-
PDF
- Split View
-
Views
-
Cite
Cite
Katelynn E Boerner, Lauren E Harrison, Eleanor A J Battison, Corrin Murphy, Anna C Wilson, Topical Review: Acute and Chronic Pain Experiences in Transgender and Gender-Diverse Youth, Journal of Pediatric Psychology, Volume 48, Issue 12, December 2023, Pages 984–991, https://doi.org/10.1093/jpepsy/jsad075
Close - Share Icon Share
Abstract
To provide an overview of the existing literature on gender diversity in pediatric acute and chronic pain, propose an ecological systems model of understanding pain in transgender and gender-diverse (TGD) youth, and identify a direction for future work that will address the key knowledge gaps identified.
Relevant literature on pain and gender diversity was reviewed, drawing from adult literature where there was insufficient evidence in pediatric populations. Existing relevant models for understanding minority stress, gender and pain, and pain experiences within marginalized groups were considered with the reviewed literature to develop a pain model in TGD youth.
While there is an abundance of literature pointing to increased risk for pain experiences amongst TGD youth, there is comparably little empirical evidence of the rates of pain amongst TGD youth, prevalence of TGD identities in pain care settings, effective pain treatments for TGD youth and unique considerations for their care, and the role intersectional factors in understanding TGD youth identities and pain.
Pediatric psychologists are well-positioned to advance the research on acute and chronic pain in TGD youth, make evidence-based adaptations to clinical care for TGD youth with pain, including pain related to gender affirmation, and support colleagues within the medical system to provide more inclusive care.
Introduction
Transgender and gender-diverse (TGD) youth is an umbrella term for youth whose gender identity or expression is different from culturally expected norms for their assigned sex at birth. While prevalence rates differ based on definitions and measurement, TGD youth are estimated to represent 3% of the general population and are disproportionately affected by poor physical and mental health, as well as discrimination in healthcare (Rider et al., 2018). Acute and chronic pain are common in childhood, with incidence increasing in adolescence (King et al., 2011). Acute refers to brief periods of pain (i.e.,<3 months), often associated with an illness, injury, or medical procedure, and is expected to resolve when the precipitating cause has healed (IASP, 2023). Chronic pain is defined as pain that persists or recurs for more than 3 months and can be associated with a medical condition or diagnosed as a condition in its own right (Treede et al., 2019). Both acute and chronic pain are more common among individuals assigned female at birth following puberty, with extensive understanding of biological bases of these differences from studies of animals and adult humans (Mogil, 2020). In contrast to sex, “gender” refers to a broad spectrum of individual identities, societal roles/expectations, behaviors, and expressions, and has received far less attention in pain literature (Keogh, 2021). In the current review, we focus on the experiences of acute and chronic pain in TGD youth, summarizing the scant literature and identifying key knowledge gaps. We propose a theoretical model to guide future research on biopsychosocial and ecological factors that influence pain in TGD youth and provide suggestions for increasing inclusivity in pain research and care.
Review of Existing Literature
Research on exposure to stressful experiences demonstrates that chronic pain develops from an interaction of persistent biological, psychological, and social stressors (Nelson et al., 2021). This is particularly relevant for TGD youth, given their exposure to minority stressors including transphobic legislation restricting healthcare access, discrimination, non-affirmation of gender identity, and victimization (Delozier et al., 2020). Despite this increased risk, data regarding prevalence of pain in TGD individuals is largely absent (Table I).
| Author, Year, Country . | Aims . | Study Design . | Study Population . | Main Findings . |
|---|---|---|---|---|
| Abern et al. (2022), USA | To determine the prevalence of self-reported vulvar pain symptoms and dyspareunia in this population and investigate its relationship to gender-affirming hormone therapy with testosterone. | Cross-sectional, quantitative study with a single time point survey | English-speaking trans men/masculine or AFAB individuals ages 18–64 (Mage = 27 years), n = 782. | Among the participants, 59.8% reported using testosterone. Unintentional pain with sexual intercourse was experienced in 61.5% of participants. Sixty-eight out of 710 (9.6%) participants endorsed vulvar pain symptoms; 61.8% were on testosterone. Trans-masculine individuals had a higher prevalence of dyspareunia than the general population, but the prevalence of vulvar pain was similar to that experienced among cis-gender women. |
| Aloisi et al. (2007), Italy | To study the relationship between sex hormones and pain. | Two-part semi-structured interview and questionnaire of transgender patients seen at the Movimetno Identita Transsuale Center in Bologna for at least 1 year of hormone treatment between December 2003 and December 2005. | Transgender patients (MtF, FtM) receiving hormone treatments for at least 1 year between ages 25–40, n = 73 (all Caucasian). | Results suggest that HRT might impact existing chronic pain and new pain experiences. |
| Anaya (2018), USA | Describe the experience of the impact of intersecting minority identifies of a transgender adolescent receiving psychiatric care for post-traumatic stress disorder (PTSD). | Case study describing the case of a transgender adolescent with PTSD, who experiences chronic pain, receiving care for physiologic dysregulation. | A case study of a 17-year-old Mexican-American transgender male who experienced a traumatic brain injury and consequently experienced PTSD and chronic pain. | The experience and manifestations of chronic pain and PTSD in this specific patient may likely be influenced by the stressors of his intersecting minority identities. |
