not engaged in a field-training event.
During a standard duty day, to ascertain information on their sleep, the Rangers completed a Pittsburgh Sleep Quality Index (PSQI), the Insomnia Severity Index (ISI), and the Stanford Sleepiness Scale (SSS) and were asked to rate their average sleep quality (0 equating to “poor quality” and 100 equating to “best quality”) and specify their average sleep duration over the preceding week. The Rangers were also asked whether they had any musculoskeletal injuries. The question on the survey was, “Do you currently have any musculoskeletal injuries”, with a “yes” or “no” response option.
The PSQI is a well-validated, 19-item questionnaire designed to evaluate self-reported sleep quality and disturbances in adults over the past 30 days.12 The PSQI responses are grouped to assess seven component factors, including subjective sleep quality, sleep latency, sleep duration, sleep efficiency, sleep disturbances, sleep medication use, and daytime dysfunction. Each component score is weighted equally, with scores ranging from 0 to 3 (higher scores indicating a worse score). The Global PSQI measure, which can range from 0 to 21, is the sum of the seven components and is an indicator of overall sleep quality. Global scores greater than 5 have been used to distinguish poor sleepers.
The ISI evaluates the severity of sleep disturbances over the previous 2 weeks13 and has been found to be valid and reliable in quantifying perceived insomnia severity.14 The ISI is composed of seven items (sleep onset, sleep maintenance, early morning awakening problems, sleep dissatisfaction, interference of sleep difficulties with daytime functioning, noticeability of sleep problems by others, and distress caused by sleep difficulties) that are scored using a 5-point Likert scale. The total ISI score can range from 0 to 28, with higher scores indicating more severe insomnia and the lowest scores indicating an absence of insomnia.
The SSS assesses the participant’s self-reported sleepiness at a given moment and is a one-item scale that ranges from 1 (“Feeling active and vital; alert; wide awake”) to 7 (“Almost in reverie; sleep onset soon; lost struggle to remain awake”), with higher scores indicating more sleepiness.15
All statistical analyses were performed using SPSS 26.0 (SPSS Inc., Chicago, IL, USA). Means and standard deviations were calculated for the outcome measures (PSQI, ISI, SSS, sleep quality, and sleep duration over the past week). Participants were dichotomized into groups of “injured” versus “uninjured” based on whether they indicated they had a musculoskeletal injury at the time they were completing the questionnaires. To evaluate between-group (injured versus uninjured) mean score differences of the outcome measures, independent sample t-tests were conducted. When analyzing the mean age of the participants, a significant between-group difference was observed. Therefore, an analysis of variance, controlling for age, was also conducted to compare the group (injured versus uninjured) means for each outcome measure. P values <.05 were considered statistically significant.
RESULTS
A total of 82 male Rangers (25.4 ± 4.0 years) completed all of the questionnaires described in this study. The reported musculoskeletal injury prevalence of the Rangers was 15.9% (n = 13). Demographic information is listed in Table I. Table II provides group comparisons of each outcome measure; the Rangers that reported an injury, compared to those that did not, had a significantly higher Global PSQI score (P = .012, Fig. 1A) and ISI score (P = .003, Fig. 1B), both indicative of poorer sleep. In addition, the group reporting an injury rated their average sleep quality over the preceding week significantly lower compared to those that did not (P = .001). There was no significant group difference in the reported average nightly sleep duration (P = .099) or the SSS score (P = .808). These group comparisons remained the same after controlling for age; there was a significant difference between groups (injured versus uninjured) for Global PSQI score (F (1, 79) = 7.43, P = .008), ISI score (F (1, 79) = 9.50, P = .003), and average sleep quality over the preceding week (F (1, 79) = 10.57, P = .002); however, not for the average sleep duration over the preceding week (F (1, 79) = 3.19, P = .078) or SSS scores (F (1, 79) = 0.00, P = .967).
