-
PDF
- Split View
-
Views
-
Cite
Cite
Karey L O’Hara, Sharlene A Wolchik, C Aubrey Rhodes, Rana N Uhlman, Irwin N Sandler, Jenn-Yun Tein, Preventing Adverse Outcomes for Bereaved Youth: Indirect Effects From a Randomized Trial of the Family Bereavement Program on Fear of Abandonment, Grief, and Mental Health, Journal of Pediatric Psychology, Volume 49, Issue 4, April 2024, Pages 247–258, https://doi.org/10.1093/jpepsy/jsad052
Close - Share Icon Share
Abstract
We investigated whether the self-system belief of fear of abandonment mediated the effects of intervention-induced change in 2 protective factors—positive parenting and adaptive coping—and one risk factor—stressful events—on youth mental health problems and maladaptive grief. This study extends prior research on fear of abandonment in youth who experience parental death by examining pathways through which a program reduced fear of abandonment and, in turn, affected subsequent pathways to child mental health problems in the context of a randomized experiment.
This is a secondary data analysis study. We used data from the 4-wave longitudinal 2-arm parallel randomized controlled trial of the Family Bereavement Program conducted between 1996 and 1999 in a large city in the Southwestern United States. The sample consisted of 244 offspring between 8 and 16 at the pretest. They were assessed again at posttest, 11-month follow-up, and 6-year follow-up. Offspring, caregivers, and teachers provided data.
Mediation analyses indicated that intervention-induced reductions in stressful events were prospectively associated with a lower fear of abandonment. For girls, fear of abandonment was related to self-reported maladaptive grief and teacher-reported internalizing problems 6 years later.
This study extends prior research on the relation between intervention-induced changes in risk and protective factors and improvements in outcomes of bereaved youth. The findings support the reduction of stressful events as a key proximal target of prevention programs for bereaved children.
Introduction
Although most youth who experience the death of a parent do not develop significant problems, they are at increased risk of adverse mental health and development consequences over time (Berg et al., 2016; Brent et al., 2009; Melhem et al., 2007; Pham et al., 2018). Some parentally bereaved youth also evidence maladaptive grief (estimates of 10%–40%; Kaplow et al., 2018; Melhem et al., 2011), which is associated with an increased risk of depression, behavior problems, suicidality, and functional impairment (Boelen et al., 2017; Melhem et al., 2011; Sandler et al., 2021). Prior research also indicates the potential for long-term physical health impacts (for a review, see Luecken & Roubinov, 2012).
Prevention programs promote pediatric health and development after major life events by reducing risk factors and fostering protective factors associated with short- and long-term problems (e.g., Sandler et al., 2015). The Family Bereavement Program (FBP; Ayers et al., 2013) promotes youth resilience following parental death by targeting the individual-level and environmental-level risk and protective factors of positive parenting, adaptive coping, and stressful events. The FBP includes caregiver, adolescent, and child group sessions that teach skills to bolster the caregiver–child relationship, strengthen adaptive coping, and reduce exposure to stressful events which, in turn, are theorized to protect youth psychological adjustment by affecting basic psychological needs, which are reflected in self-system beliefs (Sandler, 2001).
The Role of Self-System Beliefs in Targeted Prevention Programs
Self-system beliefs are an indicator of how adversities, such as parental bereavement, impact fulfillment of basic psychological needs, which, when threatened, can lead to mental health problems (Sandler, 2001; Skinner & Wellborn, 1994). Prevention scientists have good reason to study the role self-system beliefs play in adversity and resilience because they may be key mediators linking modifiable protective factors with downstream pediatric health outcomes. For example, characterizing the most salient basic psychological needs that are threatened in specific contexts and how correlated self-system beliefs alter the trajectory of adjustment sheds light on potentially modifiable processes in resilience. Such process-oriented research is critical for developing theory-driven preventive interventions and identifying key targets for change.
Salient Self-System Beliefs in Parental Bereavement
The basic psychological need for social relatedness is particularly salient for parentally bereaved youth. Not only have they lost a caregiver, the cascade of smaller death-related stressors (e.g., changing households, neighborhoods, and/or schools) often disrupt other meaningful social ties. From a theoretical perspective, these experiences affect the self-system belief of fear of abandonment, most prominently evidenced in bereaved youth through concerns about whether they will continue to be cared for by their caregivers. In correlational studies of bereaved youth, fear of abandonment was the most robust self-system belief linking bereavement-related risk and protective factors with mental health problems and maladaptive grief (Sandler, 2001; Wolchik et al., 2006, 2008).
Support for Proposed Multi-Link Mediation Model
Figure 1 presents the multi-link theoretical model that was tested in this paper. Below, we review the theoretical and empirical support for each link in the model.
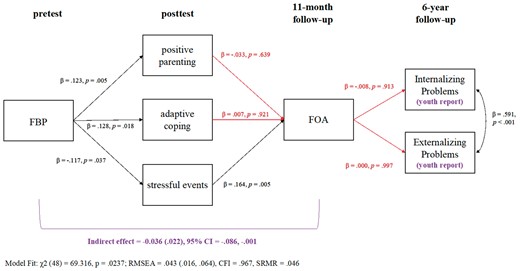
Standardized regression coefficients observed in theoretical multi-link prospective mediation model for youth-reported internalizing and externalizing problems. Note. FBP = Family Bereavement Program; FOA = fear of abandonment.
Prior studies demonstrate that the FBP increased positive parenting and adaptive coping, decreased exposure to stressful events (Sandler et al., 2003), and led to significantly decreased mental health problems for girls at the 11-month follow-up (Tein et al., 2006) and decreased maladaptive grief for boys and girls at the 6-year follow-up (Sandler et al., 2010). Youth in the FBP also had fewer internalizing (teacher report; d = 0.57) and externalizing (youth, caregiver, and teacher reports; d = 0.31 to 0.59) problems than youth in the literature control condition at the 6-year follow-up (Sandler et al., 2010).
In this study, we used data from this trial to examine whether fear of abandonment, a plausible theoretical mechanism, accounted for the links between intervention-induced changes in the targeted protective (i.e., positive parenting, adaptive coping) and risk (i.e., stressful events) factors and youth mental health problems and maladaptive grief. Each factor is theoretically related to the degree of fulfillment of the basic need of social relatedness, which we assessed with a measure of fear of abandonment. Many researchers posit that positive parenting plays a significant role in a youth’s sense of belonging in the family and attachment to caregivers (Baumeister & Leary, 1995; Sandler, 2001; Skinner & Wellborn, 1994). Parental death can lead to surviving caregivers being less emotionally available, less attentive to the youth’s needs, and inconsistent with enforcing rules and following through on discipline, all of which can threaten the youth’s sense of security in their most salient family relationship. Exposure to bereavement-related stressful events, including reduced contact with family and friends and concerns related to witnessing caregiver distress, can also threaten the youth’s sense of security in their caregiving relationship. Their use of poor coping strategies, such as avoiding previously enjoyed activities or isolating from loved ones, may exacerbate these threats.
Several correlational studies have found that positive parenting and stressful events are associated with fear of abandonment (Little et al., 2009; Sandler, 2001; Wolchik et al., 2006, 2008). Wolchik et al. (2006, 2008) showed that fear of abandonment was positively related to mental health problems and maladaptive grief concurrently and prospectively over 11 months and mediated the relations between pretest stressful events and positive parenting and mental health problems and maladaptive grief at the 3-month follow-up. To our knowledge, only one study found an association between coping and fear of abandonment. Wolchik et al. (2006, 2008) found that coping efficacy (i.e., how children view their coping efforts) was concurrently related to the fear of abandonment experienced by bereaved youth.
Current Study
This is a secondary data analysis study that extends theoretical models of self-system beliefs after bereavement by examining their role in a multi-link theoretical pathway from a prevention program to mental health problems and maladaptive grief over time. It also advances our understanding of whether the self-system belief of fear of abandonment was a pathway through which the FBP reduced mental health problems and maladaptive grief. We used the full longitudinal sample from the FBP efficacy trial whereas prior studies on FOA (i.e., Wolchik et al., 2006, 2008) used only the control group. We tested a theoretical model in which the program affects positive parenting, stressful events, and adaptive coping at posttest, leading to a reduction in fear of abandonment at the 11-month follow-up, which in turn, mediates the program effects on youth’s mental health problems and maladaptive grief at the 6-year follow-up. Studying these effects using a randomized design increases the strength of causal inference of the path between the risk and protective factors and fear of abandonment by examining whether experimentally induced change in positive parenting, adaptive coping, and stressful events precedes subsequent changes in fear of abandonment, above and beyond initial levels of fear of abandonment. This design disentangles the associations between positive parenting, stressful events, adaptive coping, and fear of abandonment. However, the links between fear of abandonment and mental health problems and maladaptive grief are not impacted by the randomized design.
We predicted that FBP participation would improve positive parenting and adaptive coping and reduce stressful events at posttest (T2; these paths are established; see Sandler et al., 2003). We expected that higher positive parenting, higher adaptive coping, and fewer stressful events at posttest (T2) would predict lower fear of abandonment at the 11-month follow-up (T3). Finally, we expected lower fear of abandonment at the 11-month follow-up (T3) would mediate program effects to reduce internalizing problems, externalizing problems, and maladaptive grief at the 6-year follow-up (T4). In a set of exploratory analyses, we tested the same theoretical model to examine gender and age moderation effects.
Methods
We used the CONSORT reporting guidelines (Schulz et al., 2010). The final checklist is available as Supplementary File 1.
Participants
Participants were 244 youth and their caregivers from 156 families who participated in a two-arm (intervention vs. active control) parallel randomized controlled trial of the FBP conducted between 1996 and 1999 in a large city in the Southwestern United States (see Sandler et al., 2003). Six-year follow-up data were collected between 2002 and 2005 (see Sandler et al., 2010). Ninety families with 135 children were randomized to the intervention condition; 66 families with 109 children were randomized to the active control condition. Youth ages 8–16 years were included in the trial. This age range was selected because youth in this age range could theoretically benefit from the intervention strategies in the program and could complete valid and reliable measures that assessed program effects.