| Lang et al. (2021), Denmark | To investigate the prevalence and severity of postsurgical persistent pain, sensory disturbances and complications in trans men after mastectomies | Cross-sectional questionnaire retrospectively evaluating postsurgical pain and disturbances in trans men who received mastectomies. | Trans men between 18 and 70 at the time of surgery who underwent mastectomies between 9/1/2013 and 8/31/2018 in Copenhagen University Hospital, Denmark. N = 92 (Mage = 23). | Adult transmasculine men who underwent masculinizing top surgery (bilateral mastectomy) in Denmark revealed that 27% reported persistent pain following surgery. Of patients reporting pain, 90.1% experienced mild to moderate pain. Neuropathic pain was reported for n = 4 (4.8%) participants. |
| MacGregor and van den Brink (2019), United Kingdom and Netherlands | Review existing literature that describes issues relating migraines and migraine management, and hormone therapy in transgender men and women. | Literature review. | Trans adults undergoing HRT experiencing migraines. | There is a higher prevalence of migraines among transgender women taking estrogen, and is reduced amongst transgender men who take testosterone. Evidence suggests migraines with aura is associated with an increased risk of ischemic stroke in cisgender women, which is increased by the use of estrogen and other biological and behavioral factors. |
| Peitzmeier et al. (2017), USA | To understand the prevalence of negative health outcomes among adults who bind, identify risk factors for negative health outcomes, and develop recommendations for healthy binding informed by these risk factors. | Quantitative 32 item cross-sectional survey study administered online to a non-random sampled of adults over the age of 18 who were assigned female at birth, or self-identified as intersex. | Open to all people assigned female at birth and intersex individuals over 18 years (ages 18–66; Mage = 23) who bound either currently or at some point in their lives (n = 1800). Participants from over 38 countries were represented in data collection. | Mental health benefits were associated with chest binding. 97% of TGD individuals who engaged in chest binding experienced at least one negative physical symptom, with 54% reporting back pain and 49% chest pain. |
| Peitzmeier et al. (2021), USA | To assess the timeline of symptoms development related to binding in transgender youth | Quantitative cross-sectional survey study administered online to a non-random sampled of adults who were assigned female at birth. Assessed lifetime prevalence of 27 symptoms related to binding. | Data were part of a larger study open to all people assigned female at birth and intersex individuals over 18 years (ages: 18–66; Mage = 23) who bound either currently or at some point in their lives (n = 1800). Participants from over 38 countries were represented in data collection. This analysis focused on study participants between ages 18–24 (58% of the original sample). | Most symptoms related to binding emerged quickly, and most people who experienced these symptoms experienced them within their first binding year. Rarer outcomes and more serious outcomes took longer to occur. There was often rapid onset of pain and intensity continued to rise over time, peaking at 5 or more years of binding. |
| Sayeem et al. (2021), USA | To review the clinical presentation of eight youths with GD in a multidisciplinary chronic pain clinic | A retrospective chart review of youth who received care in a multidisciplinary chronic pain clinic who identified as experiencing gender dysphoria. | Participants were eight youths (Mage = 14.6) who attended a multidisciplinary chronic pain clinic and endorsed experiencing gender dysphoria from January 2017 to September 2019. Patients included in the cohort were being seen by an endocrinologist concurrently. | The mean age of the onset of pain symptoms was 11.25 years with a median of 4.5 visits to the pain program for chronic pain treatment. They have a mean Pain Burden Interview score of 12.86. Researchers found a downward trend in pain scores of patients who were treated for chronic pain and gender dysphoria. |
| Yalinay Dikmen et al. (2021), Turkey | To investigate the frequency, characteristics, and treatment of migraine and tension heads among trans men (FtM), as well as in relation to psychiatric comorbidities and lifetime experiences of being a trans person in Turkey | Quantitative cross-sectional survey study assessing demographics, gender identity transition inventory, psychological health outcomes, and experiences with headaches. | Participants were n = 88 trans men (FtM individuals) 18 years and older (Mage = 24.8) diagnosed and followed up by the psychiatry department for gender dysphoria between July 2018 and December 2019. | 36.4% of participants were diagnosed with migraines and 40.9% were diagnosed with tension headaches. Participants with migraines scored higher on depression and anxiety measures, experienced longer and more severe headaches, and higher likelihood of menstruation acting as a trigger than participants with tension headaches. Higher levels of care utilization for headaches was found among the participants with migraines. Overall, migraines and tension headaches were common in the study population. |
| Author, Year, Country . | Aims . | Study Design . | Study Population . | Main Findings . |
|---|---|---|---|---|
| Abern et al. (2022), USA | To determine the prevalence of self-reported vulvar pain symptoms and dyspareunia in this population and investigate its relationship to gender-affirming hormone therapy with testosterone. | Cross-sectional, quantitative study with a single time point survey | English-speaking trans men/masculine or AFAB individuals ages 18–64 (Mage = 27 years), n = 782. | Among the participants, 59.8% reported using testosterone. Unintentional pain with sexual intercourse was experienced in 61.5% of participants. Sixty-eight out of 710 (9.6%) participants endorsed vulvar pain symptoms; 61.8% were on testosterone. Trans-masculine individuals had a higher prevalence of dyspareunia than the general population, but the prevalence of vulvar pain was similar to that experienced among cis-gender women. |
| Aloisi et al. (2007), Italy | To study the relationship between sex hormones and pain. | Two-part semi-structured interview and questionnaire of transgender patients seen at the Movimetno Identita Transsuale Center in Bologna for at least 1 year of hormone treatment between December 2003 and December 2005. | Transgender patients (MtF, FtM) receiving hormone treatments for at least 1 year between ages 25–40, n = 73 (all Caucasian). | Results suggest that HRT might impact existing chronic pain and new pain experiences. |