| . | Reported injury . | No reported injury . |
|---|---|---|
| No. of participants, n | 13 | 69 |
| Age, years (mean ± SD) | 27.5 ± 4.2 | 25.0 ± 3.8* |
| Gender, male | 100% | 100% |
| Ethnicity | ||
| American Indian | 2 (15.4%) | 0 (0.0%) |
| African American/Black | 0 (0.0%) | 1 (1.4%) |
| Asian | 0 (0.0%) | 2 (2.9%) |
| Caucasian/White | 9 (69.2%) | 56 (81.2%) |
| Hispanic | 1 (7.7%) | 7 (10.1%) |
| Native Hawaiian | 1 (7.7%) | 1 (1.4%) |
| Multi | 0 (0.0%) | 2 (2.9%) |
| . | Reported injury . | No reported injury . |
|---|---|---|
| No. of participants, n | 13 | 69 |
| Age, years (mean ± SD) | 27.5 ± 4.2 | 25.0 ± 3.8* |
| Gender, male | 100% | 100% |
| Ethnicity | ||
| American Indian | 2 (15.4%) | 0 (0.0%) |
| African American/Black | 0 (0.0%) | 1 (1.4%) |
| Asian | 0 (0.0%) | 2 (2.9%) |
| Caucasian/White | 9 (69.2%) | 56 (81.2%) |
| Hispanic | 1 (7.7%) | 7 (10.1%) |
| Native Hawaiian | 1 (7.7%) | 1 (1.4%) |
| Multi | 0 (0.0%) | 2 (2.9%) |
P-value <.05.
| . | Reported injury . | No reported injury . |
|---|---|---|
| No. of participants, n | 13 | 69 |
| Age, years (mean ± SD) | 27.5 ± 4.2 | 25.0 ± 3.8* |
| Gender, male | 100% | 100% |
| Ethnicity | ||
| American Indian | 2 (15.4%) | 0 (0.0%) |
| African American/Black | 0 (0.0%) | 1 (1.4%) |
| Asian | 0 (0.0%) | 2 (2.9%) |
| Caucasian/White | 9 (69.2%) | 56 (81.2%) |
| Hispanic | 1 (7.7%) | 7 (10.1%) |
| Native Hawaiian | 1 (7.7%) | 1 (1.4%) |
| Multi | 0 (0.0%) | 2 (2.9%) |
| . | Reported injury . | No reported injury . |
|---|---|---|
| No. of participants, n | 13 | 69 |
| Age, years (mean ± SD) | 27.5 ± 4.2 | 25.0 ± 3.8* |
| Gender, male | 100% | 100% |
| Ethnicity | ||
| American Indian | 2 (15.4%) | 0 (0.0%) |
| African American/Black | 0 (0.0%) | 1 (1.4%) |
| Asian | 0 (0.0%) | 2 (2.9%) |
| Caucasian/White | 9 (69.2%) | 56 (81.2%) |
| Hispanic | 1 (7.7%) | 7 (10.1%) |
| Native Hawaiian | 1 (7.7%) | 1 (1.4%) |
| Multi | 0 (0.0%) | 2 (2.9%) |
P-value <.05.
Comparison of Sleep Outcome Measures between the Rangers that Reported an Injury and the Rangers that Did Not
| Outcome measure . | Reported injury . | No reported injury . | P-value . |
|---|---|---|---|
| PSQI Global Score | 6.7 ± 3.7 | 4.5 ± 2.7 | .012 |
| Component 1 | 1.2 ± 2.4 | 0.7 ± 0.7 | .176 |
| Component 2 | 1.5 ± 0.9 | 0.9 ± 0.8 | .016 |
| Component 3 | 0.8 ± 0.5 | 0.6 ± 0.6 | .327 |
| Component 4 | 0.6 ± 0.8 | 0.2 ± 0.4 | .091 |
| Component 5 | 1.3 ± 0.7 | 1.1 ± 0.5 | .378 |
| Component 6 | 1.5 ± 1.3 | 0.4 ± 0.8 | .013 |
| Component 7 | 0.8 ± 0.7 | 0.7 ± 0.9 | .820 |
| Insomnia Severity Index | 10.9 ± 3.7 | 7.2 ± 4.1 | .003 |
| Stanford Sleepiness Scale | 2.8 ± 1.3 | 2.9 ± 1.4 | .808 |
