-
PDF
- Split View
-
Views
-
Cite
Cite
Casey Mueller, Colleen M Moreland, Keith L Jackson, Dana Hensley, Anton Lacap, K Aaron Shaw, Pectoralis Major Tendon Tears During Airborne Operations: Are These Injuries Isolated?, Military Medicine, Volume 188, Issue 7-8, July/August 2023, Pages e1759–e1762, https://doi.org/10.1093/milmed/usac149
Close - Share Icon Share
ABSTRACT
Pectoralis major tendon tears are an injury pattern often treated in military populations. Although the majority of pectoralis major tendon tears occur during eccentric loading as in bench press weightlifting, military service members may also experience this injury from a blunt injury and traction force produced by static line entanglement during airborne operations. Although these injuries rarely occur in isolation, associated injury patterns have not been investigated previously.
After obtaining institutional review board approval, medical records were reviewed for all patients who underwent surgical repair of a pectoralis major tendon tear sustained during static line parachuting at a single institution. Radiology imaging, operative notes, and outpatient medical records were examined to determine concomitant injury patterns for each patient identified over a 4-year study period.
Twenty-five service members met the study inclusion criteria. All patients underwent presurgical magnetic resonance imaging. Of these 25 service members, 10 (40%) presented with a total of 13 concomitant injuries identified on physical exams or imaging studies. The most common associated injuries were injuries to the biceps brachii and a partial tear of the anterior deltoid. Biceps brachii injuries consisted of muscle contusion proximal long head tendon rupture, proximal short head tendon rupture, partial muscle laceration, and complete muscle transection. Additional concomitant injuries included transection of coracobrachialis, a partial tear of the inferior subscapularis tendon, antecubital fossa laceration, an avulsion fracture of the sublime tubercle, and an avulsion fracture of the coracoid process.
Military static line airborne operations pose a unique risk of pectoralis major tendon tear. Unlike the more common bench press weightlifting tear mechanism, pectoralis major tendon tears associated with static line mechanism present with a concomitant injury in 40% of cases, with the most common associated injury occurring about the biceps brachii. Treating providers should have a high index of suspicion for concomitant injuries when treating pectoralis major tendon tears from this specific mechanism of injury.
INTRODUCTION
Pectoralis major (PM) tendon tears most frequently occur during weightlifting as a result of bench press eccentric loading.1,2 This most commonly results in a tear of the sternal head with or without the involvement of the clavicular head of the PM that occurs without concomitant injuries. Recently, a new mechanism has been reported for PM tears secondary to a blunt trauma forced hyperabduction and external rotation moment to the arm.3,4 This mechanism was originally reported in military airborne operations where the static line connected to the service member’s parachute forces the arm into the described motion, inducing a traumatic tear of the PM.3–5 This forced hyperabduction motion can also be sustained in nonmilitary situations, such as in a motor vehicle collision, zip lining, and motorcycle accidents.4,5
The forced hyperabduction and external rotation mechanism of PM tear are unique in comparison to that typically encountered with eccentric loading.4 Additionally, this high-energy blunt trauma from the static line parachuting mechanism creates the potential for associated injuries to the arm and shoulder girdle. To date, no investigations have reported potential concomitant injury patterns or their frequency in patients with forced hyperabduction PM tears. In this study, we evaluate PM tears because of static line parachuting injuries to investigate concomitant injury patterns to improve recognition and limit potential morbidity that could negatively influence the patient’s recovery through prompt recognition and treatment of their injuries.
METHODS
After obtaining approval from the institutional review board, a retrospective descriptive study was performed of all patients undergoing PM repairs at a single institution through chart review over a 4-year period (January 1, 2012 to December 31, 2016). Patients were considered for study inclusion if they (1) had a PM tendon repair because of a static line injury during airborne operations, (2) were active duty military service members, (3) were greater than 18 years of age, and (4) had a preoperative MRI study performed to evaluate injury. Patients were excluded if they did not undergo preoperative MRI or if operative reports could not be reviewed for tear characteristics.