| Anaya (2018), USA | Describe the experience of the impact of intersecting minority identifies of a transgender adolescent receiving psychiatric care for post-traumatic stress disorder (PTSD). | Case study describing the case of a transgender adolescent with PTSD, who experiences chronic pain, receiving care for physiologic dysregulation. | A case study of a 17-year-old Mexican-American transgender male who experienced a traumatic brain injury and consequently experienced PTSD and chronic pain. | The experience and manifestations of chronic pain and PTSD in this specific patient may likely be influenced by the stressors of his intersecting minority identities. |
| Lang et al. (2021), Denmark | To investigate the prevalence and severity of postsurgical persistent pain, sensory disturbances and complications in trans men after mastectomies | Cross-sectional questionnaire retrospectively evaluating postsurgical pain and disturbances in trans men who received mastectomies. | Trans men between 18 and 70 at the time of surgery who underwent mastectomies between 9/1/2013 and 8/31/2018 in Copenhagen University Hospital, Denmark. N = 92 (Mage = 23). | Adult transmasculine men who underwent masculinizing top surgery (bilateral mastectomy) in Denmark revealed that 27% reported persistent pain following surgery. Of patients reporting pain, 90.1% experienced mild to moderate pain. Neuropathic pain was reported for n = 4 (4.8%) participants. |
| MacGregor and van den Brink (2019), United Kingdom and Netherlands | Review existing literature that describes issues relating migraines and migraine management, and hormone therapy in transgender men and women. | Literature review. | Trans adults undergoing HRT experiencing migraines. | There is a higher prevalence of migraines among transgender women taking estrogen, and is reduced amongst transgender men who take testosterone. Evidence suggests migraines with aura is associated with an increased risk of ischemic stroke in cisgender women, which is increased by the use of estrogen and other biological and behavioral factors. |
| Peitzmeier et al. (2017), USA | To understand the prevalence of negative health outcomes among adults who bind, identify risk factors for negative health outcomes, and develop recommendations for healthy binding informed by these risk factors. | Quantitative 32 item cross-sectional survey study administered online to a non-random sampled of adults over the age of 18 who were assigned female at birth, or self-identified as intersex. | Open to all people assigned female at birth and intersex individuals over 18 years (ages 18–66; Mage = 23) who bound either currently or at some point in their lives (n = 1800). Participants from over 38 countries were represented in data collection. | Mental health benefits were associated with chest binding. 97% of TGD individuals who engaged in chest binding experienced at least one negative physical symptom, with 54% reporting back pain and 49% chest pain. |
| Peitzmeier et al. (2021), USA | To assess the timeline of symptoms development related to binding in transgender youth | Quantitative cross-sectional survey study administered online to a non-random sampled of adults who were assigned female at birth. Assessed lifetime prevalence of 27 symptoms related to binding. | Data were part of a larger study open to all people assigned female at birth and intersex individuals over 18 years (ages: 18–66; Mage = 23) who bound either currently or at some point in their lives (n = 1800). Participants from over 38 countries were represented in data collection. This analysis focused on study participants between ages 18–24 (58% of the original sample). | Most symptoms related to binding emerged quickly, and most people who experienced these symptoms experienced them within their first binding year. Rarer outcomes and more serious outcomes took longer to occur. There was often rapid onset of pain and intensity continued to rise over time, peaking at 5 or more years of binding. |
| Sayeem et al. (2021), USA | To review the clinical presentation of eight youths with GD in a multidisciplinary chronic pain clinic | A retrospective chart review of youth who received care in a multidisciplinary chronic pain clinic who identified as experiencing gender dysphoria. | Participants were eight youths (Mage = 14.6) who attended a multidisciplinary chronic pain clinic and endorsed experiencing gender dysphoria from January 2017 to September 2019. Patients included in the cohort were being seen by an endocrinologist concurrently. | The mean age of the onset of pain symptoms was 11.25 years with a median of 4.5 visits to the pain program for chronic pain treatment. They have a mean Pain Burden Interview score of 12.86. Researchers found a downward trend in pain scores of patients who were treated for chronic pain and gender dysphoria. |
| Yalinay Dikmen et al. (2021), Turkey | To investigate the frequency, characteristics, and treatment of migraine and tension heads among trans men (FtM), as well as in relation to psychiatric comorbidities and lifetime experiences of being a trans person in Turkey | Quantitative cross-sectional survey study assessing demographics, gender identity transition inventory, psychological health outcomes, and experiences with headaches. | Participants were n = 88 trans men (FtM individuals) 18 years and older (Mage = 24.8) diagnosed and followed up by the psychiatry department for gender dysphoria between July 2018 and December 2019. | 36.4% of participants were diagnosed with migraines and 40.9% were diagnosed with tension headaches. Participants with migraines scored higher on depression and anxiety measures, experienced longer and more severe headaches, and higher likelihood of menstruation acting as a trigger than participants with tension headaches. Higher levels of care utilization for headaches was found among the participants with migraines. Overall, migraines and tension headaches were common in the study population. |
Note. AFAB: assigned female at birth; AMAB: assigned male at birth; MtF: male-to-female; FtM: female-to-male; HRT: hormone replacement therapy; TGD: trans- and gender diverse.