| Sleep Quality (0-100) | 50.8 ± 17.5 | 68.9 ± 18.3 | .001 |
| Sleep Duration | 6.1 ± 1.0 hours | 6.5 ± 0.9 hours | .099 |
| Outcome measure . | Reported injury . | No reported injury . | P-value . |
|---|---|---|---|
| PSQI Global Score | 6.7 ± 3.7 | 4.5 ± 2.7 | .012 |
| Component 1 | 1.2 ± 2.4 | 0.7 ± 0.7 | .176 |
| Component 2 | 1.5 ± 0.9 | 0.9 ± 0.8 | .016 |
| Component 3 | 0.8 ± 0.5 | 0.6 ± 0.6 | .327 |
| Component 4 | 0.6 ± 0.8 | 0.2 ± 0.4 | .091 |
| Component 5 | 1.3 ± 0.7 | 1.1 ± 0.5 | .378 |
| Component 6 | 1.5 ± 1.3 | 0.4 ± 0.8 | .013 |
| Component 7 | 0.8 ± 0.7 | 0.7 ± 0.9 | .820 |
| Insomnia Severity Index | 10.9 ± 3.7 | 7.2 ± 4.1 | .003 |
| Stanford Sleepiness Scale | 2.8 ± 1.3 | 2.9 ± 1.4 | .808 |
| Sleep Quality (0-100) | 50.8 ± 17.5 | 68.9 ± 18.3 | .001 |
| Sleep Duration | 6.1 ± 1.0 hours | 6.5 ± 0.9 hours | .099 |
Abbreviation: PSQI = Pittsburgh Sleep Quality Index.
Mean ± standard deviation. Bold-face = P < .05. Significant between-group differences remained the same after conducting an analysis of variance, controlling for age.
Comparison of Sleep Outcome Measures between the Rangers that Reported an Injury and the Rangers that Did Not
| Outcome measure . | Reported injury . | No reported injury . | P-value . |
|---|---|---|---|
| PSQI Global Score | 6.7 ± 3.7 | 4.5 ± 2.7 | .012 |
| Component 1 | 1.2 ± 2.4 | 0.7 ± 0.7 | .176 |
| Component 2 | 1.5 ± 0.9 | 0.9 ± 0.8 | .016 |
| Component 3 | 0.8 ± 0.5 | 0.6 ± 0.6 | .327 |
| Component 4 | 0.6 ± 0.8 | 0.2 ± 0.4 | .091 |
| Component 5 | 1.3 ± 0.7 | 1.1 ± 0.5 | .378 |
| Component 6 | 1.5 ± 1.3 | 0.4 ± 0.8 | .013 |
| Component 7 | 0.8 ± 0.7 | 0.7 ± 0.9 | .820 |
| Insomnia Severity Index | 10.9 ± 3.7 | 7.2 ± 4.1 | .003 |
| Stanford Sleepiness Scale | 2.8 ± 1.3 | 2.9 ± 1.4 | .808 |
| Sleep Quality (0-100) | 50.8 ± 17.5 | 68.9 ± 18.3 | .001 |
| Sleep Duration | 6.1 ± 1.0 hours | 6.5 ± 0.9 hours | .099 |
| Outcome measure . | Reported injury . | No reported injury . | P-value . |
|---|---|---|---|
| PSQI Global Score | 6.7 ± 3.7 | 4.5 ± 2.7 | .012 |
| Component 1 | 1.2 ± 2.4 | 0.7 ± 0.7 | .176 |
| Component 2 | 1.5 ± 0.9 | 0.9 ± 0.8 | .016 |
| Component 3 | 0.8 ± 0.5 | 0.6 ± 0.6 | .327 |
| Component 4 | 0.6 ± 0.8 | 0.2 ± 0.4 | .091 |
| Component 5 | 1.3 ± 0.7 | 1.1 ± 0.5 | .378 |
| Component 6 | 1.5 ± 1.3 | 0.4 ± 0.8 | .013 |
| Component 7 | 0.8 ± 0.7 | 0.7 ± 0.9 | .820 |
| Insomnia Severity Index | 10.9 ± 3.7 | 7.2 ± 4.1 | .003 |
| Stanford Sleepiness Scale | 2.8 ± 1.3 | 2.9 ± 1.4 | .808 |
| Sleep Quality (0-100) | 50.8 ± 17.5 | 68.9 ± 18.3 | .001 |
| Sleep Duration | 6.1 ± 1.0 hours | 6.5 ± 0.9 hours | .099 |
Abbreviation: PSQI = Pittsburgh Sleep Quality Index.