Bereaved families were recruited from the community (e.g., schools and service agencies) and by mail solicitation (see Sandler et al., 2003 for full data collection procedures). Eligibility criteria were as follows: (1) family experienced parental death between 4 and 30 months before study entry, (2) family had one or more children between the ages of 8 and 16 years, (3) family was not currently receiving other mental health or bereavement services, (4) family was willing to participate in either study condition, (5) caregivers and youth were able to complete the assessment in English, (6) youth did not have an intellectual disorder, and (7) family planned to stay in the area for the next 6 months. All youth in families who met the eligibility criteria were invited to participate. Families were excluded and referred for treatment if any participant in the family indicated suicidality (i.e., intent or a plan), if the caregiver met diagnostic criteria for major depression, or if the youth met diagnostic criteria for conduct disorder, oppositional defiant disorder, or attention-deficit/hyperactive disorder that was not treated by medication. These exclusions were due to concerns that youth behavior problems associated with these diagnoses may interfere with intervention delivery and fidelity of the efficacy trial as well as group cohesion.
At pretest, youth were between the ages of 8 and 16 years (M = 11.39, SD = 2.43) and 54% (n = 131) were male (see Sandler et al., 2010 for a table of baseline characteristics for each group). Of the caregivers, 63% were mothers, 21% were fathers, and 16% were nonparental family members or friends. The racial and ethnic composition of the sample was 67% non-Hispanic White, 16% Hispanic, 7% Black, 3% Native American, 1% Asian or Pacific Islander; 6% identified as “Other.” Parental death had occurred an average of 10.81 months (SD = 6.35) before program entry. The cause of death was 74% illness, 15% accident, and 11% homicide or suicide. Median family income was between $30,000 and $35,000; 15.9% were below the poverty line according to United States, Health and Human Services poverty guidelines for 1996. As reported in a prior study (Sandler et al., 2003), there was one significant-only baseline difference between the study conditions. The percentage of non-Hispanic White participants was lower in the intervention group than in the control group (64% vs. 72%). See Table I for a description of the sample characteristics.
| . | Youth . | Caregiver . | ||
|---|---|---|---|---|
| Characteristic . | LC . | FBP . | LC . | FBP . |
| Age, M (SD), years | 11.32 (2.22) | 11.45 (2.58) | 42.16 (7.32) | 42.01 (9.09) |
| Race/ethnicity, n (%) | ||||
| White, non-Hispanic | 78 (71.56) | 87 (64.44) | 49 (74.24) | 59 (65.56) |
| Hispanic | 11 (10.09) | 26 (19.26) | 7 (10.61) | 11 (12.22) |
| Black | 7 (6.42) | 8 (5.93) | 3 (4.55) | 8 (8.89) |
| Asian American/Pacific Islander | 0 | 3 (2.22) | 0 | 2 (2.22) |
| Native American | 8 (7.34) | 2 (1.48) | 3 (4.55) | 2 (2.22) |
| Other | 5 (4.59) | 9 (6.67) | 1 (1.52) | 1 (1.11) |
| Missing | 0 | 0 | 3 (4.55) | 7 (7.78) |
| Gender, n (%) | ||||
| Male | 57 (52.29) | 73 (54.07) | 18 (27.27) | 15 (16.67) |
| Female | 52 (47.71) | 62 (45.93) | 48 (72.72) | 75 (83.33) |
| Cause of death, n (%) | ||||
| Illness | 48 (73.85) | 65 (73.07) | – | – |
| Violent | 17 (26.15) | 24 (26.96) | – | – |
| Time since death, M (SD), months | 9.61 (5.25) | 10.57 (6.33) | – | – |
| . | Youth . | Caregiver . | ||
|---|---|---|---|---|
| Characteristic . | LC . | FBP . | LC . | FBP . |
| Age, M (SD), years | 11.32 (2.22) | 11.45 (2.58) | 42.16 (7.32) | 42.01 (9.09) |
| Race/ethnicity, n (%) | ||||
| White, non-Hispanic | 78 (71.56) | 87 (64.44) | 49 (74.24) | 59 (65.56) |
| Hispanic | 11 (10.09) | 26 (19.26) | 7 (10.61) | 11 (12.22) |
| Black | 7 (6.42) | 8 (5.93) | 3 (4.55) | 8 (8.89) |
| Asian American/Pacific Islander | 0 | 3 (2.22) | 0 | 2 (2.22) |
| Native American | 8 (7.34) | 2 (1.48) | 3 (4.55) | 2 (2.22) |
| Other | 5 (4.59) | 9 (6.67) | 1 (1.52) | 1 (1.11) |
| Missing | 0 | 0 | 3 (4.55) | 7 (7.78) |
| Gender, n (%) | ||||
| Male | 57 (52.29) | 73 (54.07) | 18 (27.27) | 15 (16.67) |
| Female | 52 (47.71) | 62 (45.93) | 48 (72.72) | 75 (83.33) |
| Cause of death, n (%) | ||||
| Illness | 48 (73.85) | 65 (73.07) | – | – |
| Violent | 17 (26.15) | 24 (26.96) | – | – |
| Time since death, M (SD), months | 9.61 (5.25) | 10.57 (6.33) | – | – |
Note. FBP = family bereavement program; LC = literature control.
| . | Youth . | Caregiver . | ||
|---|---|---|---|---|
| Characteristic . | LC . | FBP . | LC . | FBP . |
| Age, M (SD), years | 11.32 (2.22) | 11.45 (2.58) | 42.16 (7.32) | 42.01 (9.09) |
| Race/ethnicity, n (%) | ||||
| White, non-Hispanic | 78 (71.56) | 87 (64.44) | 49 (74.24) | 59 (65.56) |
| Hispanic | 11 (10.09) | 26 (19.26) | 7 (10.61) | 11 (12.22) |
| Black | 7 (6.42) | 8 (5.93) | 3 (4.55) | 8 (8.89) |
| Asian American/Pacific Islander | 0 | 3 (2.22) | 0 | 2 (2.22) |
| Native American | 8 (7.34) | 2 (1.48) | 3 (4.55) | 2 (2.22) |
| Other | 5 (4.59) | 9 (6.67) | 1 (1.52) | 1 (1.11) |
| Missing | 0 | 0 | 3 (4.55) | 7 (7.78) |
| Gender, n (%) | ||||
| Male | 57 (52.29) | 73 (54.07) | 18 (27.27) | 15 (16.67) |
| Female | 52 (47.71) | 62 (45.93) | 48 (72.72) | 75 (83.33) |
| Cause of death, n (%) | ||||
| Illness | 48 (73.85) | 65 (73.07) | – | – |
| Violent | 17 (26.15) | 24 (26.96) | – | – |
| Time since death, M (SD), months | 9.61 (5.25) | 10.57 (6.33) | – | – |
| . | Youth . | Caregiver . | ||
|---|---|---|---|---|
| Characteristic . | LC . | FBP . | LC . | FBP . |
| Age, M (SD), years | 11.32 (2.22) | 11.45 (2.58) | 42.16 (7.32) | 42.01 (9.09) |
| Race/ethnicity, n (%) | ||||
| White, non-Hispanic | 78 (71.56) | 87 (64.44) | 49 (74.24) | 59 (65.56) |
| Hispanic | 11 (10.09) | 26 (19.26) | 7 (10.61) | 11 (12.22) |
| Black | 7 (6.42) | 8 (5.93) | 3 (4.55) | 8 (8.89) |
| Asian American/Pacific Islander | 0 | 3 (2.22) | 0 | 2 (2.22) |
| Native American | 8 (7.34) | 2 (1.48) | 3 (4.55) | 2 (2.22) |
| Other | 5 (4.59) | 9 (6.67) | 1 (1.52) | 1 (1.11) |
| Missing | 0 | 0 | 3 (4.55) | 7 (7.78) |
| Gender, n (%) | ||||
| Male | 57 (52.29) | 73 (54.07) | 18 (27.27) | 15 (16.67) |
| Female | 52 (47.71) | 62 (45.93) | 48 (72.72) | 75 (83.33) |
| Cause of death, n (%) | ||||
| Illness | 48 (73.85) | 65 (73.07) | – | – |
| Violent | 17 (26.15) | 24 (26.96) | – | – |
| Time since death, M (SD), months | 9.61 (5.25) | 10.57 (6.33) | – | – |
Note. FBP = family bereavement program; LC = literature control.
Procedure
Interviews were conducted on four occasions: T1: pretest, T2: posttest (3 months after the pretest; completion rate: 98% FBP vs. 95% LC), T3: 11-month follow-up (completion rate: 87% FBP vs. 91% LC), T4: 6-year follow-up (completion rate: 87% FBP vs. 94% LC). Verbal interviews were conducted in the families’ homes, with caregivers and children interviewed individually by trained interviewers who read each assessment item aloud to avoid introducing bias due to reading level. At T1–T4, caregivers provided informed consent, and youth provided informed assent. At T4, caregivers and youth who were over 18 years old provided informed consent. Caregivers and youth were interviewed separately by trained staff masked to study conditions. For T1–T3, families were paid $40 for interviews involving one youth and an additional $30 for each additional youth. At T4, families were paid $200 as this assessment was more time intensive. The university’s Institutional Review Board approved all study procedures. Study-related adverse events were monitored throughout the trial, and none occurred.
Following the pretest, families were randomized to the FBP (n = 90 families, 135 youth) or the literature control (LC; n = 66 families, 109 youth). Trained study staff used computer-generated random assignment to study conditions in a 55% (FBP) versus 45% (LC) ratio. Random assignment occurred at the family level.
Families in the FBP participated in twelve 2-hr sessions of their respective caregiver, child, or adolescent groups, as well as two family sessions to tailor the program to each family. Four of the 12 scheduled sessions had a conjoint segment with youth and parents. Youth ages 8–11 years were in the child group, and 13–16 years were in the adolescent group; 80% of the 12-year-olds were randomly assigned to the adolescent groups and 20% to the child groups to balance group enrollment numbers (Sandler et al., 2003). The groups targeted both child-level (e.g., coping, self-esteem, adaptive control beliefs, emotion expression) and family-level (e.g., positive parenting, consistent discipline, stressful life events, parent distress, and mental health problems) processes that were theoretically or empirically linked to the development of mental health problems in bereaved youth. Group members learned through in-session video demonstrations, role-play practice and feedback, and home practice exercises. The program was developed using strategies designed to enhance engagement and included home practice of program skills. Engagement was assessed in several ways, including attendance, home practice completion, and home practice fidelity (see Schoenfelder et al., 2013 for more details). For example, caregivers attended 86% of program sessions and children attended 88% of sessions. See Ayers et al. (2013) for a detailed description of the FBP.