| Author, Year, Country . | Aims . | Study Design . | Study Population . | Main Findings . |
|---|---|---|---|---|
| Abern et al. (2022), USA | To determine the prevalence of self-reported vulvar pain symptoms and dyspareunia in this population and investigate its relationship to gender-affirming hormone therapy with testosterone. | Cross-sectional, quantitative study with a single time point survey | English-speaking trans men/masculine or AFAB individuals ages 18–64 (Mage = 27 years), n = 782. | Among the participants, 59.8% reported using testosterone. Unintentional pain with sexual intercourse was experienced in 61.5% of participants. Sixty-eight out of 710 (9.6%) participants endorsed vulvar pain symptoms; 61.8% were on testosterone. Trans-masculine individuals had a higher prevalence of dyspareunia than the general population, but the prevalence of vulvar pain was similar to that experienced among cis-gender women. |
| Aloisi et al. (2007), Italy | To study the relationship between sex hormones and pain. | Two-part semi-structured interview and questionnaire of transgender patients seen at the Movimetno Identita Transsuale Center in Bologna for at least 1 year of hormone treatment between December 2003 and December 2005. | Transgender patients (MtF, FtM) receiving hormone treatments for at least 1 year between ages 25–40, n = 73 (all Caucasian). | Results suggest that HRT might impact existing chronic pain and new pain experiences. |
| Anaya (2018), USA | Describe the experience of the impact of intersecting minority identifies of a transgender adolescent receiving psychiatric care for post-traumatic stress disorder (PTSD). | Case study describing the case of a transgender adolescent with PTSD, who experiences chronic pain, receiving care for physiologic dysregulation. | A case study of a 17-year-old Mexican-American transgender male who experienced a traumatic brain injury and consequently experienced PTSD and chronic pain. | The experience and manifestations of chronic pain and PTSD in this specific patient may likely be influenced by the stressors of his intersecting minority identities. |
| Lang et al. (2021), Denmark | To investigate the prevalence and severity of postsurgical persistent pain, sensory disturbances and complications in trans men after mastectomies | Cross-sectional questionnaire retrospectively evaluating postsurgical pain and disturbances in trans men who received mastectomies. | Trans men between 18 and 70 at the time of surgery who underwent mastectomies between 9/1/2013 and 8/31/2018 in Copenhagen University Hospital, Denmark. N = 92 (Mage = 23). | Adult transmasculine men who underwent masculinizing top surgery (bilateral mastectomy) in Denmark revealed that 27% reported persistent pain following surgery. Of patients reporting pain, 90.1% experienced mild to moderate pain. Neuropathic pain was reported for n = 4 (4.8%) participants. |
| MacGregor and van den Brink (2019), United Kingdom and Netherlands | Review existing literature that describes issues relating migraines and migraine management, and hormone therapy in transgender men and women. | Literature review. | Trans adults undergoing HRT experiencing migraines. | There is a higher prevalence of migraines among transgender women taking estrogen, and is reduced amongst transgender men who take testosterone. Evidence suggests migraines with aura is associated with an increased risk of ischemic stroke in cisgender women, which is increased by the use of estrogen and other biological and behavioral factors. |
| Peitzmeier et al. (2017), USA | To understand the prevalence of negative health outcomes among adults who bind, identify risk factors for negative health outcomes, and develop recommendations for healthy binding informed by these risk factors. | Quantitative 32 item cross-sectional survey study administered online to a non-random sampled of adults over the age of 18 who were assigned female at birth, or self-identified as intersex. | Open to all people assigned female at birth and intersex individuals over 18 years (ages 18–66; Mage = 23) who bound either currently or at some point in their lives (n = 1800). Participants from over 38 countries were represented in data collection. | Mental health benefits were associated with chest binding. 97% of TGD individuals who engaged in chest binding experienced at least one negative physical symptom, with 54% reporting back pain and 49% chest pain. |
| Peitzmeier et al. (2021), USA | To assess the timeline of symptoms development related to binding in transgender youth | Quantitative cross-sectional survey study administered online to a non-random sampled of adults who were assigned female at birth. Assessed lifetime prevalence of 27 symptoms related to binding. | Data were part of a larger study open to all people assigned female at birth and intersex individuals over 18 years (ages: 18–66; Mage = 23) who bound either currently or at some point in their lives (n = 1800). Participants from over 38 countries were represented in data collection. This analysis focused on study participants between ages 18–24 (58% of the original sample). | Most symptoms related to binding emerged quickly, and most people who experienced these symptoms experienced them within their first binding year. Rarer outcomes and more serious outcomes took longer to occur. There was often rapid onset of pain and intensity continued to rise over time, peaking at 5 or more years of binding. |
| Sayeem et al. (2021), USA | To review the clinical presentation of eight youths with GD in a multidisciplinary chronic pain clinic | A retrospective chart review of youth who received care in a multidisciplinary chronic pain clinic who identified as experiencing gender dysphoria. | Participants were eight youths (Mage = 14.6) who attended a multidisciplinary chronic pain clinic and endorsed experiencing gender dysphoria from January 2017 to September 2019. Patients included in the cohort were being seen by an endocrinologist concurrently. | The mean age of the onset of pain symptoms was 11.25 years with a median of 4.5 visits to the pain program for chronic pain treatment. They have a mean Pain Burden Interview score of 12.86. Researchers found a downward trend in pain scores of patients who were treated for chronic pain and gender dysphoria. |