Mean ± standard deviation. Bold-face = P < .05. Significant between-group differences remained the same after conducting an analysis of variance, controlling for age.
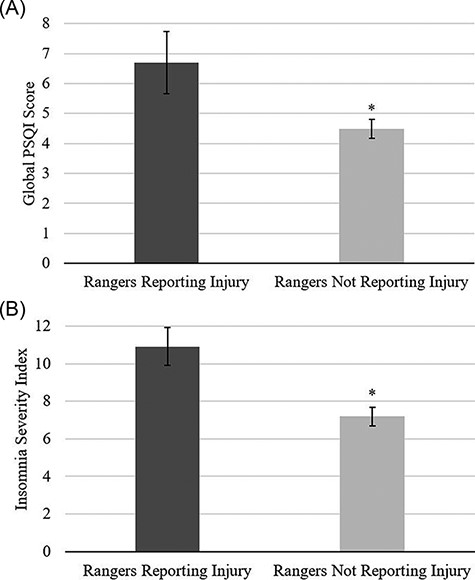
Rangers that reported an injury, compared to those that did not, had a significantly higher Global Pittsburgh Quality Sleep Index (PSQI) score (A) and Insomnia Severity Index (ISI) score (B), both indicative of poorer sleep. Average global PSQI scores above 5 are often used to distinguish good and poor sleepers. Significant between group differences remained the same after conducting an analysis of variance, controlling for age. Mean ± standard error. *P-value <.05.
DISCUSSION
In this study of male Army Rangers, during a standard duty day in garrison, slightly more than one in 10 reported having a musculoskeletal injury, and having poor sleep quality was associated with reporting an injury. The prevalence of injured Rangers in this study was significantly lower than the 50% yearly incidence rate reported in other cohorts of Rangers.2 Direct comparisons are challenging as this study simply asked participants if they had a musculoskeletal injury at the time of completing the questionnaires compared to using more frequent injury surveillance surveys, medical records reviews, and other queries of healthcare utilization over a 1-year period. While a recent large study involving infantry soldiers provided support for the use of survey data for the evaluation of injury data,16 the other study monitored injuries over a longer period. Similarly, another study involving Special Operations soldiers reported an injury incident rate around 50% when asking how many musculoskeletal injuries the soldiers sustained over the preceding 12 months5; however, it was unclear how many of those soldiers were Rangers. The current study found that injured Rangers had an average global PSQI score above 5, which is a score often used to distinguish good and poor sleepers,12 while uninjured Rangers had an average global PSQI score below 5. In addition, the injured Rangers rated their average sleep quality over the preceding week almost 20% lower than those that did not report an injury and had significantly higher (worse) ISI scores, which is an endorsement of more insomnia symptoms. Collectively, in this cohort, there appears to be an association between reporting a musculoskeletal injury and sleep quality/disturbances, whether it was over the previous 30 days (PSQI), 2 weeks (ISI), or the week prior. Although this cross-sectional study was the first to report an association between sleep quality and musculoskeletal injury in a military population, similar associations have been observed in a longitudinal study involving 297 collegiate cross-country athletes.10 That study found that runners with poor sleep quality had an increased risk of sustaining a new injury or aggravating an existing injury during the season. In other non-athlete civilian populations, sleep problems17 and poor sleep quality11 have been associated with increased work injuries.