Groups were facilitated by two master’s-level (or equivalent experience) clinicians who underwent a comprehensive 40-hr training program prior to initiating the groups. The training included didactic presentations, analysis of previously recorded program sessions, and role-play exercises. Group facilitators participated in weekly 2-hr training sessions, during which they completed quizzes on the session's content. Following each group session, a 1.5-hr supervision session was held to discuss implementation challenges and strategies for tailoring the program to accommodate the unique needs of group members. Implementation fidelity was assessed by impartial, reliable coders who examined session recordings and evaluated the execution of each action item outlined in the program manual. Based on the independent coding of these session videos (Κ = 0.68 between coders), group facilitators carried out 89% of the prescribed actions in the caregiver program manual and 84% of the actions in the child program manual.
In the LC, each participating caregiver, child, and adolescent received their own age-appropriate grief-related book once per month for 3 months. Each book was accompanied by a reading guide that emphasized the main concepts. Regarding adherence, 42.37% of caregivers, 70.91% of children, and 38.46% of adolescents reported that they read at least half of the books.
Measures
See Table II for a list of all measures. Note that reliability statistics are provided for pretest measures only; reliability was consistent across waves.
| Construct . | Measures . | Assessments . | |||
|---|---|---|---|---|---|
| pre . | post . | 11 months . | 6years . | ||
| Positive parentinga | Child Report of Parental Behavior Inventory [acceptance, rejection] | ✓ | ✓ | ||
| Dyadic Routines | ✓ | ✓ | |||
| Stable Positive Events | ✓ | ✓ | |||
| Sharing of Feelings | ✓ | ✓ | |||
| Caregiver Expression of Emotion Questionnaire | ✓ | ✓ | |||
| Child Report of Parental Behavior Inventory [inconsistent discipline] | ✓ | ✓ | |||
| Parent Perception Inventory [positive reinforcement] | ✓ | ✓ | |||
| Oregon Discipline Scale [follow-through] | ✓ | ✓ | |||
| Adaptive copingb | Children's Coping Strategies Checklist [active coping] | ✓ | ✓ | ||
| Coping Efficacy Scale | ✓ | ✓ | |||
| Stressful eventsc | General Life Events Schedule for Children; Parent Death Events List | ✓ | ✓ | ||
| Fear of abandonmentd | Children’s Beliefs about Parental Bereavement Scale [fear of abandonment] | ✓ | ✓ | ||
| Child internalizing problemse,f | Children’s Depression Inventory; Children's Manifest Anxiety Scale–Revised | ✓ | |||
| Youth Self-Report/Young Adult Self-Report | ✓ | ||||
| Child Behavior Checklist/Young Adult Behavior Checklist | ✓ | ✓ | |||
| Teacher Report Form | ✓ | ✓ | |||
| Child externalizing problemse,f | Youth Self-Report/Young Adult Self-Report | ✓ | ✓ | ||
| Child Behavior Checklist/Young Adult Behavior Checklist | ✓ | ✓ | |||
| Teacher Report Form | ✓ | ✓ | |||
| Child griefg | Texas Revised Inventory of Grief [present feeling] | ✓ | ✓ | ||
| Intrusive Grief Thoughts Scale | ✓ | ✓ | |||
| Adapted Inventory of Traumatic Grief | ✓ | ||||
| Construct . | Measures . | Assessments . | |||
|---|---|---|---|---|---|
| pre . | post . | 11 months . | 6years . | ||
| Positive parentinga | Child Report of Parental Behavior Inventory [acceptance, rejection] | ✓ | ✓ | ||
| Dyadic Routines | ✓ | ✓ | |||
| Stable Positive Events | ✓ | ✓ | |||
| Sharing of Feelings | ✓ | ✓ | |||
| Caregiver Expression of Emotion Questionnaire | ✓ | ✓ | |||
| Child Report of Parental Behavior Inventory [inconsistent discipline] | ✓ | ✓ | |||
| Parent Perception Inventory [positive reinforcement] | ✓ | ✓ | |||
| Oregon Discipline Scale [follow-through] | ✓ | ✓ | |||
| Adaptive copingb | Children's Coping Strategies Checklist [active coping] | ✓ | ✓ | ||
| Coping Efficacy Scale | ✓ | ✓ | |||
| Stressful eventsc | General Life Events Schedule for Children; Parent Death Events List | ✓ | ✓ | ||
| Fear of abandonmentd | Children’s Beliefs about Parental Bereavement Scale [fear of abandonment] | ✓ | ✓ | ||
| Child internalizing problemse,f | Children’s Depression Inventory; Children's Manifest Anxiety Scale–Revised | ✓ | |||
| Youth Self-Report/Young Adult Self-Report | ✓ | ||||
| Child Behavior Checklist/Young Adult Behavior Checklist | ✓ | ✓ | |||
| Teacher Report Form | ✓ | ✓ | |||
| Child externalizing problemse,f | Youth Self-Report/Young Adult Self-Report | ✓ | ✓ | ||
| Child Behavior Checklist/Young Adult Behavior Checklist | ✓ | ✓ | |||
| Teacher Report Form | ✓ | ✓ | |||
| Child griefg | Texas Revised Inventory of Grief [present feeling] | ✓ | ✓ | ||
| Intrusive Grief Thoughts Scale | ✓ | ✓ | |||
| Adapted Inventory of Traumatic Grief | ✓ | ||||
Scores on positive parenting were represented by a latent factor of standardized scores from a second-order factor model of positive caregiver–child relationship and discipline (χ2 [72, N = 239] = 145.69, CFI = 0.94, RMSEA = 0.06; Sandler et al., 2003).
Scores on adaptive coping were a mean composite score of the two correlated (r = 0.53) coping scales.
The stressful events measure was a count variable representing the number of stressful events experienced.
Fear of abandonment was a mean scale score.
At pretest, scores on child report of internalizing problems were a mean composite score (weighted α = 0.93) of the correlated (r = 0.65) Children’s Depression Inventory and Children's Manifest Anxiety Scale–Revised. Scores on caregiver- and teacher-report of internalizing problems were T scores.
At 6-year follow-up, scores on child and caregiver report of internalizing problems were computed from developmentally appropriate versions (youth vs. young adult) of the Achenbach scales (i.e., YSR, YASR). Scores were standardized based on an equating transformation that used item response theory to put the scale scores on a common metric (Kolen & Brennan, 1995) (see Sandler et al., 2010 for details).
At pretest, grief scores were mean scale scores from the Texas Revised Inventory of Grief and the Intrusive Grief Thoughts Scale. At 6-year follow-up, a bifactor measurement model identified specific factors of grief based on the three measures of grief (i.e., TRIG, IGTS, ITG; r = 0.44–0.64). As reported in Sandler et al., 2021, three specific dimensions of grief were identified: Social Detachment/Insecurity, Intrusive Grief Thoughts, Continuing Affective Reaction, and a General Grief dimension. The specific factors are uncorrelated with the general factor. We used scale scores and the bifactor model-derived general and specific factor scores.
| Construct . | Measures . | Assessments . | |||
|---|---|---|---|---|---|
| pre . | post . | 11 months . | 6years . | ||
| Positive parentinga | Child Report of Parental Behavior Inventory [acceptance, rejection] | ✓ | ✓ | ||
| Dyadic Routines | ✓ | ✓ | |||
| Stable Positive Events | ✓ | ✓ | |||
| Sharing of Feelings | ✓ | ✓ | |||
| Caregiver Expression of Emotion Questionnaire | ✓ | ✓ | |||
| Child Report of Parental Behavior Inventory [inconsistent discipline] | ✓ | ✓ | |||
| Parent Perception Inventory [positive reinforcement] | ✓ | ✓ | |||
| Oregon Discipline Scale [follow-through] | ✓ | ✓ | |||
| Adaptive copingb | Children's Coping Strategies Checklist [active coping] | ✓ | ✓ | ||
| Coping Efficacy Scale | ✓ | ✓ | |||
| Stressful eventsc | General Life Events Schedule for Children; Parent Death Events List | ✓ | ✓ | ||
| Fear of abandonmentd | Children’s Beliefs about Parental Bereavement Scale [fear of abandonment] | ✓ | ✓ | ||
| Child internalizing problemse,f | Children’s Depression Inventory; Children's Manifest Anxiety Scale–Revised | ✓ | |||
| Youth Self-Report/Young Adult Self-Report | ✓ | ||||
| Child Behavior Checklist/Young Adult Behavior Checklist | ✓ | ✓ | |||
| Teacher Report Form | ✓ | ✓ | |||
| Child externalizing problemse,f | Youth Self-Report/Young Adult Self-Report | ✓ | ✓ | ||
| Child Behavior Checklist/Young Adult Behavior Checklist | ✓ | ✓ | |||
| Teacher Report Form | ✓ | ✓ | |||
| Child griefg | Texas Revised Inventory of Grief [present feeling] | ✓ | ✓ | ||
| Intrusive Grief Thoughts Scale | ✓ | ✓ | |||
| Adapted Inventory of Traumatic Grief | ✓ | ||||
| Construct . | Measures . | Assessments . | |||
|---|---|---|---|---|---|
| pre . | post . | 11 months . | 6years . | ||
| Positive parentinga | Child Report of Parental Behavior Inventory [acceptance, rejection] | ✓ | ✓ | ||
| Dyadic Routines | ✓ | ✓ | |||
| Stable Positive Events | ✓ | ✓ | |||
| Sharing of Feelings | ✓ | ✓ | |||
| Caregiver Expression of Emotion Questionnaire | ✓ | ✓ | |||
| Child Report of Parental Behavior Inventory [inconsistent discipline] | ✓ | ✓ | |||
| Parent Perception Inventory [positive reinforcement] | ✓ | ✓ | |||
| Oregon Discipline Scale [follow-through] | ✓ | ✓ | |||
| Adaptive copingb | Children's Coping Strategies Checklist [active coping] | ✓ | ✓ | ||
| Coping Efficacy Scale | ✓ | ✓ | |||
| Stressful eventsc | General Life Events Schedule for Children; Parent Death Events List | ✓ | ✓ | ||
| Fear of abandonmentd | Children’s Beliefs about Parental Bereavement Scale [fear of abandonment] | ✓ | ✓ | ||
| Child internalizing problemse,f | Children’s Depression Inventory; Children's Manifest Anxiety Scale–Revised | ✓ | |||
| Youth Self-Report/Young Adult Self-Report | ✓ | ||||
| Child Behavior Checklist/Young Adult Behavior Checklist | ✓ | ✓ | |||
| Teacher Report Form | ✓ | ✓ | |||
| Child externalizing problemse,f | Youth Self-Report/Young Adult Self-Report | ✓ | ✓ | ||
| Child Behavior Checklist/Young Adult Behavior Checklist | ✓ | ✓ | |||
| Teacher Report Form | ✓ | ✓ | |||
| Child griefg | Texas Revised Inventory of Grief [present feeling] | ✓ | ✓ | ||
| Intrusive Grief Thoughts Scale | ✓ | ✓ | |||
| Adapted Inventory of Traumatic Grief | ✓ | ||||
Scores on positive parenting were represented by a latent factor of standardized scores from a second-order factor model of positive caregiver–child relationship and discipline (χ2 [72, N = 239] = 145.69, CFI = 0.94, RMSEA = 0.06; Sandler et al., 2003).