| Yalinay Dikmen et al. (2021), Turkey | To investigate the frequency, characteristics, and treatment of migraine and tension heads among trans men (FtM), as well as in relation to psychiatric comorbidities and lifetime experiences of being a trans person in Turkey | Quantitative cross-sectional survey study assessing demographics, gender identity transition inventory, psychological health outcomes, and experiences with headaches. | Participants were n = 88 trans men (FtM individuals) 18 years and older (Mage = 24.8) diagnosed and followed up by the psychiatry department for gender dysphoria between July 2018 and December 2019. | 36.4% of participants were diagnosed with migraines and 40.9% were diagnosed with tension headaches. Participants with migraines scored higher on depression and anxiety measures, experienced longer and more severe headaches, and higher likelihood of menstruation acting as a trigger than participants with tension headaches. Higher levels of care utilization for headaches was found among the participants with migraines. Overall, migraines and tension headaches were common in the study population. |
| Author, Year, Country . | Aims . | Study Design . | Study Population . | Main Findings . |
|---|---|---|---|---|
| Abern et al. (2022), USA | To determine the prevalence of self-reported vulvar pain symptoms and dyspareunia in this population and investigate its relationship to gender-affirming hormone therapy with testosterone. | Cross-sectional, quantitative study with a single time point survey | English-speaking trans men/masculine or AFAB individuals ages 18–64 (Mage = 27 years), n = 782. | Among the participants, 59.8% reported using testosterone. Unintentional pain with sexual intercourse was experienced in 61.5% of participants. Sixty-eight out of 710 (9.6%) participants endorsed vulvar pain symptoms; 61.8% were on testosterone. Trans-masculine individuals had a higher prevalence of dyspareunia than the general population, but the prevalence of vulvar pain was similar to that experienced among cis-gender women. |
| Aloisi et al. (2007), Italy | To study the relationship between sex hormones and pain. | Two-part semi-structured interview and questionnaire of transgender patients seen at the Movimetno Identita Transsuale Center in Bologna for at least 1 year of hormone treatment between December 2003 and December 2005. | Transgender patients (MtF, FtM) receiving hormone treatments for at least 1 year between ages 25–40, n = 73 (all Caucasian). | Results suggest that HRT might impact existing chronic pain and new pain experiences. |
| Anaya (2018), USA | Describe the experience of the impact of intersecting minority identifies of a transgender adolescent receiving psychiatric care for post-traumatic stress disorder (PTSD). | Case study describing the case of a transgender adolescent with PTSD, who experiences chronic pain, receiving care for physiologic dysregulation. | A case study of a 17-year-old Mexican-American transgender male who experienced a traumatic brain injury and consequently experienced PTSD and chronic pain. | The experience and manifestations of chronic pain and PTSD in this specific patient may likely be influenced by the stressors of his intersecting minority identities. |
| Lang et al. (2021), Denmark | To investigate the prevalence and severity of postsurgical persistent pain, sensory disturbances and complications in trans men after mastectomies | Cross-sectional questionnaire retrospectively evaluating postsurgical pain and disturbances in trans men who received mastectomies. | Trans men between 18 and 70 at the time of surgery who underwent mastectomies between 9/1/2013 and 8/31/2018 in Copenhagen University Hospital, Denmark. N = 92 (Mage = 23). | Adult transmasculine men who underwent masculinizing top surgery (bilateral mastectomy) in Denmark revealed that 27% reported persistent pain following surgery. Of patients reporting pain, 90.1% experienced mild to moderate pain. Neuropathic pain was reported for n = 4 (4.8%) participants. |
| MacGregor and van den Brink (2019), United Kingdom and Netherlands | Review existing literature that describes issues relating migraines and migraine management, and hormone therapy in transgender men and women. | Literature review. | Trans adults undergoing HRT experiencing migraines. | There is a higher prevalence of migraines among transgender women taking estrogen, and is reduced amongst transgender men who take testosterone. Evidence suggests migraines with aura is associated with an increased risk of ischemic stroke in cisgender women, which is increased by the use of estrogen and other biological and behavioral factors. |
| Peitzmeier et al. (2017), USA | To understand the prevalence of negative health outcomes among adults who bind, identify risk factors for negative health outcomes, and develop recommendations for healthy binding informed by these risk factors. | Quantitative 32 item cross-sectional survey study administered online to a non-random sampled of adults over the age of 18 who were assigned female at birth, or self-identified as intersex. | Open to all people assigned female at birth and intersex individuals over 18 years (ages 18–66; Mage = 23) who bound either currently or at some point in their lives (n = 1800). Participants from over 38 countries were represented in data collection. | Mental health benefits were associated with chest binding. 97% of TGD individuals who engaged in chest binding experienced at least one negative physical symptom, with 54% reporting back pain and 49% chest pain. |
| Peitzmeier et al. (2021), USA | To assess the timeline of symptoms development related to binding in transgender youth | Quantitative cross-sectional survey study administered online to a non-random sampled of adults who were assigned female at birth. Assessed lifetime prevalence of 27 symptoms related to binding. | Data were part of a larger study open to all people assigned female at birth and intersex individuals over 18 years (ages: 18–66; Mage = 23) who bound either currently or at some point in their lives (n = 1800). Participants from over 38 countries were represented in data collection. This analysis focused on study participants between ages 18–24 (58% of the original sample). | Most symptoms related to binding emerged quickly, and most people who experienced these symptoms experienced them within their first binding year. Rarer outcomes and more serious outcomes took longer to occur. There was often rapid onset of pain and intensity continued to rise over time, peaking at 5 or more years of binding. |