Due to the cross-sectional nature of the data collected in this study, it is unknown whether the poor sleep quality was a contributing mechanism to the reported injury or whether having an injury contributed to the poor sleep quality. It is reasonable to believe that the relationship is bi-directional. There is a possibility that the symptoms (i.e., pain) associated with any injury may have a negative impact on sleep quality. Acute and chronic pain has been associated with disturbed or poorer sleep,18,19 and a systematic review reported that chronic low back pain patients have greater sleep disturbances compared with controls.20 Another recent review found that sleep disturbance may impair key processes that contribute to the development and maintenance of chronic pain and that sleep impairments have been found to be a stronger predictor of pain than pain is of sleep impairments.21 Future research should use longitudinal designs to further evaluate this relationship, including whether strategies (i.e., sleep hygiene education) that improve sleep quality have any subsequent impact on injury incidence rates or injury recovery rates. Although research is needed to substantiate and improve the efficacy of specific sleep hygiene recommendations, it could potentially play a role in the promotion of sleep and subsequent health.22 In addition, research that includes more characteristics about how injuries may be negatively affecting sleep quality (i.e., injury date/type/severity/location/perception, pain, impact on job performance/mental well-being, etc.) is warranted. Considering the high injury incidence and the multifactorial risks associated with injuries in Rangers,2 it is promising to find a potential modifiable factor.
Sleep duration, as well as subjective sleepiness, in the Rangers was not associated with reported injuries; however, both the injured group and uninjured group averaged less than the recommended amount of sleep for adults, which is over 7 hours per night.23 The shorter sleep duration reported is consistent with what has been documented in other military populations.24–26 The lack of relationship between sleep duration and injury occurrence was in contrast to a large study involving over 7,500 Special Operations soldiers that found a linear trend of injury incidence decreasing with increased reported hours of sleep per night.5 While this study did not specify the percentage of soldiers that were Rangers (if any), at the extreme end, soldiers who self-reported sleeping 4 hours or less, compared to those who reported 8 hours or more, were over twice as likely to report a musculoskeletal injury over the previous 12 months. Two other studies in younger athletes have reported that athletes who slept less than 8 hours were more likely to experience an injury than those who slept 8 hours or more.6,7 In the current study, only five (6%) participants reported sleeping 8 hours (zero reported sleeping more than 8 hours), and all five did not report an injury. With the vast majority of the participants reporting between 6 and 8 hours of sleep per night, there is a chance the lack of variance in the sleep duration limited the ability to evaluate the relationship between sleep duration and musculoskeletal injury. However, the lack of relationship between sleep duration and injury occurrence has also been previously reported in elite Australian footballers27 and college football players.9 The authors caution the interpretation of the findings and encourage further investigations into whether a relationship between sleep duration and musculoskeletal injury exists in other Rangers and other military personnel/units, especially considering the high prevalence of insufficient sleep in these populations. There can also be other negative consequences of insufficient sleep in service members, such as increased risky behaviors28 and mission-related accidents.29 In addition, chronically sleep-deprived individuals may exhibit increased risk-taking behaviors and deficiencies in reasoning,30 which in return may cause soldiers to make poor decisions that consequently lead to a musculoskeletal injury.
This study had limitations. First, all data were self-reported. There is a chance that the musculoskeletal injuries in this cohort were under-reported, especially if there was any concern that the information would be utilized to make decisions on training or deployments. While research in infantry soldiers has shown a high accuracy of self-reported injuries,16 future research should also consider gaining injury information from the unit’s medical team or through a soldier’s medical records. In addition, musculoskeletal injuries should be operationally defined for the participants. Although there are varied injury definitions in the literature, just clarifying that “musculoskeletal injuries” impact the muscles, bones, tendons, ligaments, joints, cartilage, and other connective tissues31 may improve injury reporting/surveillance. Similarly, future research should incorporate objectively measuring sleep (via actigraphy) to help ascertain whether subjective sleep metrics are accurately described. This study only involved relatively young male Rangers. Future research should incorporate females and older Rangers, as well as other organizations to see if similar results are observed. There may be unit- or geographic-specific risk factors associated with injuries that comparing across units would help reveal.
CONCLUSION
In this cohort of young male Army Rangers, those with a musculoskeletal injury reported poorer sleep quality than uninjured Rangers. Sleep duration was not associated with reported injuries; however, there was minimal variance in sleep durations, and both the injured group and uninjured group averaged less than the recommended amount of sleep. Further investigation into the relationship between musculoskeletal injury and sleep in military personnel is warranted.
FUNDING
This project was funded by the Military Operational Medicine Research Program (MOMRP).
CONFLICT OF INTEREST STATEMENT
None of the authors have any relevant conflicts of interest to report.