Scores on adaptive coping were a mean composite score of the two correlated (r = 0.53) coping scales.
The stressful events measure was a count variable representing the number of stressful events experienced.
Fear of abandonment was a mean scale score.
At pretest, scores on child report of internalizing problems were a mean composite score (weighted α = 0.93) of the correlated (r = 0.65) Children’s Depression Inventory and Children's Manifest Anxiety Scale–Revised. Scores on caregiver- and teacher-report of internalizing problems were T scores.
At 6-year follow-up, scores on child and caregiver report of internalizing problems were computed from developmentally appropriate versions (youth vs. young adult) of the Achenbach scales (i.e., YSR, YASR). Scores were standardized based on an equating transformation that used item response theory to put the scale scores on a common metric (Kolen & Brennan, 1995) (see Sandler et al., 2010 for details).
At pretest, grief scores were mean scale scores from the Texas Revised Inventory of Grief and the Intrusive Grief Thoughts Scale. At 6-year follow-up, a bifactor measurement model identified specific factors of grief based on the three measures of grief (i.e., TRIG, IGTS, ITG; r = 0.44–0.64). As reported in Sandler et al., 2021, three specific dimensions of grief were identified: Social Detachment/Insecurity, Intrusive Grief Thoughts, Continuing Affective Reaction, and a General Grief dimension. The specific factors are uncorrelated with the general factor. We used scale scores and the bifactor model-derived general and specific factor scores.
Positive Parenting (Combined Youth/Caregiver Report)
At pretest and posttest, youth and caregivers’ perception of positive parenting was assessed by several scales. Youth and caregivers completed the Child Report of Parental Behavior Inventory (Schaefer, 1965) Acceptance (16 items, e.g., “Your caregiver enjoyed doing things with you,” αyouth = 0.92, αcaregiver = 0.91), Rejection (16 items, e.g., “Your caregiver said you are a big problem,” αyouth = 0.87, αcaregiver = 0.87), and Inconsistent Discipline (8 items, e.g., “Your caregiver frequently changed the rules you were supposed to follow,” αyouth = 0.80, αcaregiver = 0.86) subscales. Youth and caregivers completed the Dyadic Routines Scale (Wolchik et al., 2000; 7 items, e.g., “Your caregiver had some time each day for just talking to you,” αyouth = 0.74, αcaregiver = 0.76). Youth and caregivers completed the Stable Positive Events Scale (Sandler et al., 1991; 5 items, e.g., “Household routines got done smoothly,” reliability not calculated because items measure discrete events). Youth and caregivers completed an adapted version of the Parent Perception Inventory (Hazzard et al., 1983; 8 items, e.g., “How often does your caregiver thank you for doing things?,” αyouth = 0.91, αcaregiver = 0.92). Youth only completed the Sharing of Feelings Scale (Ayers et al., 1998; 10 items, e.g., “Your [caregiver] understands your feelings,” αyouth = 0.85). Caregivers only completed the Talk with Reassurance subscale from the Caregiver Expression of Emotion Questionnaire (Jones & Twohey, 1998; 6 items; e.g., “Reassure child that you are dealing with your sadness,” αcaregiver = 0.74) and an adapted version of the Oregon Discipline Scale Discipline Follow-Through subscale (Oregon Social Learning Center, 1991; 6 items; e.g., “How often was the child able to get around the rules you set?”, αcaregiver = 0.82). Scores reflecting higher levels of positive parenting are associated with reduced mental health problems in youth who experienced bereavement and discriminate between clinical and non-clinical samples (Ayers et al., 1998; Cohen et al., 2000; Hazzard et al., 1983; Sandler et al., 1991; West et al., 1991).
Adaptive Coping (Youth Report)
At pretest and posttest, youth completed the Children’s Coping Strategies Checklist active coping subscale (e.g., “You did something to solve the problem,” α = 0.90) and the Coping Efficacy Scale (Sandler et al., 2000; 7 items, e.g., “In the future, how good do you think you will be in handling your problems?,” α = 0.72). Scores on these measures are associated with lower youth mental health problems (Ayers et al., 1996; Sandler et al., 1994, 2000).
Stressful Events (Youth Report)
At pretest and posttest, youth completed two life events measures. Youth reported the past-month occurrence of 51 stressful events from the General Life Events Schedule for Children (Sandler et al., 1986; e.g., “Your caregiver talked about having serious money troubles.”) and the Parent Death Events List (Sandler et al., 1992; e.g., “You had a serious disagreement or verbal fight with your [parent/guardian].”). Scores on these measures are associated with higher mental health problems in parentally bereaved youth (Haine et al., 2006). Reliability was not calculated because these scales measure discrete events.
Fear of Abandonment (Youth Report)
At pretest and 11-month follow-up, youth completed an adapted version of Fear of Abandonment subscale from the Children’s Beliefs about Parental Divorce Scale (Kurdek & Berg, 1987; 7 items, e.g., “How much do you worry that you may be left all alone?”, α = 0.78). Wolchik et al. (2006, 2008) established that the 7 items fit a one-dimensional model adequately: χ2 (20) = 48.53, comparative fit index [CFI] = 0.94, root mean square error of approximation [RMSEA] = 0.06). Scores are associated with mental health problems (Wolchik et al., 2002, 2006).
Youth Mental Health Problems (Youth, Caregiver, and Teacher Report)
At pretest, youth completed the Children’s Depression Inventory (CDI; Kovacs, 1981; 27 items, e.g., “I am sad all the time,” α = 0.87), the Children’s Manifest Anxiety Scale–Revised (RCMAS; Reynolds & Richmond, 1978; 28 items, e.g., “You were afraid of a lot of things,” α = 0.86). Because some were over the age of 18 years at the 6-year follow-up, developmentally appropriate scales (youth vs. young adult versions) of the Achenbach scales (i.e., YSR, YASR) were used to assess internalizing and externalizing problems. The CDI, RCMAS, YSR, and YASR show strong correlations with established measures of youth mental health problems and adequate validity (Achenbach et al., 2017; Kovacs, 1985; Reynolds & Paget, 1981).
Caregivers completed the appropriate form of the Child Behavior Checklist or Young Adult Behavior Checklist internalizing (CBCL/YABCL [for youth 18 and over]; Achenbach, 1991; 31 items, e.g., “Cries a lot,” α = 0.87). and externalizing (33 items, e.g., “Gets in many fights,” α = 0.90) subscales. The CBCL and YABCL strongly correlate with established measures of mental health problems and have adequate validity (Achenbach et al., 2017).
At pretest and 6-year follow-up, teachers completed the Teacher Report Form (TRF) internalizing (Achenbach, 1991; 34 items, e.g., “Shy or timid,” α = 0.87). and externalizing (34 items, e.g., “Argues a lot,” α = 0.92) subscales. At the 6-year follow-up, teacher-report data were collected only for youth currently in junior high or high school (n = 117). The TRF shows strong correlations with established measures of mental health problems and has adequate validity (Achenbach et al., 2017).
Maladaptive Grief (Youth Report)
At pretest and 6-year follow-up, youth completed an adapted version of the Texas Revised Inventory of Grief (TRIG; Faschingbauer, 1981) Present Feeling subscale (11 items, e.g., “I am unable to accept the death of my [deceased relation],” α = 0.89–0.92) and the Intrusive Grief Thoughts Scale (IGTS; Program for Prevention Research, 1999; 9 items, e.g., “I think about the death when I don’t want to,” α = 0.88–0.93). At the 6-year follow-up, youth also completed the Adapted Inventory of Traumatic Grief (ITG; Prigerson & Jacobs, 2001; 26 items, e.g., “To what extent do you feel that life is empty or meaningless without your [deceased parent]?”). The grief measures predicted bereaved youth mental health problems.
Covariates
We included youth age, youth gender, time since death, and cause of death as covariates. In the mediation models, we controlled for the respective baseline covariate for each dependent variable, including positive parenting, adaptive coping, stressful events at posttest, fear of abandonment at the 11-month follow-up, youth internalizing problems, externalizing problems, and maladaptive grief at the 6-year follow-up.
Data Analysis Approach
We used Mplus Version 8.5 (Muthén & Muthén, 1998–2017) for all analyses. Models were estimated using maximum likelihood robust standard error correction estimator for unbiased estimates (i.e., MLR; Yuan & Bentler, 2000), and missing data were handled with the Full information maximum likelihood method. We used the sandwich estimator (i.e., command TYPE = COMPLEX) to account for clustering effects (i.e., youth nested within families. We did not account for group session clustering due to low ICCs [0.005 for youth self-report; 0.002 for parent report]). In all models, exogenous variables were allowed to covary.