Patients meeting inclusion criteria underwent a review of their medical records to identify demographic information (gender and age at time of injury), injury information (date of injury and mechanism of injury), and associated injuries. MRI studies were reviewed using the institution’s digital radiology imaging system (IMPAX, AGFA Healthcare, Greenville, SC) to determine associated injuries and patterns. Operative reports were also reviewed to identify concomitant injuries that were treated operatively. Concomitant injuries were subdivided according to the anatomic region involved. Data were collated using SPSS statistical package version 24 (SPSS Inc., Chicago, IL) to generate descriptive statistics.
RESULTS
Over the 4-year study period, a total of 25 soldiers were identified through chart review as sustaining a static line-induced PM tear during airborne operations (average age 31.68 ± 6.49 years, 100% male). All subjects underwent presurgical MRI to confirm the presence of the PM tear and the specific location of the tear within the tendon.
Of the 25 service members who met the inclusion criteria, 10 presented with a total of 13 concomitant injuries identified on physical exams or imaging studies. The most common associated injuries were injuries to the biceps brachii (N = 6, 24%) and a partial tear of the anterior deltoid (N = 3, 12%). Biceps brachii injuries were further subdivided into muscle contusion, proximal long head tendon rupture, proximal short head tendon rupture, partial muscle laceration, and complete muscle transection (Fig. 1). Additional identified concomitant injuries include anterior deltoid laceration (Fig. 2) transection of coracobrachialis, a partial tear of the inferior subscapularis tendon, antecubital fossa laceration, an avulsion fracture of the sublime tubercle, and an avulsion fracture of the coracoid process (Table I).
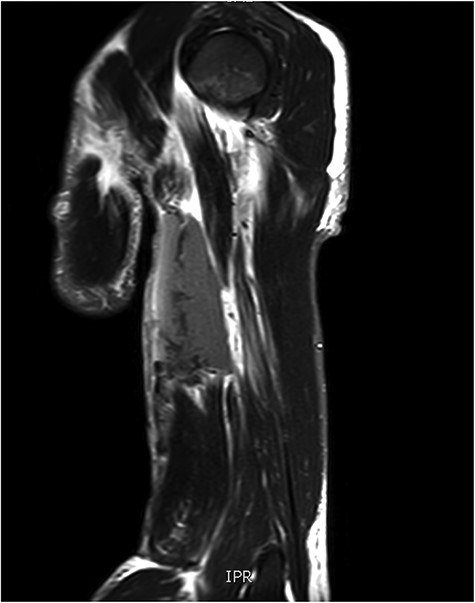
T2 sagittal view of complete biceps brachii muscle belly transection.
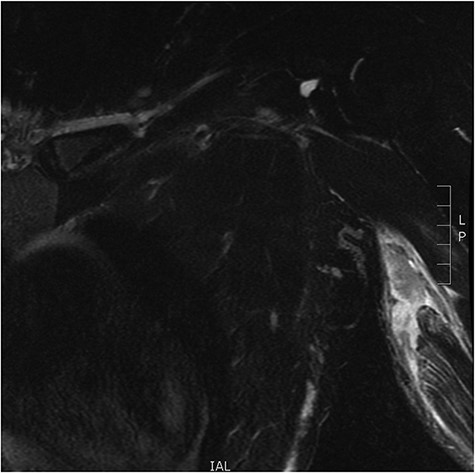
Coronal view of complete coracobrachialis rupture on T2 magnetic resonance imaging image.