| Sayeem et al. (2021), USA | To review the clinical presentation of eight youths with GD in a multidisciplinary chronic pain clinic | A retrospective chart review of youth who received care in a multidisciplinary chronic pain clinic who identified as experiencing gender dysphoria. | Participants were eight youths (Mage = 14.6) who attended a multidisciplinary chronic pain clinic and endorsed experiencing gender dysphoria from January 2017 to September 2019. Patients included in the cohort were being seen by an endocrinologist concurrently. | The mean age of the onset of pain symptoms was 11.25 years with a median of 4.5 visits to the pain program for chronic pain treatment. They have a mean Pain Burden Interview score of 12.86. Researchers found a downward trend in pain scores of patients who were treated for chronic pain and gender dysphoria. |
| Yalinay Dikmen et al. (2021), Turkey | To investigate the frequency, characteristics, and treatment of migraine and tension heads among trans men (FtM), as well as in relation to psychiatric comorbidities and lifetime experiences of being a trans person in Turkey | Quantitative cross-sectional survey study assessing demographics, gender identity transition inventory, psychological health outcomes, and experiences with headaches. | Participants were n = 88 trans men (FtM individuals) 18 years and older (Mage = 24.8) diagnosed and followed up by the psychiatry department for gender dysphoria between July 2018 and December 2019. | 36.4% of participants were diagnosed with migraines and 40.9% were diagnosed with tension headaches. Participants with migraines scored higher on depression and anxiety measures, experienced longer and more severe headaches, and higher likelihood of menstruation acting as a trigger than participants with tension headaches. Higher levels of care utilization for headaches was found among the participants with migraines. Overall, migraines and tension headaches were common in the study population. |
Note. AFAB: assigned female at birth; AMAB: assigned male at birth; MtF: male-to-female; FtM: female-to-male; HRT: hormone replacement therapy; TGD: trans- and gender diverse.
Biological mediators of pain in TGD individuals have been proposed, with gender-affirming hormones affecting pain in some adults (Aloisi et al., 2007; Yalinay Dikmen et al., 2021). Gender affirming surgeries (GAS) are part of medical care for many TGD individuals (Canner et al., 2018), with the most common GAS in youth being chest masculinization (also referred to as “mastectomy” or “top surgery”) (Handler et al., 2019). Positive outcomes related to gender affirmation and psychological well-being have been documented in youth GAS (Tang et al., 2022), however, little is known about postsurgical pain outcomes. In adults, post-mastectomy pain was present in a quarter of individuals undergoing the surgery for gender affirmation, but this pain was generally mild-moderate and managed with mild analgesics (Lang et al., 2021). Other social transition efforts to affirm gender identity (e.g., certain unsafe forms of chest binding) might also carry pain-related consequences despite mental health benefits (Peitzmeier et al., 2017, 2021).
Compared to adults, TGD youth are even further underrepresented in pain research. A recent case series describes greater depression, functional disability, and fear of pain relative to a matched sample of cisgender youth with chronic pain (Burns et al., 2020). Some quantitative studies have described pain experiences of TGD youth (see Table I), reporting health disparities and highlighting the need for inclusive, gender affirming approaches to pain care. Overall, TGD youth are theoretically at increased risk of experiencing pain and worse pain-related outcomes but are significantly underrepresented in pain literature, leading to a lack of understanding of their pain and healthcare experiences.
Key Knowledge Gaps
Prevalence of Acute and Chronic Pain, and Pain Experiences Specific to TGD Youth
Acute pains are common in childhood, with nearly all children experiencing at least one painful event (e.g., illness, injury, medical procedure) a month (van Dijk et al., 2006). Chronic pain that significantly interferes with daily functioning is estimated to be present in 3–5% of the general population of youth, though such rates are higher if non-disabling pain is also considered (King et al., 2011). While prevalence studies report increased rates of pain among girls and women following puberty, studies only examine prevalence of pain in relation to sex assigned at birth or conflate sex and gender. To date, most research on TGD youth has examined mental health and suicidality, substance use, and trauma exposure, while physical health is rarely assessed (Pike et al., 2023). Given the increased risk of developing chronic pain among TGD youth, work is needed to understand the prevalence of pain and functional impact in TGD youth. Pain experiences specific to TGD populations also warrant attention, including iatrogenic pain from hormone injections, unsafe tucking practices, and postural-related musculoskeletal pain for youth without binder access.
The Meaning of Pain in the Context of Gender Identity and Affirmation
Pain is highly individual, and the meaning that one attributes to pain (e.g., neutral vs. threatening, helpful vs. annoying) is influenced by the context in which the pain is experienced and the individual’s interpretation of that experience. The meaning of post-surgical pain in the context of gender affirmation may be different than for illness- or injury-related surgeries. While more research is needed, positive affect associated with gender affirmation and appearance congruence may mediate the impact of GAS on pain and functional outcomes. Indeed, emerging literature suggests when youth can live in line with their gender identity it can be a powerfully positive experience which may buffer against pain-related stressors or facilitate coping with pain related to gender affirming practices (Harrison et al., 2023). Understanding the meaning of pain for TGD youth should incorporate an understanding of both how gender-related factors can be a source of both risk (i.e., systematically through minority stressors) but also can promote strength and resiliency through factors such as gender euphoria and a sense of belonging or community.