Following our preregistered secondary data analytic plan (available at https://osf.io/9vg46; data available on request), we first tested a four-wave prospective mediation model in which (1) the FBP predicted posttest greater positive parenting, higher adaptive coping, and reduced stressful events. In turn, (2) greater posttest positive parenting, higher adaptive coping, and reduced stressful events predicted lower fear of abandonment at the 11-month follow-up, and in turn, (3) higher fear of abandonment at the 11-month follow-up predicted greater internalizing problems, externalizing problems, and maladaptive grief at the 6-year follow-up. Baseline covariates were included to rule out stability effects. We fitted separate models for youth, parent, and teacher reports of internalizing and externalizing problems and for youth report of grief. Teacher-report models were tested using the subsample of 117 youth who had teacher-report data at the 6-year follow-up. We estimated asymmetric confidence intervals (CIs) in Mplus to assess the significance of the indirect effects of two-link mediation models. Due to the complexity,1 we evaluated the significance of the indirect effects using the joint significance test (i.e., each link along the mediation pathway is significant; MacKinnon et al., 2012) for three-link mediation models. We conducted power analysis for estimating mediation effects. For our mediation models with the observed variables (i.e., path analysis), we were interested in power to detect individual and sets of regression parameters (Satorra & Saris, 1985). Taking the individual nested in family cluster effect into account, we had power (≥0.80) to detect small effects of (standardized) β ≥ 0.17 for linear regression coefficients based on Mplus simulation (Muthén and Muthén, 2002) and two-path (β1 β2) mediation pathways that are ≥0.04 (see Fritz & MacKinnon, 2007).
We also re-tested our mediation model to include tests of moderation by youth gender and age (children: 8–11 years [n = 132] and adolescents: 12–16 years [n = 112]) using a multiple-group procedure. Specifically, we tested youth gender and age as a moderator of the paths: (1) FBP-induced change in positive parenting, adaptive coping, and stressful events at posttest to fear of abandonment at the 11-month follow-up and (2) fear of abandonment at the 11-month follow-up to mental health and grief outcomes at the 6-year follow-up (for moderation by age, we excluded teacher reports because many members of the adolescent group did not have teacher report at the 6-year follow-up). Moderation by gender was expected based on observed gender effects in prior studies showing higher prevalence of internalizing problems and fear of abandonment in bereaved girls (Little et al., 2009; Sandler et al., 2003; Schmiege et al., 2006; Worden & Silverman, 1996). Moderation by age was expected based on fear of abandonment being a more salient threat among younger youth in prior studies of parental bereavement and divorce (O’Hara et al., 2021; Wolchik et al., 2006, 2008).
Results
Preliminary Analyses
See Table III for correlations of key study variables. Positive parenting and stressful events at posttest were related, negatively and positively, respectively, with fear of abandonment at the 11-month follow-up. Positive parenting was negatively associated with youth- and parent-reported internalizing and externalizing problems at the 6-year follow-up. Stressful events were positively related to youth-reported internalizing and externalizing problems and maladaptive grief at the 6-year follow-up. Adaptive coping was not associated with fear of abandonment at the 11-month follow-up, nor mental health problems or grief at the 6-year follow-up. Fear of abandonment at the 11-month follow-up was positively related to youth-reported internalizing problems and maladaptive grief at the 6-year follow-up.
| . | 1 . | 2 . | 3 . | 4 . | 5 . | 6 . | 7 . | 8 . | 9 . | 10 . | 11 . |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Child age | 1 | ||||||||||
| 2. Positive parenting [W2] | −0.08 | 1 | |||||||||
| 3. Stressful events [W2] | −0.07 | −0.35 | 1 | ||||||||
| 4. Adaptive coping [W2] | −0.04 | 0.30 | −0.05 | 1 | |||||||
| 5. Fear of abandonment [W3] | −0.19 | −0.22 | 0.28 | −0.03 | 1 | ||||||
| 6. Internalizing problems [W1]—youth | −0.10 | −0.38 | 0.48 | −0.16 | 0.39 | 1 | |||||
| 7. Externalizing problems [W1]—youth | 0.08 | −0.31 | 0.40 | −0.17 | 0.18 | 0.55 | 1 | ||||
| 8. Internalizing problems [W1]—parent | −0.04 | −0.25 | 0.10 | −0.11 | 0.05 | 0.27 | 0.09 | 1 | |||
| 9. Externalizing problems [W1]—parent | −0.01 | −0.36 | 0.13 | −0.09 | 0.07 | 0.16 | 0.21 | 0.58 | 1 | ||
| 10. Internalizing problems [W1]—teacher | −0.07 | 0.02 | 0.05 | 0.00 | 0.01 | 0.22 | 0.08 | 0.22 | 0.12 | 1 | |
| 11. Externalizing problems [W1]—teacher | 0.00 | −0.11 | 0.08 | 0.00 | −0.01 | 0.13 | 0.14 | 0.08 | 0.24 | 0.41 | 1 |
| 12. Internalizing problems [W4]—youth | −0.09 | −0.17 | 0.15 | −0.10 | 0.15 | 0.29 | 0.17 | 0.21 | 0.15 | 0.12 | 0.15 |
| 13. Externalizing problems [W4]—youth | −0.15 | −0.24 | 0.20 | −0.12 | 0.11 | 0.23 | 0.31 | 0.24 | 0.34 | 0.02 | 0.16 |
| 14. Internalizing problems [W4]—parent | −0.14 | −0.16 | 0.10 | −0.10 | 0.02 | 0.23 | 0.14 | 0.51 | 0.31 | 0.26 | 0.15 |
| 15. Externalizing problems [W4]—parent | −0.28 | −0.25 | 0.13 | −0.07 | 0.05 | 0.19 | 0.20 | 0.37 | 0.55 | 0.23 | 0.24 |
| 16. Internalizing problems [W4]—teacher | −0.03 | −0.22 | 0.10 | −0.10 | 0.00 | 0.15 | 0.20 | 0.23 | 0.37 | 0.27 | 0.37 |
| 17. Externalizing problems [W4]—teacher | −0.11 | −0.22 | 0.18 | −0.06 | 0.07 | 0.14 | 0.21 | 0.23 | 0.45 | 0.16 | 0.38 |
| 18. Intrusive Grief Thoughts Scale [W1] | −0.19 | −0.25 | 0.32 | 0.07 | 0.39 | 0.61 | 0.28 | 0.26 | 0.15 | 0.14 | 0.08 |
| 19. Texas Revised Inventory of Grief [W1] | −0.10 | −0.22 | 0.22 | 0.00 | 0.27 | 0.48 | 0.20 | 0.24 | 0.21 | 0.19 | 0.16 |
| 20. Intrusive Grief Thoughts Scale [W4] | −0.16 | −0.04 | 0.21 | 0.11 | 0.24 | 0.17 | 0.05 | 0.10 | 0.05 | 0.11 | 0.09 |
| 21. Texas Revised Inventory of Grief [W4] | −0.04 | −0.05 | 0.14 | 0.12 | 0.15 | 0.23 | −0.01 | 0.12 | 0.04 | 0.06 | 0.03 |
| 22. Adapted Inventory of Traumatic Grief [W4] | −0.07 | −0.11 | 0.19 | 0.07 | 0.25 | 0.27 | 0.12 | 0.20 | 0.13 | 0.05 | 0.05 |
| . | 1 . | 2 . | 3 . | 4 . | 5 . | 6 . | 7 . | 8 . | 9 . | 10 . | 11 . |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Child age | 1 | ||||||||||
| 2. Positive parenting [W2] | −0.08 | 1 | |||||||||
| 3. Stressful events [W2] | −0.07 | −0.35 | 1 | ||||||||
| 4. Adaptive coping [W2] | −0.04 | 0.30 | −0.05 | 1 | |||||||
| 5. Fear of abandonment [W3] | −0.19 | −0.22 | 0.28 | −0.03 | 1 | ||||||
| 6. Internalizing problems [W1]—youth | −0.10 | −0.38 | 0.48 | −0.16 | 0.39 | 1 | |||||
| 7. Externalizing problems [W1]—youth | 0.08 | −0.31 | 0.40 | −0.17 | 0.18 | 0.55 | 1 | ||||
| 8. Internalizing problems [W1]—parent | −0.04 | −0.25 | 0.10 | −0.11 | 0.05 | 0.27 | 0.09 | 1 | |||
| 9. Externalizing problems [W1]—parent | −0.01 | −0.36 | 0.13 | −0.09 | 0.07 | 0.16 | 0.21 | 0.58 | 1 | ||
| 10. Internalizing problems [W1]—teacher | −0.07 | 0.02 | 0.05 | 0.00 | 0.01 | 0.22 | 0.08 | 0.22 | 0.12 | 1 | |
| 11. Externalizing problems [W1]—teacher | 0.00 | −0.11 | 0.08 | 0.00 | −0.01 | 0.13 | 0.14 | 0.08 | 0.24 | 0.41 | 1 |
| 12. Internalizing problems [W4]—youth | −0.09 | −0.17 | 0.15 | −0.10 | 0.15 | 0.29 | 0.17 | 0.21 | 0.15 | 0.12 | 0.15 |
| 13. Externalizing problems [W4]—youth | −0.15 | −0.24 | 0.20 | −0.12 | 0.11 | 0.23 | 0.31 | 0.24 | 0.34 | 0.02 | 0.16 |
| 14. Internalizing problems [W4]—parent | −0.14 | −0.16 | 0.10 | −0.10 | 0.02 | 0.23 | 0.14 | 0.51 | 0.31 | 0.26 | 0.15 |