Breakdown of Injuries Associated With Pectoralis Major Tear in the Setting of Static Line Injuries
| Associated injury . | Number, N/25 . | Percentage . |
|---|---|---|
| Biceps brachii injury | N = 6 | 24 |
| Long head tendon rupture | N = 1 | 4 |
| Short head tendon rupture | N = 1 | 4 |
| Partial muscle laceration | N = 1 | 4 |
| Complete muscle transection | N = 1 | 4 |
| Muscle contusion | N = 2 | 8 |
| Anterior deltoid partial laceration | N = 3 | 12 |
| Transection of coracobrachialis | N = 1 | 4 |
| Partial tear of subscapularis | N = 1 | 4 |
| Avulsion fracture of sublime tubercle | N = 1 | 4 |
| Avulsion fracture of coracoid | N = 1 | 4 |
| Associated injury . | Number, N/25 . | Percentage . |
|---|---|---|
| Biceps brachii injury | N = 6 | 24 |
| Long head tendon rupture | N = 1 | 4 |
| Short head tendon rupture | N = 1 | 4 |
| Partial muscle laceration | N = 1 | 4 |
| Complete muscle transection | N = 1 | 4 |
| Muscle contusion | N = 2 | 8 |
| Anterior deltoid partial laceration | N = 3 | 12 |
| Transection of coracobrachialis | N = 1 | 4 |
| Partial tear of subscapularis | N = 1 | 4 |
| Avulsion fracture of sublime tubercle | N = 1 | 4 |
| Avulsion fracture of coracoid | N = 1 | 4 |
Breakdown of Injuries Associated With Pectoralis Major Tear in the Setting of Static Line Injuries
| Associated injury . | Number, N/25 . | Percentage . |
|---|---|---|
| Biceps brachii injury | N = 6 | 24 |
| Long head tendon rupture | N = 1 | 4 |
| Short head tendon rupture | N = 1 | 4 |
| Partial muscle laceration | N = 1 | 4 |
| Complete muscle transection | N = 1 | 4 |
| Muscle contusion | N = 2 | 8 |
| Anterior deltoid partial laceration | N = 3 | 12 |
| Transection of coracobrachialis | N = 1 | 4 |
| Partial tear of subscapularis | N = 1 | 4 |
| Avulsion fracture of sublime tubercle | N = 1 | 4 |
| Avulsion fracture of coracoid | N = 1 | 4 |
| Associated injury . | Number, N/25 . | Percentage . |
|---|---|---|
| Biceps brachii injury | N = 6 | 24 |
| Long head tendon rupture | N = 1 | 4 |
| Short head tendon rupture | N = 1 | 4 |
| Partial muscle laceration | N = 1 | 4 |
| Complete muscle transection | N = 1 | 4 |
| Muscle contusion | N = 2 | 8 |
| Anterior deltoid partial laceration | N = 3 | 12 |
| Transection of coracobrachialis | N = 1 | 4 |
| Partial tear of subscapularis | N = 1 | 4 |
| Avulsion fracture of sublime tubercle | N = 1 | 4 |
| Avulsion fracture of coracoid | N = 1 | 4 |
Of these associated injuries, additional surgical treatment was provided in only two patients. One patient with complete muscle transection of the biceps brachii who underwent operative repair of the tear using suture fixation with a multistrand core jacketed suture (FiberWire, Arthrex). Recovery of biceps function in this patient was complicated by an associated injury to the musculocutaneous nerve that did not require neural repair. The patient developed a painful scar and subsequently underwent scar revision with suture removal from the biceps, performed 153 days from the initial injury. The second additional surgical management of an associated injury was a partial tear of the anterior deltoid which developed a fascial defect with a large seroma and underwent an aspiration for seroma decompression.
DISCUSSION
PM tears are most described as occurring in bench-pressing exercises during eccentric contraction and occur as isolated injuries.2 This study reports on the rate of concomitant injuries in military service members who sustain a traumatic PM tear during static line airborne operations.6 These injuries occur because of violent, forced hyperabduction and external rotation from direct blunt trauma to the proximal medial arm.3,4 This study identified a 40% rate of concomitant injuries, most commonly being injuries to the biceps brachii, followed by the deltoid.