Both pain and gender are embodied experiences, where there may be dissonance between one’s body and what it represents from one’s identity. While embodiment has been discussed in both the transgender health (Huttunen et al., 2019) and pain literatures (Tabor et al., 2017), these areas of research have not been brought together. This may be relevant to explore in the context of stereotypically gendered pain experiences in TGD youth (e.g., dysmenorrhea in trans masculine youth), whereby pain may serve as a sense of disconnection between identity and body.
Diversity Within Gender Identities and Intersectionality
Due to underrepresentation of TGD youth in pediatric pain research, sample sizes are often so small that diverse identities are combined into an “Other” category (e.g., encompassing non-binary, genderfluid, and transgender youth), but increasing evidence from other fields of research suggests this approach is inappropriate (Burgwal et al., 2019; Johnson et al., 2020). Even within a single gender identity, the experience of that identity and its relationship to pain can vary significantly. For example, researchers may consider the different influences on pain among TGD youth who engage in gender-affirming medical treatments versus those who undergo social transition alone. Youth who socially transition may experience minority stressors that influence pain, pain from social transition efforts to affirm gender identity (pain from unsafe binding or tucking), or changes to their gendered social interactions around pain. However, unique to youth who engage in gender-affirming medical treatments are hormone-related pain changes or procedural/surgical pain from gender-affirming medical procedures. The relationship between gender and pain may also differ based on the extent to which the youth identifies with a specific gender, experiences their gender as fluid, or eschews the practice of assigning labels to gender experience (Harrison et al., 2023). Youth who identify as agender or non-binary may have different experiences of gendered pain norms than youth with a binary transgender identity. More research is needed to understand how psychological flexibility about gendered pain behaviors, as well as the social dismantling of binary gender, might inform pain experiences of TGD youth, and their interactions with their families, care providers, and community.
One cannot consider the role of gender and gender diversity in pain without applying an intersectional framework. Intersectionality is a concept that arose out of Black feminist scholarship describing how intersecting identities and social positions intersect to create systems of power, privilege, and marginalization (Crenshaw, 1989). Intersectional frameworks may be used to understand the diversity observed within pain and healthcare experiences of a specific gender identity, particularly other identities associated with oppressive systems. While literature on intersectionality and pediatric pain is still emerging, there are a few examples: in sickle-cell disease, it has been demonstrated that older girls exposed to increased racial bias report decreased health-related quality of life, which is hypothesized as being related to the unique forms of racial bias and societal expectations of pain Black girls experience (Hood et al., 2022). Research has also identified interactions between gender identity and sexual orientation (Katz-Wise et al., 2015), as well as gender identity and neurodiversity (Harrison et al., 2023), as being relevant to chronic pain outcomes. Traumatic experiences, both direct and vicarious, may be particularly relevant for understanding pain experiences of youth who are exposed to anti-trans rhetoric in conjunction with other forms of oppression, such as racism and ableism. Previous research has demonstrated that adverse childhood experiences, a known risk factor for pain (Nelson et al., 2021), are higher amongst individuals who have intersecting identities of being female-identifying, marginalized race or ethnicity, low household income, and minoritized sexual orientation (Giano et al., 2023; Kim et al., 2023). Intersectional perspectives can also be used to highlight unique sources of strength and resilience, for example, having affinity to a supportive community. Researchers, funding bodies, and journals are increasingly adopting frameworks such as A.D.D.R.E.S.S.I.N.G. (Hays, 2022) to capture intersectional identities in research.
An Ecological-Systems Model of Understanding Pain in TGD Youth
With intersectionality in mind, we propose a theoretical model synthesizing socio-ecological, cumulative stress, and biopsychosocial models of understanding pain in this population (Figure 1). While there is longstanding support for the biopsychosocial model in pain, the Ecological-Systems model was included as it has been previously applied to experiences of marginalized populations and to pediatric chronic pain (Johns et al., 2018; Katz-Wise et al., 2022; Logan et al., 2012). The model was adapted from an existing framework by Bakhshaie and colleagues and incorporates concepts from existing models of gender influences in pain (Keogh, 2021) and minority stress (Bakhshaie et al., 2022; Christian et al., 2021).
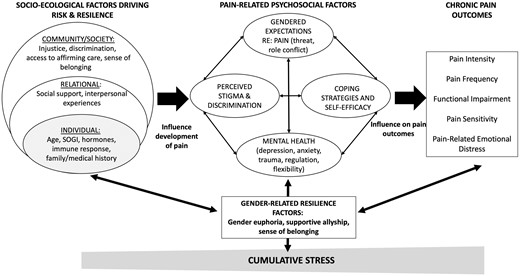
Socio-ecological factors related to the experience of gender diversity and pain, their impact on pain-related psychosocial factors, and pain-related outcomes. Adapted from Bakhshaie et al. (2022) SOGI = sexual orientation and gender identity.