| 15. Externalizing problems [W4]—parent | −0.28 | −0.25 | 0.13 | −0.07 | 0.05 | 0.19 | 0.20 | 0.37 | 0.55 | 0.23 | 0.24 |
| 16. Internalizing problems [W4]—teacher | −0.03 | −0.22 | 0.10 | −0.10 | 0.00 | 0.15 | 0.20 | 0.23 | 0.37 | 0.27 | 0.37 |
| 17. Externalizing problems [W4]—teacher | −0.11 | −0.22 | 0.18 | −0.06 | 0.07 | 0.14 | 0.21 | 0.23 | 0.45 | 0.16 | 0.38 |
| 18. Intrusive Grief Thoughts Scale [W1] | −0.19 | −0.25 | 0.32 | 0.07 | 0.39 | 0.61 | 0.28 | 0.26 | 0.15 | 0.14 | 0.08 |
| 19. Texas Revised Inventory of Grief [W1] | −0.10 | −0.22 | 0.22 | 0.00 | 0.27 | 0.48 | 0.20 | 0.24 | 0.21 | 0.19 | 0.16 |
| 20. Intrusive Grief Thoughts Scale [W4] | −0.16 | −0.04 | 0.21 | 0.11 | 0.24 | 0.17 | 0.05 | 0.10 | 0.05 | 0.11 | 0.09 |
| 21. Texas Revised Inventory of Grief [W4] | −0.04 | −0.05 | 0.14 | 0.12 | 0.15 | 0.23 | −0.01 | 0.12 | 0.04 | 0.06 | 0.03 |
| 22. Adapted Inventory of Traumatic Grief [W4] | −0.07 | −0.11 | 0.19 | 0.07 | 0.25 | 0.27 | 0.12 | 0.20 | 0.13 | 0.05 | 0.05 |
| . | 12 . | 13 . | 14 . | 15 . | 16 . | 17 . | 18 . | 19 . | 20 . | 21 . |
|---|---|---|---|---|---|---|---|---|---|---|
| 13. Externalizing problems [W4]—youth | 0.59 | 1 | ||||||||
| 14. Internalizing problems [W4]—parent | 0.41 | 0.35 | 1 | |||||||
| 15. Externalizing problems [W4]—parent | 0.22 | 0.50 | 0.68 | 1 | ||||||
| 16. Internalizing problems [W4]—teacher | 0.14 | 0.30 | 0.31 | 0.43 | 1 | |||||
| 17. Externalizing problems [W4]—teacher | 0.10 | 0.36 | 0.29 | 0.52 | 0.80 | 1 | ||||
| 18. Intrusive Grief Thoughts Scale [W1] | 0.21 | 0.20 | 0.18 | 0.16 | 0.16 | 0.18 | 1 | |||
| 19. Texas Revised Inventory of Grief [W1] | 0.19 | 0.15 | 0.09 | 0.07 | 0.19 | 0.18 | 0.69 | 1 | ||
| 20. Intrusive Grief Thoughts Scale [W4] | 0.44 | 0.26 | 0.23 | 0.16 | 0.13 | 0.13 | 0.37 | 0.2 | 1 | |
| 21. Texas Revised Inventory of Grief [W4] | 0.42 | 0.24 | 0.18 | 0.04 | 0.23 | 0.25 | 0.36 | 0.3 | 0.64 | 1 |
| 22. Adapted Inventory of Traumatic Grief [W4] | 0.61 | 0.43 | 0.34 | 0.22 | 0.26 | 0.28 | 0.37 | 0.3 | 0.77 | 0.74 |
| . | 12 . | 13 . | 14 . | 15 . | 16 . | 17 . | 18 . | 19 . | 20 . | 21 . |
|---|---|---|---|---|---|---|---|---|---|---|
| 13. Externalizing problems [W4]—youth | 0.59 | 1 | ||||||||
| 14. Internalizing problems [W4]—parent | 0.41 | 0.35 | 1 | |||||||
| 15. Externalizing problems [W4]—parent | 0.22 | 0.50 | 0.68 | 1 | ||||||
| 16. Internalizing problems [W4]—teacher | 0.14 | 0.30 | 0.31 | 0.43 | 1 | |||||
| 17. Externalizing problems [W4]—teacher | 0.10 | 0.36 | 0.29 | 0.52 | 0.80 | 1 | ||||
| 18. Intrusive Grief Thoughts Scale [W1] | 0.21 | 0.20 | 0.18 | 0.16 | 0.16 | 0.18 | 1 | |||
| 19. Texas Revised Inventory of Grief [W1] | 0.19 | 0.15 | 0.09 | 0.07 | 0.19 | 0.18 | 0.69 | 1 | ||
| 20. Intrusive Grief Thoughts Scale [W4] | 0.44 | 0.26 | 0.23 | 0.16 | 0.13 | 0.13 | 0.37 | 0.2 | 1 | |
| 21. Texas Revised Inventory of Grief [W4] | 0.42 | 0.24 | 0.18 | 0.04 | 0.23 | 0.25 | 0.36 | 0.3 | 0.64 | 1 |
| 22. Adapted Inventory of Traumatic Grief [W4] | 0.61 | 0.43 | 0.34 | 0.22 | 0.26 | 0.28 | 0.37 | 0.3 | 0.77 | 0.74 |
Note. W2 = posttest; W3 = 11-month follow-up, W4 = 6-year follow-up. Bolded text indicates p < .05.
| . | 1 . | 2 . | 3 . | 4 . | 5 . | 6 . | 7 . | 8 . | 9 . | 10 . | 11 . |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Child age | 1 | ||||||||||
| 2. Positive parenting [W2] | −0.08 | 1 | |||||||||
| 3. Stressful events [W2] | −0.07 | −0.35 | 1 | ||||||||
| 4. Adaptive coping [W2] | −0.04 | 0.30 | −0.05 | 1 | |||||||
| 5. Fear of abandonment [W3] | −0.19 | −0.22 | 0.28 | −0.03 | 1 | ||||||
| 6. Internalizing problems [W1]—youth | −0.10 | −0.38 | 0.48 | −0.16 | 0.39 | 1 | |||||
| 7. Externalizing problems [W1]—youth | 0.08 | −0.31 | 0.40 | −0.17 | 0.18 | 0.55 | 1 | ||||
| 8. Internalizing problems [W1]—parent | −0.04 | −0.25 | 0.10 | −0.11 | 0.05 | 0.27 | 0.09 | 1 | |||
| 9. Externalizing problems [W1]—parent | −0.01 | −0.36 | 0.13 | −0.09 | 0.07 | 0.16 | 0.21 | 0.58 | 1 | ||
| 10. Internalizing problems [W1]—teacher | −0.07 | 0.02 | 0.05 | 0.00 | 0.01 | 0.22 | 0.08 | 0.22 | 0.12 | 1 | |
| 11. Externalizing problems [W1]—teacher | 0.00 | −0.11 | 0.08 | 0.00 | −0.01 | 0.13 | 0.14 | 0.08 | 0.24 | 0.41 | 1 |
| 12. Internalizing problems [W4]—youth | −0.09 | −0.17 | 0.15 | −0.10 | 0.15 | 0.29 | 0.17 | 0.21 | 0.15 | 0.12 | 0.15 |
| 13. Externalizing problems [W4]—youth | −0.15 | −0.24 | 0.20 | −0.12 | 0.11 | 0.23 | 0.31 | 0.24 | 0.34 | 0.02 | 0.16 |
| 14. Internalizing problems [W4]—parent | −0.14 | −0.16 | 0.10 | −0.10 | 0.02 | 0.23 | 0.14 | 0.51 | 0.31 | 0.26 | 0.15 |
| 15. Externalizing problems [W4]—parent | −0.28 | −0.25 | 0.13 | −0.07 | 0.05 | 0.19 | 0.20 | 0.37 | 0.55 | 0.23 | 0.24 |
| 16. Internalizing problems [W4]—teacher | −0.03 | −0.22 | 0.10 | −0.10 | 0.00 | 0.15 | 0.20 | 0.23 | 0.37 | 0.27 | 0.37 |
| 17. Externalizing problems [W4]—teacher | −0.11 | −0.22 | 0.18 | −0.06 | 0.07 | 0.14 | 0.21 | 0.23 | 0.45 | 0.16 | 0.38 |
| 18. Intrusive Grief Thoughts Scale [W1] | −0.19 | −0.25 | 0.32 | 0.07 | 0.39 | 0.61 | 0.28 | 0.26 | 0.15 | 0.14 | 0.08 |
| 19. Texas Revised Inventory of Grief [W1] | −0.10 | −0.22 | 0.22 | 0.00 | 0.27 | 0.48 | 0.20 | 0.24 | 0.21 | 0.19 | 0.16 |
| 20. Intrusive Grief Thoughts Scale [W4] | −0.16 | −0.04 | 0.21 | 0.11 | 0.24 | 0.17 | 0.05 | 0.10 | 0.05 | 0.11 | 0.09 |
| 21. Texas Revised Inventory of Grief [W4] | −0.04 | −0.05 | 0.14 | 0.12 | 0.15 | 0.23 | −0.01 | 0.12 | 0.04 | 0.06 | 0.03 |
| 22. Adapted Inventory of Traumatic Grief [W4] | −0.07 | −0.11 | 0.19 | 0.07 | 0.25 | 0.27 | 0.12 | 0.20 | 0.13 | 0.05 | 0.05 |
| . | 1 . | 2 . | 3 . | 4 . | 5 . | 6 . | 7 . | 8 . | 9 . | 10 . | 11 . |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Child age | 1 | ||||||||||
| 2. Positive parenting [W2] | −0.08 | 1 | |||||||||
| 3. Stressful events [W2] | −0.07 | −0.35 | 1 | ||||||||
| 4. Adaptive coping [W2] | −0.04 | 0.30 | −0.05 | 1 | |||||||
| 5. Fear of abandonment [W3] | −0.19 | −0.22 | 0.28 | −0.03 | 1 | ||||||
| 6. Internalizing problems [W1]—youth | −0.10 | −0.38 | 0.48 | −0.16 | 0.39 | 1 | |||||
| 7. Externalizing problems [W1]—youth | 0.08 | −0.31 | 0.40 | −0.17 | 0.18 | 0.55 | 1 | ||||
| 8. Internalizing problems [W1]—parent | −0.04 | −0.25 | 0.10 | −0.11 | 0.05 | 0.27 | 0.09 | 1 | |||
| 9. Externalizing problems [W1]—parent | −0.01 | −0.36 | 0.13 | −0.09 | 0.07 | 0.16 | 0.21 | 0.58 | 1 | ||
| 10. Internalizing problems [W1]—teacher | −0.07 | 0.02 | 0.05 | 0.00 | 0.01 | 0.22 | 0.08 | 0.22 | 0.12 | 1 | |
| 11. Externalizing problems [W1]—teacher | 0.00 | −0.11 | 0.08 | 0.00 | −0.01 | 0.13 | 0.14 | 0.08 | 0.24 | 0.41 | 1 |
| 12. Internalizing problems [W4]—youth | −0.09 | −0.17 | 0.15 | −0.10 | 0.15 | 0.29 | 0.17 | 0.21 | 0.15 | 0.12 | 0.15 |
| 13. Externalizing problems [W4]—youth | −0.15 | −0.24 | 0.20 | −0.12 | 0.11 | 0.23 | 0.31 | 0.24 | 0.34 | 0.02 | 0.16 |
| 14. Internalizing problems [W4]—parent | −0.14 | −0.16 | 0.10 | −0.10 | 0.02 | 0.23 | 0.14 | 0.51 | 0.31 | 0.26 | 0.15 |
| 15. Externalizing problems [W4]—parent | −0.28 | −0.25 | 0.13 | −0.07 | 0.05 | 0.19 | 0.20 | 0.37 | 0.55 | 0.23 | 0.24 |
| 16. Internalizing problems [W4]—teacher | −0.03 | −0.22 | 0.10 | −0.10 | 0.00 | 0.15 | 0.20 | 0.23 | 0.37 | 0.27 | 0.37 |
| 17. Externalizing problems [W4]—teacher | −0.11 | −0.22 | 0.18 | −0.06 | 0.07 | 0.14 | 0.21 | 0.23 | 0.45 | 0.16 | 0.38 |
| 18. Intrusive Grief Thoughts Scale [W1] | −0.19 | −0.25 | 0.32 | 0.07 | 0.39 | 0.61 | 0.28 | 0.26 | 0.15 | 0.14 | 0.08 |
| 19. Texas Revised Inventory of Grief [W1] | −0.10 | −0.22 | 0.22 | 0.00 | 0.27 | 0.48 | 0.20 | 0.24 | 0.21 | 0.19 | 0.16 |
| 20. Intrusive Grief Thoughts Scale [W4] | −0.16 | −0.04 | 0.21 | 0.11 | 0.24 | 0.17 | 0.05 | 0.10 | 0.05 | 0.11 | 0.09 |