Static line injuries almost exclusively occur in junior enlisted army service members between 25 and 34 years of age, although most PM tears occur as bench press weightlifting injuries in recreational weightlifters.2,7–9 With different mechanisms of injury, there are different tear patterns in the PM tendon and associated injuries. Eccentric loading mechanism injuries often occur at the myotendinous junction or bony insertion and are not associated with other injuries. Synovec et al. compared MRIs of PM tears sustained from eccentric loading mechanisms to the blunt trauma. The authors demonstrated that eccentric loading mechanism PM tears occur most commonly at the myotendinous junction (44%), with 40% occurring as a complete tendon avulsion. This contrasts with static line injuries where 6% were myotendinous injuries with 81% as complete tendinous avulsion injuries.6,7,10
Differences in tear location of the PM tendon may correlate to outcomes. Shaw et al. demonstrated that when treated within 6 weeks of injury, static line injuries have improved postoperative strength and function compared to standard eccentric loading injuries.3,4,11 Additionally, acute treatment of either traumatic or eccentric loading injury mechanism has improved functional outcomes compared to delayed surgical repair or reconstruction.12 There was a 100% rate of return to full preoperative duty in static line injuries versus a 94% return rate in eccentric loading injuries when treated acutely compared to only a 78% return rate to full duty in delayed surgery requiring allograft PM tendon reconstruction.4,12,13 Additionally, Shakir et al. demonstrated equal outcomes when PM tears were repaired in the deployed setting when compared to in the CONUS setting.8,9,14
Biceps brachii concomitant injuries were present in 24% of patients with static line PM tears, although 12% of patients had a concomitant injury to the deltoid. Most of these injuries are amenable to nonsurgical management; however, a small percentage did require operative repair. Surgical repair of a concomitant biceps brachii injury was required in one patient, which can cause significant morbidity if not treated in a timely manner.15
Biceps brachii muscle belly injuries are rarely reported in the literature, with most reports arising from Fort Bragg in the setting of static line airborne operations. Heckman et al. reported improved outcomes with treatment within the first 72 hours demonstrating comparable results with hematoma evacuation and hyperflexion splinting versus surgical repair. The operative group more consistently had a palpable gap of less than 2 cm compared to the aspiration group; however, each treated (aspiration or surgery) group returned to 77% of full elbow flexion strength compared to 53% of elbow flexion strength in the splinting only group.15 Additionally, Kragh et al. demonstrated that surgical repair in the setting of completed biceps brachii rupture resulted in improved supination, cosmetic appearance, and patient satisfaction when compared to non-operative treatment.16
Many studies have demonstrated superior outcomes for PM repairs and biceps brachii muscle transections when treated within 3 weeks and 3 days, respectively. If there is suspicion for PM tear, it should be assessed and treated expeditiously with elevated concern for concomitant injury, especially biceps brachii tear, as both injuries have good to excellent outcomes and minimal complications when recognized and treated acutely.1,5,7,13,15,17
This study has several limitations. As a retrospective review, it has inherent bias and is reliant upon the quality and accuracy of medical documentation. Although this is in part addressed by the review of advanced imaging studies obtained at the time of injury, the potential for missed or inaccurate information remains. Treatment was provided by multiple orthopedic surgeons without a standard algorithm for treatment which introduces additional variability in the data. Follow-up after injury was limited, and the long-term effects and functional implications of these concomitant injury patterns are not known.
CONCLUSION
Pectoralis major tendon tears because of blunt trauma hyperabduction mechanisms, as seen in static line airborne operations, represent a unique injury pattern. Unlike an eccentric weightlifting mechanism, these injuries present with a concomitant injury in 40% of cases with the most common associated injury involving the biceps brachii. Treating providers should have a high index of suspicion for concomitant injuries when evaluating individuals with this specific injury mechanism.
ACKNOWLEDGMENTS
None declared.
FUNDING
None declared.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
Author notes
The views expressed are solely those of the authors and do not reflect the official policy or position of the U.S. Army, U.S. Navy, U.S. Air Force, the Department of Defense, or the U.S. Government.
- magnetic resonance imaging
- medical records
- diagnostic radiologic examination
- institutional review board
- lacerations
- military personnel
- outpatients
- surgical procedures, operative
- tendon injuries
- traction
- nonpenetrating wounds
- diagnostic imaging
- radiology specialty
- avulsion fracture
- biceps brachii muscle
- muscle laceration
- muscle contusion
- coracoid process of scapula
- deltoid muscle
- cubital fossa
- coracobrachialis muscle
- subscapularis tendon
- pectoralis major tendon
- mechanism of injury
- bench press