Socio-ecological factors at individual, relational, and societal levels influence the development of pain. These factors influence psychosocial responses to pain, add to cumulative stress, and may diminish coping capacity and perpetuate pain-related disability. Alternatively, the influence of factors that promote resilience and coping amongst TGD youth, including the presence of queer communities and supportive allyship as well as resistance to sources of oppression (Paceley et al., 2021), must also be considered and fostered in the context of pain care.
Increasing Inclusivity in Pediatric Pain Research: Next Steps
Significant inadequacies in assessment of gender identity in youth with chronic pain has contributed to their underrepresentation in research. Additionally, the structure and norming of measurement tools has historically been binary, heteronormative, and cisnormative (binary body maps, limited forced choice items assessing gender and sexual orientation, binary assessment of pubertal development). To address this issue, the Trevor Project has been developing best practice recommendations for inclusive assessment of gender identity, shaped in large part by data from their National Survey on LGBTQ Youth Mental Health collected in 2019, 2020, and 2021. Current best practice recommendations include using an open-response item about gender identity and two forced choice items asking about (1) gender identity and (2) sex assigned at birth.1 As language can quickly change, researchers and clinicians should be prepared to continue refining and adapting gender identity items over time. Providers should also be aware of whether the youth’s gender identity is something they share openly with their parents and take care to safeguard this information if not.
Sample sizes for research on TGD youth with pain may be smaller than studies of cisgender youth. Qualitative research may provide an opportunity to better understand some of the key knowledge gaps described above, including taking an intersectional perspective in understanding how TGD youth experience gender role norms related to pain, navigate ableism, experience healthcare interactions, and make sense of their pain. Additionally, research using methods such as Ecological Momentary Assessment may provide sufficient data to understand temporal experiences of TGD youth with pain, such as how gender euphoria may buffer against negative outcomes in the context of acute and chronic pain experiences of minority stressors influence acute or chronic pain outcomes.
Many opportunities also exist for understanding how to provide affirming pain care for TGD youth. While (assumed cisgender) girls and boys show differences in chronic pain and psychological treatment outcomes, little is known regarding the therapeutic experiences of gender-diverse youth (Boerner et al., 2017). There is relevant existing literature on affirming interventions and support that could be incorporated into evidence-based psychological therapies for pain (Coyne et al., 2020). Empirically supported treatments for mental health concerns demonstrate equal effectiveness for TGD youth, but with slower and less reliable improvements, and lower youth-reported satisfaction compared to cisgender youth (Hollinsaid et al., 2020). With high rates of trauma reported among TGD youth, and the association between trauma and chronic pain, effective treatments for chronic pain in TGD youth may require treatment of co-occurring trauma, or at a minimum, trauma-informed care delivery (Nelson et al., 2021). Adaptations may also be informed by literature on treatment considerations for TGD populations with related concerns, such as orthopedic conditions or functional neurological disorders (Lerario et al., 2023; Meneses et al., 2023).
Pediatric psychologists can also help other medical providers better serve TGD youth. For instance, guidelines exist for the post-operative care of TGD patients presenting for GAS, which could also be applied when TGD patients are managing post-operative pain related to other surgeries (Tollinche et al., 2018). Psychologists can also help identify how systemic barriers and discrimination impact treatment compliance. For instance, TGD youth and young adults report lower levels of physical activity compared to cisgender peers (Bishop et al., 2020), often related to the gendered culture of sports, which may interfere with pain rehabilitation treatment.
Conclusion
Despite a significant need, research to inform the clinical care of TGD youth with pain is lacking. A myriad of resources exists within other areas of trans health and gender studies more generally to support researchers in developing ethical, appropriate protocols for study (Bauer et al., 2019). Community-engaged research is critical to guide work in this space, from the inception of projects through to dissemination and translation to practice. Thoughtful consideration is needed in determining how to assess gender and intersectional identities and incorporate into pain research efforts, regardless of whether this is the primary focus of study. Ongoing efforts to increasing equity and inclusion of TGD youth in pediatric pain psychology research and practice will help improve access to tailored interventions, understand how pediatric psychologists can support painful aspects of gender affirmation, provide education to our clinical colleagues, and dismantle the systemic cisnormative barriers to safe pain care access for TGD youth.
Footnotes
Most recent recommendations, as of June 2023, are available at https://www.thetrevorproject.org/wp-content/uploads/2021/07/Measuring-Youth-Sexual-Orientation-and-Gender-Identity.pdf
Author Contributions
Katelynn Elizabeth Boerner (Conceptualization [lead], Writing—original draft [equal], Writing—review & editing [equal]), Lauren E. Harrison (Conceptualization [lead], Writing—original draft [equal], Writing—review & editing [equal]), Eleanor Battison (Conceptualization [supporting], Data curation [equal], Writing—original draft [equal], Writing—review & editing [equal]), Corrin Murphy (Data curation [equal], Writing—original draft [equal], Writing—review & editing [equal]) and Anna Camille Wilson (Conceptualization [supporting], Supervision [equal], Writing—original draft [equal], Writing—review & editing [equal])
Funding
K.E.B. was supported by a postdoctoral fellowship from the Canadian Child Health Clinician Scientist Program during the preparation of this manuscript. An earlier version of this review and model was presented at the 2023 Society of Pediatric Psychology Annual Conference.
Conflicts of interest: None declared.
Data Availability
No new data were generated or analyzed in support of this research.