| 21. Texas Revised Inventory of Grief [W4] | −0.04 | −0.05 | 0.14 | 0.12 | 0.15 | 0.23 | −0.01 | 0.12 | 0.04 | 0.06 | 0.03 |
| 22. Adapted Inventory of Traumatic Grief [W4] | −0.07 | −0.11 | 0.19 | 0.07 | 0.25 | 0.27 | 0.12 | 0.20 | 0.13 | 0.05 | 0.05 |
| . | 12 . | 13 . | 14 . | 15 . | 16 . | 17 . | 18 . | 19 . | 20 . | 21 . |
|---|---|---|---|---|---|---|---|---|---|---|
| 13. Externalizing problems [W4]—youth | 0.59 | 1 | ||||||||
| 14. Internalizing problems [W4]—parent | 0.41 | 0.35 | 1 | |||||||
| 15. Externalizing problems [W4]—parent | 0.22 | 0.50 | 0.68 | 1 | ||||||
| 16. Internalizing problems [W4]—teacher | 0.14 | 0.30 | 0.31 | 0.43 | 1 | |||||
| 17. Externalizing problems [W4]—teacher | 0.10 | 0.36 | 0.29 | 0.52 | 0.80 | 1 | ||||
| 18. Intrusive Grief Thoughts Scale [W1] | 0.21 | 0.20 | 0.18 | 0.16 | 0.16 | 0.18 | 1 | |||
| 19. Texas Revised Inventory of Grief [W1] | 0.19 | 0.15 | 0.09 | 0.07 | 0.19 | 0.18 | 0.69 | 1 | ||
| 20. Intrusive Grief Thoughts Scale [W4] | 0.44 | 0.26 | 0.23 | 0.16 | 0.13 | 0.13 | 0.37 | 0.2 | 1 | |
| 21. Texas Revised Inventory of Grief [W4] | 0.42 | 0.24 | 0.18 | 0.04 | 0.23 | 0.25 | 0.36 | 0.3 | 0.64 | 1 |
| 22. Adapted Inventory of Traumatic Grief [W4] | 0.61 | 0.43 | 0.34 | 0.22 | 0.26 | 0.28 | 0.37 | 0.3 | 0.77 | 0.74 |
| . | 12 . | 13 . | 14 . | 15 . | 16 . | 17 . | 18 . | 19 . | 20 . | 21 . |
|---|---|---|---|---|---|---|---|---|---|---|
| 13. Externalizing problems [W4]—youth | 0.59 | 1 | ||||||||
| 14. Internalizing problems [W4]—parent | 0.41 | 0.35 | 1 | |||||||
| 15. Externalizing problems [W4]—parent | 0.22 | 0.50 | 0.68 | 1 | ||||||
| 16. Internalizing problems [W4]—teacher | 0.14 | 0.30 | 0.31 | 0.43 | 1 | |||||
| 17. Externalizing problems [W4]—teacher | 0.10 | 0.36 | 0.29 | 0.52 | 0.80 | 1 | ||||
| 18. Intrusive Grief Thoughts Scale [W1] | 0.21 | 0.20 | 0.18 | 0.16 | 0.16 | 0.18 | 1 | |||
| 19. Texas Revised Inventory of Grief [W1] | 0.19 | 0.15 | 0.09 | 0.07 | 0.19 | 0.18 | 0.69 | 1 | ||
| 20. Intrusive Grief Thoughts Scale [W4] | 0.44 | 0.26 | 0.23 | 0.16 | 0.13 | 0.13 | 0.37 | 0.2 | 1 | |
| 21. Texas Revised Inventory of Grief [W4] | 0.42 | 0.24 | 0.18 | 0.04 | 0.23 | 0.25 | 0.36 | 0.3 | 0.64 | 1 |
| 22. Adapted Inventory of Traumatic Grief [W4] | 0.61 | 0.43 | 0.34 | 0.22 | 0.26 | 0.28 | 0.37 | 0.3 | 0.77 | 0.74 |
Note. W2 = posttest; W3 = 11-month follow-up, W4 = 6-year follow-up. Bolded text indicates p < .05.
Preregistered Analyses
The FBP significantly increased positive parenting (β = 0.123, SE = 0.044, 95% CI = [0.037–0.210], p = .005), significantly increased adaptive coping (β = 0.128, SE = 0.054, 95% CI = [0.022– 0.234], p = .018), and significantly reduced stressful events (β = −.117, SE = 0.056, 95% CI = [−0.226 to −.007], p = .037) at posttest (note that these paths were previously established; see Sandler et al., 2003 for all primary analyses and subgroup analyses). Fewer stressful events at posttest were in turn associated with lower fear of abandonment at the 11-month follow-up (β = 0.164, SE = 0.058, 95% CI = [0.050–0.277], p = .005). However, after accounting for the effect of stressful events, positive parenting and adaptive coping at posttest were not related to fear of abandonment at the 11-month follow-up (p = .639 and p = .921, respectively). Fear of abandonment at the 11-month follow-up was not related to internalizing or externalizing problems at the 6-year follow-up, according to youth (p = .913 and p = .997, respectively), caregiver (p = .866 and p = .692, respectively), or teacher report (p = .975 and p = .857, respectively). Fear of abandonment at the 11-month follow-up was also not related to maladaptive grief at the 6-year follow-up, as measured by the bifactor model of grief (General factor: p = .250, Social Detachment/Insecurity factor: p = .678, Intrusive Grief Thoughts factor: p = .146, Continuing Affective Reactions factor: p = 1.00) or by individual grief scales (IGTS: p = .113, TRIG: p = .254, ITG: p = .054). The indirect effect of the FBP on fear of abandonment through the reduction of stressful events was significant (ab = −.036; 95% CI = [−0.086 to −0.001]; see Figure 1).
After accounting for fear of abandonment, the direct effects of the FBP on youth outcomes at the 6-year follow-up were not significant (p’s range from .103 to .949) with two exceptions. There were direct effects of the FBP on teacher-reported internalizing and externalizing problems (β = −.235, SE = 0.095, 95% CI = [−0.417 to −0.051], p = .013 and β = −.238, SE = 0.098, 95% CI = [−0.438 to −0.048], p = .115, respectively). In the model, there was a direct effect of posttest positive parenting on youth self-report of externalizing problems at the 6-year follow-up (β = −.162, SE = 0.079, 95% CI = [−0.313 to −0.003], p = .041). There was also a direct effect (in the opposite expected direction) of posttest adaptive coping on children’s self-report of maladaptive grief as measured by the IGTS scale (β = 0.131, SE = 0.063, 95% CI = [0.000–0.246], p = .039) at the 6-year follow-up. However, although the p value was below .05, the 95% CI included zero.
Exploratory Analyses
We re-tested the mediation model to assess age and gender moderation effects. The effects of the FBP on positive parenting, adaptive coping, and stressful events at posttest were tested in the prospective models reported previously; results are not repeated here.
Moderation by Youth Age and Gender
Age did not moderate FBP-induced changes in positive parenting, adaptive coping, or stressful events at posttest on fear of abandonment at the 11-month follow-up or paths from fear of abandonment at the 11-month follow-up to youth- or caregiver-reported mental health problems or youth-reported maladaptive grief at six-year follow-up.
Gender did not moderate paths from FBP-induced changes in positive parenting, adaptive coping, or stressful events at posttest on fear of abandonment at the 11-month follow-up. Gender significantly moderated the effect of fear of abandonment at the 11-month follow-up on teacher-reported internalizing problems and youth-reported maladaptive grief at the 6-year follow-up. Simple slope analyses indicated that for girls only, higher fear of abandonment at the 11-month follow-up predicted higher teacher-reported internalizing problems (girls: β = 0.218, SE = 0.104, 95% CI = [0.015–0.422], p = .035; boys: β = −0.216, SE = 0.132, 95% CI = [−0.474, 0.042], p = .101) and higher scores on the self-reported ITG (girls: β = 0.352, SE = 0.124, 95% CI = [0.108–0.596], p = .005; boys: β = 0.013, SE = 0.107, 95% CI = [−0.197 to 0.222], p = .907) at the 6-year follow-up. Thus, the indirect effect of the FBP on girls’ internalizing problems (teacher-reported) and grief (self-reported) through reduction of posttest stressful events and in turn, fear of abandonment, was significant according to the joint significance test (MacKinnon et al., 2012). See path models by gender in Supplementary Table 1. Note that although certain A paths from FBP to positive parenting, adaptive coping, and stressful events are not significant in some of the gender-specific models, the effect sizes were equal to or larger than the corresponding parameters in the overall model. We attribute the differences to statistical power. The B path from stressful events to fear of abandonment is statistically significant only for girls in the gender-specific path models. However, the formal difference test conducted via model constraint was not significant. Considering the multiple exploratory analyses conducted, we opted to only interpret model differences that were statistically significant.
Discussion
To our knowledge, this is the first study to assess the preventive effects of intervention-induced changes in individual- and family-level processes on the self-system belief of fear of abandonment and its prospective effects on youth mental health problems beyond one year. The findings showed that intervention-induced reductions in stressful events were significantly, prospectively associated with a lower fear of abandonment for youth who experienced the death of a parent. For girls only, fear of abandonment mediated the effect of the FBP on teacher reports of internalizing problems and self reports of maladaptive grief during late adolescence/young adulthood six years later. Positive parenting and adaptive coping were significantly related to fear of abandonment in univariate analyses, but these effects were nonsignificant after controlling for stressful events.
These findings extend our understanding of how the self-system belief of fear of abandonment affects the outcomes of at-risk youth. Although other studies that have used different subsets of the larger project from which the current sample was drawn (Wolchik et al., 2006, 2008) found significant associations between fear of abandonment and mental health problems and grief concurrently and about a year later, this study is the first to examine the longer-term effects of fear of abandonment on youth outcomes and to test mediation effects across 6 years. Also, the experimental design strengthens the inferences that can be made about the effects of stressful events on fear of abandonment compared to inferences that can be drawn from previous cross-sectional and passive longitudinal designs with parentally bereaved youth (Wolchik et al., 2006, 2008) and youth in divorced families (O’Hara et al., 2021; Wolchik et al., 2002). This study strengthens the evidence of the importance of fear of abandonment after parental death by demonstrating its role in the multi-link pathway through which the FBP affects mental health problems and grief in parentally bereaved youth. The finding that fear of abandonment predicted mental health problems is consistent with studies with samples of youth who experienced other adverse family events, such as parental divorce (O’Hara et al., 2021; Wolchik et al., 2002).
The findings on the mental health implications of fear of abandonment are consistent with theoretical work on the relations between the need for relatedness and attachment organization and mental health outcomes in the general population (see Baumeister & Leary, 1995 and Greenberg, 1999, for reviews), and in bereaved populations (Kosminsky & Jordan, 2016). They also support the theoretical proposition that the effects of stressful events on mental health problems are mediated through threats to the basic motivational need to be part of a caring social group (Sandler, 2001). In addition, they suggest a unique protective effect of reducing stressful events, given that posttest positive parenting and adaptive coping were related to fear of abandonment in univariate analyses, but these effects became nonsignificant after controlling for stressful events.
These findings extend the underlying theory of the FBP by identifying which factors targeted by the FBP affected the basic psychological need for social relatedness. Prior studies have found that increases in adaptive coping (Sandler et al., 2023) and positive parenting (Sandler et al., 2015) but not reductions in stressful events at posttest mediated the effects of the FBP on internalizing problems at 6-year follow-up. In this study, an indirect effect of stressful events on 6-year internalizing problems was found through its effects to reduce fear of abandonment at the 11-month follow-up. This is the first study to support a prospective multi-link pathway through which the FBP reduced intrusive grief 6 years later. The study helps to unpack the multiple pathways through which different components of the FBP impact long-term outcomes for bereaved youth. Taken together, these studies illustrate that multi-component prevention programs may impact children’s needs in different ways. The current study provides support for the activities in the FBP that may have contributed to reducing children’s exposure to stressful events, including activities to reduce parent depression and grief, and to protect children from involvement in stressors that are beyond their control (see Ayers et al., 2013 for a full description of the components of the FBP).
The finding that the longitudinal effects on internalizing problems and grief were significant only for girls is consistent with prior evidence that FBP significantly improved mental health problems at the 11-month follow-up for girls but not for boys (Sandler et al., 2003). Fear of abandonment may have a greater impact on girls than boys due to girls’ higher implicit need for affiliation (Drescher & Schultheiss, 2016), a need that is likely to be threatened by fear of abandonment. Girls may also be more likely than boys to take on nurturing and caregiving roles in their family after death and may be more affected by the stress that their caregivers experience (Grant & Compas, 1995) both of which could lead to higher internalizing problems and more maladaptive grief. An important direction for future research is identifying the processes that explain these gender differences. It is important to note that the effect of fear of abandonment on teachers' reports of girls’ internalizing problems may reflect a developmental effect in addition to a gender effect. Participants who had teacher reports at the 6-year follow-up were those youth who participated in the program at a younger age. Future research should investigate whether this effect generalizes to older youth. Including other reporters in future investigations, such as a boss or a friend, could answer this question.
It is interesting to speculate how fear of abandonment mediated relations between intervention-induced reductions in stressful events and mental health problems and maladaptive grief. Parental death is accompanied by major changes in a child’s social world. In addition to the loss of a parent, parental death often results in a cascade of other changes, such as spending less high-quality time with their other parent or caregiver, who is also managing their grief and grappling with death-related stressful events like moving or taking on additional work responsibilities. They may also lose contact with important peers and supportive adults if they move neighborhoods or change schools. Stressful events involving social losses may lead to concerns about who will provide for their basic needs which may increase attention to distressing internal cues and result in rumination or feelings of helplessness, which can then lead to internalizing problems and maladaptive grief (Eisma & Stroebe, 2017; Reivich et al., 2013; van der Houwen et al., 2010; Wolchik et al., 2002).
The current study has many methodological strengths, including using a four-wave longitudinal study design, multiple reporters of parenting and youth mental health problems, and a relatively diverse sample (i.e., 33% non-White; 16% below the poverty line). However, some limitations should be addressed in future research. First, except for teacher reports of bereaved girls’ internalizing problems, the significant effects are within-reporter effects, raising concerns about the possibility of bias due to shared method variance. Second, the study was a university-based efficacy trial in a metropolitan area with many exclusion criteria. For example, although youth enrolled in other forms of grief counseling were excluded to better understand the unique effects of the FBP, it is possible that youth experiencing greater difficulties after the death are not well represented. Tests of the current model with more representative samples of bereaved families in community settings across regions would be important. Third, the bifactor models used to measure grief are methodologically sophisticated but have only been evaluated in the current sample. Data from other samples will support the bifactor model’s generalizability. Fourth, although the sample is relatively diverse in socioeconomic status, race, and ethnicity, the sample size is too small to assess subgroup-specific intervention effects. Fifth, although its longitudinal measurement is an important strength of the data, this trial was conducted nearly 20 years ago. We cannot identify strong reasons to believe the psychological processes of grief would change as a function of time. However, the context of death and loss certainly has changed, including increased exposure to media reports of gun violence and pandemic-related deaths, and widespread availability of information about local and worldwide tragedies. It is unknown whether the findings generalize to bereavement in the context of these situations. Finally, the prospective aspect of the study had a lag of five years between assessments. It is possible that a shorter lag may have shown additional links between fear of abandonment and youth outcomes.
The current findings suggest that reducing stressful events should be included as a central focus of preventive interventions to promote pediatric health and development after parental death. Bereaved children are often targeted for prevention efforts through community- or church-based grief support and hospice agencies. These interventions may be strengthened by focusing on factors that have been shown to impact children’s resilience. For example, other prevention programs for bereaved families may benefit from incorporating skills taught in the FBP that may be responsible for reducing stressful events following the death, such as teaching caregivers to protect their children from stressful events (e.g., seeing their caregiver intoxicated, emotionally upset, or arguing with others, and hearing about financial struggles), and helping caregivers establish positive stable routines to reassure children that they are secure in their new family structure. For programs to have a significant public health impact, it will require process-oriented translational research, theory- and evidence-informed intervention development, and rigorous evaluation and optimization of the programs.
Footnotes
We attempted to estimate these models in Mplus but the models would not converge.
Supplementary Data
Supplementary data can be found at: https://dbpia.nl.go.kr/jpepsy.
Acknowledgments
We thank the parents and children who participated in this study and the graduate students and REACH staff who helped to conduct the earlier waves of the project. The content is solely the authors' responsibility and does not necessarily represent the official views of the National Institutes of Health. Trial registration: ClinicalTrials.gov NCT01008189.
Author Contributions
Karey L. O’Hara (Conceptualization [lead], Formal analysis [lead], Writing—original draft [lead], Writing—review & editing [equal]), Sharlene A. Wolchik (Conceptualization [equal], Funding acquisition [equal], Methodology [equal], Project administration [equal], Writing—original draft [supporting], Writing—review & editing [equal]), C. Aubrey Rhodes (Conceptualization, Writing—review & editing [supporting]), Rana N. Uhlman (Conceptualization, Formal analysis, Writing—review & editing [supporting]), Irwin N. Sandler (Conceptualization [supporting], Funding acquisition [equal], Methodology [equal], Project administration [equal], Writing—review & editing [supporting]), and Jenn-Yun Tein (Formal analysis, Writing—review & editing [supporting])
Funding
This research was funded by the National Institute of Mental Health (R01MH49156 and P30MH068685). K. L. O’Hara’s work on this paper was supported by a career development award provided by the National Institute of Mental Health (K01MH120321). C. A. Rhodes’ work was supported by a predoctoral fellowship provided by the National Institute on Drug Abuse (T32DA039772). S. A. Wolchik and I. N. Sandler’s work on this paper was supported by a grant from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (R01HD094334) and the New York Life Foundation. J.-Y. Tein’s work was supported by a grant from the National Institute on Drug Abuse (4R37DA009757) and the Eunice Kennedy Shriver National Institute of Child Health and Human Development (R01HD094334).
Conflicts of interest
None declared.
Data Availability
Data are available on request.
References
Jones, S., & Twohey, J. L. (1998, August). Parents' expression of emotions questionnaire: Psychometric properties. In 106th Annual Convention of the American Psychological Association, San Francisco.
Program for Prevention Research. Family Bereavement Program documentation. Arizona State University; Tempe, AZ:



